Introduction
Stroke is a leading cause of long-term disability,
morbidity and mortality globally (1). Worldwide, stroke is the second leading
cause of mortality (2,3), and has continued to increase in recent
years. A major economic and social burden is the high prevalence of
stroke because the psychological, social and physical consequences
of strokes on patients are devastating (4). Stroke influences personal autonomy and
quality of life (QOL). QOL is an important healthcare issue in
patients with stroke which is influenced by various factors such as
sex, age, comorbidity, mood and disability (5,6). In
addition, patients with silent strokes remain poorly treated
because the symptoms are clinically undetectable and difficult to
discover (7-9).
The majority of stroke patients suffer from ischemic
stroke and are older than 65 years. Post-stroke survivors are
affected in multiple ways. First, motor impairment is the main
factor that contributes to a decrease of social activities and
gives rise to emotional and behavioural changes in post-stroke
patients. Cognitive impairments are also important sequelae after
stroke. Mental and emotional instability due to brain signalling
pathway disruption early after stroke is a key factor that affects
the post-stroke recovery and decreases QoL. However, long-term
emotional and behavioural changes are challenging issues to be
addressed (7-9).
In addition, post-stroke depression (PSD) is an
important aspect to deal with in stroke survivors and their
families. PSD is one of the main contributors to a diminished QoL
after stroke and an increase in mortality (10,11).
Notably, one third of post-stroke survivors are affected by PSD in
the early stage after stroke but also, after several years after
stroke onset.
Despite the research effort made in the field of
strokes, clinical studies in the Romanian population are scarce.
Management of stroke remains frequently limited by state of the art
rehabilitation facilities and by financial considerations hindering
access to thrombolytic therapy (12).
Coronavirus disease-19 (COVID-19) first occurred in
Wuhan, China; it was declared a pandemic in March 2020 and
subsequently became a major global health threat. Since 2021, over
100 million individuals from 210 countries have been confirmed to
have been infected with the COVID-19 virus (13).
In Romania, the first case of infection with the new
coronavirus was confirmed on February 26, 2020 and the first three
deaths were recorded on March 22, 2020 reaching a maximum of 591
deaths per day on November 2, 2021. The virus is expected to remain
active until 2024 even after adequate control measures,
particularly with the emergence of numerous mutants called variants
of concern, including B.1.1.7 (alpha), B.1.617.2 (delta), and
B.1.1.529 (omicron) (14).
PSD is frequently under-detected and under-treated
due to social stigma and cognitive deficits that mask the
post-stroke depression symptoms. Mental and physical health
assessments are crucial in the determination of post-stroke
cognitive complications including PSD and long-term outcomes in
stroke patients. The QoL indicator is useful to assess beneficial
or detrimental changes in patients with stroke after treatment.
However, the functional outcome after stroke depends on multiple
factors. The hypothesis of the authors is that assessment of the
Health-Related Quality of Life (HRQoL) is a powerful tool that can
improve the diagnosis of post-stroke comorbidities, including PSD
and predict the long-term outcome of stroke survivors (10,11).
However, an important factor that influences PSD
development is the absence of family support. The incidence of
post-stroke mental complications is increased in individuals
without family support. On the other hand, the caregivers of stroke
patients are often neglected. There is a lack of tools, that enable
the investigation of the impact of stroke on the QoL of caregivers.
Since, QoL of caregivers is directly associated with the long-term
outcome of post-stroke survivors, there is an urgent need to
correctly identify the effects of stroke from a social point of
view. This gap of knowledge is even more deep regarding informal
caregivers, which are the main support system in low and
middle-income countries. This is due to limited access and limited
resources in the transitional period from hospital to home-care
services (10,11).
Since post-stroke recovery is strongly dependent by
socio-cultural, genetic and personal factors, the aim of the
present study was to identify socio-demographic key factors that
play a role in the impairment of the HRQoL of patients or their
caregivers, in the southern part of Romania. The findings of the
present study may provide an improved understanding of the
socio-cultural differences in stroke-related complications, and in
the identification of the optimal specific interventions, in the
multimodal approach therapy of post-stroke survivors. In addition,
the present study may aid in attracting attention on the critically
decreasing QoL of stroke-survivors and their caregivers, thus,
leading to significant improvements through the development of
adapted health policy strategies.
Materials and methods
Ethical issues
The present study was approved (Registration no.
156/2021) by the Academic and Scientific Ethics and Deontology
Committee of the University of Medicine and Pharmacy in Craiova
(Craiova, Romania) according to the European Union Guidelines
(Declaration of Helsinki). All the patients signed an information
and acceptance form to be included in the present study.
Study design
A total of 70 patients out of 95, diagnosed with
ischemic stroke (mild and severe) between October 2021 and March
2022, were included in the present study. The inclusion criteria
were as follows: i) Only patients who had a caregiver also willing
to participate in the present study, >18 years of age; ii)
consecutive patients; and iii) patients that returned home after
the discharge. The exclusion criteria were as follows: i) Patients
not adherent to the questionnaire; ii) patients in a coma or
non-cooperative; and iii) patients with a caregiver that did not
adhere to the questionnaire. The present study constitutes a
prospective follow-up study.
In order to assess the most difficult period
according to a previous study (15), namely, the transitional period from
hospital care to home care, assessment was performed at two time
points: i) A baseline time point at the end of the hospitalization
period and ii) after three months of home care.
Examination and tools
The demographic variables included were sex, age,
marital status, employment status, urban/rural environment, level
of education, smoking, obesity, number of comorbidities and family
support. The communication deficiency (no deficiency, with aphasia,
dysarthria, aphasia and dysarthria), lesion location (right, left,
base), hospitalization days, Trial of Org 101072 in Acute Stroke
Treatment (TOAST), activities of daily living (ADL), Barthel Index,
discharge Modified Rankin Scale (mRS) score and HRQoL, were
included. In order to appreciate the functional outcome, available
scale assessment was performed by a trained specialist.
ADL is a scale that was first used for functional
assessment status of elderly individuals associated with daily
living activities. This tool can be used as a self-report or by
indirect/direct observation. The ADL scale includes 5 parameters:
Personal hygiene, dressing, toilet hygiene, mobility and
self-feeding. The ADL score is between 0-7, where 0 indicates total
dependance and 7 indicates independance. The ADL scale is currently
used for chronically ill patients (4).
The Barthel index is a stroke severity scale
consisting of 10 activities including feeding, personal toileting,
bladder and bowel control, movement from chair or bed, and walking
or use of stairs. Similar to the ADL scale, it can be conducted as
a self-report or through indirect/direct observation. Each
parameter is rated according to the ability of whether the patient
can or cannot perform a task. The index rating is in the 0-100
range, where 0-20 is considered total dependency and 100 is
independency (5).
TOAST is a tool used as a stroke classification
system that establishes five stroke subtypes and the stratification
of stroke patient in clinical studies (16).
The 15-dimensional (15D) HRQoL measure is a generic
and validated questionnaire that explores 15 dimensions (mobility,
vision, hearing, breathing, sleeping, eating, speech, excretion,
usual activities, mental function, discomfort and symptoms,
depression, distress, vitality and sexual activity), through a 15D
score representing the overall HRQoL on a 0-1 scale (0=being dead
and 1=full health). The translated version for the Romanian
population (17) that was
successfully applied on stroke patients (17-19),
was used.
Statistical analysis
Statistical analysis was performed using SPSS
version 20 (IBM Corp.). Descriptive statistics included calculation
of the mean, median, standard deviation (SD) and interquartile
range. Matched samples were compared using Wilcoxon's signed-rank
test. Violin plots were drawn to visualize the distribution of
HRQoL across the two assessed periods of time in such a manner that
those distributions could be compared. Spearman's correlation
analysis was performed to illustrate the correlations between the
variables. The heatmap matrix was drawn in order to visualize the
strength and direction of the correlations. Colours ranged from
bright blue (strong positive correlation; r=1.0) to bright orange
(strong negative correlation; r=-1.0). P<0.05 was considered to
indicate a statistically significant difference.
Results
Characteristics of patients and their
caregivers
From October 2021 to March 2022, 70 patients with
stroke were treated at the Department of Neurology of the
Neuropsychiatry Hospital of Craiova (Craiova, Romania) and were
included in the present study.
The characteristics of the patients are revealed in
Table I. The mean age of patients
was 67.91 (SD, 12.39; range, 32-86) years. Females (41/70; 58.6%)
were slightly more than males and the majority of the patients
(38/70; 54.3%) were married. The most common comorbidities were
hypertension (15.7%) and chronic obstructive pulmonary disease
(15.7%).
 | Table ICharacteristics of the patients
enrolled in the study. |
Table I
Characteristics of the patients
enrolled in the study.
| Demographics | Total no. of
patients (N=70) |
|---|
| Male sex, no.
(%) | 29 (41.4%) |
| Age (years), mean
(SD) and | 67.91 (12.39) |
| median (IQR) | 68.5 (60-79) |
| Marital status | |
|
Married | 38 (54.3%) |
|
Single | 2 (2.9%) |
|
Divorced | 10 (14.3%) |
|
Widowed | 20 (28.6%) |
| Employment
status | |
|
Employed,
no. (%) | 15 (21.4%) |
|
Unemployed,
no. (%) | 14 (20%) |
|
Retired, no.
(%) | 41 (58.6%) |
| Education
level | |
|
Middle
School | 19 (27.1%) |
|
High
School | 46 (65.7%) |
|
College or
University | 5 (7.1%) |
| Environment | |
|
Urban | 37 (52.9%) |
|
Rural | 33 (47.1%) |
| Smoking | |
|
Never | 35 (50%) |
|
Former
smoker | 35 (50%) |
| Obesity | |
|
No
obesity | 47 (67.1%) |
|
I | 19 (27.1%) |
|
II | 4 (5.7%) |
| Familial support,
yes (%) | 46 (65.71%) |
| No. of
comorbidities (%) | |
|
0 | 3 (4.29%) |
|
1 | 63 (90.0%) |
|
2 | 4 (5.71%) |
| Comorbidities | |
|
Hypertension,
no. (%) | 11 (15.7%) |
|
Diabetes,
no. (%) | 9 (12.9%) |
|
Bronchial
asthma, COPD | 11 (15.7%) |
|
Heart
failure | 4 (5.7%) |
|
Glaucoma | 3 (4.2%) |
| TOAST | |
|
Large-artery
atherosclerosis | 15 (21.4%) |
|
Cardioembolism | 11 (15.7%) |
|
Small-vessel
occlusion | 17 (24.3%) |
|
Stroke of
other determined etiology | 17 (24.3%) |
|
Stoke of
undetermined etiology | 10 (14.3%) |
| ADL | 2.80 (0.88%) |
| Barthel index | 32.29 (8.63%) |
The characteristics of the caregivers of the
patients are revealed in Table II.
Their mean age was 50.67 (SD, 12.72; range 25-75) years. Most of
the caregivers were employed (51.4%), female (62.9%), and were the
children of the patients (44.3%).
 | Table IICharacteristics of the caregivers of
stroke patients enrolled in the study. |
Table II
Characteristics of the caregivers of
stroke patients enrolled in the study.
| Demographics | Total no. of
caregivers (N=70) |
|---|
| Male sex, no.
(%) | 26 (37.1%) |
| Age (years), mean
(SD) and median (IQR) | 50.67 (12.72) |
| Type | |
|
Parents | 1 (1.4%) |
|
Brother/sister | 5 (7.1%) |
|
Wife/husband | 23 (32.9%) |
|
Children | 31 (44.3%) |
|
Grandchildren | 10 (14.2%) |
| Employment
status | |
|
Employed,
no. (%) | 36 (51.4%) |
|
Unemployed,
no. (%) | 20 (30%) |
|
Retired, no.
(%) | 13 (18.6%) |
| Level of
education | |
|
Middle
School | 9 (12.9%) |
|
High
School | 42 (60%) |
|
College or
University | 19 (27.1%) |
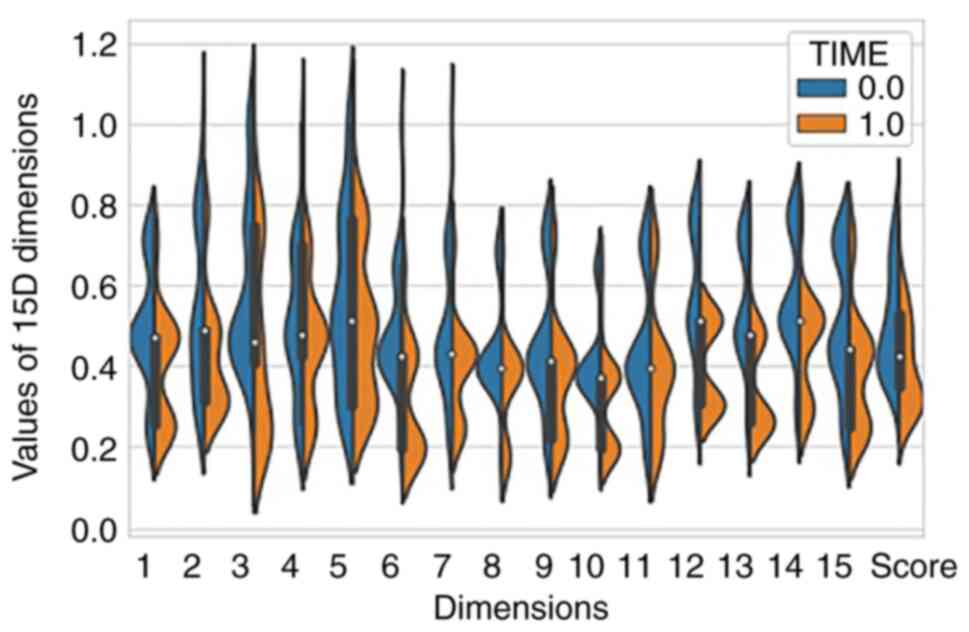
The response rate to the 15D questionnaire was 100%
for both patients and the caregivers of the patients. The
progression of the 15D scores at baseline and the follow-up visit
are revealed in Fig. 1. A
statistically significant decreased HRQoL was observed in the
follow-up visit, after 3 months of home care, than at the end of
the hospitalization period (P<0.0001).
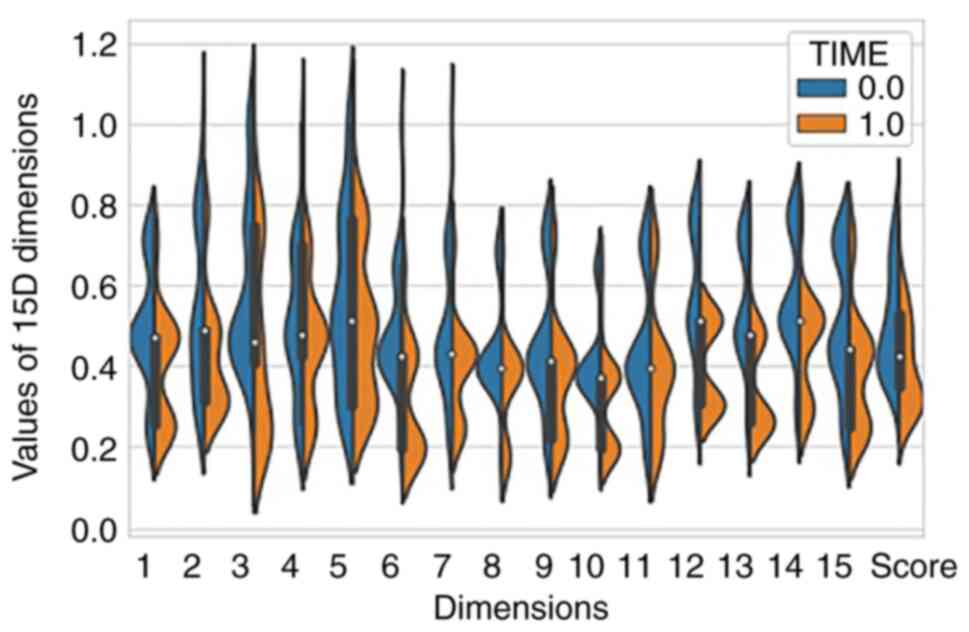 | Figure 1Mean 15D score and health-related
quality of life dimensions for stroke patients before and after
stroke treatment. 1, Mobility; 2, Vision; 3, Hearing; 4, Breathing;
5, Sleeping; 6, Eating; 7, Speech; 8, Excretion; 9, Usual
activities; 10, Mental function; 11, Discomfort and symptoms; 12,
Depression; 13, Distress; 14, Vitality; 15, Sexual activity; Score,
15D Score. Time=0.0 (baseline), at the end of the hospitalization
period; Time=1.0, after 3 months of home care. 15D, 15
dimensions. |
Descriptive data of the HRQoL
The 15D scores of patients with stroke were low at
baseline and further decreased at the follow-up visit, after 3
months (Fig. 1): Mobility
(0.49±0.15 vs. 0.4±0.14), vision (0.55±0.21 vs. 0.42±0.15), hearing
(0.6±0.21 vs. 0.44±0.23), breathing (0.52±0.19 vs. 0.46±0.16),
sleeping (0.57±0.22 vs. 0.5±0.19), eating (0.49±0.16 vs.
0.32±0.14), speech (0.49±0.17 vs. 0.39±0.12), excretion (0.44±0.13
vs. 0.35±0.13), usual activities (0.45±0.16 vs. 0.37±0.15), mental
function (0.41±0.12 vs. 0.29±0.1), discomfort/symptoms (0.45±0.17
vs. 0.39±0.16), depression (0.57±0.17 vs. 0.4±0.1), distress
(0.55±0.16 vs. 0.35±0.11), vitality (0.57±0.15 vs. 0.46±0.13),
sexual activity (0.51±0.17 vs. 0.39±0.15), total 15D score
(0.51±0.13 vs. 0.4±0.12).
All 15 dimensions were statistically lower than
baseline, as revealed in Table
III. The difference regarding the values was >0.015 for all
indicators, thus, the change was also considered clinically
important.
 | Table IIIComparison of the 15D assessment of
stroke patients between two time points (baseline and after 3
months). |
Table III
Comparison of the 15D assessment of
stroke patients between two time points (baseline and after 3
months).
| Dimension | Mean
difference | Standard
deviation | Significance |
|---|
| Mobility | -0,098073 | 0,1142439 | <0.0001 |
| Vision | -0,125993 | 0,1237864 | <0.0001 |
| Hearing | -0,152793 | 0,1158872 | <0.0001 |
| Breathing | -0,058933 | 0,1083690 | <0.0001 |
| Sleeping | -0,066443 | 0,1131272 | <0.0001 |
| Eating | -0,176349 | 0,1107134 | <0.0001 |
| Speech | -0,094429 | 0,1239735 | <0.0001 |
| Excretion | -0,087267 | 0,1196142 | <0.0001 |
| Usual
activities | -0,075794 | 0,1260933 | <0.0001 |
| Mental
function | -0,122897 | 0,1058255 | <0.0001 |
| Discomfort and
symptoms | -0,050396 | 0,1009079 | <0.0001 |
| Depression | -0,164797 | 0,1260221 | <0.0001 |
| Distress | -0,196131 | 0,0989375 | <0.0001 |
| Vitality | -0,116026 | 0,1209333 | <0.0001 |
| Sexual
activity | -0,115749 | 0,1194684 | <0.0001 |
| 15D score | -0,107696 | 0,0373576 | <0.0001 |
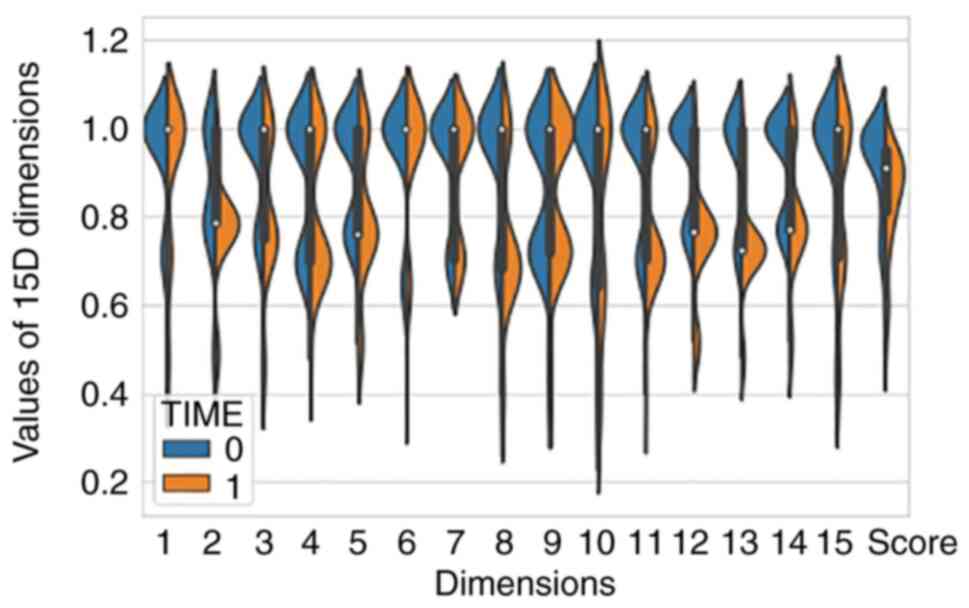
Similarly, the HRQoL was also decreased for the
caregivers of the patients, as revealed in Fig. 2. The 15D scores of the caregivers of
the patients were low at baseline and further decreased after the
follow-up visit that occured 3 months later: Mobility (0.93±0.14
vs. 0.90±0.17), vision (0.86±0.15 vs. 0.77±0.13), hearing
(0.92±0.14 vs. 0.82±0.16), breathing (0.88±0.15 vs. 0.82±0.16),
sleeping (0.90±0.13 vs. 0.80±0.16), eating (0.94±0.13 vs.
0.92±0.16), speech (0.92±0.13 vs. 0.89±0.14), excretion (0.91±0.16
vs. 0.76±0.17), usual activities (0.86±0.16 vs. 0.86±0.16), mental
function (0.91±0.17 vs. 0.81±0.23), discomfort/symptoms (0.91±0.14
vs. 0.80±0.23), depression (0.92±0.11 vs. 0.74±0.13), distress
(0.92±0.13 vs. 0.72±0.11), vitality (0.92±0.11 vs. 0.80±0.14),
sexual activity (0.93±0.16 vs. 0.84±0.19), score total 15D
(0.91±0.11 vs. 0.83±0.12).
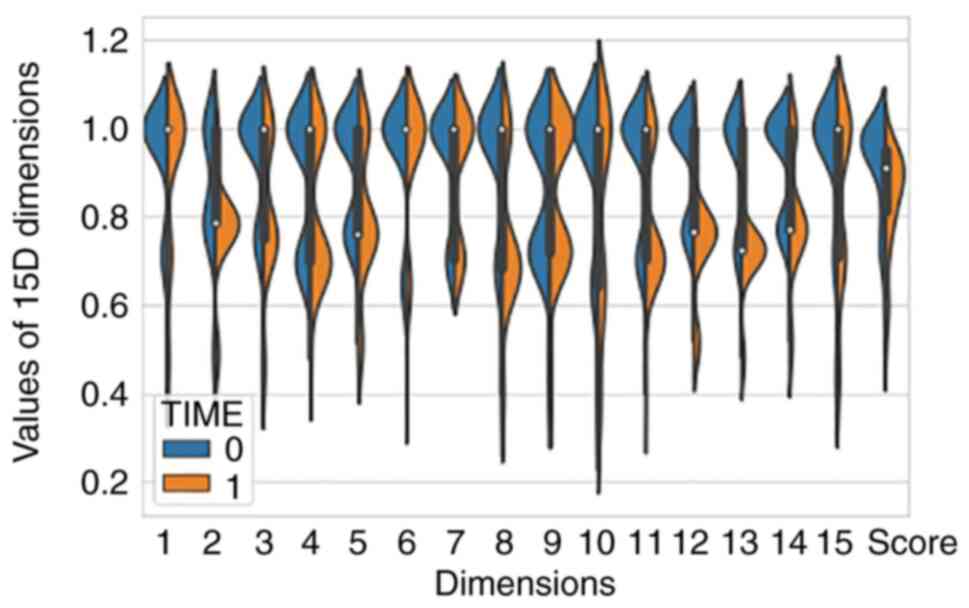 | Figure 2Mean 15D score and health-related
quality of life dimensions for the caregivers of stroke patients at
baseline and follow-up visit. 1, Mobility; 2, Vision; 3, Hearing;
4, Breathing; 5, Sleeping; 6, Eating; 7, Speech; 8, Excretion; 9,
Usual activities; 10, Mental function; 11, Discomfort and symptoms;
12, Depression; 13, Distress; 14, Vitality; 15, Sexual activity;
Score, 15D Score. Time=0 (baseline), at the end of the
hospitalization period; Time=1, after 3 months of home care. 15D,
15 dimensions. |
According to the responses provided in the 15D
assessment, the caregivers of the patients did not declare
significant modifications for mobility and usual activities.
Clinically and statistically significant differences were observed
among the other 13 dimensions and for the total score of the HRQoL,
as presented in Table IV.
 | Table IVComparison of the 15D assessment of
the caregivers of stroke patients between two time points (baseline
and after 3 months). |
Table IV
Comparison of the 15D assessment of
the caregivers of stroke patients between two time points (baseline
and after 3 months).
| Dimension | Mean
difference | Standard
deviation | Significance |
|---|
| Mobility | 0,844640 | 0,1908114 | 0.073 |
| Vision | 0,830527 | 0,1178299 | <0.0001 |
| Hearing | -0,030120 | 0,1094324 | <0.0001 |
| Breathing | -0,089739 | 0,1117594 | <0.0001 |
| Sleeping | -0,098733 | 0,1257868 | <0.0001 |
| Eating | -0,066780 | 0,1242550 | 0.038 |
| Speech | -0,093053 | 0,1183144 | 0.008 |
| Excretion | -0,021434 | 0,0798299 | <0.0001 |
| Usual
activities | -0,029670 | 0,0896527 | <0.0001 |
| Mental
function | -0,152094 | 0,1577240 | <0.0001 |
| Discomfort and
symptoms | 0,000000 | 0,0822726 | <0.0001 |
| Depression | -0,098160 | 0,1527564 | <0.0001 |
| Distress | -0,110663 | 0,1450031 | <0.0001 |
| Vitality | -0,184069 | 0,1010856 | <0.0001 |
| Sexual
activity | -0,197444 | 0,1216742 | <0.0001 |
| 15D score | -,120749 | ,1184799 | <0.0001 |
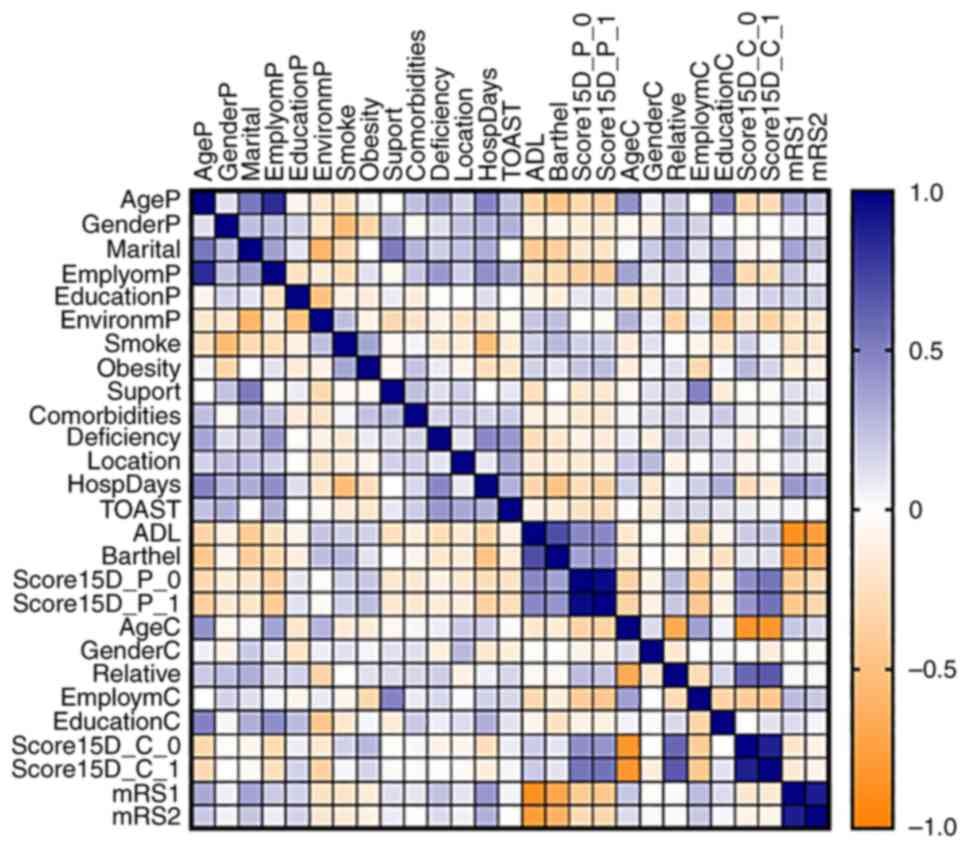
The correlations between all of the assessed factors
and the HRQoL of the patients and their caregivers was evaluated,
and some of the correlations established are revealed in Fig. 3.
At baseline, the HRQoL of the patients was
influenced by age (r=-0.320; P=0.007; the younger survivors had an
improved QoL), employment status (r=-0.368; P=0.002; the lack of
employment decreased the QoL), the number of hospitalization days
(r=-0.288; P=0.016), the ADL (r=0.469; P<0.0001), the Barthel
index (r=0.368; P=0.002), the age of the caregiver (r=-0.356;
P=0.003), the employment status of the caregiver (r=-0.414;
P<0.0001), and the mRS1 (r=-0.423; P<0.0001) (Fig. 3).
After 3 months, during the follow-up visit, the
HRQoL of the patients was influenced by age (r=-0.388; P=0.001; the
younger survivors had an improved QoL), employment status
(r=-0.407; P=0.002; the lack of employment decreased the QoL),
obesity (r=0.259; P=0.031), the number of hospitalization days
(r=-0.365; P=0.002), TOAST (r=-0.264; P=0.027), ADL (r=0.467;
P<0.0001), the Barthel index (r=0.414; P<0.0001), the age of
the caregiver (r=-0.355; P=0.003), the employment status of the
caregiver (r=-0.449; P<0.0001), mRS1 (r=-0.444; P<0.001), and
mRS2 (r=-0.329; P=0.005) (Fig.
3).
At baseline, the HRQoL of the caregivers was
influenced by age (r=-0.335; P=0.005; the younger individuals had
an improved QoL), employment status (r=-0.305; P=0.010; the lack of
employment decreased the QoL), the number of hospitalization days
(r=-0.288; P=0.016), the age of the caregiver (r=-0.840,
P<0.0001), the employment status of the caregiver (r=-0.410;
P<0.0001), the QoL of the patient at baseline (r=0.438;
P<0.0001) and after 3 months (r=0.413; P<0.0001). No
correlation was observed between the HRQoL and mRS of the
caregivers at baseline (r=-0.101; P=0.078) (Fig. 3).
After 3 months, the HRQoL of the patients was
influenced by age (r=-0.293; P=0.014; the younger survivors had an
improved QoL), employment status (r=-0.262; P=0.028; the lack of
employment decreased the QoL), environmental (r=-0.373; P=0.001;
improved QoL for urban life), obesity (r=0.259; P=0.031), the
number of hospitalization days (r=-0.365; P=0.002), the age of the
caregiver (r=-0.827, P<0.0001), the employment status of the
caregiver (r=-0.450, P<0.0001), the QoL of patient at baseline
(r=0.547; P<0.0001) and after 3 months (r=0.552; P<0.0001).
No correlation was identified between the HRQoL and mRS of
caregivers at baseline (r=-0.188; P=0.120) or after 3 months
(r=-0.101; P=0.404) (Fig. 3).
With regard to the decreased HRQoL of the survivors,
ADL was the only factor that significantly influenced it (r=-0.336;
P=0.004), which is logical due to the limitation of daily living
activities and social interaction. Among caregivers, the intensity
of their HRQoL decrease was significantly correlated with their age
(r=-0.265; P=0.027), sex (r=-0.239; P=0.046; females had a worse
QoL than males), initial QoL of the patient (r=0.444; P<0.0001)
and post 3-month QoL (r=0.493, P<0.0001) (Fig. 3).
Given the number of significantly influencing
factors, multiple linear regression was performed. ADL (P=0.014)
and QoL after 3 months (P=0.043) were the factors most
significantly correlated to the decreased HRQoL of the survivors
and to the decreased HRQoL of the caregivers (Fig. 3).
Following examination of the influence of lesion
location on the scores for the QoL of patients, a significant
difference across categories was not identified. In the present
study, stroke location was not associated with the magnitude of the
decreased QoL of patients (Table
V). A possible explanation for this result is the low number of
patients included in this study. Further study on a large cohort is
required in order to establish which location is strongly
associated with QoL in stroke survivors. Furthermore, these
findings can be partially explained by the delay in the post-stroke
intervention due to delayed presentation to emergency care during
the pandemic period.
 | Table VAssociation between stroke location
and QoL. |
Table V
Association between stroke location
and QoL.
| | Location of the
stroke | |
|---|
| Difference in
scores for QoL for stroke patients | Right (n=26) | Left (n=26) | Basal (n=18) | P-value |
|---|
| Mean ± SD | -0.103±0.026 | -0.116±0.05 | -0.1±0.028 | 0.727 |
| Median (IQR) | -0.1 (-0.12 to
-0.08) | -0.11 (-0.15 to
-0.07) | -0.09 (-0.13 to
-0.09) | |
Discussion
The present study investigated for the first time,
the impairment in QoL among patients who suffered stroke and their
caregivers in a single center located in Romania during the
COVID-19 pandemic, after a three-month post-stroke period, without
any intervention to support the transition from hospital to home.
For this purpose, demographic variables, the 15D assessment tool,
TOAST, ADL, Barthel index and discharge mRS score, that were
studied separately in the literature, were used, without
comparative evaluation before and during the COVID-19 pandemic
(20-23).
Muresanu et al highlighted the significant
decrease in hospital discharges in Romania among patients who
suffered stroke during the COVID-19 pandemic (21). The pandemic led to global chaos,
particularly in the healthcare system where it caused sudden
interruptions in the provision of healthcare to all patients across
the country, induced by the relocation of workforces from
healthcare facilities to treating patients with COVID-19(24) or by the panic instilled in the
population that led to a decrease in trust in the medical act with
a therapeutic (25) or preventive
purpose such as vaccination (23).
The number of non-COVID-19 acute emergency cases decreased, a fact
reflected by the low number of emergency presentations and the
number of CT scans performed (25,26).
Moreover, a negative impact of COVID-19 was identified in patients
who had risk factors for diseases or already suffered from
life-threatening diseases such as stroke, with some hesitation from
the patient to initially visit a doctor due to the associated risk
of exposure to the virus (27,28).
The present study revealed that the HRQoL of
survivors and their caregivers was decreased. The stroke survivors
and their family proxies modestly agreed to undergo assessment of
QoL following a stroke, as well as functionality assessment at 1 to
2 months post-stroke (29). In the
present study, at baseline and after 3 months, the HRQoL of
survivors was influenced by age, employment status, number of
hospitalization days, ADL, Barthel index, and age as well as
employment status of the caregiver. Younger survivors had improved
QoL and the lack of employment decreased it. Obesity and TOAST
influenced HRQoL after 3 months.
In addition, at baseline and after 3 months, the
HRQoL of the caregiver was influenced by age, employment status,
ADL, Barthel index, and their employment status. Life satisfaction
of family caregivers was associated with feelings and emotions of
the patients only. It was strongly linked with the four WHOQOL-BREF
domains (physical health, psychological health, environment, and
social relationships) of the caregiver (30). Strong psychological repercussions
may be generated for both patients and family caregivers (31). The family proxy rated QoL worse than
stroke survivors rated that domain, however, the rates were similar
in more objective domains such as physical functioning but not
analogous in more subjective domains such as mood. What is
difficult to determine is whether the patient or the proxy is
closer to the ‘truth’. For example, depressed patients report a
lower HRQoL and these scores are more consistent with proxy HRQoL
ratings, but whether the reported lower HRQoL of the patient is
accurate or whether it is lower than their ‘actual’ HRQoL,
resulting from the overlying depression, is not clear.
The findings of the present study are not consistent
with those of a previous study regarding sex differences in HRQoL
in patients who suffered stroke, where it was reported that females
had a lower QoL than males (32).
Worse HRQoL in female patients with stroke was not identified and
the interventions including those increasing rehabilitation efforts
could be assessed in the future regardless of sex in Romania.
A previous study identified differences in the
levels HRQoL with regard to employment status. Unlike individuals
at home with no activity and despite their handicap, stoke patients
who are retired may have less stress or unhappiness and may
maintain a social position/identity, which is based not only on age
and social characteristics but also on the sense of self of the
individual (33). As expected, it
was demonstrated that, both at baseline and after 3 months of home
post-stroke stay, the lack of employment decreased HRQoL.
In the present study, the length of hospitalization
and mRS at discharge were negatively correlated with HRQoL and the
tendency towards depressive mood was likely to influence the HRQoL,
concurrently as the other assessed dimensions including mobility,
usual activities, mental function, distress, or sexual activity.
The same results were detected by Pedersen et al for
post-stroke Scandinavian patients (33).
Following the pandemic period, significant changes
in the QoL of patients were reported, including stroke survivors.
In a previous study, a significant decrease in stroke
hospitalization time was reported during and after
Covid-19(34). This had a high
impact on the outcome of the disease as well as on the QoL of
patients and their caregivers.
During Covid-19, an increased number of cases with
clinical signs of severe and moderate stroke were recorded.
According to the American Heart Association, patients with Covid-19
are more exposed to stroke by a different mechanism than
atherosclerosis (35). As a result,
this can change the impact of the disease and requires further
investigation in order to identify pre- and post-Covid 19 changes
in the QoL-related stroke pattern. The delay of thrombolytic
therapy for patients who have suffered a stroke has a high impact
on post-stroke recovery and functional outcome. It is associated
with long term disability and increased healthcare costs.
Notably, a recent study reported an increased risk
of stroke in middle-aged individuals, independent of age (35). In the post-Covid-19 era, the
consequences of the pandemic have to be carefully monitored
(36). The QoL of caregivers is an
important topic to be addressed. The post-Covid-19 public health
policy has to be wary of the impact of Covid-19 on both stroke
survivors and their caregivers.
The present study had several limitations. The
statistical assessment of QoL in a relatively small population
during the pandemic was extremely difficult, as outliers can alter
the results. The trend that was identified in the present study,
should be further validated on large cohorts in a multicentric
clinical study. Thus, the results are consistent, but some other
covariates could influence the QoL, including medication adherence
or fatigue, assessed by evaluating post-stroke QoL (37). In order to quantify the HRQoL, a
valid tool for the Romanian population is required, based on a
precise and valid measurement algorithm for stroke patients. There
is still a lack of tools for the assessment of HRQoL in stroke
patients in Romania, and this difficulty must be resolved in the
future.
The aim of the present study was to identify the
multidimensional effects of post-stroke HRQoL among patients and
caregivers, in order to propose and implement suitable intervention
approaches, to support the transition from hospital to home after
stroke, in Romania (36-38).
In conclusion, HRQoL is an important issue to be
addressed in the multimodal management of stroke survivors
following the acute period. As revealed in the present study, the
HRQoL of post-stroke patients and their caregivers was decreased in
a significant clinical percentage, in Romania. The aim of the
present study was to raise awareness on this issue, identifying
certain important key factors with direct consequences on the HRQoL
of stroke survivors and their caregivers. The clinical reduction of
the QoL of both patients and their caregivers was observed during
the pandemic, and changes in health policies in Romania are
warranted regarding this issue, particularly in a pandemic.
Acknowledgements
Professor Harri Sintonen from the University of
Helsinki, Finland is the developer of the 15D instrument and
obtains royalties from its electronic versions.
Funding
Funding: This research was funded by the University of Medicine
and Pharmacy of Craiova (grant no. 26/531/4/31.05.2022).
Availability of data and materials
The datasets used during the present study are
available from the corresponding author upon reasonable
request.
Authors' contributions
VP, CVA, AMB, DCC, RP, VB, MMF, MSS and ATS equally
contributed to the acquisition, analysis and systematization of
data, manuscript writing and critical revision for its important
intellectual content. VP and RP confirm the authenticity of all the
raw data. All authors read and approved the final version of the
manuscript.
Ethics approval and consent to
participate
The present study was performed in line with the
principles of the Declaration of Helsinki. Ethical approval
(Registration no. 156/2021) was obtained from the Academic and
Scientific Ethics and Deontology Committee of the University of
Medicine and Pharmacy of Craiova (Craiova, Romania). Informed
consent was obtained from all participants involved in the
study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Murray CJL, Vos T, Lozano R, Naghavi M,
Flaxman AD, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S,
et al: Disability-adjusted life years (DALYs) for 291 diseases and
injuries in 21 regions, 1990-2010: A systematic analysis for the
global burden of disease study 2010. Lancet. 380:2197–2223.
2012.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Albu CV, Padureanu V, Boldeanu MV, Bumbea
AM, Enescu AS, Albulescu DM, Silosi CA and Enescu A: Vascular
neurocognitive disorders and the vascular risk factors. J Mind Med
Sci. 5:7–15. 2018.
|
|
3
|
Lozano R, Naghavi M, Foreman K, Lim S,
Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R, Ahn SY, et
al: Global and regional mortality from 235 causes of death for 20
age groups in 1990 and 2010: A systematic analysis for the global
burden of disease study 2010. Lancet. 380:2095–2128.
2012.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Gill TM and Feinstein AR: A critical
appraisal of the quality of quality-of-life measurements. JAMA.
272:619–626. 1994.PubMed/NCBI
|
|
5
|
Hopman WM and Verner J: Quality of life
during and after inpatient stroke rehabilitation. Stroke.
34:801–805. 2003.PubMed/NCBI View Article : Google Scholar
|
|
6
|
White JH, Alston MK, Marquez JL,
Sweetapple AL, Pollack MR, Attia J, Levi CR, Sturm J and Whyte S:
Community-dwelling stroke survivors: Function is not the whole
story with quality of life. Arch Phys Med Rehabil. 88:1140–1146.
2007.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Howard G, Safford MM, Meschia JF, Moy CS,
Howard VJ, Pulley L, Gomez CR and Crowther M: Stroke symptoms in
individuals reporting no prior stroke or transient ischemic attack
are associated with a decrease in indices of mental and physical
functioning. Stroke. 38:2446–2452. 2007.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Howard VJ, McClure LA, Meschia JF, Pulley
L, Orr SC and Friday GH: High prevalence of stroke symptoms among
persons without a diagnosis of stroke or transient ischemic attack
in a general population: The REasons for geographic and racial
differences in stroke (REGARDS) study. Arch Intern Med.
166:1952–1958. 2006.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Kleindorfer D, Judd S, Howard VJ, McClure
L, Safford MM, Cushman M, Rhodes D and Howard G: Self-reported
stroke symptoms without a prior diagnosis of stroke or transient
ischemic attack: A powerful new risk factor for stroke. Stroke.
42:3122–3126. 2011.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Wu QE, Zhou AM, Han YP, Liu YM, Yang Y,
Wang XM and Shi X: Poststroke depression and risk of recurrent
stroke: A meta-analysis of prospective studies. Medicine
(Baltimore). 98(e17235)2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Cojocaru GR, Popa-Wagner A, Stanciulescu
EC, Babadan L and Buga AM: Post-stroke depression and the aging
brain. J Mol Psychiatry. 1(14)2013.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Boudokhane S, Migaou H, Kalai A, Jellad A,
Borgi O, Bouden A, Sriha Belguith A and Ben Salah Frih Z:
Predictors of quality of life in stroke survivors: A 1-year
follow-up study of a tunisian sample. J Stroke Cerebrovasc Dis.
30(105600)2021.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Wang C, Wang Z, Wang G, Lau JY, Zhang K
and Li W: COVID-19 in early 2021: Current status and looking
forward. Signal Transduct Target Ther. 6(114)2021.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Kissler SM, Tedijanto C, Goldstein E, Grad
YH and Lipsitch M: Projecting the transmission dynamics of
SARS-CoV-2 through the postpandemic period. Science. 368:860–868.
2020.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Lindblom S, Tistad M, Flink M, Laska AC,
von Koch L and Ytterberg C: Referral-based transition to subsequent
rehabilitation at home after stroke: One-year outcomes and use of
healthcare services. BMC Health Serv Res. 22(594)2022.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Adams HP Jr, Bendixen BH, Kappelle LJ,
Biller J, Love BB, Gordon DL and Marsh EE III: Classification of
subtype of acute ischemic stroke. Definitions for use in a
multicenter clinical trial. TOAST. Trial of Org 10172 in acute
stroke treatment. Stroke. 24:35–41. 1993.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Subtirelu MS, Turcu-Stiolica A and
Sintonen H: PMU133 translation and cultural adaptation of 15D
quality of life questionnaire from English to Romanian language.
Value Health. 22(S731)2019.
|
|
18
|
Turcu-Stiolica A, Subtirelu MS and Bumbea
AM: Can incobotulinumtoxin-A treatment improve quality of life
better than conventional therapy in spastic muscle post-stroke
patients? Results from a pilot study from a single center. Brain
Sci. 11(934)2021.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Turcu-Stiolica A, Subtirelu MS and Bumbea
AM: Cost-utility analysis of incobotulinumtoxin-A compared with
conventional therapy in the management of post-stroke spasticity in
Romania. Front Pharmacol. 10(1516)2020.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Hayati F, Lah NASN, Zakaria AD, Rahim SSSA
and Azizan N: Issues and impact of COVID-19 on surgical services in
Northern Borneo, Sabah. BJMS. 16:1–4. 2022.
|
|
21
|
Muresanu DF, Strilciuc S, Lorenzovici L,
Sófalvi A and Grad D: COVID-19 indirectly hits stroke patients, as
hospital discharges in Romania see a dramatic decrease during the
pandemic. Eur J Neurol. 28 (Suppl 1)(S757)2021.
|
|
22
|
Grad DA, Chereches RM, Strilciuc S and
Muresanu D: Scars of stroke care emerge as COVID-19 shifts to an
endemic in many countries. J Med Life. 15:589–591. 2022.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Mărcău FC, Purec S and Niculescu G: Study
on the refusal of vaccination against covid-19 in Romania. Vaccines
(Basel). 10(261)2022.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Mărcău FC, Peptan C, Nedelcuță RM, Băleanu
VD, Băleanu AR and Niculescu B: Parental COVID-19 vaccine hesitancy
for children in Romania: National survey. Vaccines (Basel).
10(547)2022.PubMed/NCBI View Article : Google Scholar
|
|
25
|
O'Brien CM, Jung K, Dang W, Jang HJ and
Kielar AZ: Collateral damage: The impact of the covid-19 pandemic
on acute abdominal emergency presentations. J Am Coll Radiol.
17:1443–1449. 2020.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Nodora JN, Gupta S, Howard N, Motadel K,
Propst T, Rodriguez J, Schultz J, Velasquez S, Castañeda SF, Rabin
B and Martínez ME: The COVID-19 pandemic: Identifying adaptive
solutions for colorectal cancer screening in underserved
communities. J Natl Cancer Inst. 113:962–968. 2021.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Baumann M, Le Bihan E, Chau K and Chau N:
Associations between quality of life and socioeconomic factors,
functional impairments and dissatisfaction with received
information and home-care services among survivors living at home
two years after stroke onset. BMC Neurol. 14(92)2014.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Alanne S, Roine RP, Räsänen P, Vainiola T
and Sintonen H: Estimating the minimum important change in the 15D
scores. Qual Life Res. 24:599–606. 2015.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Williams LS, Bakas T, Brizendine E, Plue
L, Tu W, Hendrie H and Kroenke K: How valid are family proxy
assessments of stroke patients' health-related quality of life?
Stroke. 37:2081–2085. 2006.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Cardoso AL, Silva-Junior GO, Bastos LF,
Cesar ALM, Serrano LG, Dziedzic A and Picciani BLS: Preliminary
assessment of the quality of life and daily burden of caregivers of
persons with special needs: A questionnaire-based, cross-sectional
survey. Int J Environ Res Public Health. 20(2012)2023.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Gargano JW and Reeves MJ: Paul Coverdell
National Acute Stroke Registry Michigan Prototype Investigators.
Sex differences in stroke recovery and stroke-specific quality of
life: Results from a statewide stroke registry. Stroke.
38:2541–2548. 2007.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Minichiello V, Browne J and Kendig H:
Perceptions and consequences of ageism: Views of older people.
Ageing Soc. 20:253–278. 2000.
|
|
33
|
Pedersen SG, Friborg O, Heiberg GA,
Arntzen C, Stabel HH, Thrane G, Nielsen JF and Anke A:
Stroke-specific quality of life one-year post-stroke in two
Scandinavian country-regions with different organisation of
rehabilitation services: A prospective study. Disabil Rehabil.
43:3810–3820. 2021.PubMed/NCBI View Article : Google Scholar
|
|
34
|
De Bruijn MAAM, Synhaeve NE, van
Rijsbergen MWA, de Leeuw FE, Mark RE, Jansen BPW and de Kort PL:
Quality of life after young ischemic stroke of mild severity is
mainly influenced by psychological factors. J Stroke Cerebrovasc
Dis. 24:2183–2188. 2015.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Yang Q, Tong X, Coleman King S, Olivari BS
and Merritt RK: Stroke hospitalizations before and during COVID-19
pandemic among medicare beneficiaries in the United States. Stroke.
52:3586–3601. 2021.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Shakil SS, Emmons-Bell S, Rutan C, Walchok
J, Navi B, Sharma R, Sheth K, Roth GA and Elkind MSV: Stroke among
patients hospitalized with COVID-19: Results from the american
heart association COVID-19 cardiovascular disease registry. Stroke.
53:800–807. 2022.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Coman AE, Ceasovschih A, Petroaie AD, Popa
E, Lionte C, Bologa C, Haliga RE, Cosmescu A, Slănină AM, Bacușcă
AI, et al: The significance of low magnesium levels in COVID-19
patients. Medicina (Kaunas). 59(279)2023.PubMed/NCBI View Article : Google Scholar
|
|
38
|
O'Callaghan G, Fahy M, Murphy P, Langhorne
P, Galvin R and Horgan F: Effectiveness of interventions to support
the transition home after acute stroke: A systematic review and
meta-analysis. BMC Health Serv Res. 22(1095)2022.PubMed/NCBI View Article : Google Scholar
|