Introduction
Lumbar degenerative spondylolisthesis (LDS) is
defined as the excessive displacement of one vertebral body
relative to another due to degenerative changes in spinal support
structures, such as disks, ligaments, and facet joints (1-3).
LDS can occur in any segment of the spine but is most commonly
found in the L4/L5 segment, which may be due to the large range of
flexion-extension motion that involves this segment (3,4).
Lumbar instability refers to any abnormal movements of the spine
beyond its normal range. Mechanical instability due to spinal
degeneration can cause clinical symptoms, such as back pain or
nerve compression, presenting as leg pain, leg weakness, and cauda
equina syndrome (1,5,6). When
clinical symptoms worsen, surgical treatments should be considered.
Early and accurate diagnosis can promote the initiation of
appropriate treatment strategies and improve clinical outcomes in
this patient population. The treatment strategies include surgery
with decompression or decompression with fusion and conservative
treatment (7,8). Standing lateral flexion-extension
(SLFE) radiographs are used as the gold standard for diagnosing
spinal instability (1,2,5).
Previously, several studies have reported that disk degeneration
and signs of facet joint effusion detected on T2-weighted (T2W) MRI
can be indicators of potential lumbar spine instability (8,9).
However, qualitative MRI evaluations are highly dependent on the
subjective judgments of the radiologist. In this study,
quantitative value assessments including disk height, facet fluid
thickness, ligamentum flavum thickness, and disk signal intensity
on T1-weighted (T1W) and T2W MRI were assessed to identify
potential factors and their efficacy in the diagnosis of unstable
L4/L5 degenerative spondylolisthesis.
Materials and methods
Study subjects
A retrospective study was conducted on 81 patients
(age range, 39 to 85 years old, median age, 59 years old) diagnosed
with L4/L5 LDS based on X-ray and MRI evaluations at the Viet Duc
Hospital between January 2021 and January 2022. The patients were
divided into 2 groups, the stable group (SG) which included 39
women and 19 men and the unstable group (UG) which included 20
women and 3 men. The institutional review board of Hanoi Medical
University approved this retrospective study (approval no.
2444/QĐ-ĐHYHN, dated 13 July 2021). Due to the retrospective nature
of this study, the requirement for informed consent was waived by
the institutional review board of Hanoi Medical University. The
study was performed in accordance with the ethical standards of the
responsible committee on human experimentation and in line with the
guidelines described in the Declaration of Helsinki 1975, as
revised in 2013(10). All patients
underwent 4 postural lumbar spine X-rays and lumbar spine MRI with
basic pulse sequences. Exclusion criteria included
spondylolisthesis with trauma, tumor, infection, spondylolysis,
surgical history, and congenital hypoplasia of the joints.
Plain film technique
X-rays of the lumbar spine were obtained for all
cases in 4 positions: anteroposterior, lateral, maximal flexion,
and maximal extension while standing. X-rays were performed using
GE Definium XR120 (75-80 kV, 20-25 mAs, 100 cm).
MRI technique
All MRI scans were performed using either a Siemens
1.5 T Magnetom Essenza (Siemens Healthineers) or a Philips Ingenia
1.5 T (Philips Medical Systems) using basic sequences, including
sagittal T1W, sagittal and axial T2W, and coronal short tau
inversion recovery. The parameters of these sequences are described
in Table I.
 | Table ILumbar MRI parameters. |
Table I
Lumbar MRI parameters.
| Parameters | Repetition time,
ms | Echo time, ms | Slice thickness,
mm | Field of view,
mm | Matrix |
|---|
| Sagittal T1W | 600-700 | 20-30 | 4 | 160-250 | 256x256 |
| Sagittal T2W | 2000-3000 | 90-100 | 4 | 160-250 | 256x256 |
| Coronal short tau
inversion recovery | 3000-3200 | 90-100 | 4 | 160-250 | 256x256 |
| Axial T2W | 2000-3000 | 90-100 | 4 | 160-250 | 256x256 |
Image analysis
X-rays and MRI data were stored using the INFINITT
PACS system (INFINITT Healthcare) and analyzed retrospectively by a
radiologist with >10 years of experience with musculoskeletal
imaging.
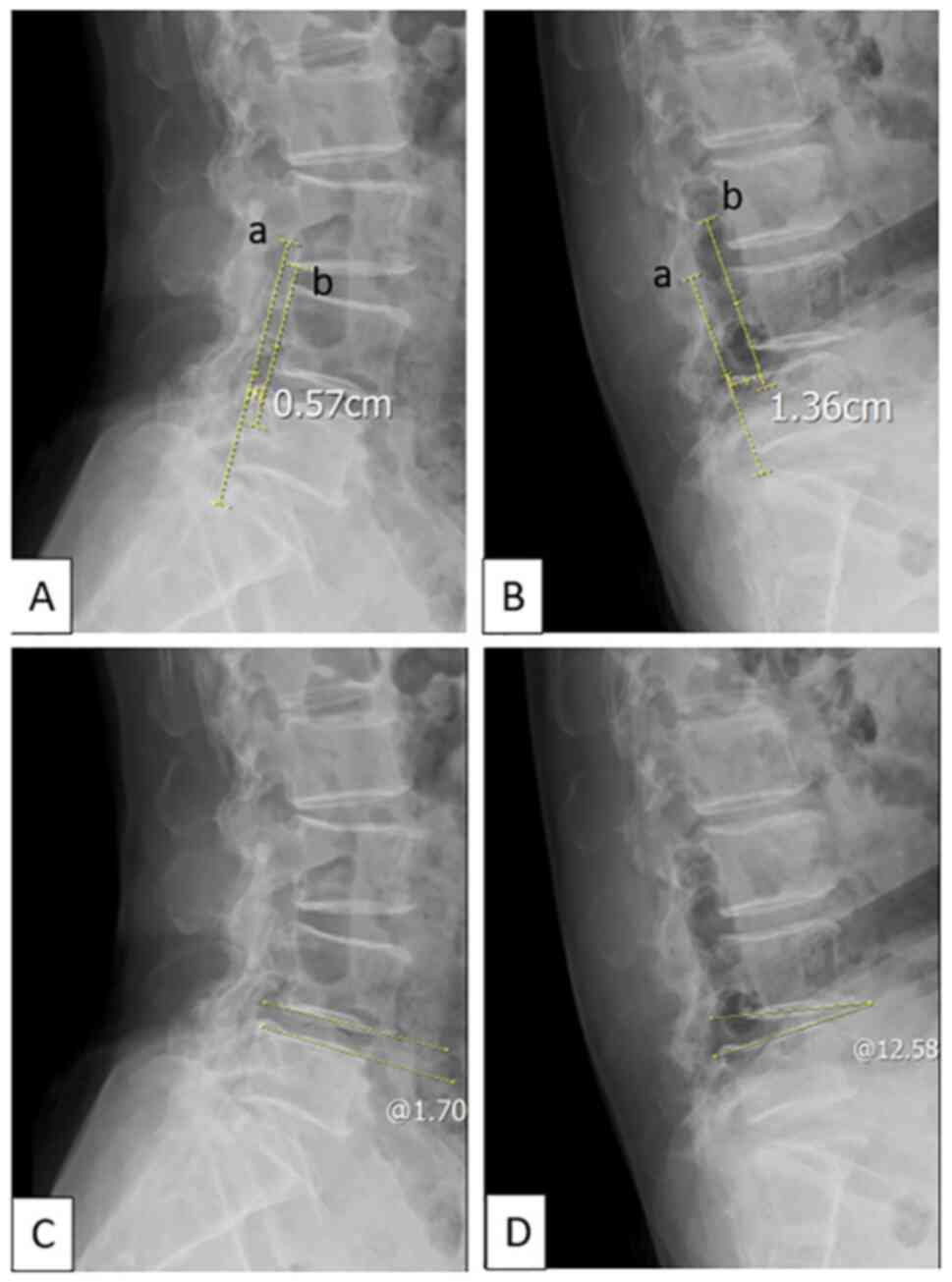
The Tailliard method was used to measure the slip
distance on dynamic radiographs and MRI (11): The first line passes through the
dorsal edges of the L5 vertebral body (line a), whereas the second
line passes through the lower posterior margin of the L4 vertebral
body and is parallel to the first line (line b). The distance
between two lines where they pass through the upper ends of the
lower vertebra is recorded as the slip distance (Figs. 1 and 2).
On dynamic radiographs, dynamic translation is
calculated as the difference in displacement distance between
maximal flexion and maximal extension in the same position; angular
displacement is calculated as the difference in angle between the
lower ends of the L4 vertebral body and the upper ends of the L5
vertebral body comparing maximal flexion and maximal extension in
the same position (Fig. 1). Dynamic
translation >5 mm or angular displacement >10˚ is defined as
an unstable vertebral body slip (12-15).
Based on these criteria, the study subjects were divided into two
groups: The UG and the SG.
The disk height was determined by calculating the
Farfan Index, as the sum of the anterior and posterior border
heights divided by the disk width as measured on the sagittal plane
of T2W images (Fig. 2) (16). Facet fluid was measured
perpendicular to the joint at the site of greatest volume on axial
T2W images (Fig. 3) (17,18).
The ligamentum flavum was measured at the joint surface level on
axial T2W images (Fig. 3) (19). Quantitative values for disk signal,
including minimum, maximum, and mean signal values, were obtained
by placing a region of interest (ROI) ellipse in the center of the
intervertebral disk on sagittal T1W and T2W images (Fig. 2).
Statistical analysis
Statistical analysis was performed using SPSS
version 20 (IBM Corp). Quantitative variables are presented as the
mean ± SD. Qualitative variables are presented as the frequency and
percentage. Differences between two quantitative variables were
compared using an independent-samples Student's t-test. Normality
was evaluated using the Kolmogorov-Smirnov test. A χ2
test or Fisher's exact test were used to compare the distribution
of sexes. P<0.05 was considered to indicate a statistically
significant difference.
Receiver operating characteristic (ROC) curve
analysis was used to evaluate quantitative variables that can be
used to differentiate between two groups, and a cut-off value, the
area under the curve (AUC), sensitivity (Se), specificity (Sp),
positive predictive value (PPV), and negative predictive value
(NPV) were obtained for significant predictive variables.
Results
Clinico-radiological characteristics
of the patient population
A total of 58 patients with a definitive diagnosis
of L4/L5 LDS without instability, as assessed using SLFE
radiographs (SG, 58 cases, 71.6%), and 31 patients with instability
based on SLFE radiographs (UG, 23 cases, 28.4%) were identified for
study inclusion (Table II).
 | Table IIClinico-radiological characteristics
of the patient population. |
Table II
Clinico-radiological characteristics
of the patient population.
| Characteristics | Stable group,
n=58 | Unstable group,
n=23 | P-value |
|---|
| Age, years | 58.93±10.2 | 57.22±9.7 | 0.486 |
| Sex, n (%) | | | |
|
Male | 19 (32.75) | 3 (13.04) | 0.422 |
|
Female | 39 (67.25) | 20 (86.96) | 0.432 |
| Plain films | | | |
|
Dynamic
translation, mm | 1.93±1.2 | 4.97±1.5 | ≤0.001a |
|
Angular
displacement, ˚ | 4.17±2.3 | 7.85±4.1 | ≤0.001a |
| Slip distance on the
MRI scan, mm | 5.11±2.2 | 5.44±1.9 | 0.53 |
No significant differences were identified in the
age or sex distribution between the SG and UG. X-ray-based
measurements of dynamic translation and angular displacement were
significantly higher in the UG than in the SG. The slip distance
measured on MRI in the UG was 5.44±1.9 mm, which was larger than
the distance measured in the SG of 5.11±2.2 mm; however, this
difference was not significant.
MRI characteristics
The mean disk height of the UG was lower than that
of the SG, but the difference was not significant. The mean facet
joint was significantly thicker in UG than in the SG. The UG also
displayed a thicker mean ligamentum flavum than the SG, but the
difference was not significant. No significant differences in the
minimum, maximum, or mean disk signal intensity values were
measured on either T1W or T2W images between the UG and SG.
However, these values tended to be lower in the UG than in the SG
(Table III).
 | Table IIIMRI characteristics. |
Table III
MRI characteristics.
|
Characteristics | Stable group,
n=58 | Unstable group,
n=23 | P-value |
|---|
| Mean disk height,
mm | 0.45±0.15 | 0.52±0.58 | 0.381 |
| Mean facet fluid
thickness, mm | 0.89±1.11 | 2.15±1.23 | ≤0.001a |
| Mean ligamentum
flavum thickness, mm | 3.70±1.17 | 4.09±1.02 | 0.144 |
| Disk signal
T1W | | | |
|
Min | 226.66±135.9 | 189.70±162.98 | 0.342 |
|
Max | 341.55±171.96 | 306.39±168.53 | 0.405 |
|
Mean | 287.41±150.95 | 245.98±163.61 | 0.300 |
| Disk signal
T2W | | | |
|
Min | 66.36±53.54 | 57.52±45.47 | 0.458 |
|
Max | 231.29±112.34 | 210.26±105.86 | 0.433 |
|
Mean | 171.34±225.36 | 145.27±69.99 | 0.591 |
Based on the significant difference observed in the
mean value of facet joint fluid thickness between the UG and SG,
the ROC curve was analyzed, as shown in Fig. 4.
The mean facet fluid thickness was a significant
predictor of the differential diagnosis between the SG and UG, with
moderate accuracy (0.7<AUC=0.77<0.8) with Se, Sp, PPV, and
NPV values of 73.9, 67.2, 69.3, and 69.77%. respectively.
Discussion
In the present study, the quantitative values
obtained from MRI scans were analyzed to determine their relevance
in the diagnosis of unstable L4/L5 degenerative spondylolisthesis.
Although only facet joint fluid factor was the only statistically
significant factor, other quantitative values between the two
groups were compared, including the mean disk height, ligamentum
flavum thickness, or disk signal intensity on T1W or T2W images.
This study used ROC curves for mean facet joint fluid thickness
assessment, which provided the area under the curve, cut-off value,
Se, Sp, PPV, and NPV of quantitative values from MRI scans in the
diagnosis of unstable L4/L5 degenerative spondylolisthesis.
LDS is a common cause of spondylolisthesis (20) that can occur in any spinal segment,
but typically affects the L4/L5 level; 69% of cases, according to
Cho et al (9) and 71.05% of
cases according to Even et al (21) due to the large range of motion
experienced at this spinal level. Kirkaldy-Willis and Farfan
(22) proposed that lumbar
degenerative diseases progress in three clinical stages: Transient
dysfunction, followed by instability, and culmination in
restability. A spinal instability diagnosis in LDS patients is
essential for developing an appropriate treatment plan and
evaluating the prognosis of the patient (23). Lumbar spinal instability is an
independent risk factor for spinal surgery failure (24). Previous reports have defined the
unstable LDS stage (also known as mobile LDS) according to changes
in the slip distance and angular displacement on SLFE radiographs
(12-15).
In a study of 91 patients with LDS by Cho et al (9), the study sample was divided into two
groups (SG and UG), with unstable LDS defined as a dynamic
translation >5 mm or angular displacement >10˚ based on SLFE
radiographs. Thus, this definition was applied to the 81 patients
in the present study, resulting in 58 patients being categorized
into the SG and 23 in the UG.
The present study showed that the mean age of the SG
was higher than that of the UG, but this difference was not
significant. This outcome is similar to that reported by Kuhns
et al (8), who reported mean
ages for the SG and UG of 67 and 64 years, respectively. However,
Cho et al (9) showed a
significant difference in age between the SG and UG, which were
62.2 and 65.3 years, respectively.
According to the present study, no significant
difference was identified in the mean disk height. However, the UG
had a larger mean disk height than the SG. This result was similar
to that reported by Kuhns et al (8), who reported a larger mean disk height
for the UG (0.70 mm) than for the SG (0.67 mm), although the
difference was not significant. Disk height is correlated with the
disk degeneration grade, with a larger degeneration grade
associated with a smaller disk height. Cho et al (9) demonstrated that the average disk
degeneration grade in the SG was significantly higher than that in
the UG. Fujiwara et al (25)
showed that the greatest range of motion was observed on SLFE films
associated with grade III and IV disk degeneration, whereas spinal
motion was reduced in patients with grade V disk degeneration.
Hypertrophy of the ligamentum flavum is significantly correlated
with disk and facet joint degeneration, which may be a predisposing
factor for spinal instability (19). In the study by Yoshiiwa et al
(19), the group with a ligamentum
flavum thickness ≥4 mm showed greater angular displacement than the
group with a ligamentum flavum thickness <4 mm, although this
difference was not significant. The authors concluded that
hypertrophy of the ligamentum flavum may be a useful sign for
diagnosing spinal instability on MRI scans. These results are
similar to the results of the present study. Although no
significant difference was observed for the thickness of the
ligamentum flavum between the UG and SG, the ligamentum flavum in
the UG (4.09±1.02 mm) was thicker on average than that of the SG
(3.70±1.17 mm).
In the present study, the mean facet joint fluid in
the UG was significantly thicker than that in the SG. This result
is in agreement with the results reported in previous studies.
Chaput et al (17)
demonstrated that facet joint fluid thickness ≥1 mm on MRI scans
was indicative of an unstable LDS on SLFE radiographs. According to
the study by Snoddy et al (26), an increase of 1 mm in facet joint
fluid thickness increased the risk of spinal instability by 41.6%
(95% CI: 1.8-97.0%), by contrast, facet joint fluid thickness ≤0.5
mm was associated with a 90% chance of spinal stability. Moreover,
this previous study also reported a PPV of 30% for facet joint
fluid thickness in detecting spinal instability (26). The study results reported by Kuhns
et al (8) showed a
significant difference in the facet joint fluid thickness between
the UG and SG, with mean values of 2.0 and 1.2 mm, respectively.
The PPV of the facet joint fluid thickness for detection of an
unstable lumbar spine increased from 52% with an effusion width
>1 mm to 100% with an effusion width >3.5 mm. In addition, in
the study by Lattig et al (18), the unstable LDS group had a larger
mean facet joint fluid thickness value than the stable LDS group
(1.77 vs. 0.10 mm). The results of the present study showed that
the mean value of the facet joint fluid thickness could be used to
differentiate the SG from the UG using a cut-off value of 1.45 mm
with an AUC of 0.77, and a Se, Sp, PPV, and NPV of 73.9, 67.2,
69.3, and 69.77%, respectively. It is thus hypothesized that an
increase in the facet joint fluid may be related to changes in
spinal kinematics in weight-bearing positions, leading to an
increased probability of spinal instability.
According to the present study, the minimum,
maximum, and mean disk signal intensity values on both T1W and T2W
images were lower in the UG than in the SG. However, these
differences were not significant. By contrast, in the study by Cho
et al (9), examining
qualitative levels of disk degeneration described a significantly
higher disk degeneration grade for the SG (3.96+0.88) than for the
UG (3.0+0.77). Disk degeneration is caused by dehydration in the
nucleus disk, leading to a reduced disk signal on T2W. A higher
disk degeneration grade is associated with a lower disk signal on
T2W (1).
The present study has some limitations. First, the
study was performed using a small cohort, which may not be
sufficiently representative of the overall population of
individuals with LDS. Second, the use of a single L4/L5 evaluation
may represent another weakness. Although this is the most common
level associated with LDS, the conclusions drawn may not apply to
patients with LDS at other levels or patients with multistage LDS.
In addition, the measurement of facet joint fluid thickness on
axial T2W images does not reflect the true 3D volume of facet joint
fluid (17,18). The quantitative measurements of ROI
signals were performed by a single radiologist in this study and
may thus be subject to measurement error. In the future, similar
studies with larger cohorts, and with data analysis performed by at
least 2 radiologists, with the inclusion of assessments of
different lumbar levels will be performed.
In conclusion, facet joint fluid thickness measured
on axial T2W images may be predictive of an unstable LDS,
especially if >1.45 mm. Therefore, when LDS is clinically
suspected, the use of SLFE and MRI are recommended for
diagnosis.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
NDHung, NTH, NTHA, NDM, and NDHue were the patient's
physicians, and they reviewed the literature search, and
contributed to acquisition, analysis and interpretation of data,
and manuscript drafting. NDHung and NMD contributed to manuscript
drafting and acquisition of data. NTH and NTHA analyzed and
interpreted the imaging findings. NDHung and NDHue confirm the
authenticity of all the raw data. All authors read and approved
final version of this manuscript for publication.
Ethics approval and consent to
participate
The institutional review board of Hanoi Medical
University approved this retrospective study (approval no.
2444/QĐ-ĐHYHN). Due to the retrospective nature of this study, the
requirement for informed consent was waived by institutional review
board of Hanoi Medical University. The study was performed in
accordance with the ethical standards of the responsible committee
on human experimentation and in accordance with the guidelines
described in the Declaration of Helsinki 1975, as revised in
2013.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Greenberg MS: Spine and Spinal Cord. In:
Handbook of Neurosurgery. Eighth edition, New York, Thieme,
pp1098-1099, 2016.
|
|
2
|
Jacobsen S, Sonne-Holm S, Rovsing H,
Monrad H and Gebuhr P: Degenerative lumbar spondylolisthesis: An
epidemiological perspective: The Copenhagen osteoarthritis study.
Spine (Phila Pa 1976). 32:120–125. 2007.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Rosenberg NJ: Degenerative
spondylolisthesis. Predisposing factors. J Bone Joint Surg Am.
57:467–474. 1975.PubMed/NCBI
|
|
4
|
Sanderson PL and Fraser RD: The influence
of pregnancy on the development of degenerative spondylolisthesis.
J Bone Joint Surg Br. 78:951–954. 1996.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Errico T, Blondel B and Xavier S: Schmidek
& Sweet operative neurosurgical techniques: Indications,
methods, and results. Management of Degenerative Lumbar Stenosis
and Spondylolisthesis 6th edition. Philadelphia, Elsevier Saunders,
pp1891-1899, 2012.
|
|
6
|
Standaert CJ and Herring SA:
Spondylolysis: A critical review. Br J Sports Med. 34:415–422.
2000.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Alfieri A, Gazzeri R, Prell J and
Röllinghoff M: The current management of lumbar spondylolisthesis.
J Neurosurg Sci. 57:103–113. 2013.PubMed/NCBI
|
|
8
|
Kuhns BD, Kouk S, Buchanan C, Lubelski D,
Alvin MD, Benzel EC, Mroz TE and Tozzi J: Sensitivity of magnetic
resonance imaging in the diagnosis of mobile and nonmobile L4-L5
degenerative spondylolisthesis. Spine J. 15:1956–1962.
2015.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Cho IY, Park SY, Park JH, Suh SW and Lee
SH: MRI findings of lumbar spine instability in degenerative
spondylolisthesis. J Orthop Surg (Hong Kong).
25(2309499017718907)2017.PubMed/NCBI View Article : Google Scholar
|
|
10
|
World Medical Association. World Medical
Association Declaration of Helsinki: Ethical principles for medical
research involving human subjects. JAMA. 310:2191–2194.
2013.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Sun Y, Wang H, Yang D, Zhang N, Yang S,
Zhang W and Ding W: Characterization of radiographic features of
consecutive lumbar spondylolisthesis. Medicine (Baltimore).
95(e5323)2016.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Boden SD and Wiesel SW: Lumbosacral
segmental motion in normal individuals. Have we been measuring
instability properly? Spine (Phila Pa 1976). 15:571–576.
1990.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Hayes MA, Howard TC, Gruel CR and Kopta
JA: Roentgenographic evaluation of lumbar spine flexion-extension
in asymptomatic individuals. Spine (Phila Pa 1976). 14:327–331.
1989.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Knutsson F: The instability associated
with disk degeneration in the lumbar spine. Acta Radiologica.
25:593–609. 1944.
|
|
15
|
Shaffer WO, Spratt KF, Weinstein J,
Lehmann TR and Goel V: 1990 Volvo Award in clinical sciences. The
consistency and accuracy of roentgenograms for measuring sagittal
translation in the lumbar vertebral motion segment. An experimental
model. Spine (Phila Pa 1976). 15:741–750. 1990.PubMed/NCBI
|
|
16
|
Farfan HF: The pathological anatomy of
degenerative spondylolisthesis. A cadaver study. Spine (Phila Pa
1976). 5:412–418. 1980.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Chaput C, Padon D, Rush J, Lenehan E and
Rahm M: The significance of increased fluid signal on magnetic
resonance imaging in lumbar facets in relationship to degenerative
spondylolisthesis. Spine (Phila Pa 1976). 32:1883–1887.
2007.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Lattig F, Fekete TF, Grob D, Kleinstück
FS, Jeszenszky D and Mannion AF: Lumbar facet joint effusion in
MRI: A sign of instability in degenerative spondylolisthesis? Eur
Spine J. 21:276–281. 2012.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Yoshiiwa T, Miyazaki M, Notani N, Ishihara
T, Kawano M and Tsumura H: Analysis of the relationship between
ligamentum flavum thickening and lumbar segmental instability, disc
degeneration, and facet joint osteoarthritis in lumbar spinal
stenosis. Asian Spine J. 10:1132–1140. 2016.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Wiltse LL, Newman PH and Macnab I:
Classification of spondylolisis and spondylolisthesis. Clin Orthop
Relat Res. 23–29. 1976.PubMed/NCBI
|
|
21
|
Even JL, Chen AF and Lee JY: Imaging
characteristics of ‘dynamic’ versus ‘static’ spondylolisthesis:
Analysis using magnetic resonance imaging and flexion/extension
films. Spine J. 14:1965–1969. 2014.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Kirkaldy-Willis WH and Farfan HF:
Instability of the lumbar spine. Clin Orthop Relat Res. 110–123.
1982.PubMed/NCBI
|
|
23
|
Wood KB, Popp CA, Transfeldt EE and
Geissele AE: Radiographic evaluation of instability in
spondylolisthesis. Spine (Phila Pa 1976). 19:1697–1703.
1994.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Blumenthal C, Curran J, Benzel EC, Potter
R, Magge SN, Harrington JF Jr, Coumans JV and Ghogawala Z:
Radiographic predictors of delayed instability following
decompression without fusion for degenerative grade I lumbar
spondylolisthesis. J Neurosurg Spine. 18:340–346. 2013.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Fujiwara A, Lim TH, An HS, Tanaka N, Jeon
CH, Andersson GB and Haughton VM: The effect of disc degeneration
and facet joint osteoarthritis on the segmental flexibility of the
lumbar spine. Spine (Phila Pa 1976). 25:3036–3044. 2000.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Snoddy MC, Sielatycki JA, Sivaganesan A,
Engstrom SM, McGirt MJ and Devin CJ: Can facet joint fluid on MRI
and dynamic instability be a predictor of improvement in back pain
following lumbar fusion for degenerative spondylolisthesis? Eur
Spine J. 25:2408–2415. 2016.PubMed/NCBI View Article : Google Scholar
|