Introduction
The most relevant of the Aspergillus species
are fumigatus, flavus and niger. These grow in the
natural environment, and in tissues and cultures in the form of
hyphae that produce conidia upon exposure to air. Conidia consist
of a conidiophore with a terminal vesicle in which one or two
layers of phialides are developed. The prevalence of genitourinary
tract infections has been reported to be as high as 52% in the
female population, with the most common cause being Candida
albicans in 28% (1). With the
exception of Candida, other fungi are rarely observed in
Papanicolaou (Pap) smears or biopsies, with isolated reports of
opportunistic infections, such as Blastomyces dermatitidis,
Coccidioides immitis, Cryptococcus neoformans and
mucor being published (2,3). To the best
of our knowledge, this is one of few Aspergillus infection
cases reported regarding infection by Aspergillus as
diagnosed via liquid-based gynecologic cytology, including a
clinical and cytological follow-up.
Case report
The patient was a 57-year-old Mexican woman who had
been through the menopause five years previously and she had no
relevant medical history. During an annual medical checkup in July
2015, the patient went to the gynecology service at the Hospital
Universitario ‘Dr José Eleuterio González’ (Monterrey, Mexico). She
presented without any signs, symptoms or concerns. Furthermore,
previous checkups revealed no anomalies. However, the physical
examination revealed an atrophic state in the vagina and
cervix.
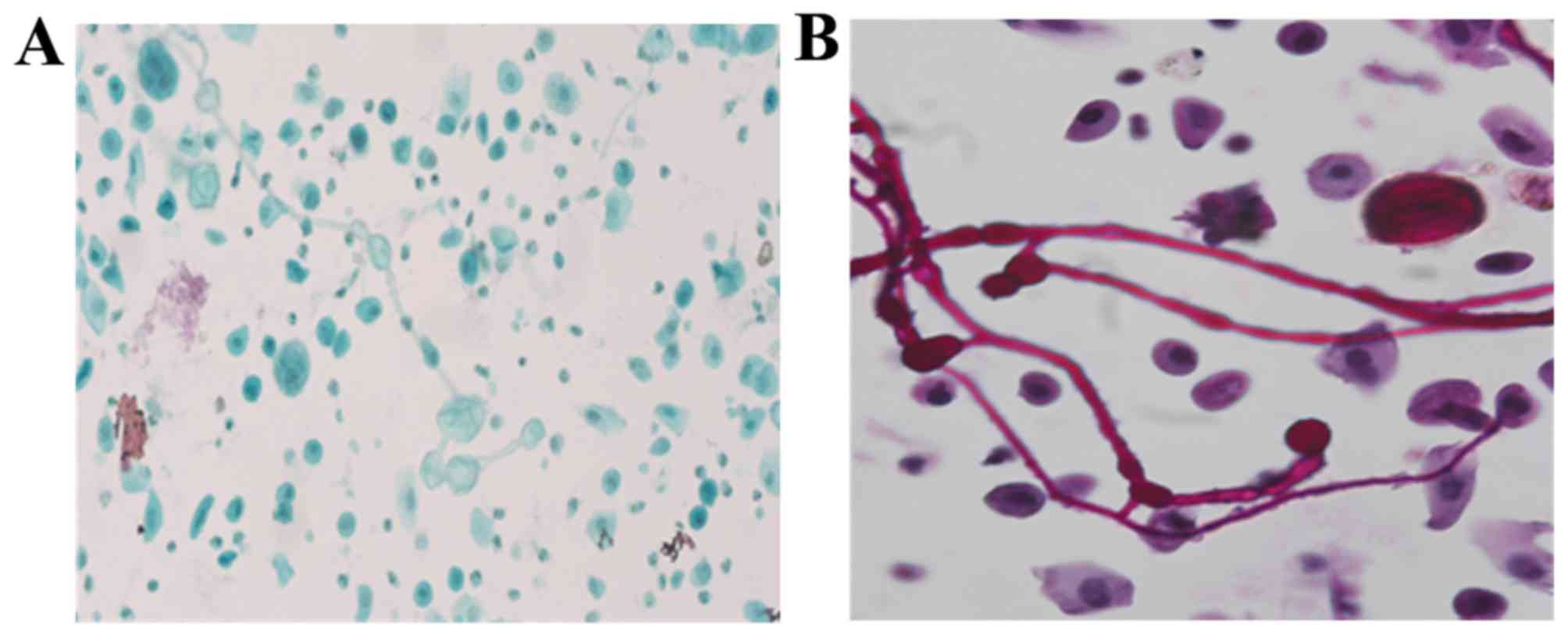
Previous patient authorization, a routine
liquid-based cervical cytology was performed and demonstrated
atrophy with a predominance of parabasal cells and scarce
endocervical cells. Of note, multiple fungal structures with
uniform and homogeneous forms, and a parallel contour were
identified; septate hyphae, and acute-angle branching (45°)
consistent with Aspergillus spp. were observed too. Terminal
vesicles were identified, but there were no phialides. The
Aspergillus' morphology was accompanied by features of severe
chronic and acute inflammation, foreign body giant cells and
numerous benign squamous cells. The squamous cells and fungal
structures were situated in the same plane.
As laboratory contamination is a diagnostic
challenge, and even though fungal structures were observed in the
same plane as cells, a novel aliquot was created from the same
sample (Fig. 1). The second slide
demonstrated the same findings and Periodic acid-Schiff (PAS)
staining was used to highlight the microorganisms (Fig. 2). As the patient was asymptomatic it
was decided to obtain a novel sample 10 days later to rule out
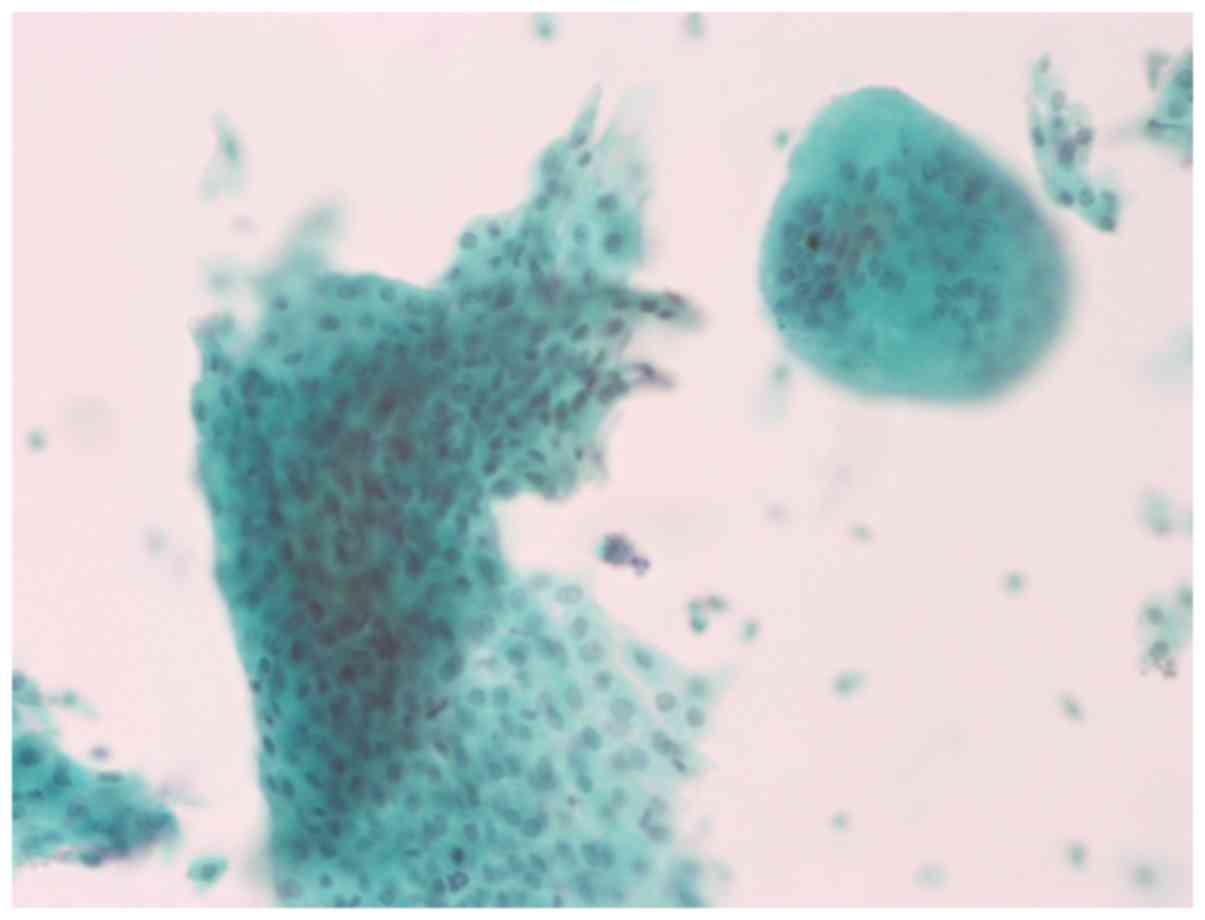
cross-contamination. This second sample again presented numerous
hyphae and vesicles consistent with Aspergillus (Fig. 3). Post-treatment cytology, also
liquid-based, exhibited large numbers of parabasal cells, a cleaner
background, multinucleated giant cells and an absence of fungi
(Fig. 4). Treatment was initiated with
vaginal itraconazole for seven days, although the patient was
asymptomatic. The only risk factor that was established was
occasional cleansing of the genital area after cleansing of the
nostrils, using the same handkerchief.
The fruiting bodies of Aspergillus provide
information about this fungus and its species. Identification of
the length and size of the conidiophore, as well as the shape of
the vesicles of the conidia, are important. In histological
sections and smears, thick and uniform septate hyphae (3–6 µm) are
observed. In addition, a dichotomy division at an angle of 45° is
characteristic (4). These findings
correlate with the fungus that was observed in multiple smears in
the present study. The fungus is easily observed using a Pap smear;
however, stains for fungi, such as PAS and Grocott, highlight the
morphology. Conidia are rarely observed in tissue samples in human
infections, as these forms when the fungus is exposed to air.
Conidia are observed in conditions, such as fungus
ball/aspergillomas. The observation of Aspergillus in a Pap
smear is rare. It can represent a symptomatic infection in
immunosuppressed patients or patients undergoing prolonged
antibiotic treatment or in patients with a contamination. Previous
studies have reported that equipment used for the Pap test (vaginal
mirrors, foil and spray attachments) may be contaminated (5–8). In the
current case, the quantity of pseudo-hyphae and the presence of a
significant chronic inflammatory infiltrate, in addition to its
position in the same plane as the epithelial cells, indicated that
this was a genuine infection.
Discussion
There are previous reports on the presence of
Aspergillus in smear tests. Certain reports describe
cervical smears where the authors conclude that the results could
be due to contamination, as the other five slides exhibited the
same hyphae (5,6). Additional case reports exhibited a smear
test result with a description of a fruiting body in a patient
(6,7).
Deb and Srivastava (3) and Gupta et
al (5) reported concomitant
Aspergillus in patients with high-grade intraepithelial
lesions, which could be explained by their immunocompromised state
(3,5,9). To the best
of our knowledge, Hoda et al (10) are the only other authors to report on
liquid-based Aspergillus, identifying only one fruiting
body; however, they do not report any inflammatory infiltrate or
hyphae that could clarify whether the finding was due to
contamination (10).
Identification of a fungus that tends to cause
systemic infection alerts the attending physician to look for and
identify risk factors, specifically factors that lead to
immunocompromise. In the current case, all the necessary
precautions were taken to identify whether this was truly an
infection rather than a contamination. Initially, all slides that
were processed immediately were evaluated to observe any
pseudo-hyphae, in addition to repeating the liquid-based cytology
to rule out equipment contamination in the cytology department.
Finally, a second cytology specimen was performed with completely
different equipment from that which was used during the first
sample. Once the diagnosis of Aspergillus was confirmed,
adequate treatment was administered. All appropriate measures were
taken to confirm that the observation of cervicovaginal
Aspergillus infection from liquid-based cytology and a Pap
smear was not due to contamination.
Acknowledgements
The authors would like to thank Dr Sergio
Lozano-Rodríguez for the critical reading of the manuscript.
References
|
1
|
Sullam SA, Mahfouz AA, Dabbous NI,
el-Barrawy M and el-Said MM: Reproductive tract infections among
married women in Upper Egypt. East Mediterr Health J. 7:139–146.
2001.PubMed/NCBI
|
|
2
|
Sheyn I, Mira JL and Thompson MB:
Paracoccidioides brasiliensis in a postpartum Pap smear. A
case report. Acta Cytol. 45:79–81. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Deb P and Srivastava A: Aspergillus
in a cervico-vaginal smear of an adult postmenopausal female: An
unusual case. J Cytol. 26:123–124. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Donta B, Naik DD, Mali BN, Bandiwadekar A,
Ramnath K and Rao M: ‘Fruiting body’ Penicillium species:
Papanicolaou stained conventional cervical smear findings. Diagn
Cytopathol. 38:34–35. 2010.PubMed/NCBI
|
|
5
|
Gupta P, Goyal S and Kaushal M:
Concomitant aspergillus species infection and squamous cell
carcinoma diagnosed on Pap smear. Turk Patoloji Derg. 32:54–56.
2016.PubMed/NCBI
|
|
6
|
Brimo F, Ouad L, Brodeur J, Charbonneau M
and Auger M: Unusual microbial organisms seen in two cervical
smears. Diagn Cytopathol. 37:836–838. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Martínez-Girón R and Fernández-García C:
Aspergillus/Penicillium sp. spores as a contaminant on
conventional Pap smear. Diagn Cytopathol. 37:899–900. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Policarpio-Nicolas ML, Covell J, Moore K
and Stelow EB: ‘Paintbrush’ appearance of Penicillium
species in Thin-Prep cervico-vaginal (Pap) test. Diagn Cytopathol.
36:721–722. 2008. View
Article : Google Scholar : PubMed/NCBI
|
|
9
|
Chandra S, Gaur D, Harsh M, Chaturvedi J
and Kishore S: An unusual presentation of Aspergillus
species in a routine cervicovaginal pap smear: A case report. Acta
Cytol. 53:229–231. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Hoda RS, Colello C, Roddy M and Houser PM:
‘Fruiting body’ of Aspergillus species in a routine
cervico-vaginal smear (Pap test). Diagn Cytopathol. 33:244–245.
2005. View
Article : Google Scholar : PubMed/NCBI
|