Introduction
Preeclampsia (PE) is a pregnancy-specific syndrome
associated with hypertension and proteinuria or thrombocytopenia,
renal insufficiency, impaired liver function, pulmonary oedema,
cerebral symptoms, and visual symptoms (1). PE affects 2–5% of pregnancies worldwide
(2–4). It
can lead to severe maternal and perinatal morbidity, including
uterine growth restriction and prematurity. PE is responsible for
an elevated perinatal mortality rate and causes 10–15% of maternal
deaths (3,5).
The placenta plays a key role in the initiation and
progression of the disorders caused by PE (6). As commonly described, PE has a combined
genetic, immune, and angiogenic aetiology. The origin of PE seems
to be the impaired invasion of maternal spiral arteries by
trophoblast cells in the context of local abnormal immune
interactions between the fetoplacental unit and mother (7–9). Placental
underperfusion induces a chronic hypoxic state (10). Combined with the reoxygenation that
occurs, it creates increased local oxidative stress, resulting in
apoptosis and necrosis of the placenta. Placental pro-inflammatory
and antiangiogenic mediators and apoptotic bodies, released in the
maternal circulation, cause maternal systemic endothelial cell
dysfunction and systemic inflammation (5,11). Although
several hypotheses have been suggested to explain this vascular,
multi-systemic pregnancy-related disease, its complete pathogenesis
remains poorly understood (12,13), and PE
prevention, diagnosis, and treatment remain an important
challenge.
MicroRNAs (miRNAs or miRs) are small non-coding RNAs
(20–24 nucleotides) that regulate gene expression through
post-transcriptional repression or degradation of messenger RNA
(14,15). miRNAs are present in animals and plants
and have been detected in several human fluids (16). They are critical in many biological
processes, including the regulation of cell differentiation,
proliferation, apoptosis, angiogenesis, and metabolism (17). Specific plasma-related miRNAs were
identified in maternal plasma or serum in normal pregnancies, as
well as in pathological pregnancy conditions, such as PE (18,19). Several
recent reports described the significant dysregulation of specific
miRNA expression in the maternal circulation of PE patients
compared with controls (miR-24, miR-26a, miR-29a, miR-103,
miR-130b, miR-141, miR-144, miR-152, miR-181a, miR-210, miR-342-3p,
miR-520, miR-574-5p, and miR-1233) (20–23).
We hypothesized that the expression levels of
specific miRNAs in maternal blood could be dysregulated before the
onset of PE and be used to enhance screening, diagnosis, or
prognosis. We aimed to analyse, in a case-control study, several
miRNAs that were previously described as differentially expressed
in PE.
Materials and methods
miRNA selection
After performing a review on PubMed until 26
February, 2015, using the key words, ‘miRNA, pregnancies,
preeclampsia, placenta, circulating’, and consulting the miRNA
database, 17 miRNAs were selected (Table
I).
 | Table I.Primers used in quantitative PCR. |
Table I.
Primers used in quantitative PCR.
| miRNA | miRBase | Reference
Qiagen | Sequence of primer
(5′-3′) |
|---|
| hsa-miR-144-3p | MIMAT0000436 | MS00020328 |
TACAGTATAGATGATGTACT |
| hsa-miR-29a-3p | MIMAT0000086 | MS00003262 |
TAGCACCATCTGAAATCGGTTA |
| hsa-miR-210-3p | MIMAT0000267 | MS00003801 |
CTGTGCGTGTGACAGCGGCTGA |
| hsa-miR-210-5p | MIMAT0026475 | MS00045836 |
AGCCCCTGCCCACCGCACACTG |
|
hsa-miR-1233-3p | MIMAT0005588 | MS00008512 |
TGAGCCCTGTCCTCCCGCAG |
|
hsa-miR-1233-5p | MIMAT0022943 | MS00045213 |
AGTGGGAGGCCAGGGCACGGCA |
| hsa-miR-24-3p | MIMAT0000080 | MS00006552 |
TGGCTCAGTTCAGCAGGAACAG |
| hsa-miR-26a-5p | MIMAT0000082 | MS00029239 |
TTCAAGTAATCCAGGATAGGCT |
|
hsa-miR-130b-3p | MIMAT0000691 | MS00003451 |
CAGTGCAATGATGAAAGGGCAT |
|
hsa-miR-130b-5p | MIMAT0004680 | MS00008610 |
ACTCTTTCCCTGTTGCACTAC |
|
hsa-miR-181a-5p | MIMAT0000256 | MS00008827 |
AACATTCAACGCTGTCGGTGAGT |
|
hsa-miR-181a-3p | MIMAT0000270 | MS00006692 |
ACCATCGACCGTTGATTGTACC |
| hsa-miR-342-3p | MIMAT0000753 | MS00004011 |
TCTCACACAGAAATCGCACCCGT |
| hsa-miR-574-5p | MIMAT0004795 | MS00043617 |
TGAGTGTGTGTGTGTGAGTGTGT |
|
hsa-miR-16-2-3p | MIMAT0004518 | MS00008813 |
CCAATATTACTGTGCTGCTTTA |
| hsa-miR-124-3p | MIMAT0000422 | MS00006622 |
TAAGGCACGCGGTGAATGCC |
| hsa-miR-155-5p | MIMAT0000646 | MS00031486 |
TTAATGCTAATCGTGATAGGGGT |
| c-miR-39 | MIMAT0000010 | MS00019789 |
TCACCGGGTGTAAATCAGCTTG |
| RNU6-2 |
| MS00033740 |
|
Study population
In this retrospective study, 67 pregnant women, aged
19–44 years, with a gestational age of 24–36 weeks and 6 days of
amenorrhea, were selected among a prospective cohort of pregnant
women presenting, at 24 to <37 weeks' gestation, clinical
suspicion of, but not manifesting preeclampsia/eclampsia/HELLP
syndrome. Suspicion of PE was assessed on the basis of the
following criteria: New elevation of blood pressure (<140/90
mmHg), with or without pre-existing essential hypertension; de
novo or major proteinuria (<30 mg/dl or <2+ on a urine
dipstick); and clinical (epigastric pain, headache, visual
disturbances, and excessive weight gain), biological
(thrombocytopenia or elevation of transaminases), and ultrasonic
(intrauterine growth restriction, elevation of the uterine artery
pulsatility index, or uterine artery notch) characteristics
favouring PE. Manifestation of PE at selection was an exclusion
criterion.
In each patient presenting with the aforementioned
signs and symptoms who agreed to participate, blood was collected
and further pregnancy follow-up was performed. Retrospectively, the
PE and control cohorts were defined based on the diagnosis of PE at
delivery.
The present study was approved by the Ethics
Committee of the CHR Citadelle Hospital, Liège, Belgium, and
informed consent was obtained from all the patients.
Sample collection
Blood samples were immediately centrifuged at 1,000
× g for 15 min, and sediment-free serum samples were collected. The
serum aliquots were frozen at −80°C until further analysis and were
thawed only once thereafter.
miRNA extraction
Total RNA, including miRNA, was extracted from 200
µl of serum using the miRNeasy Serum/Plasma kit (Qiagen; Hilden,
Germany) according to the manufacturer's instructions, and it was
then eluted in 30 µl of nuclease-free water. A synthetic spike-in
control miRNA (C. elegans miR-39 mimic, Qiagen) was added
for subsequent normalisation.
Quantitative polymerase chain reaction
(qPCR) for miRNAs
Total miRNA (2 µl) from each sample was
reverse-transcribed with the miScript II TR kit (Qiagen) according
to the manufacturer's instructions. The miRNAs were subsequently
quantified using the miScript SYBR-Green PCR kit (Qiagen) and
specific forward primers. The reaction mixture included 2.5 µl of
cDNA, 12.5 µl of QuantiTect SYBR-Green PCR Master Mix (Qiagen), 2.5
µl of forward primer, 2.5 µl of miScript Universal Primer (Qiagen),
and 5 µl of RNase-free water for a final reaction volume of 25 µl.
The thermal cycling consisted of an initial denaturation at 95°C
for 15 min, followed by 45 cycles at 95°C for 15 sec, 55°C for 30
sec, and 70°C for 30 sec.
The reactions were run in duplicate. Threshold cycle
(Cq) and melting curves were acquired using the quantification and
melting curve programs of the LightCycler® 96 Real-Time
System (Roche Diagnostics GmbH, Mannheim, Germany). U6 small
nuclear RNA (RNU6) and c-miR-39 were used to determine relative
miRNA expression with the 2-ΔCq method (24–26). The
miRNA-specific primer sequences are listed in Table I.
Statistical analysis
Quantitative parameters are presented as the means ±
standard errors or medians. The statistical significance of
differences in the expression levels of serum miRNAs between PE
patients and controls was determined by the non-parametric
Mann-Whitney U-Wilcoxon test. To determine the diagnostic accuracy
of the miRNA expression levels, we generated receiver operating
characteristic (ROC) curves and calculated the area under the ROC
curves (AUC) (27). An evaluation of
the diagnostic power of multiple combinations of the miRNA serum
levels was performed using a logistic regression model. For all the
statistical analyses, we used the statistics toolbox of Matlab
R2024a software (MathWorks Inc., Natick, MA, USA). P<0.05 was
considered to indicate a statistically significant difference.
Results
Clinical characteristics
Table II shows the
main features of the patients in each group. The median of
gestational ages at inclusion (min-max) of the pregnant women were
32.1 (25.3–36.6) (PE patients) and 31.1 (24.3–36.5) weeks
(controls). There were no significant differences between the
subjects and controls with respect to gestational age, maternal
age, body mass index, smoking status, parity, gestity, ethnicity,
personal and family history of PE, previous hypertension,
proteinuria, and mean uterine artery pulsatility index. The median
of gestational ages (min-max) at delivery were 36.4 (30.0–39.3) (PE
patients) and 39.1 (35.2–41.3) weeks (controls) (P<0.0001).
 | Table II.Demographic and clinical
characteristics of controls and preeclamptic (PE) pregnancies. |
Table II.
Demographic and clinical
characteristics of controls and preeclamptic (PE) pregnancies.
|
Characteristics | Controls
(n=44) | PE (n=23) | P-value |
|---|
| Maternal age
(years) | 30 (19–38) | 29 (19–44) | 0.82701 |
| Gestational age at
inclusion (weeks) | 31.1
(24.3–36.5) | 32.1
(25.3–36.6) | 0.51313 |
| Gestational age at
delivery (weeks) | 39.1
(35.2–41.3) | 36.4
(30.0–39.3) | <0.0001 |
| Body mass
index | 27.2
(16.1–39.30) | 27.40
(19–41.5) | 0.85331 |
| Gestity | 2 (1–6) | 2 (1–7) | 0.19814 |
| Parity | 1 (0–5) | 0 (0–3) | 0.13570 |
| Smoking status |
|
|
|
|
Previous smokers | 6 (13.6%) | 3 (13%) | 0.66976 |
|
Smokers | 4 (9%) | 3 (13%) |
|
| Previous HTA | 3 (6.8%) | 2 (8.7%) | 0.79403 |
| Family history of
PE | 7 (16%) | 6 (26%) | 0.31431 |
| Proteinuria | 36 (81.8%) | 19 (82.6%) | 0.68365 |
| Mean artery
pulsatility index | 0.77
(0.36–1.50) | 0.86
(0.37–1.88) | 0.27001 |
| Systolic blood
pressure (mmHg) | 129 (105–160) | 134 (120–159) | 0.01763 |
| Diastolic blood
pressure (mmHg) | 80 (60–100) | 85 (70–100) | 0.01551 |
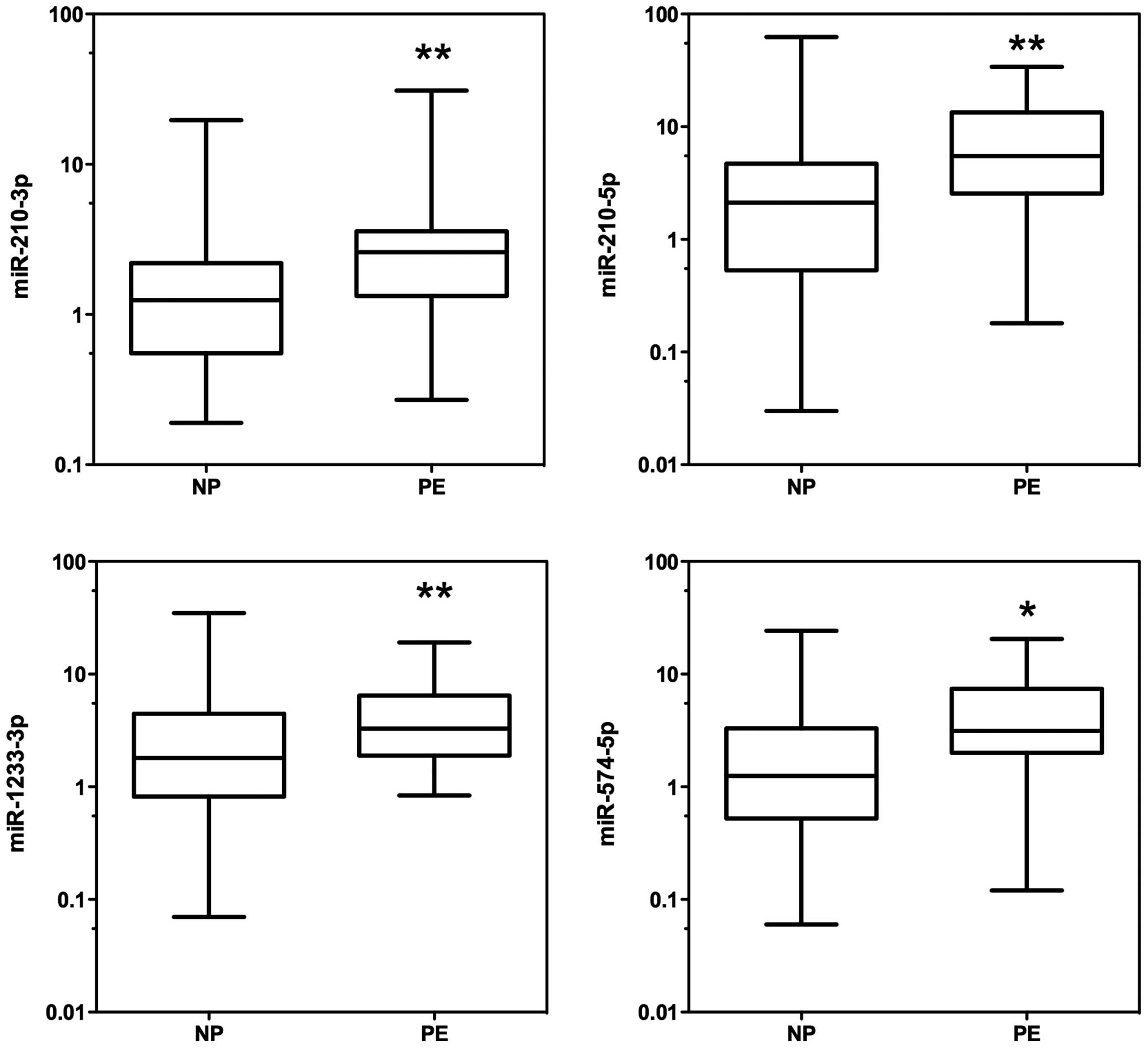
Differential expression of circulating
miRNAs
The expression levels of the 17 miRNAs (miR-16-2-3p,
miR-24-3p, miR-26a-5p, miR-29a-3p, miR-124-3p, miR-130b-5p
miR-130b-3p, miR-144-3p, miR-155-5p, miR-181a-3p, miR-181a-5p,
miR-210-3p, miR-210-5p, miR-342-3p, miR-574-5p, miR-1233-3p, and
miR-1233-5p) from the serum samples in the two groups (PE patients
and controls) were analysed with reverse transcription quantitative
polymerase chain reaction (RT-qPCR). According to RT-qPCR analysis,
there was a significant upregulation of 4 miRNAs: miR-210-3p,
miR-210-5p, miR-1233-3p, and miR-574-5p, in the serum of PE
patients compared with controls (P<0.05) (Table III, Fig.
1).
 | Table III.Circulating miRNA expression levels
in controls and preeclamptic pregnancies. |
Table III.
Circulating miRNA expression levels
in controls and preeclamptic pregnancies.
| miRNA | Controls
(n=44) | PE (n=23) | P-value
(Wilcoxon) |
|---|
| miR-210-3p | 2.25±0.51 | 4.10±1.30 | 0.005 |
| miR-210-5p | 5.46±1.78 | 9.18±2.00 | 0.006 |
| miR-1233-3p | 3.73±0.96 | 4.97±0.98 | 0.021 |
| miR-574-5p | 2.47±0.59 | 5.84±1.30 | 0.005 |
| miR-144-3p | 2.47±0.49 | 3.56±1.05 | 0.187 |
| miR-29a-3p | 2.84±0.46 | 2.85±0.30 | 0.129 |
| miR-1233-5p | 3.23±0.86 | 2.91±0.42 | 0.129 |
| miR-24-1-3p | 2.99±0.46 | 3.15±0.35 | 0.088 |
| miR-26a-5p | 2.63±0.36 | 2.41±0.33 | 0.736 |
| miR-130b-3p | 3.55±0.69 | 3.22±0.40 | 0.352 |
| miR-130b-5p1 | 4.39±0.87 | 4.92±0.92 | 0.113 |
| miR-181a-5p | 2.04±0.27 | 2.27±0.32 | 0.222 |
| miR-181a-3p | 2.63±1.17 | 2.28±0.61 | 0.113 |
| miR-342-3p | 3.06±0.39 | 3.18±0.34 | 0.282 |
| miR-16-2-3p | 2.14±0.36 | 3.27±0.90 | 0.124 |
| miR-124-3p | 3.51±0.72 | 2.97±0.35 | 0.362 |
| miR-155-5p | 3.58±0.62 | 3.76±0.65 | 0.402 |
Assessment of the screening value of
circulating miRNAs in PE
We constructed and examined the ROC curves of the 4
miRNAs that were upregulated in PE serum to evaluate their
potential utility as biomarkers (Fig.
2). The AUCs of miR-210-3p, miR-210-5p, miR-1233-3p, and
miR-574-5p were 0.7090 [95% confidence interval (CI), 0.582–0.836],
0.7040 (95% CI, 0.568–0.840), 0.673 (95% CI, 0.543–0.803), and
0.710 (95% CI, 0.578–0.842), respectively (Table IV). To improve the diagnostic power of
the miRNA expression levels, we applied a logistic regression model
to the data from PE patients and controls. Different combinations
were added to the model, and a maximum AUC of 0.7223 was found for
miR-210-5p and miR-574-5p (Fig. 3).
The fitted logistic regression model is as follows:
 | Table IV.ROC results for several miRs. |
Table IV.
ROC results for several miRs.
| miRs | Area under the ROC
curve (SE) | 95% CI | P-value |
|---|
| miR-210-3p | 0.7090
(0.06496) | 0.5816–0.8363 | 0.005 |
| miR-210-5p | 0.7041
(0.06918) | 0.5684–0.8397 | 0.006 |
| miR-1233-3p | 0.6729
(0.06632) | 0.5429–0.8029 | 0.021 |
| miR-574-5p | 0.7100
(0.06717) | 0.5783–0.8417 | 0.005 |
logitP(Y=1)1–P(Y=1)=–1.3036+0.05773*miR210–5p+0.1279*miR574–5p
where P(Y=1) is the probability that the sample is a
preeclamptic sample.
Discussion
Recently, the aberrant expression of miRNAs has been
documented in different pregnancy-related conditions, such as PE,
ectopic pregnancy, gestational diabetes mellitus, small for
gestational age, recurrent pregnancy loss, and preterm delivery
(28). These findings may be useful to
improve our understanding of the underlying pathophysiology of
these conditions.
In the present study, we confirmed the differential
expression of several miRNAs that were identified in previous
studies (20–23). Of the 17 miRNAs selected, miR-210-3p,
miR-210-5p, miR-1233-3p, and miR-574-5p were upregulated in the
sera of women who later developed PE compared with the controls who
did not develop PE according to RT-qPCR. By performing logistic
regression analysis of the differentially expressed miRNAs, we
found that the combination of miR-210-5p and miR-574-5p had the
best diagnostic power with an AUC of 0.7223.
In our selection of miRNAs based on the data
published in previous studies, we found very little overlap between
the reported studies. This may be due to differences in the sample
collection (sera versus plasma) or methods used for the analyses
(RT-qPCR versus microarrays). Even results obtained from the same
platform using products from different companies may be responsible
for this low correlation of results (29,30). RT-qPCR
is often considered as the ‘gold standard’ for the detection and
quantification of gene expression. As a result, we chose to
validate previously identified miRNA results using this procedure.
However, one important step of RT-qPCR is normalisation of the
miRNA expression level. Using improper reference genes for
normalisation can result in evaluation bias during data analysis.
To the best of our knowledge, there has been no consensus regarding
a reliable housekeeping miRNA for analysing circulating miRNAs.
Therefore, it becomes difficult to directly compare the results
from different studies. In the present study, we used a double
normalisation procedure, including the use of the synthetic
c-miR-39 and RNU6B. The same amount of c-miR-39 was added to each
sample before the extraction procedure, and the c-miR-39 expression
level reflected differences at the same time in the extraction,
reverse transcription, and PCR amplification procedures (31). However, the use of RNU6B complements
technical bias with biological bias. Although RNU6B does not
necessarily represent the ‘best’ reference, it has been previously
used to analyse miRNAs in the sera of preeclamptic women (23,32).
The selection of the patients included in different
studies may also introduce some bias. To identify new biomarkers
for PE, a common strategy is to analyse a few samples or a pool of
samples when performing miRNA profiling. This step is further
followed by a validation procedure, frequently RT-qPCR, with
additional samples from PE cases and controls. Usually, the second
step does not completely validate the profiling step (18,20,21). Thus, in order to evaluate previously
differentially reported miRNAs in PE, we performed a case-control
study with 23 PE patients and 44 controls. The two groups were
found to be comparable with respect to their maternal age,
gestational age at inclusion, gestity, and parity. However, the
retrospective nature of the investigation was one limitation of the
study. A second limitation is that we were unable to separately
analyse early- and late-onset PE due to the small sample size.
There is currently no consensus regarding a set of
differentially expressed miRNAs in PE that may be used as
biomarkers. Our approach was to collect several potentially
interesting miRNAs that were previously described in the literature
and test them in our set of case-control samples.
Notably, miR-210, which is one of the more commonly
recurring miRNAs overexpressed in PE (22,32–36), was also elevated in our PE cohort. This
particular miR-210 has been identified as a hypoxia-induced miRNA
in many cell types and tissues and is consistently upregulated by
hypoxia in both physiological and malignant conditions (37,38). Several
target genes with roles in mitochondrial metabolism, angiogenesis,
and DNA repair have been identified, and most of them may be
involved in the pathogenesis of PE. However, it remains unclear
whether the differential expression of miR-210 is the consequence
or origin of PE even though this particular miRNA has been
described as a serum biomarker for PE (32).
There was also a higher level of circulating
miR-1233 in the group of women who developed PE compared with the
group of women with a normal pregnancy. Our results confirmed those
of Ura et al (23), who were
the first researchers to identify a potential role for miR-1233,
which has already been described in renal carcinoma, in predicting
PE. It is important to note that both miR-1233 and miR-210, which
are upregulated in PE, are also upregulated in renal cell
carcinoma. Of note, in patients with renal cell carcinoma, only
miR-1233 was found to be increased (39). Information on the function of miR-1233,
located on chromosome 15q14, is incomplete. Several potential
target genes have been predicted using TargetScan 6.0 (40), but they have not been validated. The
expression level of miR-574-5p was also elevated in the blood of
women with PE (21). However, the
expression of miR-574-5p has been poorly investigated.
Although there are many studies on PE screening, a
biologically predictive and prognostic test with high accuracy for
routine clinical use has yet to be identified (41–43). The
most promising strategies are multiparametric approaches that
include a combination of maternal factors, biophysical tests (mean
blood pressure, uterine artery Doppler), and biochemical markers
(44–50). Sequential multiparametric testing is
superior to screening in the first trimester alone (51). Nevertheless, a panel of tests is
necessary to effectively identify women early in pregnancy who are
at the highest risk for developing PE.
Although the prevalence of PE is relatively low and
miRNA analysis is technically challenging, further studies with
larger cohorts are mandatory. Discriminating between the different
phenotypes of PE is also important because they may involve
different sets of miRNA expression.
Furthermore, patients were sampled before the onset
of PE and delivery (mean:one month before). Indeed, cases were
enrolled when there was suspicion of PE, but manifest PE was an
exclusion criterion. This protocol may partially explain the reason
for only 4 of the 17 selected miRNAs being significantly
upregulated.
The fact that four circulating miRNAs (miR-210-3p,
miR-210-5p, miR-1233-3p, and miR-574-5p) were differentially
expressed in the sera of women who later developed PE compared with
women who did not develop PE, confirms the possible
pathophysiological role of miRNAs in PE, as previously suggested
(19,52,53).
Particularly, exploring the role of miR-1233 and miR-574 in PE
could enrich our understanding of this disease.
Future research on the biological pathway of
circulating miRNAs may enhance our understanding of the
pathogenesis of PE and aid in the development of new biomarkers for
clinical application. Using these miRNAs in a multiparametric test
may also provide a new clinical strategy for identifying women who
are at risk for developing PE.
Acknowledgements
The authors acknowledge Nathalie Lefin and Sophie
Kessler for their excellent technical assistance. C.M. is a
Research Associate from the Fonds de la Recherche Scientifique-FNRS
(F.R.S.-FNRS, Belgium). This study was supported by grants from the
Fonds de la Recherche Scientifique-FNRS (F.R.S.-FNRS, Belgium), the
Fonds spéciaux de la Recherche (University of Liège), the Fonds
Léon Fredericq (University of Liège), the Direction Générale
Opérationnelle de l'Economie, de l'Emploi et de la Recherche from
the S.P.W. (Région Wallonne, Belgium).
Glossary
Abbreviation
Abbreviations:
References
|
1
|
American College6 of Obstetricians and
Gynecologists, . Task Force on Hypertension in Pregnancy:
Hypertension in pregnancy. Report of the American College of
Obstetricians and Gynecologists' Task Force on Hypertension in
Pregnancy. Obstet Gynecol. 122:1122–1131. 2013.PubMed/NCBI
|
|
2
|
Redman CW and Sargent IL: Latest advances
in understanding preeclampsia. Science. 308:1592–1594. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Duley L: The global impact of
pre-eclampsia and eclampsia. Semin Perinatol. 33:130–137. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Report of the National High Blood Pressure
Education Program Working Group on High Blood Pressure in
Pregnancy. Am J Obstet Gynecol. 183:S1–S22. 2000. View Article : Google Scholar
|
|
5
|
Sibai B, Dekker G and Kupferminc M:
Pre-eclampsia. Lancet. 365:785–799. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Huppertz B: Placental origins of
preeclampsia: Challenging the current hypothesis. Hypertension.
51:970–975. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Foidart JM, Noël A, Chantraine F, Lorquet
S, Petit P, Munaut C, Berndt S, Pequeux C and Schaaps JP: Defective
placental implantation and its effects on maternal endothelial
function. Bull Acad Natl Med. 193:1059–1064; discussion 1064–1066,
1067–1068. 2009.(In French). PubMed/NCBI
|
|
8
|
Foidart JM, Schaaps JP, Chantraine F,
Munaut C and Lorquet S: Dysregulation of anti-angiogenic agents
(sFlt-1, PLGF, and sEndoglin) in preeclampsia-a step forward but
not the definitive answer. J Reprod Immunol. 82:106–111. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Redman CW, Sargent IL and Staff AC: IFPA
Senior Award Lecture: Making sense of pre-eclampsia - two placental
causes of preeclampsia? Placenta. 35:S20–S25. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Munaut C, Lorquet S, Pequeux C, Blacher S,
Berndt S, Frankenne F and Foidart JM: Hypoxia is responsible for
soluble vascular endothelial growth factor receptor-1 (VEGFR-1) but
not for soluble endoglin induction in villous trophoblast. Hum
Reprod. 23:1407–1415. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Roberts JM and Hubel CA: The two stage
model of preeclampsia: Variations on the theme. Placenta. 30:(Suppl
A). S32–S37. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Redman CW and Sargent IL: Immunology of
pre-eclampsia. Am J Reprod Immunol. 63:534–543. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Dechend R and Staff AC: Placenta messages
to the mother: Not just debris. Hypertension. 59:191–193. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Bartel DP: MicroRNAs: Target recognition
and regulatory functions. Cell. 136:215–233. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lai EC: Micro RNAs are complementary to 3
UTR sequence motifs that mediate negative post-transcriptional
regulation. Nat Genet. 30:363–364. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Weber JA, Baxter DH, Zhang S, Huang DY,
Huang KH, Lee MJ, Galas DJ and Wang K: The microRNA spectrum in 12
body fluids. Clin Chem. 56:1733–1741. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ong SG, Lee WH, Kodo K and Wu JC:
MicroRNA-mediated regulation of differentiation and
trans-differentiation in stem cells. Adv Drug Deliv Rev. 88:3–15.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Miura K, Miura S, Yamasaki K, Higashijima
A, Kinoshita A, Yoshiura K and Masuzaki H: Identification of
pregnancy-associated microRNAs in maternal plasma. Clin Chem.
56:1767–1771. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Tsochandaridis M, Nasca L, Toga C and
Levy-Mozziconacci A: Circulating microRNAs as clinical biomarkers
in the predictions of pregnancy complications. BioMed Res Int.
2015:2949542015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Li H, Ge Q, Guo L and Lu Z: Maternal
plasma miRNAs expression in preeclamptic pregnancies. Biomed Res
Int. 2013:9702652013.PubMed/NCBI
|
|
21
|
Wu L, Zhou H, Lin H, Qi J, Zhu C, Gao Z
and Wang H: Circulating microRNAs are elevated in plasma from
severe preeclamptic pregnancies. Reproduction. 143:389–397. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Gunel T, Zeybek YG, Akçakaya P, Kalelioğlu
I, Benian A, Ermis H and Aydınlı K: Serum microRNA expression in
pregnancies with preeclampsia. Genet Mol Res. 10:4034–4040. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Ura B, Feriotto G, Monasta L, Bilel S,
Zweyer M and Celeghini C: Potential role of circulating microRNAs
as early markers of preeclampsia. Taiwan J Obstet Gynecol.
53:232–234. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Zhang Y, Jia Y, Zheng R, Guo Y, Wang Y,
Guo H, Fei M and Sun S: Plasma microRNA-122 as a biomarker for
viral-, alcohol-, and chemical-related hepatic diseases. Clin Chem.
56:1830–1838. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(−Delta Delta C(T)) Method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Kok MG, Halliani A, Moerland PD, Meijers
JC, Creemers EE and Pinto-Sietsma SJ: Normalization panels for the
reliable quantification of circulating microRNAs by RT-qPCR. FASEB
J. 29:3853–3862. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Hanley JA and McNeil BJ: The meaning and
use of the area under a receiver operating characteristic (ROC)
curve. Radiology. 143:29–36. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Zhao Z, Moley KH and Gronowski AM:
Diagnostic potential for miRNAs as biomarkers for
pregnancy-specific diseases. Clin Biochem. 46:953–960. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Chen Y, Gelfond JA, McManus LM and
Shireman PK: Reproducibility of quantitative RT-PCR array in miRNA
expression profiling and comparison with microarray analysis. BMC
Genomics. 10:4072009. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Sato F, Tsuchiya S, Terasawa K and
Tsujimoto G: Intra-platform repeatability and inter-platform
comparability of microRNA microarray technology. PLoS One.
4:e55402009. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Roberts TC, Coenen-Stass AML and Wood MJA:
Assessment of RT-qPCR normalization strategies for accurate
quantification of extracellular microRNAs in murine serum. PLoS
One. 9:e892372014. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Anton L, Olarerin-George AO, Schwartz N,
Srinivas S, Bastek J, Hogenesch JB and Elovitz MA: miR-210 inhibits
trophoblast invasion and is a serum biomarker for preeclampsia. Am
J Pathol. 183:1437–1445. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Pineles BL, Romero R, Montenegro D, Tarca
AL, Han YM, Kim YM, Draghici S, Espinoza J, Kusanovic JP, Mittal P,
et al: Distinct subsets of microRNAs are expressed differentially
in the human placentas of patients with preeclampsia. Am J Obstet
Gynecol. 196:261.e1–261.e6. 2007. View Article : Google Scholar
|
|
34
|
Enquobahrie DA, Abetew DF, Sorensen TK,
Willoughby D, Chidambaram K and Williams MA: Placental microRNA
expression in pregnancies complicated by preeclampsia. Am J Obstet
Gynecol. 204:178.e12–178.e21. 2011. View Article : Google Scholar
|
|
35
|
Muralimanoharan S, Maloyan A, Mele J, Guo
C, Myatt LG and Myatt L: miR-210 modulates mitochondrial
respiration in placenta with preeclampsia. Placenta. 33:816–823.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Zhang Y, Fei M, Xue G, Zhou Q, Jia Y, Li
L, Xin H and Sun S: Elevated levels of hypoxia-inducible
microRNA-210 in pre-eclampsia: New insights into molecular
mechanisms for the disease. J Cell Mol Med. 16:249–259. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Camps C, Buffa FM, Colella S, Moore J,
Sotiriou C, Sheldon H, Harris AL, Gleadle JM and Ragoussis J:
hsa-miR-210 Is induced by hypoxia and is an independent prognostic
factor in breast cancer. Clin Cancer Res. 14:1340–1348. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Fasanaro P, D'Alessandra Y, Di Stefano V,
Melchionna R, Romani S, Pompilio G, Capogrossi MC and Martelli F:
MicroRNA-210 modulates endothelial cell response to hypoxia and
inhibits the receptor tyrosine kinase ligand Ephrin-A3. J Biol
Chem. 283:15878–15883. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Wulfken LM, Moritz R, Ohlmann C,
Holdenrieder S, Jung V, Becker F, Herrmann E, Walgenbach-Brünagel
G, von Ruecker A, Müller SC, et al: MicroRNAs in renal cell
carcinoma: Diagnostic implications of serum miR-1233 levels. PLoS
One. 6:e257872011. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Lewis BP, Shih IH, Jones-Rhoades MW,
Bartel DP and Burge CB: Prediction of mammalian microRNA targets.
Cell. 115:787–798. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Grill S, Rusterholz C, Zanetti-Dällenbach
R, Tercanli S, Holzgreve W, Hahn S and Lapaire O: Potential markers
of preeclampsia-a review. Reprod Biol Endocrinol. 7:702009.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Meads CA, Cnossen JS, Meher S,
Juarez-Garcia A, ter Riet G, Duley L, Roberts TE, Mol BW, van der
Post JA, Leeflang MM, et al: Methods of prediction and prevention
of pre-eclampsia: systematic reviews of accuracy and effectiveness
literature with economic modelling. Health Technol Assess.
12:1–270. 2008. View Article : Google Scholar
|
|
43
|
Zakiyah N, Postma MJ, Baker PN and van
Asselt AD: IMPROvED Consortium: Pre-eclampsia diagnosis and
treatment options: A review of published economic assessments.
Pharmacoeconomics. 33:1069–1082. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Poon LC, Stratieva V, Piras S, Piri S and
Nicolaides KH: Hypertensive disorders in pregnancy: Combined
screening by uterine artery Doppler, blood pressure and serum
PAPP-A at 11–13 weeks. Prenat Diagn. 30:216–223. 2010.PubMed/NCBI
|
|
45
|
Poon LC, Maiz N, Valencia C, Plasencia W
and Nicolaides KH: First-trimester maternal serum
pregnancy-associated plasma protein-A and pre-eclampsia. Ultrasound
Obstet Gynecol. 33:23–33. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Scazzocchio E, Figueras F, Crispi F, Meler
E, Masoller N, Mula R and Gratacos E: Performance of a
first-trimester screening of preeclampsia in a routine care
low-risk setting. Am J Obstet Gynecol. 208:203.e1–203.e10. 2013.
View Article : Google Scholar
|
|
47
|
Park FJ, Leung CH, Poon LC, Williams PF,
Rothwell SJ and Hyett JA: Clinical evaluation of a first trimester
algorithm predicting the risk of hypertensive disease of pregnancy.
Aust N Z J Obstet Gynaecol. 53:532–539. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Akolekar R, Syngelaki A, Poon L, Wright D
and Nicolaides KH: Competing risks model in early screening for
preeclampsia by biophysical and biochemical markers. Fetal Diagn
Ther. 33:8–15. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Akolekar R, Syngelaki A, Sarquis R, Zvanca
M and Nicolaides KH: Prediction of early, intermediate and late
pre-eclampsia from maternal factors, biophysical and biochemical
markers at 11–13 weeks. Prenat Diagn. 31:66–74. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Foidart JM, Munaut C, Chantraine F,
Akolekar R and Nicolaides KH: Maternal plasma soluble endoglin at
11–13 weeks' gestation in pre-eclampsia. Ultrasound Obstet Gynecol.
35:680–687. 2010.PubMed/NCBI
|
|
51
|
Kusanovic JP, Romero R, Chaiworapongsa T,
Erez O, Mittal P, Vaisbuch E, Mazaki-Tovi S, Gotsch F, Edwin SS,
Gomez R, et al: A prospective cohort study of the value of maternal
plasma concentrations of angiogenic and anti-angiogenic factors in
early pregnancy and midtrimester in the identification of patients
destined to develop preeclampsia. J Matern Fetal Neonatal Med.
22:1021–1038. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Lycoudi A, Mavreli D, Mavrou A,
Papantoniou N and Kolialexi A: miRNAs in pregnancy-related
complications. Expert Rev Mol Diagn. 15:999–1010. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Morales Prieto DM and Markert UR:
MicroRNAs in pregnancy. J Reprod Immunol. 88:106–111. 2011.
View Article : Google Scholar : PubMed/NCBI
|