Introduction
Human inflammatory bowel diseases (IBD), ulcerative
colitis (UC) and Crohn's disease (CD) are a group of chronic
inflammatory conditions of the gastrointestinal tract (1). UC and CD are differentiated by the
location of inflammation in the digestive tract (2).
Incidence and prevalence of IBD in the Nordic
countries, North America and developing countries is steadily
increasing (3,4). New Zealand has the highest rates of IBD
in the world (5), and the exact rates
of IBD in Iran are not clear, but it appears that the frequency of
IBD is increasing (6,7). The exact causes of this disease remains
unknown, but studies have proposed that it may be the result of
complex interactions between multiple factors, such as genetic,
environmental and immunological factors (8,9). There is
direct evidence for the role of genetics in IBD, associated with
the family history of patients, as well as increased rates of IBD
in monozygotic twins (10,11). The predominant genetic association in
IBD is divided into genes that contribute to innate and adaptive
immune responses (12). Tumor necrosis
factor (TNF)-α is a multifunctional cytokine involved in the
advancement of inflammatory responses and is critical in the
pathogenesis of inflammatory, autoimmune and malignant diseases
(13). TNF-α is key in
cell-mediated immunity, as demonstrated by high serum levels of
TNF-α in IBD blood and tissue samples (14,15).
TNF-α has numerous polymorphisms, the majority of which are
located in its promoter region and certain polymorphisms affect the
expression level of the gene (16,17). The
present study hypothesized that differences in cytokine levels are
due to gene polymorphisms, which may have an important role in the
inflammatory response and influence the pathophysiology of IBD.
No association between the TNF-α promoter
polymorphisms at position-1031 and susceptibility to IBD in Iranian
patients was demonstrated in our previous findings (18). Subsequently, studies have proposed a
direct correlation between the single nucleotide polymorphism (SNP)
genotype with disease; an important reason for regulatory SNPs to
cause human genetic disease is that SNPs are located in regulatory
sequences, for example promoter regions or UTRs, that could
effected the expression of the gene. Tt is therefore important to
investigate the association between the TNF-α gene expression
pattern and its association with the −1031 polymorphism. The
present study investigated the association between the TNF-α
gene expression pattern and its association with the −1031
polymorphism in an Iranian population of patients with IBD.
Materials and methods
Patients
Between 2011 and 2014, 101 IBD patients (15 CD and
86 UC) and 100 healthy control subjects, who had been referred to
the Research Institute for Gastroenterology and Liver Diseases,
Shahid Beheshti University of Medical Sciences (Tehran, Iran), were
included in the present study. The control group individuals did
not have a family history of gastrointestinal disorders.
Furthermore, control group subjects were selected based on an
absence of any evidence, personal or family history of IBD or
inflammatory diseases, such as gastritis, ulcerative colitis and
CD. The patients and healthy individuals were all Iranian.
Colonoscopy was performed by a gastroenterologists and the
diagnosis of IBD was confirmed by a pathologist. Patients with a
history of using anti-inflammatory drugs, such as 5-aminosalicylic
acid (5ASA), prednisone (Pred), azathioprine (AZA) and infliximab
(IFX) were evaluated. Written informed consent was obtained from
each patient and healthy volunteer, and peripheral blood samples (6
ml) were collected in EDTA tubes and stored at 4°C until DNA/RNA
extraction. The Ethics Committee of the Research Institute for
Gastroenterology and Liver diseases, Shahid Beheshti University of
Medical Sciences provided approval for the present study.
Genotyping
Genomic DNA was isolated from 5 ml peripheral blood
mononuclear cells (PBMCs) using the standard salting out method
(19). The quality and quantity of DNA
was determined using a spectrophotometer and electrophoresis on
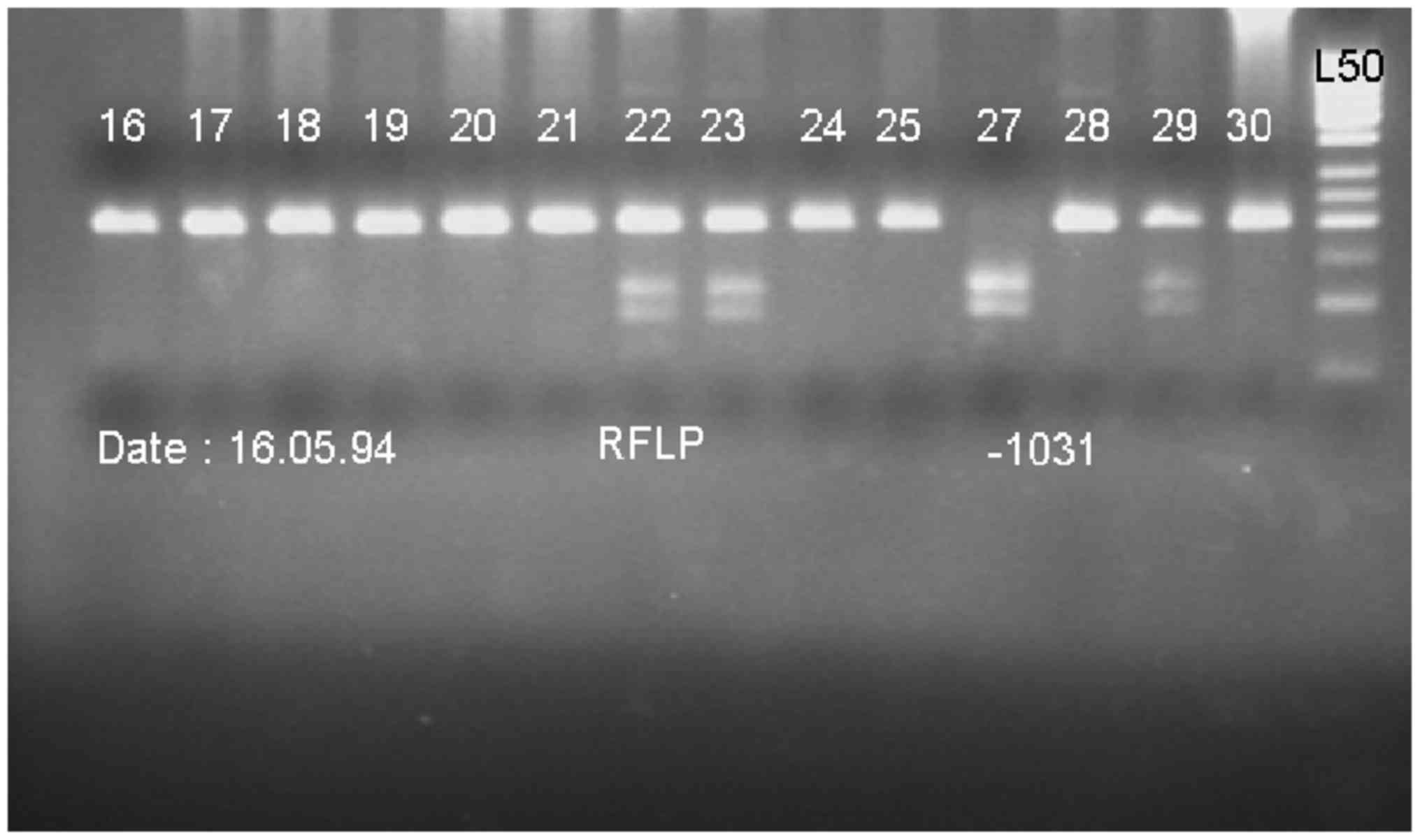
agarose gel. Genotype determination was performed by polymerase
chain reaction (PCR); the promoter −1031 TNF-α gene
polymorphism was PCR amplified in a 186-bp fragment using the
following primers: Forward, 5-CTT CAG GGA TAT GTG ATG GAC TC-3 and
reverse, 5-GGA GAC CTC TGG GGA GAT GT-3. Followed by restriction
fragment length polymorphism (RFLP). The PCR reaction was performed
on a Mastercycler (Eppendorf; Hamburg, Germany) as follows:
Denaturation for 5 min at 94°C, followed by 36 cycles of
amplification (40 sec at 94°C, 35 sec at 62°C and 40 sec at 72°C).
A final elongation step (5 min at 72°C) was applied at the end of
the 36 cycles. The PCR product was 186 bp. Following amplification,
PCR products were digested (at 37°C) by restriction endonuclease
BbsI (Thermo Fisher Scientific, Inc.; C allele, 106 and 80
bp; T allele, 186 bp) overnight. The digested PCR products were
visualized by electrophoresis in a 2.5% agarose gel (120 V for 40
min; Fig. 1).
Sequencing
To confirm the results of genotyping, 10% of the PCR
products were sequenced using the ABI PRISM 3130xL Genetic Analyzer
(Applied Biosystems; Thermo Fisher Scientific, Inc., Carlsbad, CA,
USA) and the results were fully concordant.
RNA isolation with reverse
transcription-PCR
Total RNA was extracted from PBMCs using a YTA RNA
Extraction kit (Yekta Tajhiz Azma, Tehran, Iran) according to the
manufacturer's instructions. The RNA quantity and quality was
determined from spectrophotometric optical density measurement
(wavelength, 260 and 280 nm). The cDNA was synthesized using a
Revert Aid RT Reverse Transcription kit (cat. no. K1691; Thermo
Fisher Scientific, Inc.) according to the manufacturer's
instructions. The expression rate of the TNF-α gene was analyzed
using an ABI 7500 real-time PCR system (Applied Biosystems; Thermo
Fisher Scientific, Inc.) and SYBR Master Mix (Takara Bio, Inc.,
Otsu, Japan) according to the manufacturer's instructions. Primers
were designed using Genscript and Primer3 online programs
(http://primer3.ut.ee/). The following primer
pairs were used: Forward, 5-CTGAACTTCGGGGTGATCG-3 and reverse,
5-GCT TGG TGG TTT GCT ACG AC-3 for TNF-α; forward, 5-ACA ACC TTC
TTG CAG CTC CTC-3 and reverse, 5-TGACCCATACCCACCATCAC-3 for β-actin
(ACTB). The expression levels of all target genes were normalized
against the expression of ACTB, which served as the endogenous
control (20). The first stage,
initial denaturation at 95°C for 30 sec, was followed by a second
40-replication cycle (two-step cycling at 95°C for 5 sec and 60°C
for 34 sec) and the third step (performed following creation of the
PCR melting curve) was as follows: 95°C for 15 sec, 60°C for 60 sec
and 95°C for 15 sec. The melting curve differentiates between the
different products, and demonstrates contamination and the
absorption peak. Melting curve analysis detects non-specific and
primer dimer products. The ΔΔCq method was used according to Livak
and Schmittgen (21).
Statistical analysis
SPSS statistical software version 21 (IBM Corp.,
Armonk, NY, USA) was used to perform statistical analysis of the
genotyping. The χ2 test was used to evaluate the distribution of
the allele and genotype frequencies. Furthermore, the
Hardy-Weinberg equilibrium was performed along with the χ2 test to
compare the observed genotype frequencies among the investigated
cases and control subjects with the expected genotype frequencies.
Logistic regression was applied to calculate odds ratio (OR) and
95% confidence intervals, and to adjust the data for confounding
factors, such as age and gender. P<0.05 was considered to
indicate a statistically significant difference. GraphPad prism 5
software (https://www.graphpad.com/scientific-software/prism/)
was used to perform statistical analysis of the TNF-α mRNA
expression levels. One-way ANOVA was used to examine the TNF-α mRNA
expression level between groups.
Results
Demographics
A total 101 patients with the diagnosis of IBD were
investigated, including 59 males (58.4%) and 42 females (41.6%).
The control group consisted of 100 non-IBD subjects, 58 males (58%)
and 42 females (42%). The percentage of male and female subjects in
the two groups was not significantly different (P>0.05). The
mean age of the IBD group was significantly higher than that in the
healthy control subjects group (P<0.05). Furthermore, no
significant differences were identified between the IBD group and
healthy control subjects with regard to the body mass index and
smoking behavior (P>0.05; Table
I).
 | Table I.Demographic characteristics of the
study population, including inflammatory bowel disease patients and
control subjects. |
Table I.
Demographic characteristics of the
study population, including inflammatory bowel disease patients and
control subjects.
| Variable | Patient (n=101) | Control (n=100) | P-value |
|---|
| Age (mean ± standard
deviation), years | 33.99±10.86 | 42.00±13.52 | <0.001 |
| Body mass index
(kg/m2)b | 25.19±4.99 | 25.49±5.85 | 0.698 |
| Gender, n
(%)b |
|
| 0.138 |
|
Female | 42 (41.6) | 42 (42) |
|
| Male | 59 (58.4) | 58 (58) |
|
| Smoking, n
(%)b |
|
| 0.462 |
|
Smoker | 16 (15.8) | 15 (15) |
|
|
Non-smoker | 85 (84.2) | 85 (85) |
|
Lack of associations of the
TNF-α-1031T>C polymorphism with IBD in the Iranian
population
According to our previous study (18), the frequency of TT, TC and CC genotypes
in patients were 64.4, 28.7 and 6.9%, respectively and 63, 29 and
8%, respectively in the control groups. No statistically
significant differences were identified between genotypes during
the observation and study groups (18)
(Table II).
 | Table II.Genotype distribution of −1031
polymorphism among inflammatory bowel disease patients and healthy
control subjects. |
Table II.
Genotype distribution of −1031
polymorphism among inflammatory bowel disease patients and healthy
control subjects.
| Genotype | Patients, n
(%) | Controls, n
(%) | Odds ratio (95%
confidence interval) | P-value |
|---|
| TT | 65 (64.4) | 63 (63.0) | 1.00 (Ref.) |
|
| TC | 29 (28.7) | 29 (29.0) | 0.986
(0.509–1.912) | 0.968 |
| CC | 7 (6.9) | 8 (8.0) | 1.308
(0.419–4.088) | 0.644 |
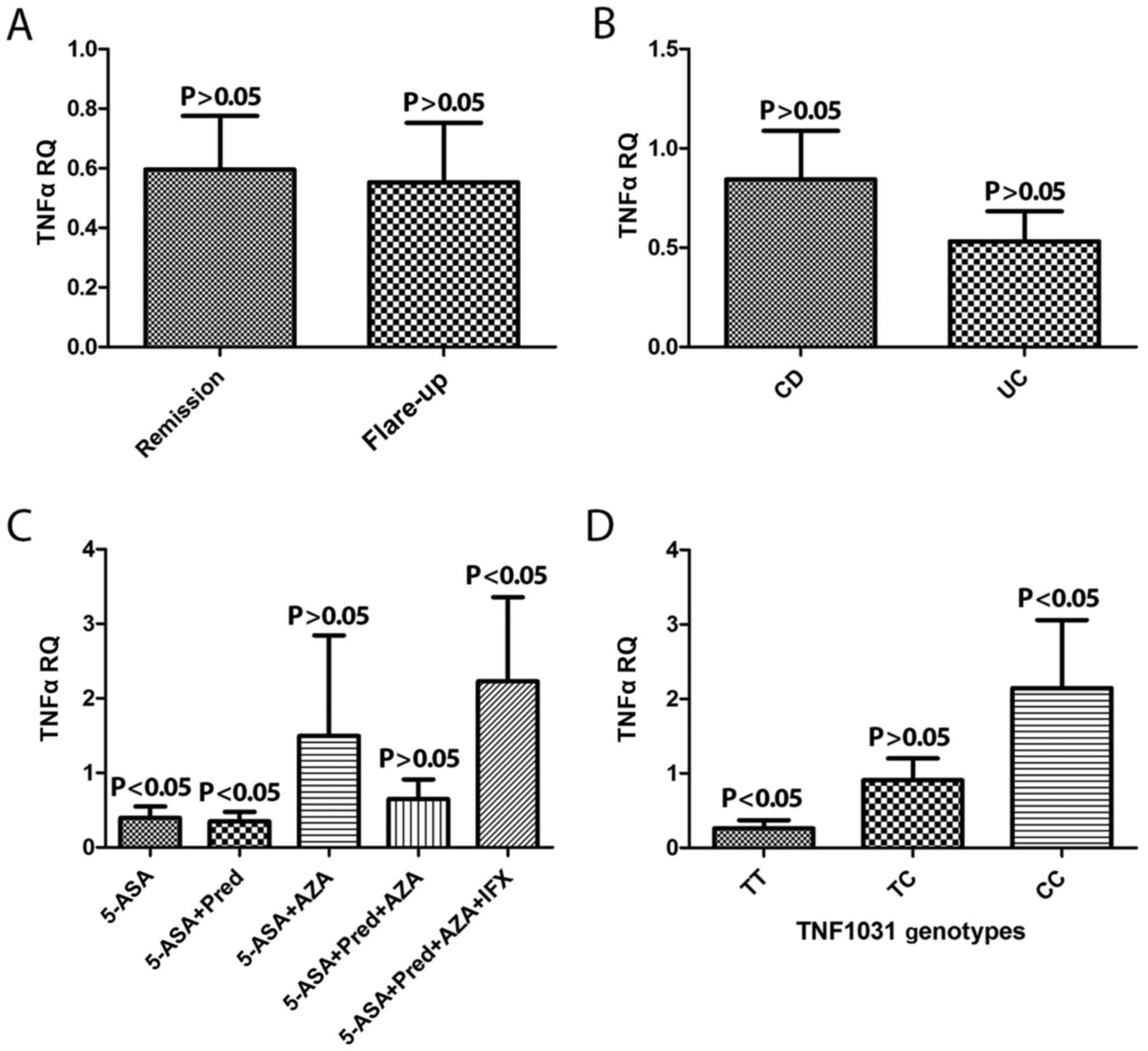
TNF-α gene expression patterns were
associated with pathological IBD subtypes
The extent of TNF-α gene expression in two
disease phases, remission and flare up, were compared. The
expression level of the TNF-α gene remained the same
(Fig. 2A). In addition, the expression
of TNFα mRNA levels between the CD and UC type of IBD
patient were analyzed and were not statistically different
(Fig. 2B).
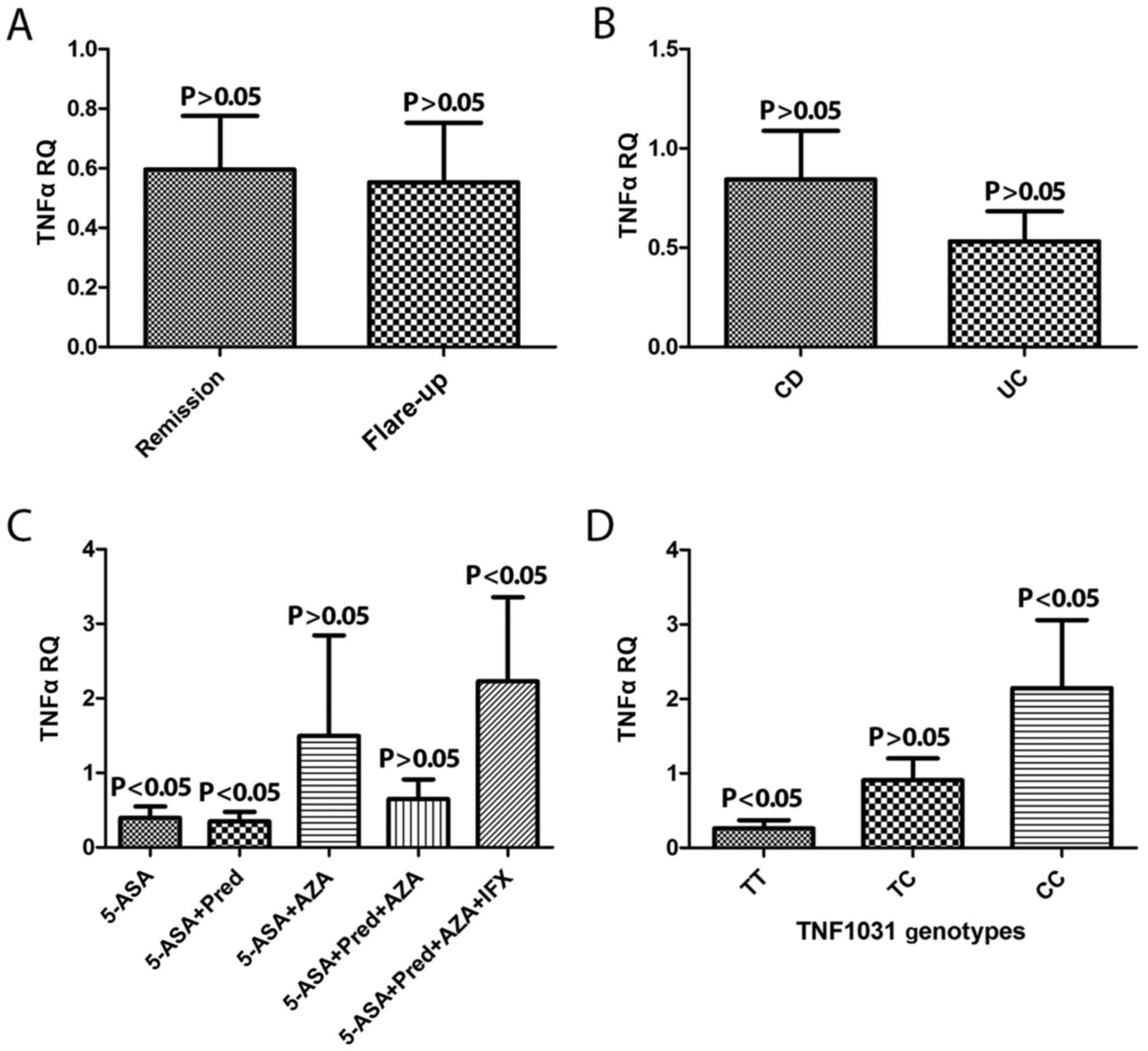 | Figure 2.TNF-α mRNA expression level (A) at
different IBD pathological phases, (B) according to the type of IBD
(UC or CD) and (C) according to drug history. (D) Interaction
between the −1031 genotype and TNF-α expression level. TNF-α, tumor
necrosis factor-α; IBD, inflammatory bowel disease; UC, ulcerative
colitis; CD, Crohn's disease; RQ, relative quantification; 5-ASA,
5-aminosalicylic acid; Pred, prednisone; AZA, azathioprine; IFX,
infliximab. |
An assessment of patients who had a history of
taking medication was also performed and patients were classified
into five different groups as follows: i) 5-ASA; ii) 5-ASA + Pred;
iii) 5-ASA + AZA; iv) 5-ASA + Pred + AZA; v) 5-ASA + Pred + AZA +
IFX according to medication usage. TNF-α gene upregulation
of mRNA exhibited a significant association in the group that
received all four types of drug when compared with the other groups
(P<0.05; Fig. 2C).
Interaction between the −1031 T>C
polymorphism genotype, phenotype and TNF-a expression levels
TNF-α gene expression was screened for the
polymorphism −1031 T>C genotypes TT, TC and CC. Overexpression
of TNF-α mRNA was observed in genotype CC when compared with
CT and TT (P<0.05; Fig. 2D).
Discussion
IBD is complex multifactorial disease, the
pathogenesis of which is not well understood (22). Allelic variants in cytokine genes have
been shown to influence gene expression and subsequently the
susceptibility to and severity of inflammation diseases (23). There is increasing evidence that TNF-α
is key in the pathogenesis of IBD and may represent novel
therapeutic targets (12). Studies
indicate the TNF-α gene as an appropriate and functional candidate
for IBD treatment (24,25). In the present study, the allele
frequency of SNP-1031 T>C was greater in patients when compared
with the control group, although the difference between the
patients and control group was not significant. Similar studies to
the current study, performed in Canada (26) and Japan (27) and Iran (28), demonstrated that the allele frequency
between the control group and CD group in polymorphism −1031 was
significant, but no significant association was observed between
the UC and the control groups. This mutant allele frequency in
certain studies, for example in the UK (24,29) and a
Canadian study (30) was not
significantly different. In another study, the T allele was shown
to confer a significant risk for developing UC in Iranian Azeri
Turkish patients (31). Previous
studies have reported conflicting results in the TNF-α gene
polymorphism susceptibility to IBD. The reasons for these
contradictory findings remain unknown. Different ethnicities,
distribution of genotype, environment-genetic interactions and
sample size, may be the cause of the inconsistent results in the
frequency of the −1031 TNF-α gene polymorphisms in the present
study.
In the current study, a correlation between
polymorphism −1031 T> C and the TNF-α mRNA expression level was
significant. The results demonstrated that the level of TNF-α gene
mRNA expression was reduced in genotype TT when compared with the
other genotypes. A recent independent study by Rad et al
(32) in 2004 demonstrated similar
results with regard to the polymorphisms of cytokines and their
effect on gene expression, which was increased in patients with the
Helicobacter pylori infection. The results showed that
variations in SNPs may change gene expression levels, leading to a
significant association with IBD. Another study by Chen et
al (33) in 1995, examined the
effect of TNF-α gene polymorphisms with mRNA expression in patients
with pre-eclampsia, and indicated that TNF-α gene mRNA expression
may be associated with its gene polymorphism.
The findings of the current study provide evidence
that patients who had taken the four drugs (5-ASA + Pred + AZA and
5. 5-ASA + Pred + AZA + IFX) for the treatment of IBD exhibit
overexpression of TNF-α mRNA. To the best of our knowledge, no
study has determined the correlation between drug use and TNF-α
gene expression in IBD patients. However, it may be that the TNF-α
gene expression may serve as a biomarker for the drug-resistant
inflammation in IBD initiation. Therefore, it is proposed that, in
future studies, an improved understanding of the association with
other TNF-α gene promoter polymorphisms and the underlying
mechanism of functional polymorphisms may provide novel therapeutic
target gene expression for the treatment of IBD patients.
In conclusion, the present study examined the
association between the TNF-α gene expression pattern and its
association with the −1031 polymorphism, which demonstrated an
increased expression of the CC genotype and a decreased expression
of the TT genotype. The overexpression of the CC genotype may
represent a genetic risk factor for IBD in an Iranian population.
In addition, overexpression of TNF-α was observed in patients who
had a history of taking the four types of drug (5-ASA, Pred, AZA or
IFX). Thus, these analyses may be used in the prognosis, diagnosis
and treatment of IBD.
References
|
1
|
Liu TC and Stappenbeck TS: Genetics and
pathogenesis of inflammatory bowel disease. Annu Rev Pathol.
11:127–148. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Okamoto R and Watanabe M: Role of
epithelial cells in the pathogenesis and treatment of inflammatory
bowel disease. J Gastroenterol. 51:11–21. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Portela F, Dias CC, Caldeira P, Cravo M,
Deus J, Gonçalves R, Lago P, Morna H, Peixe P, Ramos J, et al: The
who-when-why triangle of CAM use among portuguese IBD patients. Dig
Liver Dis. 49:388–396. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bernstein CN, Fried M, Krabshuis JH, Cohen
H, Eliakim R, Fedail S, Gearry R, Goh KL, Hamid S, Khan AG, et al:
World gastroenterology organization practice guidelines for the
diagnosis and management of IBD in 2010. Inflamm Bowel Dis.
16:112–124. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lakatos PL: Recent trends in the
epidemiology of inflammatory bowel diseases: Up or down? World J
Gastroenterol. 12:6102–6108. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Cosnes J, Gower-Rousseau C, Seksik P and
Cortot A: Epidemiology and natural history of inflammatory bowel
diseases. Gastroenterology. 140:1785–1794. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ananthakrishnan AN: Epidemiology and risk
factors for IBD. Nat Rev Gastroenterol Hepatol. 12:205–217. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Leppkes M, Neurath MF, Herrmann M and
Becker C: Immune deficiency vs. immune excess in inflammatory bowel
diseases-STAT3 as a rheo-STAT of intestinal homeostasis. J Leukoc
Biol. 99:57–66. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Khor B, Gardet A and Xavier RJ: Genetics
and pathogenesis of inflammatory bowel disease. Nature.
474:307–317. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Sadler T, Bhasin JM, Xu Y, Barnholz-Sloan
J, Chen Y, Ting AH and Stylianou E: Genome-wide analysis of DNA
methylation and gene expression defines molecular characteristics
of Crohn's disease-associated fibrosis. Clin Epigenetics. 8:302016.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
McGovern DP, Kugathasan S and Cho JH:
Genetics of inflammatory bowel diseases. Gastroenterology.
149:1163–1176.e2. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Francescone R, Hou V and Grivennikov SI:
Cytokines, IBD, and colitis-associated cancer. Inflamm Bowel Dis.
21:409–418. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zhang M, Viennois E, Prasad M, Zhang Y,
Wang L, Zhang Z, Han MK, Xiao B, Xu C, Srinivasan S and Merlin D:
Edible ginger-derived nanoparticles: A novel therapeutic approach
for the prevention and treatment of inflammatory bowel disease and
colitis-associated cancer. Biomaterials. 101:321–340. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lykouras D, Sampsonas F, Kaparianos A,
Karkoulias K, Tsoukalas G and Spiropoulos K: Human genes in TB
infection: Their role in immune response. Monaldi Arch Chest Dis.
69:24–31. 2008.PubMed/NCBI
|
|
15
|
Mocellin S, Verdi D, Pooley KA and Nitti
D: Genetic variation and gastric cancer risk: A field synopsis and
meta-analysis. Gut. 64:1209–1219. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hajeer AH and Hutchinson IV: TNF-alpha
gene polymorphism: Clinical and biological implications. Microsc
Res Tech. 50:216–228. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Li CI, Li TC, Liao LN, Liu CS, Yang CW,
Lin CH, Hsiao JH, Meng NH, Lin WY, Wu FY and Lin CC: Joint effect
of gene-physical activity and the interactions among CRP TNF-α, and
LTA polymorphisms on serum CRP, TNF-α levels and handgrip strength
in community-dwelling elders in Taiwan-TCHS-E. Age (Dordr).
38:462016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Nourian M, Asgharian AM and Aghdaei H
Asadzadeh: Lack of association between tumor necrosis factor alpha
(TNFα) gene-1031C/T polymorphisms and susceptibility to
inflammatory bowel disease (IBD). Arak Univ Med Sci J. 19:71–79.
2016.
|
|
19
|
Miller SA, Dykes DD and Polesky HF: A
simple salting out procedure for extracting DNA from human
nucleated cells. Nucleic Acids Res. 16:12151988. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Moura AC, Lazzari VM, Agnes G, Almeida S,
Giovenardi M and Veiga AB: Transcriptional expression study in the
central nervous system of rats: What gene should be used as
internal control? Einstein (Sao Paulo). 12:336–341. 2014.(In
English, Portuguese). View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(−Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Chatzikonstantinou M, Konstantopoulos P,
Stergiopoulos S, Kontzoglou K, Verikokos C, Perrea D and
Dimitroulis D: Calprotectin as a diagnostic tool for inflammatory
bowel diseases. Biomed Rep. 5:403–407. 2016.PubMed/NCBI
|
|
23
|
Takeuchi O: Posttranscriptional regulation
of cytokine mRNA controls the initiation and resolution of
inflammationChronic Inflammation. Springer; pp. 319–332. 2016,
View Article : Google Scholar
|
|
24
|
van Heel DA, Udalova IA, de Silva AP,
McGovern DP, Kinouchi Y, Hull J, Lench NJ, Cardon LR, Carey AH,
Jewell DP and Kwiatkowski D: Inflammatory bowel disease is
associated with a TNF polymorphism that affects an interaction
between the OCT1 and NF(−kappa)B transcription factors. Hum Mol
Genet. 11:1281–1289. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Chaparro M, Guerra I, Muñoz-Linares P and
Gisbert JP: Systematic review: Antibodies and anti-TNF-α levels in
inflammatory bowel disease. Aliment Pharmacol Ther. 35:971–986.
2012.PubMed/NCBI
|
|
26
|
Sanchez R, Levy E, Costea F and Sinnett D:
IL-10 and TNF-alpha promoter haplotypes are associated with
childhood Crohn's disease location. World J Gastroenterol.
15:3776–3782. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Negoro K, Kinouchi Y, Hiwatashi N,
Takahashi S, Takagi S, Satoh J, Shimosegawa T and Toyota T: Crohn's
disease is associated with novel polymorphisms in the 5′-flanking
region of the tumor necrosis factor gene. Gastroenterology.
117:1062–1068. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Naderi N, Farnood A, Dadaei T, Habibi M,
Balaii H, Firouzi F, Mahban A, Soltani M and Zali M: Association of
tumor necrosis factor alpha gene polymorphisms with inflammatory
bowel disease in Iran. Iran J Public Health. 43:630–636.
2014.PubMed/NCBI
|
|
29
|
Tremelling M, Waller S, Bredin F,
Greenfield S and Parkes M: Genetic variants in TNF-alpha but not
DLG5 are associated with inflammatory bowel disease in a large
United Kingdom cohort. Inflamm Bowel Dis. 12:178–184. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Zipperlen K, Peddle L, Melay B, Hefferton
D and Rahman P: Association of TNF-alpha polymorphisms in Crohn
disease. Hum Immunol. 66:56–59. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Bonyadi M, Abdolmohammadi R, Jahanafrooz
Z, Somy MH and Khoshbaten M: TNF-alpha gene polymorphisms in
Iranian Azari Turkish patients with inflammatory bowel diseases.
Saudi J Gastroenterol. 20:108–112. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Rad R, Dossumbekova A, Neu B, Lang R,
Bauer S, Saur D, Gerhard M and Prinz C: Cytokine gene polymorphisms
influence mucosal cytokine expression, gastric inflammation, and
host specific colonisation during Helicobacter pylori infection.
Gut. 53:1082–1089. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Chen G, Wilson R, Wang SH, Zheng HZ,
Walker JJ and McKillop JH: Tumour necrosis factor-alpha (TNF-alpha)
gene polymorphism and expression in pre-eclampsia. Clin Exp
Immunol. 104:154–159. 1996. View Article : Google Scholar : PubMed/NCBI
|