Introduction
Hepatic ischemia/reperfusion (I/R) injury is a major
cause of liver dysfunction and is a common consequence of liver
surgery, particularly following hepatectomy and liver
transplantation. The restoration of the blood supply following a
period of ischemia or lack of oxygen will generally cause I/R
injury. Systemic low-flow ischemia and hypoxia, such as trauma,
hemorrhagic shock, sepsis, congestive heart failure and respiratory
failure, may also lead to hepatic I/R injury. Hepatic I/R injury
can make patients prone to lethal complications of liver diseases
(1), involving numerous
pathophysiological processes, such as an increase in inflammatory
mediators and cytokines, Kupffer cell activation and release of
oxygen free radicals (2,3). The prevention and treatment of hepatic
I/R injury is an important clinical problem, which can help with
the treatment of severe liver disease and improve the outcome of
liver transplantation.
Preconditioning has a significant preventive effect
on hepatic I/R injury by inducing the endogenous protective
mechanism of cells (4,5). This includes ischemia, pharmacological
and ozone oxidative preconditioning. Ischemia preconditioning is
limited due to its safety, operability and the individual
differences of patients. Pharmacological modulation may currently
have a more universal application. Characteristics include more
safety, simple operation, no other specialist instrument required
and ease of facility, and it has become of current interest in
recent years (6).
Minocycline (Mino) is a semisynthetic tetracycline
antibiotic that exhibits anti-inflammatory, antiapoptotic,
antioxidant and immunosuppression properties (7). Previous studies have reported that
Mino has protective effects in the kidney, brain and retinal I/R
injury (8–10). However, the effect of Mino on liver
I/R injury remains unknown. In the present study, the aim was to
evaluate the hepatoprotective effect of Mino on rat I/R liver
injury and investigate the underlying mechanism, providing novel
insights into Mino treatment for I/R liver injury.
Materials and methods
Animals
The protocols of animal use and care conformed to
the Guide for the Care and Use of Laboratory Animals from the
National Institutes of Health and were approved by the Animal Care
and Use Committee of Central South University (Changsha, Hunan,
China). Male Sprague-Dawley rats (250–300 g) were purchased from
the Animal Center of the Second Xiangya Hospital, Central South
University. The rats were housed under temperature-controlled
conditions with a 12-h light/dark cycle and ad libitum
access to water and food. The rats were randomly divided into three
groups: i) sham-operated group (control group), which isolated the
blood vessels of the left and middle liver lobe, but did not clamp,
and the abdomen was subseqeuently closed without treatment and
medication; ii) I/R model (I/R group) as below; and iii) Mino
preconditioning group (Mino group), in which the rats were
administered Mino (45 mg/kg; Sigma, St. Louis, MO, USA) by gastric
irrigation at 36 h before surgery and were subsequently
administered with 22.5 mg/kg every 12 h for the 36 h before
surgery. Each group comprised 18 rats.
Hepatic I/R injury
The rats underwent hepatic I/R or sham surgery.
Partial hepatic ischemia was induced as previously described
(11). In brief, the rats were
anesthetized with isoflurane. A midline laparotomy was performed
and an atraumatic clip (Fine Science Tools, Foster City, CA, USA)
was placed across the portal vein, hepatic artery and bile duct to
interrupt the blood supply to the left lateral and median lobes
(~70%) of the liver. After 90 min of partial hepatic ischemia, the
clip was removed to initiate reperfusion. The abdomen was closed
with 4–0 silk sutures and the animals were allowed to awaken and
were provided free access to food and water. Sham control rats
underwent the same protocol without vascular occlusion. Rats were
sacrificed at 2, 6 and 24 h after reperfusion and samples of blood
and ischemic lobes were collected for analyses.
Biochemical analysis
Blood was drawn from the postcava and centrifuged at
3,000 x g for 10 min. Serum was collected and stored at −20°C.
Levels of alanine aminotransferase (ALT), aspartate
aminotransferase (AST) and lactate dehydrogenase (LDH) in the serum
were measured with an autobiochemical analyzer (Hitachi, Tokyo,
Japan).
Liver samples were obtained from the median lobe,
washed in cold saline and quickly placed into −196°C liquid
nitrogen during sampling and maintained at −80°C until use. Prior
to detection, the samples were first unfrozen at 4°C and
subsequently homogenized in ice-cold phosphate buffer (pH 7.4). The
homogenates that were centrifuged at 3,500 x g for 10 min at 4°C
were used to determine the level of malondialdehyde (MDA) and
myeloperoxidase (MPO), and were assessed with a spectrophotometer
at 532 and 460 nm, respectively. The protein level in the liver
homogenates was measured using colorimetric assay kits (Jiancheng
Bioengineering, Nanjing, China).
Light microscopic examination
Liver specimens of the left lateral lobe were
sectioned, fixed in 10% (w/v) formalin buffer and embedded in
paraffin. The sections were cut into 4-µm sections and stained with
hematoxylin/eosin for histological examination with a light
microscope. The histological severity of I/R injury was graded
using Suzuki's criteria (Table I).
The quantification of the injured area was conducted in a
double-blind manner by involving at least two independent
investigators.
 | Table ISuzuki's criteria of hepatic
ischemia/reperfusion injury. |
Table I
Suzuki's criteria of hepatic
ischemia/reperfusion injury.
| Score | Congestion (%) | Vacuolization
(%) | Necrosis (%) |
|---|
| 0 | None | None | None |
| 1 | Minimal (10) | Minimal (10) | Single cell
necrosis |
| 2 | Mild (11~30) | Mild (11~30) | Mild (<30) |
| 3 | Moderate (31~60) | Moderate (31~60) | Moderate
(<60) |
| 4 | Severe (>60) | Severe (>60) | Severe (>60) |
Quantitative polymerase chain reaction
(qPCR)
RNA was extracted from liver tissues using
TRIzol® reagent (Invitrogen Life Technologies, Grand
Island, NY, USA) and converted into cDNA as described using the
primer oligo(dT)15 and Moloney murine leukemia virus reverse
transcriptase (Promega Corporation, Madison, WI, USA) at 42°C for
60 min. qPCR was performed with the following specific primers
using the SYBR-Green PCR Master mix (Takara, Liaoning, China):
Mouse tumor necrosis factor-α (TNF-α) forward, 5′-AGGGTCT
GGGCCATAGAACT-3′; and reverse, 5′-CCACCACGCTCT TCTGTCTAC-3′;
interleukin-1β (IL-1β) forward, 5′-GCAAC
TGTTCCTGAACTCAACT-3′; and reverse, 5′-ATCTTTTGG GGTCCGTCAACT-3′;
and β-actin (used as an internal positive control) forward,
5′-CCCATCTATGAGGGTTACGC-3′; and reverse,
5′-TTTAATGTCACGCACGATTTC-3′. The experiments were repeated three
times independently under identical conditions. The relative
density expressed as a ratio of target genes/β-actin is
presented in the present study.
Western immunoblot analysis
Ground tissues were lysed with
radioimmunoprecipitation assasy buffer, containing 50 mmol/l
Tris-HCl (pH 7.5), 150 mmol/l NaCl, 1% Nonidet P40, 1% sodium
deoxycholate, 1% inhibitor of phosphatase, 0.1% protease and 1
mmol/l phenylmethanesulfonylfluoride. Lysates (20–100 µg of protein
per lane) were separated by SDS/PAGE (10% gels) and transferred on
to nitrocellulose membranes. The membranes were incubated with
primary antibodies as follows: Dickkopf-1 (DKK-1) rabbit monoclonal
antibody (cat. no. ab109416), β-catenin rabbit monoclonal antibody
(cat. no. ab32572) and tubulin rabbit polyclonal antibody(cat. no.
ab126165) (Abcam, San Francisco, CA, USA). The filters were washed
and incubated with horseradish peroxidase donkey anti-rabbit Ab
(Abcam). Relative quantities of DKK-1 and β-catenin protein were
determined using a densitometer (Kodak Digital Science 1D analysis
software; Rochester, NY, USA).
Statistical analysis
All the data were performed with SPSS version 11.5
software (SPSS Inc., Chicago, IL, USA) and expressed as mean ±
standard deviation. Student's t-test was used to evaluate the
statistical significance. P<0.05 was considered to indicate a
statistically significant difference.
Results
Levels of ALT, AST and LDH in
serum
After reperfusion for 2, 6 and 24 h, the levels of
AST, ALT and LDH were higher in the I/R and Mino groups compared to
the control group at each time point and reached the peak at 6 h
after reperfusion (P<0.05). Whereas the levels of AST, ALT and
LDH in the serum were significantly reduced in the Mino group
compared to those in the I/R group (Table II; P<0.05).
 | Table IIRat serum levels of ALT, AST and LDH
in each group after 2, 6 and 24 h reperfusion. |
Table II
Rat serum levels of ALT, AST and LDH
in each group after 2, 6 and 24 h reperfusion.
| Index | Groups | No. of rats | 2 h | 6 h | 24 h |
|---|
| ALT | Con | 6 | 64.37±13.65 | 70.80±8.11 | 64.20±7.49 |
| ALT | I/R | 6 |
617.33±69.63a |
1305.60±255.40a |
270.90±23.42a |
| ALT | Mino | 6 |
255.90±28.04a,b |
516.93±72.50a,b |
121.20±11.10a,b |
| AST | Con | 6 | 161.57±26.88 | 171.35±25.47 | 152.08±21.76 |
| AST | I/R | 6 |
1524.70±315.26a |
2488.1±365.52a |
743.47±61.59a |
| AST | Mino | 6 |
908.98±80.40a,b |
1533.47±319.70a,b |
511.20±45.25a,b |
| LDH | Con | 6 | 256.23±32.11 | 311.70±56.72 | 258.30±37.18 |
| LDH | I/R | 6 |
2467.21±322.70a |
3601.34±345.33a |
1909.65±197.30a |
| LDH | Mino | 6 |
988.67±103.46a,b |
1763.98±579.23a,b |
879.56±231.78a,b |
Effect of Mino on liver antioxidant
ability
There were no clear changes of MDA and MPO levels in
the control group at each time point. Compared to the control, the
MDA and MPO levels increased in I/R group after reperfusion for 2,
6 and 24 h. Following Mino treatment, the MDA and MPO levels were
markedly decreased compared to those in the I/R group (Table III; P<0.05).
 | Table IIILevel of MDA and MPO in rat liver
tissues following hepatic ischemia/reperfusion at different time
point in each group. |
Table III
Level of MDA and MPO in rat liver
tissues following hepatic ischemia/reperfusion at different time
point in each group.
| Index | Groups | No. of rats | 2 h | 6 h | 24 h |
|---|
| MDA | Con | 6 | 4.07±1.21 | 4.25±1.02 | 4.01±1.36 |
| MDA | IR | 6 |
16.81±4.17a |
27.43±5.09a |
14.95±2.31a |
| MDA | Mino | 6 |
9.52±2.14a,b |
15.23±2.97a,b |
8.47±1.91a,b |
| MPO | Con | 6 | 1.01±0.98 | 1.98±1.20 | 0.96±3.17 |
| MPO | IR | 6 |
5.31±5.47a |
7.28±1.76a |
4.96±2.17a |
| MPO | Mino | 6 |
2.98±0.79a,b |
3.47±3.70a,b |
2.20±4.25a,b |
Liver histology in the ischemia model
followed by reperfusion
The control group showed no marked abnormalities in
liver tissue morphology after reperfusion for 2, 6 and 24 h. The
boundaries between liver cell cords and hepatic sinusoids became
unclear in the I/R group after 2 h reperfusion. Furthermore,
inflammatory cell accumulation, oncosis and apoptosis of the liver
cells were evidently observed after 6 h of reperfusion in the I/R
group. After reperfusion for 24 h, the histopathological changes
started to improve. However, in the Mino group, the liver cells had
less swelling, remained well arranged and had no clear signs of
oncosis and apoptosis; but the hepatic sinusoid was dilated
following reperfusion (Fig. 1).
Compared to the I/R group, the Suzuki scores decreased in the Mino
group in regards to hepatic congestion, vacuolization and necrosis
(Table IV).
 | Table IVSuzuki's for each group at different
time points. |
Table IV
Suzuki's for each group at different
time points.
| Group | 2 h | 6 h | 24 h |
|---|
| Con | 0 | 0 | 0 |
| IR |
5.50±1.76a |
8.17±1.33a |
5.50±2.26a |
| Mino |
3.33±0.52a,b |
5.67±1.37a,b |
3.33±0.52a,b |
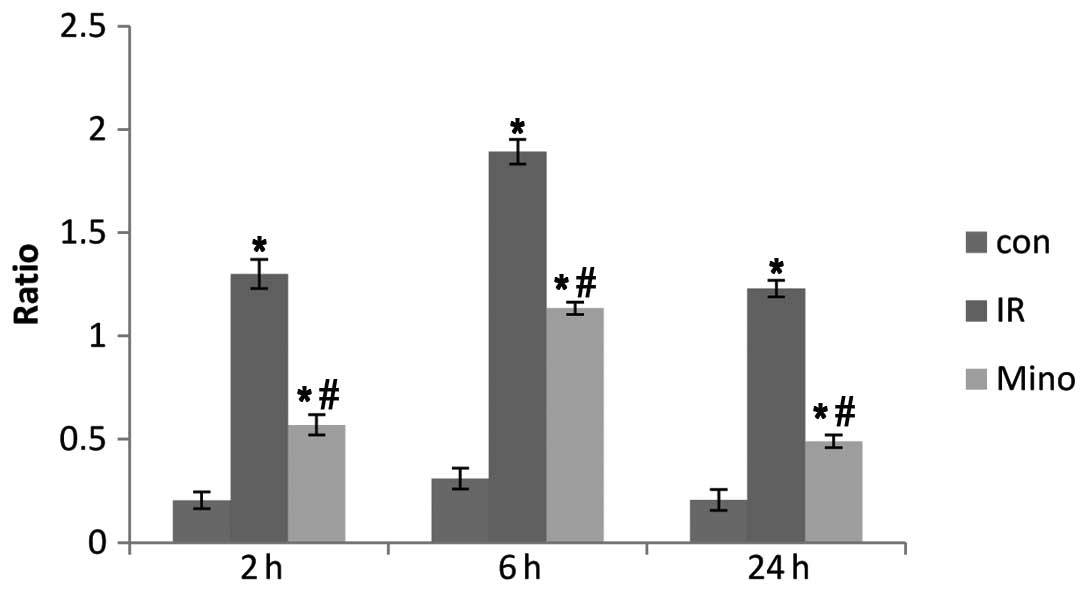
Levels of TNF-α and IL-1β mRNA
TNF-α and IL-1β levels at 2, 6 and 24
h after reperfusion were significantly increased in the I/R and
Mino groups compared to the control group (P<0.05). However,
following treatment with Mino, the mRNA expression of TNF-α
and IL-1β decreased compared to the I/R group at each time
point (Figs. 2 and 3; P<0.05).
Expressions of DKK-1 and β-catenin in
liver tissues
DKK-1 and β-catenin protein expression of rat liver
tissues was detected in each group after 24 h reperfusion using
western blot analysis. The results showed that there was no evident
expression of DKK-1 in the control group. The protein expression of
DKK-1 was upregulated by 77.8% in the I/R group, and when compared
to the I/R group, it decreased by 44.4% in Mino group
(P<0.05).
By contrast, the protein expression of β-catenin was
downregulated by 72.2% in the I/R group compared to the control.
Following Mino treatment, it increased by 55.6% compared to the I/R
group, but it remained lower than the control (Fig. 4, P<0.05).
Discussion
Hepatic I/R injury is a complex multifactorial
pathophysiological process (12),
and it also has a wide range of clinical concern. Studies have
shown that pharmacological preconditioning has a significantly
preventive effect on hepatic I/R injury. In addition to the
antimicrobial actions of Mino, previous studies have demonstrated
its cytoprotective potential in a variety of settings, including
ischemic cardiac, renal and central nervous system disease. In the
present study, hepatic injury after reperfusion for 6 h was more
pronounced compared to 2 and 24 h, which is consistent with the
previous study on the rat hepatic I/R model by Zhou et al
(13). Furthermore, pretreatment
with Mino prior to ischemia and the subsequent reperfusion
significantly reduced congestion, edema, vacuolization and necrosis
of liver cells and protected the hepatic cells against I/R injury
in a rat model. As for the protective effect, there may be a number
of essential components participating in the procedure, including
MDA, MPO and certain pro-inflammatory cytokines.
The damage to the liver caused by reperfusion is
more serious than ischemia. Previous studies have shown that it is
mainly the Kupffer cells and complement activation, and aggregation
and cluster of differentiation 4+ lymphocytes activation
in the early stage of hepatic I/R injury (14). Once the Kupffer cells are activated,
they release large amounts of pro-inflammatory cytokines (TNF-α and
IL-1), the lipid inflammatory mediators and oxygen free radicals,
which mediate liver injury (15,16).
As a pro-inflammatory cytokine, TNF-α can result in liver
microcirculation disturbance by interacting with neutrophils and
endothelial cells. In addition, IL-1β is considered to be a valid
target for therapeutic intervention in diseases associated with
tissue remodeling (17). Thus,
downregulation of the level of TNF-α and/or IL-1β
will be beneficial for the alleviation of I/R injury. In the
present study, the expression of TNF-α and IL-1β was
significantly reduced by Mino, and the levels of serum ALT, AST and
LDH decreased in comparison to the I/R group. Therefore, it is
speculated that Mino performs its liver protective effect mainly
due to the suppression on Kupffer cells, which can further
influence the expression of TNF-α and IL-1β.
Additionally, this decrease in inflammation coincided with a
greatly reduced level of MPO in liver tissue, indicating the
prevention of neutrophil infiltration into the liver following I/R
with Mino treatment.
Oxidative stress plays an important role in the
development of hepatic I/R injury. Reducing oxygen radicals is one
of the goals to intervene the hepatic I/R injury. Due to the
presence of the diethyamino group on the phenolic carbon, Mino has
a superior scavenging ability (18). MDA and MPO are regarded as the
indirect indexes reflecting the levels of oxygen free radical and
degree of lipid peroxidation. In the present study, the
pretreatment of Mino reduced the MDA and MPO levels in liver tissue
and subsequently further improved the antioxidant ability of the
liver. The result shows that Mino inhibited liver oxidative damage
through its antioxidant ability.
The liver differs from other visceral organs in its
innate ability for short-term regeneration (19). Therefore, therapy aimed at
stimulating the pathways involved in the proliferation of new
hepatocytes to replace dead/damaged cells, or at conditioning cells
to respond differently to an ischemic insult, may prove
particularly beneficial in cases of hepatic I/R. One crucial
pathway in cell replication and regeneration is the Wnt/β-catenin
signaling axis. Canonical Wnt signaling has been identified as
central to embryonic development, progenitor cell differentiation
and proliferation of cells arising from all three germ layers
(20,21). Additionally, Wnt/β-catenin signaling
has been shown to play a key role specifically in liver
development, prevention of apoptosis and protection from metabolic
stress (22). β-catenin, 88 kDa, is
a dual function protein, regulating the coordination of cell-cell
adhesion and gene transcription. DKK-1 is known to be a secreted
protein that functions as a negative regulator of Wnt signaling and
plays a crucial role in inducing various tumor cells apoptosis. A
previous study showed that the Wnt agonist protects against hepatic
I/R injury through its known proliferative and anti-apoptotic
properties (23).
Funato et al (24) reported the important links between
oxidative stress and the canonical Wnt signaling pathway. Essers
et al (25) have identified,
as a protective reaction, that β-catenin can bind directly to
forkhead box O (FoxO), enhance FoxO transcriptional activity in
mammalian cells and regulate cell cycles, thus reducing the liver
damage of oxidative stress. Previous studies have shown that liver
damage is mainly caused by energy metabolism and oxidative stress,
and oxidative stress is believed to be the initiating factor in I/R
injury (26). The results of the
present study showed that the expression of β-catenin in the I/R
group was significantly lower compared to the control group, while
DKK-1 expression was significantly increased, indicating that the
Wnt/β-catenin signaling pathway is inhibited during the hepatic I/R
injury. Compared to the I/R group, the expression of β-catenin in
the Mino group was increased and DKK-1 expression was decreased,
the oncosis and apoptosis in liver tissue were reduced, MDA and MPO
production was reduced, and TNF-α and IL-1β mRNA
expression was downregulated. All these results indicate that Mino
protects the liver from I/R injury mainly through reducing
oxidative stress and inhibiting the release of pro-inflammatory
cytokines by activating Wnt/β-catenin signaling pathway in the
liver.
In conclusion, Mino has a protective effect on
hepatic I/R injury in rats, but whether it has a dose-dependent
manner requires further investigation.
References
|
1
|
Subhas G, Gupta A, Bakston D, et al:
Protective effect of methylprednisolone on warm
ischemia-reperfusion injury in a cholestatic rat liver. Am J Surg.
199:377–381. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Schauer RJ, Kalmuk S, Gerbes AL, et al:
Intravenous administration of glutathione protects parenchymal and
non-parenchymal liver cells against reperfusion injury following
rat liver transplantation. World J Gastroenterol. 10:864–870.
2004.
|
|
3
|
Su JF, Guo CJ, Wei JY, et al: Protection
against hepatic ischemia-reperfusion injury in rats by oral
pretreatment with quercetin. Biomed Environ Sci. 16:1–8.
2003.PubMed/NCBI
|
|
4
|
Que X, Debonera F, Xie J, et al: Pattern
of ischemia reperfusion injury in a mouse orthotopic liver
transplant model. J Surg Res. 116:262–268. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Jaeschke H: Reperfusion injury after warm
ischemia or cold storage of the liver: role of apoptotic cell
death. Transplant Proc. 34:2656–2658. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Jaeschke H: Molecular mechanisms of the
hepatic ischemia-reperfusion injury and preconditioning. Am J
Physiol Gastrointest Liver Physiol. 284:G15–G26. 2003.PubMed/NCBI
|
|
7
|
Griffin MO, Ceballos G and Villarreal FJ:
Tetracycline compounds with non-antimicrobial organ protective
properties: possible mechanisms of action. Pharmacol Res.
63:102–107. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yu XD, Wu XH, Du XW, et al: Protective
effects of minocycline on renal ischemia-reperfusion injury in
rats. J Chongqing Med Univ. 32:1172–1174. 2007.
|
|
9
|
Plane JM, Shen Y, Pleasure DE, et al:
Prospects for minocycline neuroprotection. Arch Neurol.
67:1442–1448. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Abcouwer SF, Lin CM, Shanmugam S, et al:
Minocycline prevents retinal inflammation and vascular permeability
following ischemia-reperfusion injury. J Neuroinflammation.
10:1492013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zhai Y, Shen XD, O'Connell R, et al:
Cutting Edge: TLR4 activation mediates liver ischemia/reperfusion
inflammatory response via IFN regulatory factor 3-dependent
MyD88-independent pathway. J Immunol. 173:7115–7119. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Xing HC, Li LJ, Xu KJ, et al: Intestinal
microflora in rats with ischemia/reperfusion liver injury. J
Zhejiang Univ Sci B. 6:14–21. 2005. View Article : Google Scholar
|
|
13
|
Zhou JX, Ye QF, Ming YZ, et al: Effects of
PNS on expression of nuclear factor-κB and ICAM-1 in rat liver
graft after ischemia reperfusion. Chin J Mod Med. 15:1330–1332.
2005.
|
|
14
|
Fondevila C, Busuttil RW and
Kupiec-Weglinski JW: Hepatic ischemia/reperfusion injury - a fresh
look. Exp Mol Pathol. 74:86–93. 2003. View Article : Google Scholar
|
|
15
|
Thobe BM, Frink M, Hildebrand F, et al:
The role of MAPK in Kupffer cell toll-like receptor (TLR) 2-,
TLR4-, and TLR9-mediated signaling following trauma-hemorrhage. J
Cell Physiol. 210:667–675. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Tsung A, Hoffman RA, Izuishi K, et al:
Hepatic ischemia/reperfusion injury involves functional TLR4
signaling in nonparenchymal cells. J Immunol. 175:7661–7668. 2005.
View Article : Google Scholar
|
|
17
|
Kolb M, Margetts PJ, Anthony DC, et al:
Transient expression of IL-1beta induces acute lung injury and
chronic repair leading to pulmonary fibrosis. J Clin Invest.
107:1529–1536. 2001. View
Article : Google Scholar : PubMed/NCBI
|
|
18
|
Griffin MO, Fricovsky E, Ceballos G, et
al: Tetracyclines: a pleitropic family of compounds with promising
therapeutic properties. Review of the literature. Am J Physiol Cell
Physiol. 299:C539–C548. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Fausto N, Campbell JS and Riehle KJ: Liver
regeneration. Hepatology. 43 (2 Suppl 1):S45–S53. 2006. View Article : Google Scholar
|
|
20
|
Kwon C, Arnold J, Hsiao EC, et al:
Canonical Wnt signaling is a positive regulator of mammalian
cardiac progenitors. Proc Natl Acad Sci USA. 104:10894–10899. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Masckauchan TN, Shawber CJ, Funahashi Y,
et al: Wnt/beta-catenin signaling induces proliferation, survival
and interleukin-8 in human endothelial cells. Angiogenesis.
8:43–51. 2005. View Article : Google Scholar
|
|
22
|
Behari J, Yeh TH, Krauland L, et al:
Liver-specific beta-catenin knockout mice exhibit defective bile
acid and cholesterol homeostasis and increased susceptibility to
diet-induced steatohepatitis. Am J Pathol. 176:744–753. 2010.
View Article : Google Scholar
|
|
23
|
Kuncewitch M, Yang WL, Molmenti E, et al:
Wnt agonist attenuates liver injury and improves survival after
hepatic ischemia/reperfusion. Shock. 39:3–10. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Funato Y, Michiue T, Asashima M, et al:
The thioredoxin-related redox-regulating protein nucleoredoxin
inhibits Wnt-beta-catenin signaling through dishevelled. Nat Cell
Biol. 8:501–508. 2006. View
Article : Google Scholar : PubMed/NCBI
|
|
25
|
Essers MA, de Vries-Smits LM, Barker N, et
al: Functional interaction between beta-catenin and FOXO in
oxidative stress signaling. Science. 308:1181–1184. 2005.
View Article : Google Scholar
|
|
26
|
Goode HF, Webster NR, Howdle PD, et al:
Reperfusion injury, antioxidants and hemodynamics during orthotopic
liver transplantation. Hepatology. 19:354–360. 1994. View Article : Google Scholar : PubMed/NCBI
|