Introduction
In the last five years, several studies have
evaluated whether a correlation between the C677T and A1298C
polymorphisms of the methylenetetrahydrofolate reductase (MTHFR)
gene and a higher risk of recurrent pregnant loss (RPL) exists
(1,2).
The C677T and A1298C variants of the MTHFR gene, in certain
conditions, may lead to an increase in plasma homocysteine (Hcy)
and homocysteineemia, which can cause endothelial damage in blood
vessels (3). This may increase
thromboembolic risk, which in pregnant women can lead to an
obstruction of the placental vessels resulting in recurrent
abortions. Thus, hyperhomocysteinemia is considered a risk factor
for recurrent pregnancy loss (RPL), and patients with RPL may
exhibit hyperhomocysteinemia; therefore, as part of routine
check-up for RPL, serum homocysteine should be measured. Once
diagnosed, treatment of hyperhomocysteinemia with folic acid and
vitamin B12 is able to markedly decrease homocysteine levels
(3).
Homocysteine (Hcy) is a non-essential,
sulfur-containing, non-proteinogenic amino acid. It is an
intermediate metabolite in the synthesis of methionine
(remethylation reaction) and in the synthesis of cysteine
(transulfuration reaction) (3). The
enzymes involved in these metabolic pathways are: i) MTHFR, the
coenzyme for which is vitamin B9, also known as folic acid
(FA)/folate or pteroyl-L-glutamate; ii) methionine synthetase (MS),
which uses vitamin B12 (cobalamin) as a cofactor; and iii)
cystathionin-β-synthetase (CBS), with vitamin B6 as its coenzyme
(3).
The active form of FA in an organism is derived from
a reduction reaction of FA into tethrahydrofolic acid
(tethrahydrofolate, THF), with the latter being the true coenzyme
of MTHFR. MTHFR and MS are involved in the recycling of Hcy into
methionine (remethylation reactions), whereby Hcy acquires a methyl
group from 5-MTHF to form the methionine (3). A mild or moderate form of
hyperhomocysteinemia can be caused by folate deficiency, a direct
or indirect lack of 5-methilentethrahydrofolate, a functional
defect in MTHFR, MS, CBS or B9, or deficiencies in B12 and B6
vitamins (3).
MTHFR catalyzes irreversible conversion of
5,10-methylentethrahydrofolate to 5-methiltethrahydrofolate
(CH3-THF). The normal activity of MTHFR aids to maintain folate and
methionine in the bloodstream at constant levels, preventing Hcy
accumulation (3). Polymorphisms in
the gene encoding MTHFR may lower its enzymatic activity. The
variant C677T leads to a substitution of a cytosine into a thymine
at position 677 within exon 4 of the MTHFR gene. This genetic
variant leads to an amino acidic substitution in position 222 at
the protein level (p.Ala>Val) (3).
Individuals carrying the MTHFRA222V variant in heterozygous form
(genotype Ala/Val) can exhibit a 35% reduction in enzymatic
activity relative to the basal activity level of non-carriers,
while homozygotes for the variant (genotype Val/Val) can exhibit a
30% reduction in enzymatic activity relative to non-carriers
(4). An additional MTHFR polymorphism
associated with a reduction in enzyme activity is the substitution
of an adenine with a cytosine in position 1,298 (A1298C) (5,6). This
variation leads to the substitution of a glutamate with an alanine
in position 429 at the protein level (p.429Glu>Ala) (7). It has been demonstrated that the C677T
and A1298C polymorphisms in heterozygous form, along with a folate
deficiency, lead to increased levels of plasmatic Hcy (7).
Patients carrying the C677T polymorphism of MTHFR in
homozygous form (TT), leading to a thermolabile MTHFR variant,
exhibit decreased formation of CH3-THF under conditions of folate
deficiency: This leads to lower production of S-adenosylmethionine
and subsequently lower availability of methyl groups (-CH3)
required for methylation events, including the methylation of DNA
(8,9).
Additionally, the lower availability of CH3-THF results in reduced
remethylation of Hcy, followed by an increase in plasmatic Hcy
(hyperhomocysteinemia) (8).
Conversely, wild-type individuals for the C677T genotype (CC) are
not influenced by folate deficiency, and thus CH3-THF synthesis for
the methylation reaction and for the conversion of Hcy in
methionine is preserved. Regarding these processes, the C677T and
A1298C genotypes should not affect the availability of CH3-THF
under an adequate supply of folate (9). However, current methods are unable to
delineate a direct correlation between the aforementioned variants
of the MTHFR gene and thromboembolic risk, and in turn, risk of RPL
in pregnant women. The aim of the present study was to investigate
the putative association between the C677T and A1298C variants and
RPL risk.
Subjects and methods
Subjects
A total of 767 pregnant women (mean age, 30±1.2
years) who visited the Unit of Cytogenetic and Molecular Genetics,
‘Madonna delle Grazie’ Hospital (Matera, Italy) from January 2010
to July 2016 to undergo molecular tests for the detection of the
C677T and A1298C variants of the MTHFR gene were enrolled. The
pregnant women were divided into two groups (group A and group B)
based on miscarriage history. The present study protocol was
approved by the Ethics Committee of Basilicata University (Potenza,
Italy) and all participants provided written informed consent.
Pregnant women belonging to group A (n=380) had
positive anamnesis of at least two miscarriage events. These women
exhibited negative responses to antithrombin deficiency,
anticoagulant C protein and protein S tests, exhibited no increased
resistance to activated C protein, had neither the A20210G mutation
in prothrombin gene nor the G1691A mutation in Leiden factor V gene
(p.Arg506Gln). They also had a negative response to
antiphospholipid antibodies. The pregnant women belonging to group
B (n=387) were experiencing their second or third pregnancy and had
negative anamnesis for miscarriage, as well as negative results in
the aforementioned clinical tests. All enrolled patients and their
partners carried a normal karyotype.
Groups A and B were further divided into two
subgroups based on gestational age [first trimester (≤13 weeks of
gestation) and second trimester (from 17 weeks and 4 days to 26
weeks and 2 days of gestation)]. Thus, the 380 women in group A
were partitioned as those who had a miscarriage during the first
trimester of pregnancy (343/380) and those who had a miscarriage in
the second trimester of pregnancy (37/380). The 387 women in group
B (control group) were partitioned as those subjected to molecular
testing in the first trimester of pregnancy (244/387) and those
subjected to molecular testing in the second trimester of pregnancy
(143/387).
Groups A and B were subjected to preconception
prophylaxis (at least one month prior to conception) with oral
administration of 400 mcg (6S)-5-methyltetrahydrofolic acid
glucosamine salt, 1.75 g myo-inositol, 250 mg D-chiro-inositolo,
120 mg vitamin C; 100 mg methylsulfonylmethane and 12.5 mg zinc
(Logus Pharma Srl, San Marino, Italy; cat. no. SM22015 47849).
DNA extraction and molecular
analysis
For all subjects, molecular testing was performed on
venous blood samples (in EDTA-K3) according to the following steps:
i) DNA was isolated from 25 µl venous blood using a DNA extraction
kit obtained from Nuclear Laser Medicine Srl (Settala, Italy; cat.
no. AA1001); ii) to study the C677T and A1298C variants of the
MTHFR gene, the target genomic area was amplified by polymerase
chain reaction (PCR) using two commercial kits provided by Nuclear
Laser Medicine Srl [cat. nos. AA901 (C677T) and AA902 (A1298C)].
Following kit protocols, this enabled the detection of single
nucleotide polymorphisms using a Rotor-Gene Q MDx (Qiagen Srl,
Milan, Italy) using fluorescent oligos annealed to specific DNA
target sequences in the gene of interest, and the PCR products were
quantified using the Fluorescent Resonance Energy Transfer method
(10); iii) the variants of the
target sequences were measured from melting curves.
Statistical analysis
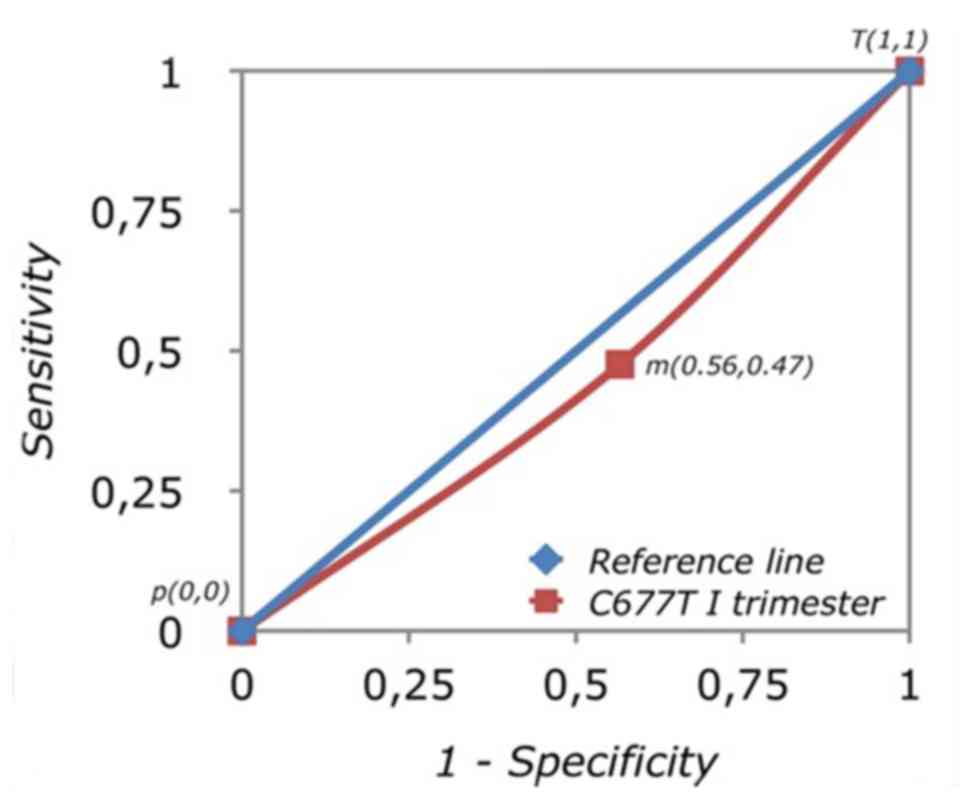
The results were compared through receiver operating
characteristic (ROC) curve using JMP software version 2 (https://www.jmp.com/it_it/home.html). The ROC
curve permits assessment of the accuracy of a diagnostic test.
Analysis of a ROC curve is based on the evaluation of the area
under the curve (AUC): This expresses the probability that the
parameter of an individual randomly selected from the test
population is higher than the parameter of an individual randomly
selected from the control sample. In reality, it considers
appropriate tests with an AUC ≥80%. The statistical indicators used
to define this graph are specificity (Sp) and sensitivity (Se). The
Sp of a diagnostic test indicates the ability of the test to
correctly separate, in the studied population, healthy individuals
from individuals carrying the medical condition of interest
(11).
Results and Discussion
MTHFR polymorphism genotypes
Of the 380 pregnant women in group A, 86
heterozygotes and 74 homozygotes for C677T were identified, while
54 heterozygotes and 32 homozygotes for A1298C were identified. A
total of 103 were compound heterozygotes, and31 were devoid of
mutation.
Of the 387 pregnant women in group B, 100
heterozygotes and 90 homozygotes for C677T were identified. For the
A1298C variant, 35 were heterozygous and 32 were homozygous. A
total of 110 subjects were compound heterozygotes and 20 lacked
mutation.
Comparison of polymorphism genotypes
in the first and second trimesters of pregnancy
C677T and A1298C genotype data were compared between
the women in groups A and B in their first trimester of pregnancy.
Additionally, C677T and A1289C genotype data were compared between
the women in groups A and B in their second trimester of pregnancy.
The results were compared through ROC curve and Z-score
statistics.
On ROC curve analysis of all pregnant women in their
first trimester of pregnancy based on the presence of C677T in
MTHFR, an AUC of 0.45 area units (au) with 95% confidence interval
(CI) 0.30–0.56 was derived (Fig. 1).
From a statistical point of view, the area under the reference line
is equal to 0.5 au: This value is associated with a diagnostic test
without discriminatory qualities, and thus is null. From this data,
it may be inferred that there was no association between MTHFR
C677T and RPL; therefore, the C677T variant in the considered
sample was not useful regarding diagnostic value. The probability
of identifying an individual carrying the C677T mutation in the
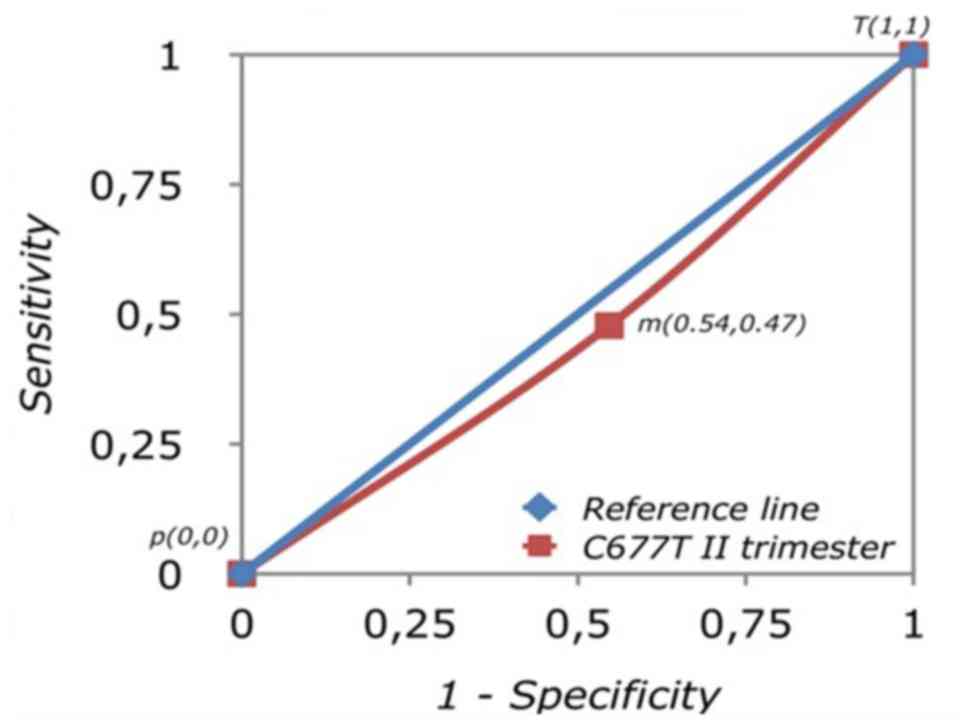
analyzed population was random. These findings were confirmed by
the same analysis (C677T vs. WT) performed in the pregnant women in
their second trimester of pregnancy. The AUC was 0.46 au with 95%
CI 0.37–0.67 (Fig. 2).
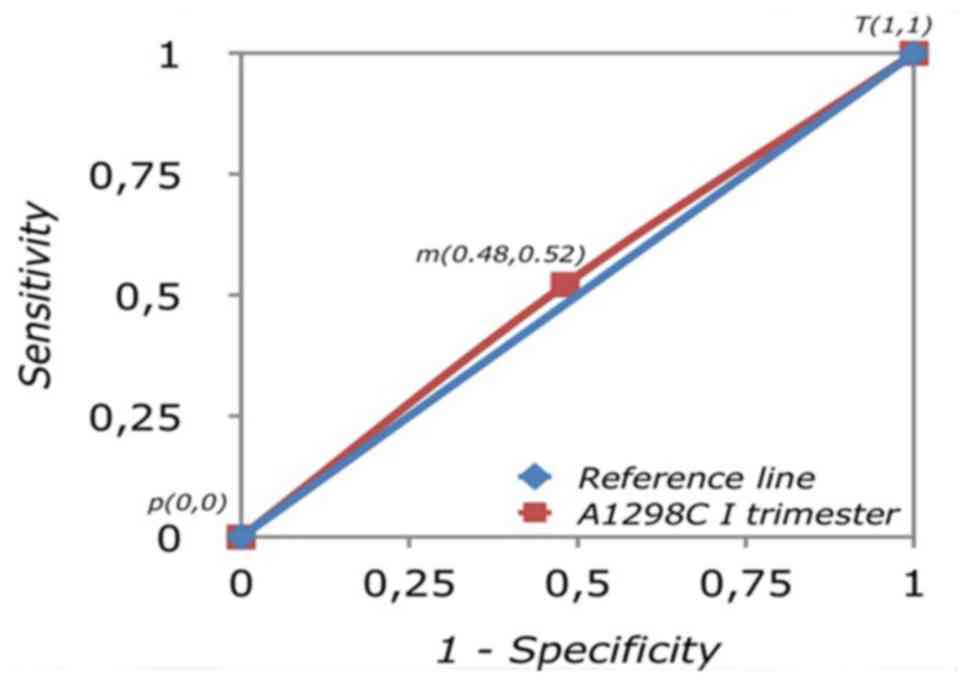
Analysis of the A1298C variant in MTHFR was
subsequently performed. The molecular screening of all women in
their first trimester obtained an AUC of 0.51 au (95% CI:
0.40–0.67; Fig. 3). In this case, the
results indicated that this screening test was not useful. The
negative diagnostic application of this molecular screening of
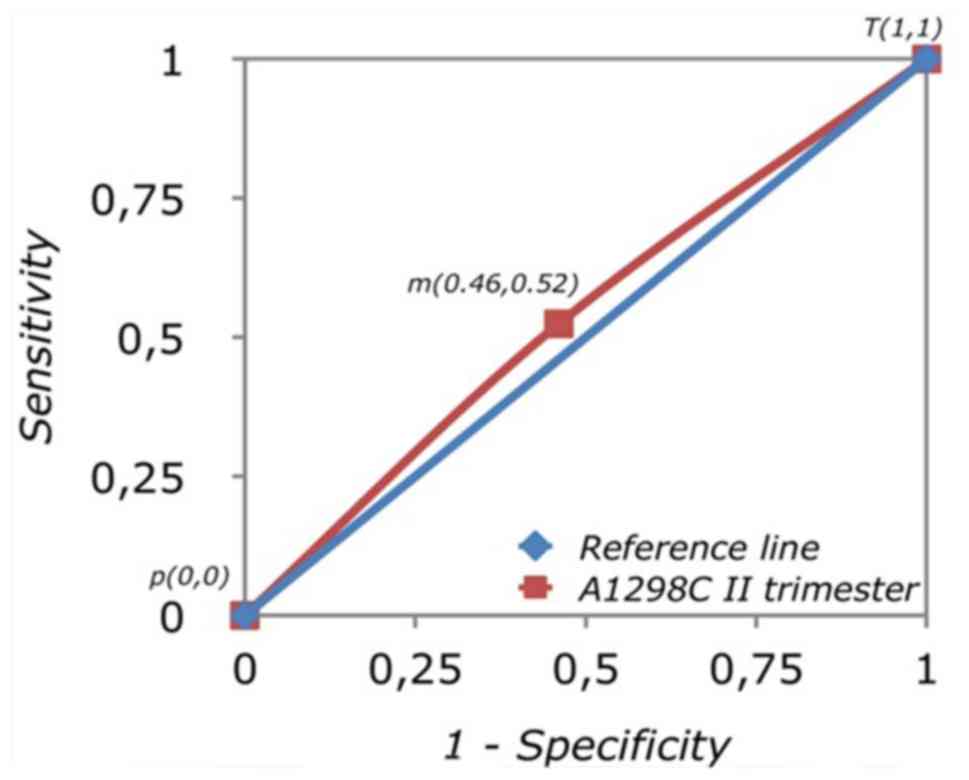
A1298C was confirmed by the same analysis in the women in their
second trimester: The AUC was 0.52 au (95% CI: 0.44–0.67; Fig. 4), indicating the random effect that an
individual carrying this mutation belonged to the study population
rather than the control. This indicated that there was no
association between the A1298C variant and RLP risk.
In conclusion, based on the present findings, to
carry the C677T and A1298C variants of the MTHFR gene does not
appear to influence predisposition to miscarriage in the first or
second trimester of pregnancy. Thus, it may be unadvantageous to
analyze them for diagnostic aims. However, daily intake of folic
acid remains an important therapeutic practice for pregnant women
in order to reduce the risk of congenital defects among other
complications (12–14). Regarding MTHFR and RPL risk,
interaction with other genetic variants has also been speculated
(15) and requires investigation.
Acknowledgements
The authors are thankful to the ‘Association Gian
Franco Lupo’ (ONLUS: a non-profit organization of social utility)
for their support.
References
|
1
|
Yang Y, Luo Y, Yuan J, Tang Y, Xiong L, Xu
M, Rao X and Liu H: Association between maternal, fetal and
paternal MTHFR gene C677T and A1298C polymorphisms and risk of
recurrent pregnancy loss: A comprehensive evaluation. Arch Gynecol
Obstet. 293:1197–1211. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Levin BL and Varga E: MTHFR: Addressing
Genetic Counseling Dilemmas Using Evidence-Based Literature. J
Genet Couns. 25:901–911. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Park WC and Chang JH: Clinical
Implications of Methylenetetrahydrofolate Reductase Mutations and
Plasma Homocysteine Levels in Patients with Thromboembolic
Occlusion. Vasc Spec Int. 30:113–119. 2014. View Article : Google Scholar
|
|
4
|
Baum L, Wong KS, Ng HK, Tomlinson B,
Rainer TH, Chan DK, Thomas GN, Chen X, Poon P, Cheung WS, et al:
Methylenetetrahydrofolate reductase gene A222V polymorphism and
risk of ischemic stroke. Clin Chem Lab Med. 42:1370–1376. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sibani S, Leclerc D, Weisberg IS,
O'Ferrall E, Watkins D, Artigas C, Rosenblatt DS and Rozen R:
Characterization of mutations in severe methylenetetrahydrofolate
reductase deficiency reveals an FAD-responsive mutation. Hum Mutat.
21:509–520. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Botto N, Andreassi MG, Manfredi S, Masetti
S, Cocci F, Colombo MG, Storti S, Rizza A and Biagini A: Genetic
polymorphisms in folate and homocysteine metabolism as risk factors
for DNA damage. Eur J Hum Genet. 11:671–678. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Friso S and Choi SW: Gene-nutrient
interactions and DNA methylation. J Nutr. 132:2382S–2387S.
2002.PubMed/NCBI
|
|
8
|
Dell'edera D, Tinelli A, Milazzo GN,
Malvasi A, Domenico C, Pacella E, Pierluigi C, Giuseppe T, Marcello
G, Francesco L, et al: Effect of multivitamins on plasma
homocysteine in patients with the 5,10 methylenetetrahydrofolate
reductase C677T homozygous state. Mol Med Rep. 8:609–612. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Martinez-Serra J, Robles J, Nicolàs A,
Gutierrez A, Ros T, Amat JC, Alemany R, Vögler O, Abelló A, Noguera
A, et al: Fluorescence resonance energy transfer-based real-time
polymerase chain reaction method without DNA extraction for the
genotyping of F5, F2, F12, MTHFR, and HFE. J Blood Med. 5:99–106.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Pritchett YL and Tamura R: Global
benefit-risk assessment in designing clinical trials and some
statistical considerations of the method. Pharm Stat. 7:170–178.
2008. View
Article : Google Scholar : PubMed/NCBI
|
|
11
|
Schmidt RJ, Tancredi DJ, Ozonoff S, Hansen
RL, Hartiala J, Allayee H, Schmidt LC, Tassone F and
Hertz-Picciotto I: Maternal periconceptional folic acid intake and
risk of autism spectrum disorders and developmental delay in the
CHARGE (CHildhood Autism Risks from Genetics and Environment)
case-control study. Am J Clin Nutr. 96:80–89. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Parker SE, Yazdy MM, Tinker SC, Mitchell
AA and Werler MM: The impact of folic acid intake on the
association among diabetes mellitus, obesity, and spina bifida. Am
J Obstet Gynecol. 209:239.e1–239.e8. 2013. View Article : Google Scholar
|
|
13
|
Friberg AK and Jørgensen FS:
Periconceptional folic acid prophylaxis and neural tube defects.
Ugeskr Laeger. 177:1595–1598. 2015.(In Danish). PubMed/NCBI
|
|
14
|
Greene ND, Leung KY, Gay V, Burren K,
Mills K, Chitty LS and Copp AJ: Inositol for prevention of neural
tube defects: A pilot randomised controlled trial - CORRIGENDUM. Br
J Nutr. 115:16972016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Settin A, Elshazli R, Salama A and ElBaz
R: Methylenetetrahydrofolate reductase gene polymorphisms in
Egyptian women with unexplained recurrent pregnancy loss. Genet
Test Mol Biomarkers. 15:887–892. 2011. View Article : Google Scholar : PubMed/NCBI
|