Introduction
Creatine kinase (CK) is an enzyme which catalyzes
the reaction of creatine and adenosine triphosphate to create
phosphocreatine and adenosine diphosphate. The three isoenzymes
involved are CK-MM, which is mainly present in skeletal muscle;
CK-MB in cardiac muscle and CK-BB which is predominantly expressed
in the brain. The sum of these three isoenzymes quantifies the
total serum CK (sCK) levels (1,2). CK levels
have been reported based on age, ethnicity and gender and can be
stratified in a ‘high CK’ group among men of African descent with a
mean CK value of 237.8 U/l, an ‘intermediate CK’ group comprising
of non-African-American men and women with mean CK levels between
109.3 and 149.7 U/l and a ‘low CK’ group consisting of Caucasian
women with mean CK levels between 64.6 and 79.8 U/l (3). Recent European Federation of Neurological
Society (EFNS) guidelines recommended that hyperCKemia should be
redefined as sCK >1.5 fold the upper limit of normal (4), according to a 97.5% threshold and normal
values introduced by Brewster et al (5) for both genders of African and Caucasian
descent.
CK measurement represents a usual laboratory
parameter as a part of routine follow-up in the daily practice or
to assess patients complaining of muscle-related symptoms. sCK
(phospho) level elevation sometimes represents an incidental
laboratory finding leading to a diagnostic enigma as it can be
related to a variety of disorders such as those of neuromuscular,
cardiac, metabolic, endocrine and traumatic origin (2,4,6). Other clinical situations that can lead to
hyperCKemia include viral infections, toxin accumulation, heavy
muscle exercise, surgery, pregnancy, obstructive sleep apnoea,
neuroacanthocytosis syndromes, macro-CK, malignant hyperthermia
syndrome and medications (4,6). However, elevated CK levels may be
observed rarely among asymptomatic individuals.
We present a case of asymptomatic idiopathic
hyperCKemia with such extremely high levels of CK as to be of the
very few internationally reported and, to the best of our
knowledge, the first case reported from a rural primary care
setting in Greece. Thus, we carried out a literature overview by
discussing this condition.
Case presentation
Informed consent was obtained from the patient for
publication of this case report. A Caucasian 61-year-old woman with
a previous history of arterial hypertension, diabetes mellitus and
hyperlipidemia diagnosed 5 years ago and a transient ischemic
attack at the age of 57, presented as completely asymptomatic to
her general practitioner for a routine follow-up. She was under
treatment with olmesartan/amlodipine (20+5 mg),
vildagliptin/metformin (50+850 mg), atorvastatin 40 mg and aspirin
100 mg. Previous sCK levels after being started on statin were all
within normal ranges. Routine serum chemistry revealed an elevated
CK level at 6,122 IU/l [normal CK values of the manufacturer of the
CK assay (HITACHI-ROCHE, COBAS 6000; Roche Diagnostics GmbH,
Manheim, Germany) was <167 IU/l) without CK-MB fraction
elevation. Levels of SGOT 135 IU/l, SGPT 199 IU/l and HGB 10.9 g/dl
were detected (Table I). Electrolytes
and kidney function parameters were all within normal ranges. No
myalgias, cramps, fatigue or other neurological symptoms were
described, while family history was negative for any neuromuscular
disease and non-informative for any sCK elevations. Physical
examination including neurologic evaluation, showed no evidence of
neuropathy while vital signs measures and ECG findings were all
normal. Further laboratory investigations including thyroid and
parathyroid hormone levels, abdominal ultrasonography, computed
tomography of the thorax and abdomen revealed no pathological
findings. Electromyogram of left and right tibialis anterior and
gastrocnemius muscles was negative for any type of myopathy. Muscle
biopsy did not reveal any significant alterations. Striated muscle
fibers with normal size and without hypertrophy, atrophy, necrosis,
inflammation or malignant lesions of neoplasia were identified
microscopically. Discontinuation of statin therapy and abstinence
from any physical exercise were strongly suggested for a 7-day
period of observation (4). After a
period of 2 years the patient remains asymptomatic but sCK levels
remain elevated, ranging between 180 and 2,372 U/l with sporadic
peaks rising to 6,591 IU/l (>50-fold higher than normal values)
and without any obvious reason for such laboratory deviations.
 | Table I.Biochemical result analysis (May
2014). |
Table I.
Biochemical result analysis (May
2014).
| Laboratory
parameters | Results | Normal ranges |
|---|
| Glucose | 122 mg/dl |
65–115 |
| Urea | 35.5 mg/dl | 10.0–50.0 |
| Uric acid | 3.2 mg/dl | <5.7 |
| Creatinine | 0.44 mg/dl | 0.50–1.00 |
| Total
cholesterol | 192 mg/dl |
70–200 |
| Triglycerides | 104 mg/dl |
<200 |
| HDL cholesterol | 56 mg/dl | >35 |
| Serum glutamic
oxaloacetic transaminase | 135.0 U/l | <31 |
| Serum glutamic
pyruvic transaminase | 198.9 U/l | <31 |
| Creatine
phosphokinase | 6,122 U/l |
<142 |
| Potassium (K) | 4.1 mmol/l | 3.5–5.1 |
| Sodium (Na) | 142.7 mmol/l | 136.0–145.0 |
Discussion
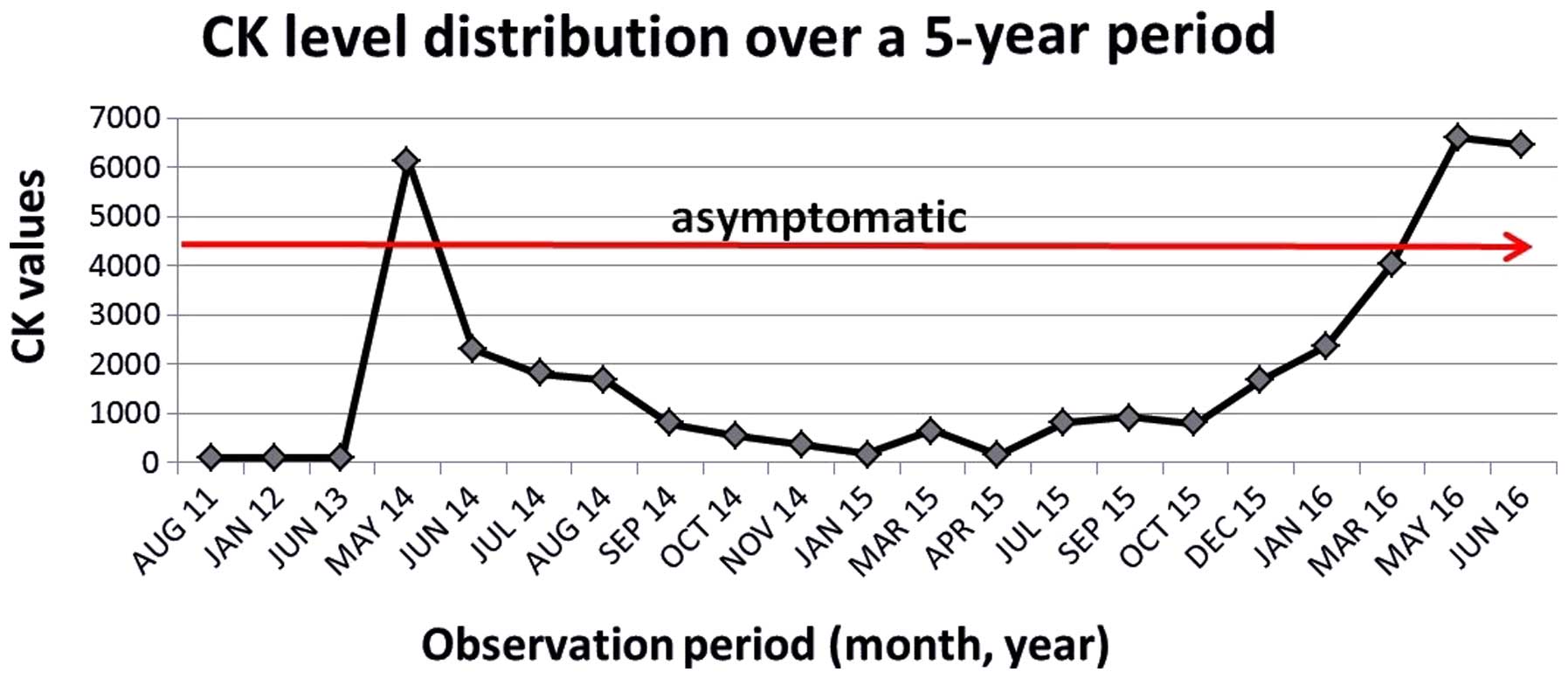
The currently reported case, after 2 years of
patient follow-up, shows that extremely abnormal CK levels are not
necessarily associated with neuromuscular exhaustion and physical
demolition. This finding of CK elevation was noted and repeatedly
confirmed in routine blood check procedures (Fig. 1) with a patient being active and
self-describing a ‘healthy’ overall condition. Additionally, it was
shown that there was a total divergence between laboratory levels,
medication intake and biopsy findings. The most negative effect of
CK abnormality was related to the great stress provoked on both
patient and physician by an extremely abnormal laboratory result.
Discontinuation of statin therapy was assessed to be risky due to a
previous cardiovascular event that occurred in our patient. As
there are reports suggesting that this condition is
under-recognized by primary care physicians (7), it is crucial to identify case-finding
approaches to better detect and report similar cases for primary
care settings.
The term ‘idiopathic hyperCKemia’ was first
introduced by Rowland et al, defining an uncommon condition
characterized by persistent elevation of the serum concentration of
CK without any clinical, neurophysiological or histopathological
evidence of neuromuscular disease, using the available laboratory
procedures (8). In a number of cases
this benign condition could be inherited as an autosomal dominant
trait, known as Familial Idiopathic HyperCKemia (9).
Brewster and de Visser (10) added criteria for exclusion such as
hypothyroidism, medication side effects and family history of
neuromuscular disorder, while Prelle et al suggested that a
non-diagnostic muscle biopsy is required for a real case of
idiopathic hyperCKemia (6). Despite
the fact that in some cases CPK concentration levels may be
extremely high, long-term follow-up has no clinical impact since
the prognosis of this condition is benign (11,12). A
follow-up study identified persistent hyperCKemia in 78% of
asymptomatic patients after a 6-year period as well as an
association between CK normalization and a normal muscle biopsy in
22% (12).
Some researchers have correlated the high level of
hyperCKemia (CK levels >5- to 10-fold normal) and early age with
an increased possibility to reach a specific diagnosis after a
muscle biopsy (6,13). In our case, despite the extremely high
levels of CK, after all the recommended diagnostic procedures, a
specific diagnosis was not established. According to Dabby et
al, even though muscle biopsy is often non-normal in patients
with persistent hyperCKemia, the majority of the abnormalities are
non-specific, rendering the confirmation of a definite diagnosis
relatively low (14). On the other
hand, based on a diagnostic approach to pauci- or asymptomatic
hyperCKemia guidelines, a normal electromyogram increases the
probability of a normal biopsy to ≤74–80% (4,6,15).
Weglinski et al associated malignant
hyperthermia susceptibility, an autosomal dominant disease, to
almost half of patients with idiopathic hyperCKemia and suggested
that caffeine-halothane contracture testing be used in patients
with persistent elevated CK levels who undergo a muscle biopsy
procedure (16). Another important
cause of increased CK levels is Duchenne dystrophy (17). Guidelines suggest DNA analysis for
Duchenne/Becker mutation in case of women of <3-fold CK
elevation to exclude a carrier status (4). However, our patient had a 50-fold CK
level elevation. Her son and daughter, adults of late thirties, are
healthy without any sign of neuromuscular disorder. No family
history of similar laboratory findings was reported.
Another cause of idiopathic hyperCKemia may be the
caveolin-3 gene mutations. Three elements of the Caveolin gene
family have been recognized, Cav-1, Cav-2 and
Cav-3 (18). The latter one,
Cav-3, is expressed mainly in muscle cells such as smooth,
skeletal and cardiac cells (19).
Cav-3 gene deficiency leads to four skeletal muscle
phenotypes, including the isolated hyperCKemia (20). Persistent isolated sporadic hyperCKemia
was the only manifestation in two children with a novel sporadic
Cav-3 p.R26Q mutant (21,22). Additionally, in a case of familial
hyperCKemia the Cav-3p. P28L substitution was identified (23).
Even though genetic testing was strongly suggested
to our patient and her family members, mainly for research reasons,
the patient refused to undergo any other type of examination, based
on her asymptomatic clinical situation and the negative family
history for any neuromuscular or other inherited disorder. The
patient remains under close follow-up.
References
|
1
|
Nanji AA: Serum creatine kinase
isoenzymes: A review. Muscle Nerve. 6:83–90. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Silvestri NJ and Wolfe GI:
Asymptomatic/pauci-symptomatic creatine kinase elevations
(hyperckemia). Muscle Nerve. 47:805–815. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wong ET, Cobb C, Umehara MK, Wolff GA,
Haywood LJ, Greenberg T and Shaw ST Jr: Heterogeneity of serum
creatine kinase activity among racial and gender groups of the
population. Am J Clin Pathol. 79:582–586. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kyriakides T, Angelini C, Schaefer J,
Sacconi S, Siciliano G, Vilchez JJ and Hilton-Jones D: European
Federation of Neurological Societies: EFNS guidelines on the
diagnostic approach to pauci- or asymptomatic hyperCKemia. Eur J
Neurol. 17:767–773. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Brewster LM, Mairuhu G, Sturk A and van
Montfrans GA: Distribution of creatine kinase in the general
population: Implications for statin therapy. Am Heart J.
154:655–661. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Prelle A, Tancredi L, Sciacco M, Chiveri
L, Comi GP, Battistel A, Bazzi P, Boneschi F Martinelli, Bagnardi
V, Ciscato P, et al: Retrospective study of a large population of
patients with asymptomatic or minimally symptomatic raised serum
creatine kinase levels. J Neurol. 249:305–311. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kaushik P and Gonuguntla A: Idiopathic
Benign Hyper-CK-Emia. Int J Biomed Sci. 5:79–80. 2009.PubMed/NCBI
|
|
8
|
Rowland LP, Willner J, DiMauro S and
Miranda A: Approaches to the membrane theory of Duchenne muscular
dystrophyMuscular dystrophy-advances and new trends. Angelini C,
Danieli GA and Fontarni D: Excerpta Medica; Amsterdam: pp. 3–13.
1980
|
|
9
|
Capasso M, De Angelis MV, Di Muzio A,
Scarciolla O, Pace M, Stuppia L, Comi GP and Uncini A: Familial
idiopathic hyper-CK-emia: An underrecognized condition. Muscle
Nerve. 33:760–765. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Brewster LM and de Visser M: Persistent
hyperCKemia: Fourteen patients studied in retrospect. Acta Neurol
Scand. 77:60–63. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Reijneveld JC, Notermans NC, Linssen WH
and Wokke JH: Benign prognosis in idiopathic hyper-CK-emia. Muscle
Nerve. 23:575–579. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
D'Adda E, Sciacco M, Fruguglietti ME,
Crugnola V, Lucchini V, Martinelli-Boneschi F, Zecca C, Lamperti C,
Comi GP, Bresolin N, et al: Follow-up of a large population of
asymptomatic/oligosymptomatic hyperckemic subjects. J Neurol.
253:1399–1403. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Fernandez C, de Paula AM,
Figarella-Branger D, Krahn M, Giorgi R, Chabrol B, Monfort MF,
Pouget J and Pellissier JF: Diagnostic evaluation of clinically
normal subjects with chronic hyperCKemia. Neurology. 66:1585–1587.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Dabby R, Sadeh M, Herman O, Berger E,
Watemberg N, Hayek S, Jossiphov J and Nevo Y: Asymptomatic or
minimally symptomatic hyperCKemia: Histopathologic correlates. Isr
Med Assoc J. 8:110–113. 2006.PubMed/NCBI
|
|
15
|
Joy JL and Oh SJ: Asymptomatic
hyper-CK-emia: An electrophysiologic and histopathologic study.
Muscle Nerve. 12:206–209. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Weglinski MR, Wedel DJ and Engel AG:
Malignant hyperthermia testing in patients with persistently
increased serum creatine kinase levels. Anesth Analg. 84:1038–1041.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Tachi N, Wakai S, Yutoh Y, Chiba S and
Miura J: Asymptomatic hyperCKemia: Detection of an isolated carrier
of Duchenne muscular dystrophy. J Child Neurol. 5:351–353. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Chen D and Che G: Value of caveolin-1 in
cancer progression and prognosis: Emphasis on cancer-associated
fibroblasts, human cancer cells and mechanism of caveolin-1
expression (Review). Oncol Lett. 8:1409–1421. 2014.PubMed/NCBI
|
|
19
|
Song KS, Scherer PE, Tang Z, Okamoto T, Li
S, Chafel M, Chu C, Kohtz DS and Lisanti MP: Expression of
caveolin-3 in skeletal, cardiac, and smooth muscle cells.
Caveolin-3 is a component of the sarcolemma and co-fractionates
with dystrophin and dystrophin-associated glycoproteins. J Biol
Chem. 271:15160–15165. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Gazzerro E, Sotgia F, Bruno C, Lisanti MP
and Minetti C: Caveolinopathies: From the biology of caveolin-3 to
human diseases. Eur J Hum Genet. 18:137–145. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Carbone I, Bruno C, Sotgia F, Bado M,
Broda P, Masetti E, Panella A, Zara F, Bricarelli FD, Cordone G, et
al: Mutation in the CAV3 gene causes partial caveolin-3 deficiency
and hyperCKemia. Neurology. 54:1373–1376. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Reijneveld JC, Ginjaar IB, Frankhuizen WS
and Notermans NC: CAV3 gene mutation analysis in patients with
idiopathic hyper-CK-emia. Muscle Nerve. 34:656–658. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Merlini L, Carbone I, Capanni C, Sabatelli
P, Tortorelli S, Sotgia F, Lisanti MP, Bruno C and Minetti C:
Familial isolated hyperCKaemia associated with a new mutation in
the caveolin-3 (CAV-3) gene. J Neurol Neurosurg Psychiatry.
73:65–67. 2002. View Article : Google Scholar : PubMed/NCBI
|