Introduction
Bone augmentation has taken different forms over
time, depending partly on the experience of the surgeon but also on
the available bone of the patient. Following tooth extraction, bone
resorption from the jawbone occurs within 12 months (1,2). Most
of this resorption happens in the first 6 months, with the
literature reporting loss of >40% of the height and 60% of the
thickness of the alveolar process during this period (3-5).
Horizontally, the size of the edentulous ridge is reduced by 5-7 mm
and implant insertion become difficult (6). To compensate for this loss, various
methods of managing the remaining bone tissue and augmentation have
been proposed. Guided bone regeneration (GBR) with titanium mesh,
resorbable or non-resorbable membranes, the ridge-split (RS)
technique, addition of autologous onlay bone block grafts, use of
narrow implants and, lately, ridge expansion via osseodensification
(OD) are methods used to preserve and enhance the available bone
(7). The present review proposed
the evaluation and comparison of three horizontal ridge
augmentation techniques. Ridge expansion via OD, introduced by
Huwais in 2013(8), allows bone
density to be increased by using specially designed burs to
increase the primary stability of implants and placing them in
areas of low density (D3, D4) (9).
The force pushing the bone tissue, increasing its density, creates
a plastic deformation and causes expansion of the alveolar process
and an increase of the horizontal dimension of the alveolar ridge
(10). GBR uses bone particles of
different origin which, together with a resorbable or
non-resorbable membrane, promote the migration of osteoprogenitor
cells and bone tissue neoformation at the sites of bone defects
(11). The RS technique aims to
increase the width of the alveolar bone by using the viscoelastic
properties of the medullary bone in order to create space for the
insertion of implants, the remaining space being filled with
biomaterials or bone grafts of different origin (3). Considering the recent emergence of
ridge expansion via OD, reviews and meta-analyses related to the
ability of the technique to induce expansion of the alveolar
process horizontally have not been published thus far, most studies
addressing the technique with reference to different variables
related to the increase in bone density. A meta-analysis published
in February 2021(2) examined the
bone area fraction occupancy, the moment of force at implant
insertion and the primary stability of the implants reported in
various publications. Few studies present complete data on the
dimensions of the alveolar ridge in a horizontal direction before
treatment and the immediate postoperative bone gain. Regarding the
RS technique, a meta-analysis conducted in 2017(3) identified data related to the
horizontal dimensions of the ridge before and after implant
placement. Thus, as with GBR, the survival rate of implants is
>95%, and complications are rare (7%) (4). A number of studies (12-15)
have been published related to bone gain and the choice of membrane
and graft for GBR, the literature concluding that titanium mesh and
autologous grafts have the highest predictability in regenerating
bone tissue from the defect (5).
The ridge width required to insert an implant represents the actual
width of the implants chosen according to different factors (of
which the location of the edentation and the available bone would
be among the most important) plus 3 mm equally divided in the
vestibular and oral areas relative to the location of the implant
(6). The present systematic review
aimed to determine the amount of the horizontal increase of the
alveolar ridge depending on the method (the primary variable), the
basal dimensions of the edentulous ridge for each technique and the
survival rate of implants inserted (secondary variables) and other
factors that may influence these results.
Materials and methods
PICO process design
The PICO question (population, intervention,
comparison, outcome) was formulated as follows: ‘How much does the
horizontal dimension of the edentulous ridge increase by use of
different surgical methods?’ The population was represented by
patients that require oral rehabilitation with dental implant
surgery in areas with insufficient horizontal bone, the
intervention horizontal ridge augmentation and the comparison was
made between the three surgical techniques described, while the
outcome is the amount of bone gain following the ridge expansion or
augmentation.
Search strategy
Selection of the articles was performed in
compliance with the Preferred Reporting Items for Systematic
reviews and Meta-Analyses (PRISMA) model from the following
electronic databases: PubMed-Medline, Cochrane Central Register of
Controlled Trials, EMBASE, Cochrane Oral Health Group Trials
Register and Web of Science, and from various publications and
specialized journals (Journal of Craniofacial Surgery, Compendium
of Continuous Education in Dentistry and International Journal of
Dentistry) to identify articles from between January 2017 and June
2022. The following keywords and MeSH terms (mh) were used in the
online search: ‘osseodensification’ OR ‘Densah bur’ OR ‘Versah’ OR
‘bone densification’ OR ‘narrow ridge’ OR ‘guided bone
regeneration’ OR ‘guided tissue regeneration’ OR ‘ridge-split’ OR
‘horizontal augmentation’ OR ‘split crest’ OR ‘bone split’ OR
‘ridge expansion’ OR ‘bone condensation’ OR ‘horizontal expansion’
OR ‘bone graft’ (mh) AND ‘dental implants’ (mh), ‘dental
implantation’ NOT ‘animals’ (mh). The terms used in the search were
connected via AND, NOT and OR Boolean operators.
Eligibility criteria
Studies were included in the present systematic
review if they met the following criteria: They were prospective or
retrospective, with or without a control, and they present data
related to lateral ridge augmentation by one of the three
techniques to be compared: Ridge expansion via OD, GBR and RS. The
articles were published between January 2017 and December 2022. The
5-year period was chosen due to the recent advent of the OD
technique for which the first clinical trials were published in
PubMed-Medline in the early 2018. On the other hand, studies that
were not published in English, those with <10 subjects, articles
that did not accurately present the edentulous ridge dimensions
prior to surgery or the increase of the post-intervention ridge
dimensions, studies that did not present the follow-up of the cases
of bone augmentation for ≥6 weeks following the insertion of the
implants and the types of graft (for GBR or RS), preliminary
studies, surgical guidelines, animal studies, reviews and records
that do not report sufficient data on the methodology used were
eliminated. From the studies included in the present review, the
following data were selected: Number of patients, number of
implants, location of inserted implants, bone augmentation
technique, survival rate of the implants, moment of force at the
insertion of the implants, primary stability and, in particular,
dimensions of the edentulous ridge at the beginning of the
treatment and the difference between the initial and final
width.
Reviewers
The present review was conducted by two reviewers
(AV and SD), following the PRISMA and Strengthening the reporting
of observational studies in epidemiology (STROBE) guidelines. The
searches were conducted electronically and manually, being verified
by three individuals (AV, SD and AP) and EndNote X9 software was
used for the organization of references and the elimination of the
duplicates and the studies published before 2017.
Analysis of the quality of
studies
Non-randomized studies were evaluated using the
Methodological Index for Non-randomized Studies (MINORS) modified
by Slim et al (16). This
method of assessing the quality of studies requires the allocation
of scores between 0-24 for controlled studies and between 0-6 for
those without a control by completing an evaluation report composed
of 12 questions; the answer to each of them was quantified as 0, 1
or 2 points. This assessment has been proposed for the evaluation
of studies related to surgical techniques and can be applied to
prospective, retrospective, non-randomized, controlled or
uncontrolled studies. Through this system, the following parameters
are taken into account: Clarity of the study objective, inclusion
of all available patients, rigor of data collection, conclusion in
accordance with the study objective, lack of subjectivity in
determining the conclusions, observation of cases in relation to
the study objective, <5% of patients lost after the initial
intervention and statistical analysis performed correctly, with a
confidence interval (CI) of 95%. In the case of prospective
randomized and controlled studies, the Cochrane Collaboration's
Tool for Assessing the Risk of Bias in Randomized Trials (CCRBT)
(17) was used, consisting of six
evaluation criteria: Random sequence generation, allocation
concealment, blinding of participants and personnel, blinding of
outcome assessment, incomplete outcome data, selective reporting
and other bias. Depending on these parameters, the study would have
a high, medium or low risk of bias.
Statistical analysis
The program used to perform the statistical
calculations was Comprehensive Meta-Analysis V3 (Biostat). The main
variables used in the meta-analysis were the reported bone
horizontal increase of the alveolar ridge, while the initial ridge
size and the implant survival rate were considered secondary
variables. Bone size statistics were compiled by reference to the
number of patients and survival rate calculated relative to the
number of implants. The means reported in 17 out of 18 articles and
their standard deviations for bone sizes were used, and the
survival of the implants was considered as percentage. The final
bone gain, mean of the initial ridge width and the survival rate of
the implants were assessed using a random effect model. If the
study had a control group in which patients benefited from the same
method of increasing the horizontal size of the ridge or a
comparison was included in their design with respect to the factors
on which that technique depends (e.g. type of membrane in the case
of GBR) with regard to two or more different groups as a
population, the respective study was divided according to the
number of groups, each of which was considered an independent study
in the meta-analysis. In the cases where several horizontal
dimensions were recorded depending on the measurement method,
first, the means of the clinical dimensions comprising the entire
proposed sample were taken into account and, second, those measured
with the bone calipers were preferred. Moreover, if measurements
were made at several points relative to the vertical height of the
bone (e.g., 1 or 4 mm from the top of the ridge), the smallest
dimension was taken into account in the case of the initial width
of the ridge, and the largest in the case of the final bone gain
(3). Otherwise, only values that
were recorded at a maximum of 5 mm from the top of the ridge were
accepted for statistical analysis, but all the values recorded by
the authors appear in the table in the results part of the
systematic review. The meta-regression was achieved by reference to
the augmentation technique (moderator factor) and to the type of
bone graft. This meta-analysis intended to determine a
statistically significant dependence between surgical techniques
and the final bone gain or the initial ridge dimension. Regarding
the bone substitute, an analysis was performed related to the
increase in horizontal size and the type of bone graft used, which
is the secondary moderator factor in this case. The statistical
calculation was based on the inverse-variance method proposed by
DerSimonian and Laird and the method of moments proposed by Pearson
which approximates the variation between the studies and the
distribution of the studied population.
Heterogeneity study
The value of the statistical indices I2,
Q and τ2 was calculated; these assess the variance
between the studies and the degree of heterogeneity. To assess the
risk of bias, funnel plots and Egger's regression test were used
for the initial size and the increase in the size of the ridge,
where the P-value for which statistical significance was reported
was 0.05. The strategies used for dealing with a high degree of
heterogeneity were: Usage of a random-effects model, subgroup
analysis and meta-regression. High heterogeneity is very often
reported in the studies that take into account the precise amount
of bone gain (3,7,11,18,19),
different factors such as the various approaches regarding the
ridge rehabilitation (including type of bone graft used, type of
membrane used, patients' illnesses and comorbidities and the timing
of implant placement) or the parameters of the included studies can
render the exact sources of heterogeneity very difficult to
identify.
Results
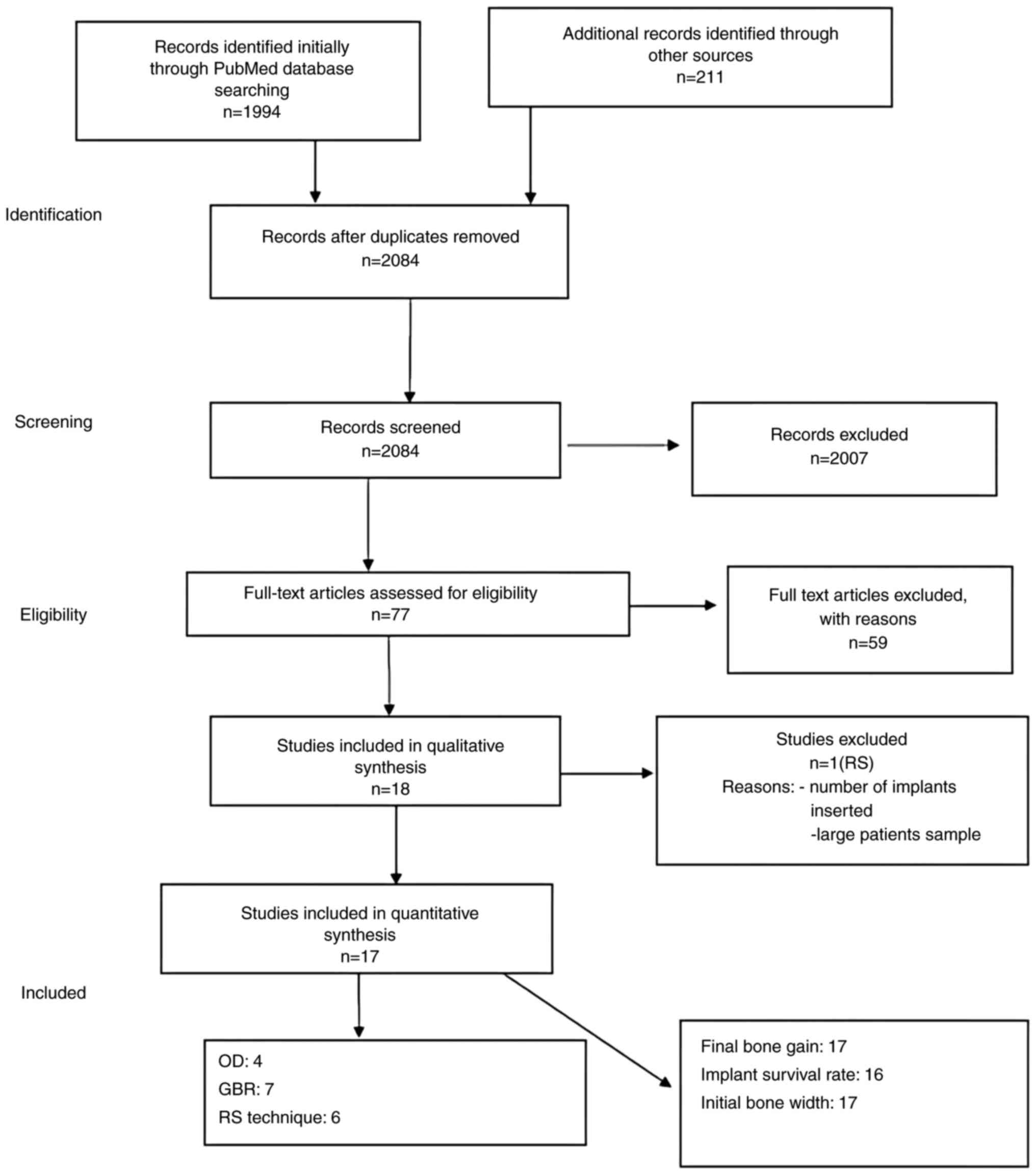
Selection of studies
The initial search resulted in the identification of
2,205 studies, 121 of which were duplicates. After reading the
titles and abstracts, 516 publications were selected. Of these, 77
studies were further evaluated, with the remaining 439 not meeting
the set inclusion criteria. For studies that appeared to meet the
criteria or those for which it was not possible to obtain
sufficient data after reading the titles and abstracts, the entire
article was evaluated. In the case of studies where certain data
not considered under the eligibility criteria were missing (e.g.
number of implants), the authors of these studies were contacted to
obtain them. Discrepancies between the authors of the present
review were managed through discussions and consultation, the
agreement between the authors being materialized by a kappa
coefficient (Cohen) of 0.96, which indicates a high degree of
consensus between them. Finally, 18 studies were included in this
review (Fig. 1), 17 of them being
considered for the meta-analysis. The article that was included in
the review, but not in the meta-analysis, did not specify the
number of implants inserted, having also a much larger sample
compared to the other studies selected (562). For the calculations
related to the initial size of edentulous ridges and the difference
between their final and initial widths, all 17 studies were
included; however, only 16 were used for the implant survival
rate.
Characteristics of the selected
studies
The data collected from the included studies are
presented in Table I. The 18
studies were divided as follows: Four studies on ridge expansion
using Densah burs (20-23),
seven studies on the RS technique (24-30)
and seven studies on GBR (31-37).
Complications and accidents were reported in eight studies
(26,27,30-35)
related to GBR and the RS technique. In five studies (31-35)
on GBR, the most common complication was dehiscence with exposure
of the membrane. This exposure did not always lead to the failure
of the technique being, however, one of the reasons why GBR does
not have the maximum success rate. The prevalence of membrane
exposure in reported cases was 20%, a percentage relative to the
number of patients. Other complications related to GBR were oedema
(9.52%), hematoma (3.8%) and peri-implant mucositis (0.9%). In the
three studies (26,27,30)
where the RS technique was practiced, dehiscence in the augmented
area was the most common complication (12.3%), followed by local
paresthesia (7.69%) and oedema (6.15%).
 | Table ICharacteristics of the included
studies. |
Table I
Characteristics of the included
studies.
| First author/s,
year | Study type | Number of
patients/grafted sites | Location of grafted
site | Surgical
procedure | Bone graft | Initial bone width
(median ± standard deviation in mm) | Final bone gain
(median ± standard deviation in mm) | Measurement
methods | Follow-up of
implants | Implant insertion
moment | Number of
implants | Implant success
rate (%) | Torque primary
stabilityisq (Ncm) | Implant dimensions
(mm) | Accidents and
complications | (Refs) |
|---|
| Koutouzis et
al, 2019 | Retrospective | 28 | Mx. Mnd.
Ant.+Post. | OD | Alp.a | 3.55± 0.46
mm(d0) 7.66± 1.41 mm (d10) 5.37± 0.43 mm
(d0) 7.58± 0.73 mm (d10) 7.07± 0.53 mm
(d0) 8.14± 1.67 mm (d10) | 2.83± 0.66 mm
(d0) 1± 0.7 mm (d10) 1.95± 0.97 mm
(d0) 0.8± 0.9 mm (d10) 1.1± 0.89 mm
(d0) 1.14± 1.06 mm (d10) | Caliper | 1.5 months | Immediate | 28 | 92.8% | 61.26±13.9
75.3±3.88 | N/A | N/A | (20) |
| | | 9 | | | | | | | | | | | | | | |
| | | 12 | | | | | | | | | | | | | | |
| | | 7 | | | | | | | | | | | | | | |
| Agha et al,
2019 | Prospective | 20 | Mx. Ant. | OD | - | 4.37± 0.58 mm | 2.36± 0.31 mm | CBCT | 4 months | Immediate | 14 | 100% | N/A | N/A | N/A | (21) |
| Jarikian et
al, 2021 | Prospective | 11 | Mnd. Post. | OD | - | 4.5±0.5 mm | 1.29± 0.41 mm | Probe | 4 months | Immediate | 40 | 100% | N/A 73.73±2.85 | N/A | N/A | (22) |
| Salman et
al, 2022 | Prospective | 23 | N/A | OD | N/Aa | 4.04± 0.7 mm | 2.35± 0.64 mm | CBCT | 6 months | Immediate | 20 | 100% | 25-49 | N/A | N/A | (23) |
| Gultekin et
al, 2017 | Retrospective | 21(39) | Mx. Mnd. Ant.
Post. | GBR | Aug. (Aug.) | 3.29± 0.87 mm | 5.31± 1.23 mm | CBCT | 1.5-3 years | 4 months | 78 | 100% | 20 | N/A | Membrane exposure
(1/21) | (31) |
| Halperin et
al, 2018 | RCT | 28 | N/A | GBR | Alg. | 3.84± 1.25 mm
(d1) 6.04± 2.03 (d4) | 1.89± 1.53 mm
(d1) 2.27± 1.69 mm (d4) | CBCT/caliper | 6 months | 6 months | 28 | N/A | N/A | N/A | Membrane exposure
(15/28) | (32) |
| Meloni et
al, 2019 | Prospective | 18/22 | Mnd. Mx. .
Post | GBR | Aug.+ X. (1:1) | 3.07± 0.64 mm | 5.03± 2.15 mm | CBCT | 3 years | 7 months | 55 | 100% | 30-45 | N/A | Membrane exposure
(2/18) | (33) |
| Mendoza et
al, 2019 | RCT | 20(42) | Ant+Post Mx.
Mnd. | GBR | X | 3±0.44 mm (2.8-3.5
mm 95%CI) | 5.6± 1.35 mm | CBCT | 1.5 years | 6-9 months | 34 | 100% | N/A | N/A | Oedema (10/22).
Hematoma (4/22). Membrane exposure (2/22) | (34) |
| Zhang et al,
2019 | Retrospective | 12 | Mx. Ant. | GBR | X. TM | 4.88± 1.94 mm | 3.10± 2.006 mm | CBCT | 13-41 months | Immediate | 16 | 93.75% | >20 | N/A | Membrane exposure
(1/16). Peri-Implant Mucositis (1/16) | (35) |
| Valladao et
al, 2020 | Retrospective | 10/39 | Ant.+Post. Mx.
Mnd. | GBR | Aug.+ X. (1:1)
i-PRF L-PRF | 5.3±1.7 mm Ant:
4.5± 1.7 mm Post: 5.9± 1.5 mm Mx: 5.1± 1.4 mm Mnd: 6.4± 2.3 mm | 5.9± 2.4 mm Ant:
7.1± 2.9 mm Post: 5.2± 1.7 mm Mx: 6.5± 1.5 mm Mnd: 3.8± 1.1 mm | CBCT | 7.5 months | N/A | 25(48) | 100% | N/A | N/A | N/A | (36) |
| Isik et al,
2021 | RCT | 20 20 | Mnd. Post. | GBR | X. PRF X. | 4.25± 0.26 mm 4.33±
0.28 mm | 1.63± 0.21mm
(d2) 2.59± 0.34 mm (d4) 3.11± 0.36 mm
(d6) 1.34± 0.14 mm (d2) 2.49± 0.24 mm
(d4) | CBCT | 6 months | Immediate | 50 48 | 100% | N/A | 10 mm 3.8 mm 11.5
mm 3.8 mm 10 mm 4.2 mm | N/A | (37) |
| | | 20 | | | | | | | | | 48 | | | | | |
| Agabiti et
al, 2017 | Retrospective | 10 | Mnd. Post. | RS | - | 4.1±0.5 mm | 2.97± 0.24 mm
(d6) | CBCT | 1-3 years | 40 days | 15 | 100% | N/A | 10.5 mm 3.8-5
mm | N/A | (24) |
| Albanese et
al, 2017 | Prospective | 10 | Mx. Post. | RS | Alg. | 2.75± 1.09 mm | 3.25± 1.45 mm | CBCT | 1 year | Immediate | 45 | 97.8% | 35-40 | 10-11.5 mm 4.3
mm | N/A | (25) |
| Gurler et
al, 2017 | Retrospective | 17(40) | N/A | RS | X (Aug.) | 3.45± 0.25 mm | 2.09± 1.29 mm | CBCT | 3 years | 3-6 months | 33(77) | 93.9% | N/A | N/A | Bone dehiscence
(1/17) Ossteoint-egration failure (2/17) | (26) |
| Jamil et al,
2017 | Prospective | 23/26 | Mx. Ant. | RS | Alp. | 2.28± 0.72 mm | 4.24± 1.72 mm | Caliper | 4 months | Immediate | 57 | 100% | N/A | N/A | Bone dehiscence
(7/26) Paresthesia (5/26) | (27) |
| Kheur et al,
2017 | RCT | 11 | Mx. Mnd.
Ant.+Post. | RS | Alp. Alg. | 3.5± 0.667 mm 3.5±
0.667 mm | 3.192± 0.6748 mm
4.000± 0.6293 mm | Caliper | 1.5 years | 3 months | 49 | 100% | N/A | N/A | N/A | (28) |
| | | 12 | | | | | | | | | | | | | | |
| Mahmoud et
al, 2020 | RCT | 562 (1129) | Mnd. Mx. Ant.
Post. | RS | Alp. (Aug.) | 1.9±0.4 mm | 6.5± 0.7 mm | CBCT | 6 months | 6 months | N/A | N/A | N/A | N/A | N/A | (29) |
| Elamrousy et
al, 2021 | RCT | 11 11 | Mx. Ant. | RS | Aug. Aug.+ Alp.
(1:1) | 4.05± 0.53 mm 3.72±
0.60 mm | 3.61± 0.42 mm 6.42±
1.38 mm | CBCT | 6 months | Immediate | 30 | 100% | N/A | N/A | Oedema (4/22) | (30) |
Evaluation of studies
The present review included 18 studies divided as
follows: Six non-randomized retrospective trials without a control
group, six prospective non-randomized trials without a control
group and six prospective randomized controlled trials. Evaluation
of the 12 uncontrolled non-randomized trials was performed using
the modified MINORS score for comparative or single interventional
trials (Table II), and the six
randomized controlled trials were assessed using the CCRBT tool
(Table III). Thus, in the case of
non-randomized trials, the mean MINORS score for comparative trials
was 17 out of 24, and in the case of trials composed of a single
intervention group it was 12.44. The trials had clear aims and drew
relevant conclusions, despite the fact that sampling and
statistical analysis should have been more refined. It was
concluded, therefore, that non-randomized studies were credible
sources of scientific information and could be included in the
present systematic review. Evaluation of randomized controlled
studies determined the risk of bias in these studies, three of
which (60%) were evaluated as posing a low risk of bias and two
(40%) a medium risk of bias. In relation to the dimensional
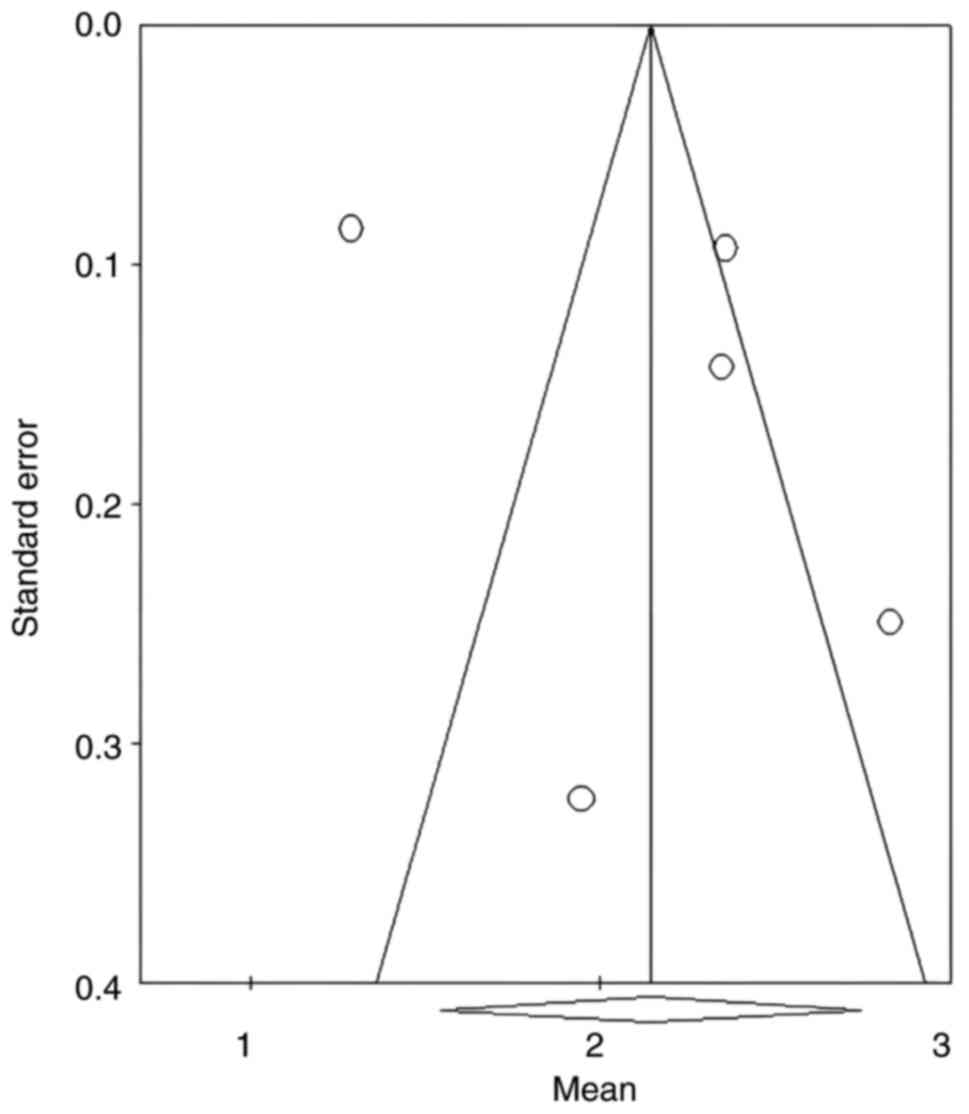
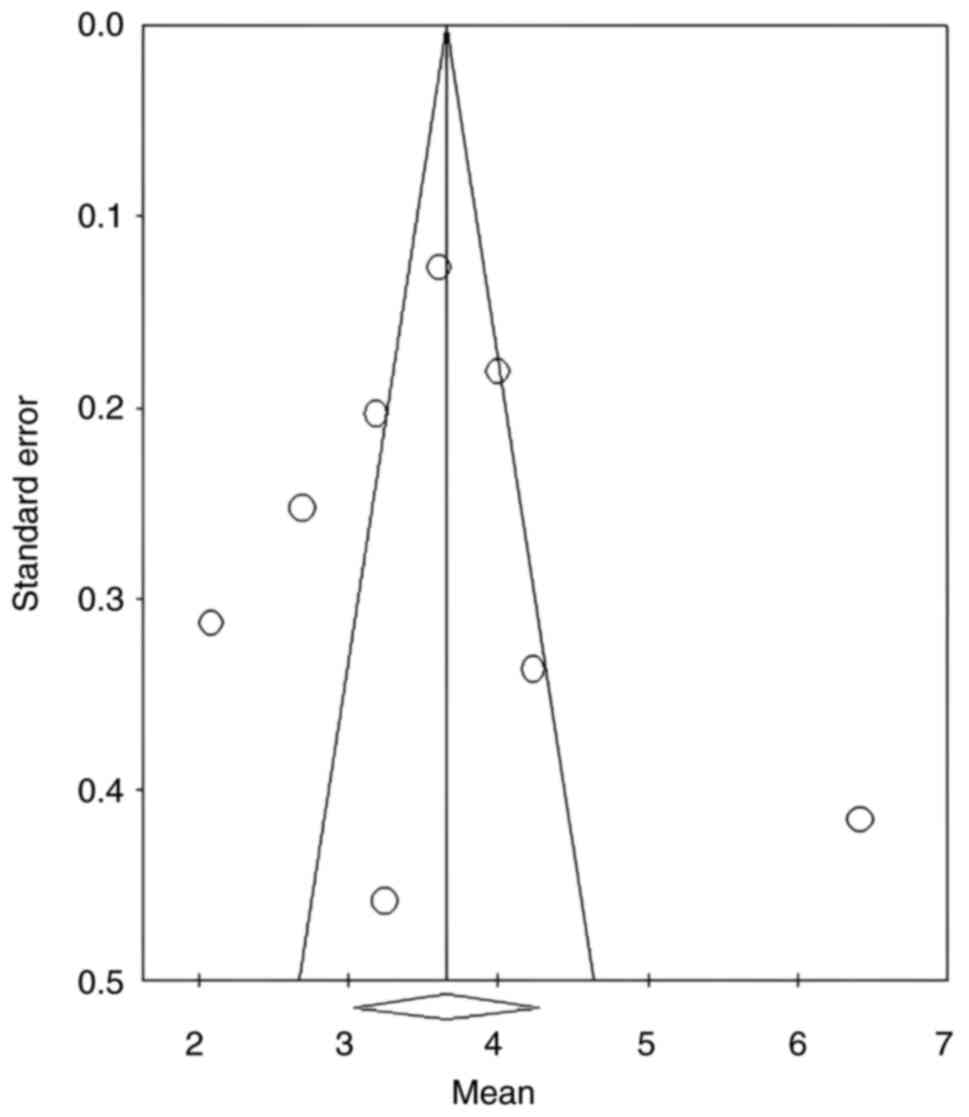
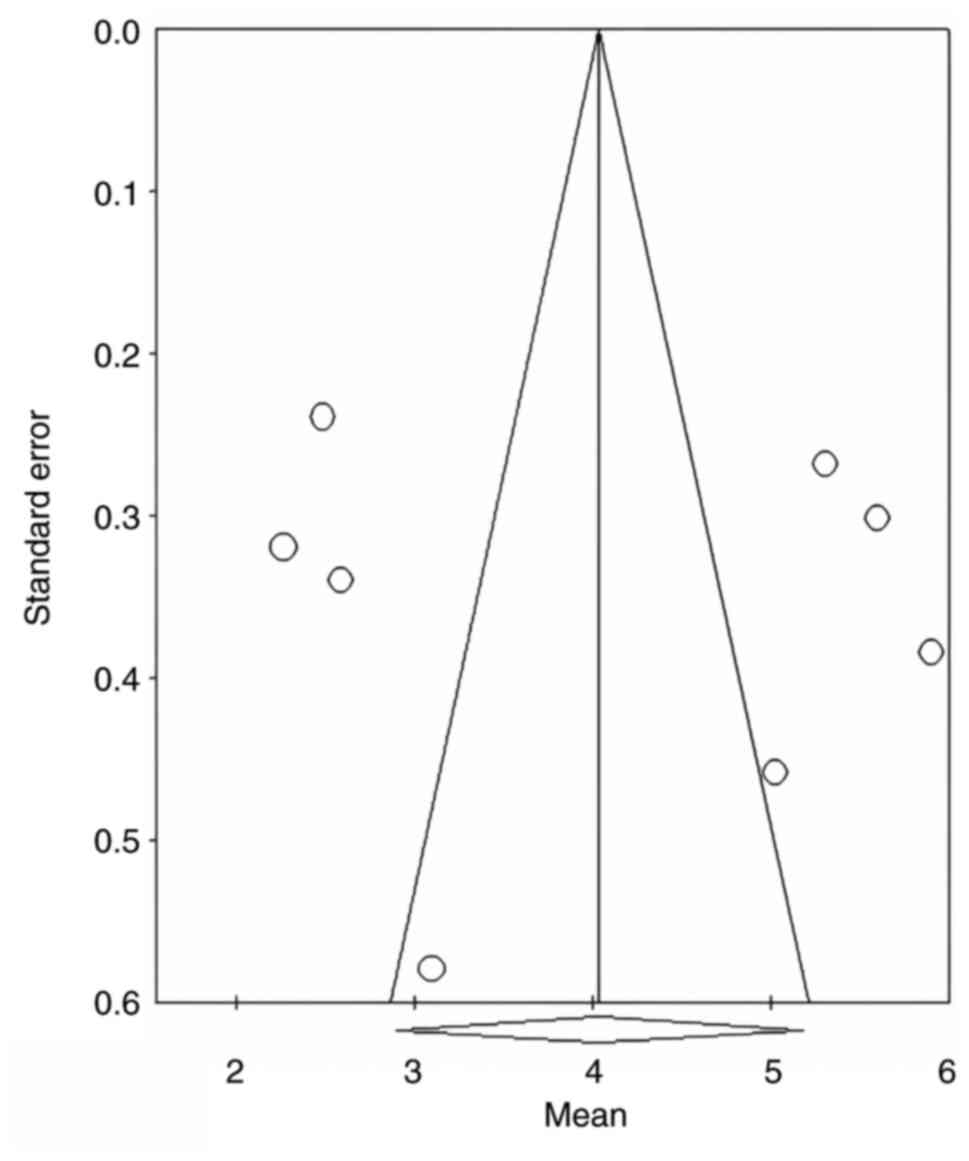
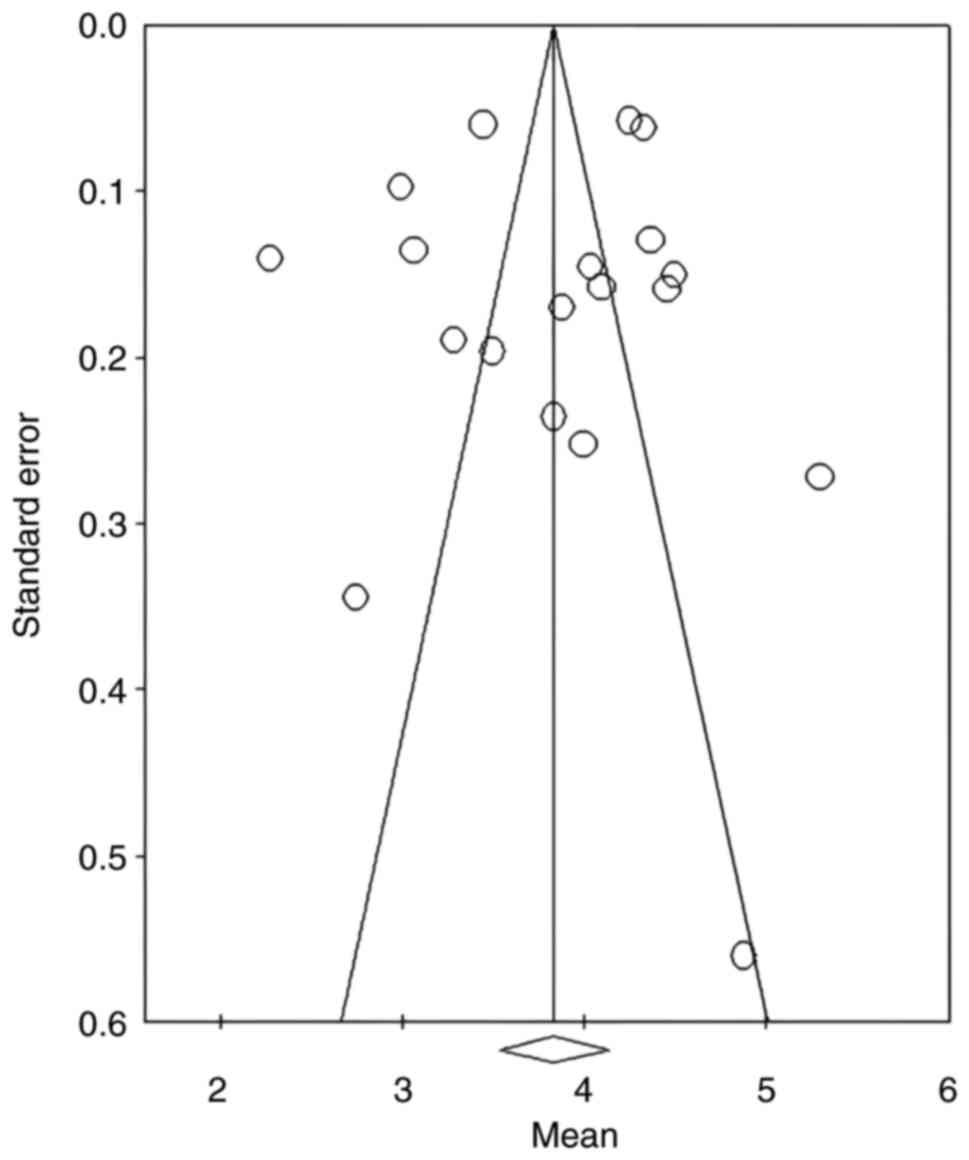
increase of the pre- and postoperative ridge, the Egger's
single-sample test was conducted in order to determine the spread
of the data at the levels of the entire study set presenting a high
risk of bias (P=0.006). However, it was considered that this
occurs, in large part, because of the differences between the
augmentation techniques applied at the level of the studies. For
this reason, the 17 studies included in the meta-analysis were
divided into three subgroups for which funnel plots were computed
(Fig. 2, Fig. 3 and Fig.
4). The study sample exhibited symmetry in regard to the median
of the funnel plots in every figure. While the large number of
studies situated outside the funnel can be a sign of bias, the
Egger's test results determined statistically insignificant
P-values (GBR: 0.35; RS: 0.4; OD: 0.23), that disprove the presence
of bias. After conducting the Egger test on the values of the
initial crest size, a statistically insignificant P-value of 0.35
was obtained, the funnel plot being represented in Fig. 5, the risk of bias being considered
low.
 | Table IIMethodological Index for
Non-randomized Studies criteria and scores applied to nonrandomized
studies included in the present study. |
Table II
Methodological Index for
Non-randomized Studies criteria and scores applied to nonrandomized
studies included in the present study.
| First author/s,
year | A clearly stated
aim | Inclusion of
consecutive patients | Prospective
collection of data | Endpoint
appropriate to the aim of the study | Unbiased assessment
of the study endpoints | Follow-up period
appropriate to the aim of the study | Loss of follow-up
less than 5% | Prospective
calculation of the study size | An adequate control
group | Contemporary
group | Baseline
equivalence of groups | Statistical
analyses adapted to the study design | Total | (Refs) |
|---|
| Koutouzis et
al, 2018 | 2 | 1 | 2 | 2 | 2 | 1 | 2 | 0 | 1 | 0 | 1 | 2 | 17/24 | (20) |
| Jarikian et
al, 2021 | 2 | 1 | 1 | 2 | 1 | 2 | 2 | 0 | 1 | 2 | 2 | 0 | 16/24 | (22) |
| Salman et
al, 2022 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 0 | - | - | - | - | 13/16 | (23) |
| Agha et al,
2019 | 2 | 2 | 1 | 2 | 1 | 2 | 2 | 0 | - | - | - | - | 12/16 | (21) |
| Gultekin et
al, 2017 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 0 | - | - | - | - | 12/16 | (31) |
| Meloni et
al, 2019 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 0 | - | - | - | - | 13/16 | (33) |
| Valladao et
al, 2020 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 0 | - | - | - | - | 13/16 | (36) |
| Zhang et al,
2019 | 2 | 1 | 1 | 2 | 1 | 2 | 2 | 0 | - | - | - | - | 11/16 | (35) |
| Agabiti et
al, 2017 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 0 | - | - | - | - | 12/16 | (24) |
| Albanese et
al, 2017 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 0 | - | - | - | - | 13/16 | (25) |
| Gurler et
al, 2017 | 2 | 2 | 1 | 2 | 1 | 2 | 2 | 0 | 2 | 2 | 1 | 1 | 18/24 | (26) |
| Jamil et al,
2017 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 0 | - | - | - | - | 13/16 | (27) |
 | Table IIIRandomized controlled studies
assessment via the RoB tool (Cochrane Collaboration's Tool for
Assessing the Risk of Bias in Randomized Trials). |
Table III
Randomized controlled studies
assessment via the RoB tool (Cochrane Collaboration's Tool for
Assessing the Risk of Bias in Randomized Trials).
| First author/s,
year | Random sequence
generation | Allocation
concealment | Blinding of
participants and personnel | Blinding of outcome
assessment | Incomplete outcome
data | Selective
reporting | Other bias | Conclusion | (Refs) |
|---|
| Halperin et
al, 2018 | ? | + | ? | ? | + | + | + | Moderate risk | (32) |
| Mendoza et
al, 2019 | + | + | + | + | + | + | + | Low risk | (34) |
| Isik et al,
2021 | + | + | + | ? | + | + | + | Low risk | (37) |
| Kheur et al,
2017 | + | + | + | ? | + | + | + | Low risk | (28) |
| Mahmoud et
al, 2020 | + | + | + | + | - | - | + | Moderate risk | (29) |
| Elamrousy et
al, 2021 | + | + | + | + | + | + | + | Low risk | (30) |
Meta-analysis between study
subgroups
The 17 articles were divided, relative to the groups
the authors compared, into 21 independent studies. The means from
the two groups of the study published by Koutouzis et al
(20) were separated into two
studies, excluding the group treating patients with crest sizes
between 7 and 8 mm. The studies published by Kheur et al
(28), Işık et al (37) and Elamrousy et al (30) were also divided into two separate
and independent studies. From the studies showing a comparison
between one of the three techniques and the addition of autogenous
bone block, only those in which bone augmentation was performed by
RS, GBR or ridge expansion via OD were selected. Thus, in total, 21
studies were analyzed, comprising 336 patients and 665 implants.
These were divided as follows: Five studies on ridge expansion via
OD, eight on GBR and eight on the RS technique. The division
according to the number of patients and implants was made as
follows: 73 patients and 93 implants for ridge expansion via OD,
149 patients and 334 implants for GBR and 105 patients and 229
implants for the RS technique.
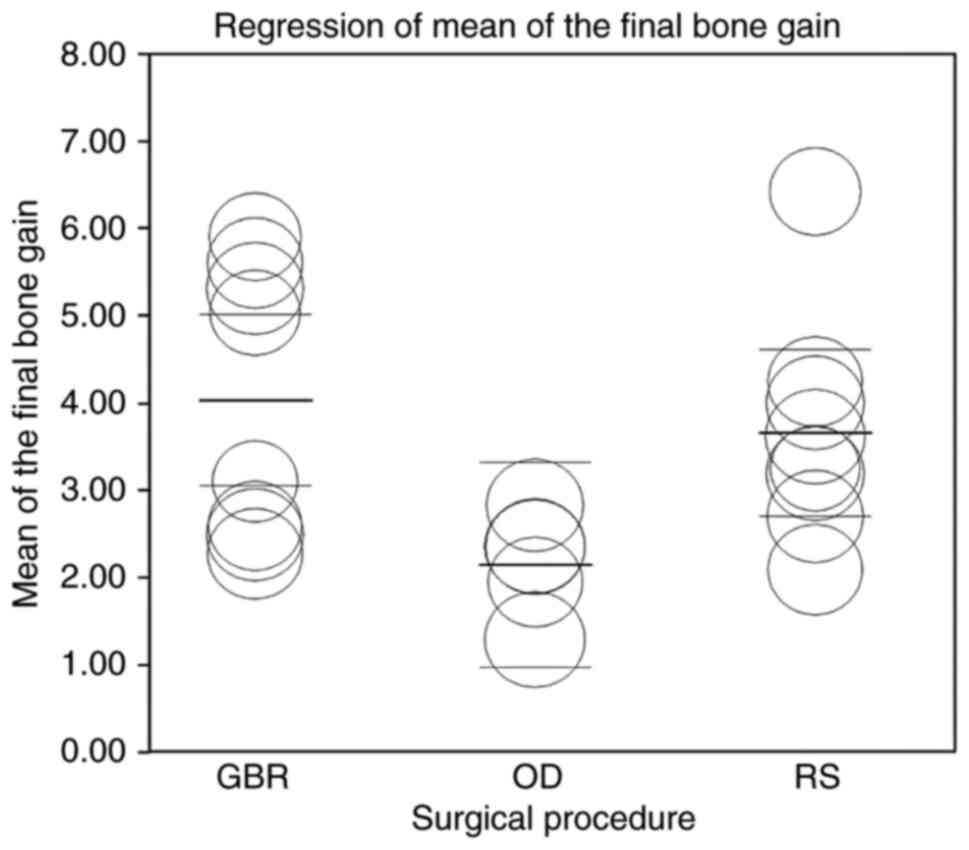
Statistical analysis of the final bone
gain. Heterogeneity and dispersion relative to the final bone
gain
The variation in studies relative to the horizontal
bone gain and calculated based on the determination of the
statistical index I2 showed a heterogeneity of 94.6%,
this value indicating a dataset with an increased variability. This
heterogeneity was based on the clinical factor, the difference
between interventions, participants and results. The division of
the studies into three subgroups according to the augmentation
method used was not sufficient to eliminate the variability between
the data sets in the case of GBR and the RS technique (Table IV). Considering these results, a
scatterplot was made using a random effects model (Fig. 6). Each circle represents the effect
size of each included study using the random effects model. The
highlighted line represents the median of all the pooled studies,
while the first lines under and over delineate the CI (95%). This
representation used the categorical moderator factor represented by
the surgical technique. In the case of ridge expansion via OD, a
portion of the study data published by Koutouzis et al
(20) exceed the confidence
interval. In the case of the RS technique, the studies by Gurler
et al (26) and Agabiti
et al (24) show on average
the lowest bone gain, well below the subgroup average and outside
the confidence interval. On the other hand, the test group of the
study by Elamrousy et al (30) presents the most bone growth, its
limit reaching the upper limit of the prediction interval. The GBR
group can be divided into two parts in terms of dimensional growth.
By applying the heterogeneity test for these groups separately, the
I2 index value is 0% for both of the studied groups
(maximum homogeneity; Table V).
 | Table IVHeterogeneity analysis of the final
bone gain. |
Table IV
Heterogeneity analysis of the final
bone gain.
| Subgroup | Number of
studies | Q |
τ2 | I2 | P-value |
|---|
| OD | 5 | 19.02 | 0.432 | 78.75 | >0.001 |
| GBR | 8 | 69.35 | 2.536 | 89.85% | >0.001 |
| RS | 8 | 54.7 | 0.697 | 87.03% | >0.001 |
 | Table VHeterogeneity analysis of the final
bone gain in the guided bone regeneration studies. |
Table V
Heterogeneity analysis of the final
bone gain in the guided bone regeneration studies.
| First author/s,
year | | | | (Refs) |
|---|
| Isik et al,
2021 | Q=2.714 |
I2=0% | P=0.438 | (37) |
| Halperin et
al, 2019 | | | | (32) |
| Zhang et al,
2019 | | | | (35) |
| Gultekin et
al, 2017 | Q=1.664 |
I2=0% | P=0.645 | (31) |
| Meloni et
al, 2019 | | | | (33) |
| Mendoza et
al, 2019 | | | | (34) |
| Valladao et
al, 2020 | | | | (36) |
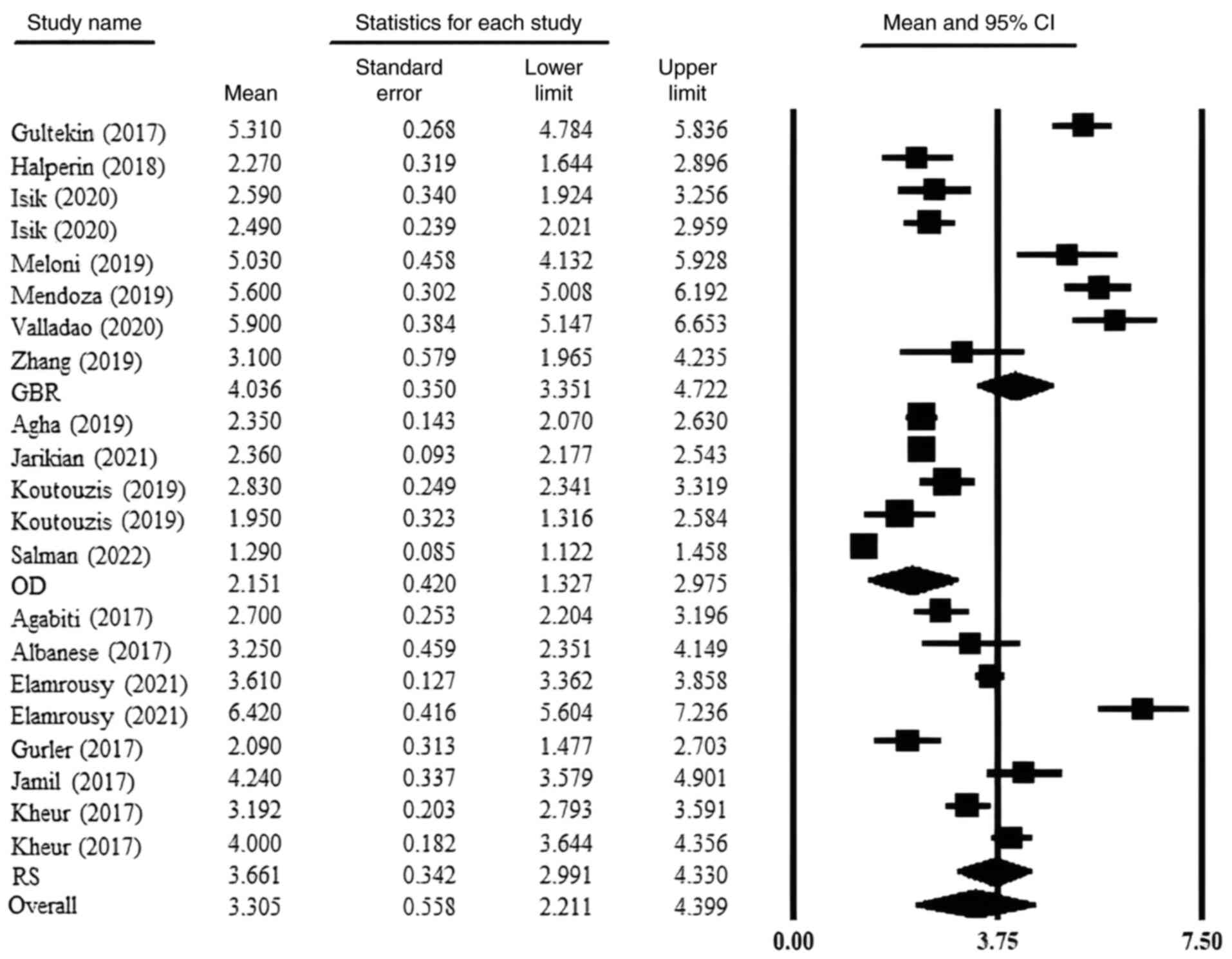
Means, confidence intervals and
comparison between procedures
The mean bone gain with regard to the GBR studies
was 4.036 mm (3.351-4.772 mm 95%CI). Breaking the GBR group of
studies into two parts in terms of heterogeneity, the means were
2.504 mm (2.189-2.818 mm 95%CI) and 4.990 mm (3.98-5.993 mm 95%CI).
The mean bone gain for the RS studies was 3.661 mm (2.991-4.330 mm
95%CI). The studies on ridge expansion via OD reported a bone gain
mean of 2.151 mm (1.327-2.975 mm 95%CI). The global mean across the
study group was 3.305 mm (2.211-4.399 mm 95%CI; Fig. 7). The null hypothesis is the
following: There is no difference between bone gains depending on
the surgical procedure used. The Cochran's heterogeneity test based
on analysis of variance (ANOVA) showed statistical significance
(P=0.002), contradicting the null hypothesis. Comparing each of the
two subgroups separately from each other results in the following
P-values: GBR vs. ridge expansion via OD (P=0.001), GBR vs. RS
(P=0.09) and RS vs. ridge expansion via OD (P=0.004).
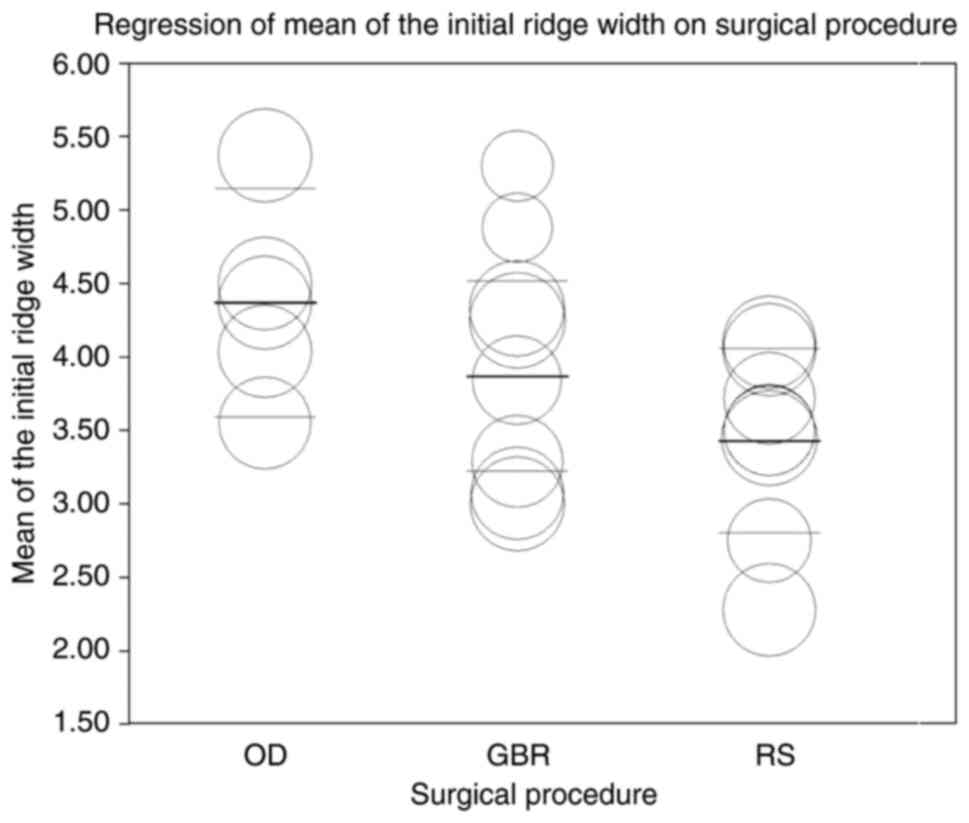
Statistical analysis of the initial
ridge size. Heterogeneity and dispersion of studies for the initial
crest width
The calculated values of the statistical indices Q
(418.02), I2 (95.69%) and τ2 (0.3765)
highlight a very significant heterogeneity across the entire set of
studies. One of the causes considered for this heterogeneity is
represented by the correlation between the surgical technique and
the horizontal diameter of the edentulous ridges to which they were
applied. Under these conditions, the values were recalculated by
dividing the studies into three subgroups determined by the
augmentation technique. The values of the statistical indices are
represented in Table VI. However,
the heterogeneity did not decrease considerably; I2
index values remaining well >50%, a number of factors causing
heterogeneity depending on the choice of a certain initial crest
size. The most important of these is that these techniques can be
applied for a very large range of dimensions. Valladão et al
(36) published in their study an
average of 5.3 mm for the application of GBR, and Mendoza et
al (34) reported 3 mm. This is
also true for the RS technique, but less so for ridge expansion via
OD, as seen from the table of heterogeneities. A scatterplot was
devised using the augmentation technique (categorical variable) as
a moderator factor, in order to observe the limits of the initial
size of the ridge within the study set proposed in this review
(Fig. 8). The meta-regression used
the random effect model. The confidence interval for GBR does not
include the published study by Valladão et al (36) and the study published by Zhang et
al (35) appears at the upper
limits of the initial crest width augmented by GBR. The lower limit
is represented by the studies written by Mendoza et al
(34) and Meloni et al (33),
the projection of a portion of the data collected from these
studies entering the prediction interval and not the confidence
one. In studies presenting data on the RS technique, the upper
limit was represented by the studies of Agabiti et al
(24) and Elamrousy et al
(30), and the lower limit is
determined by the studies of Jamil et al (27) and Albanese et al (25), the projection of the study performed
by Jamil et al (27) having
a region outside the prediction range. Regarding ridge expansion
via OD, the study of Koutouzis et al (20), divided into independent groups,
delineates the prediction intervals. Heterogeneity arises largely
because of the data generated from these studies.
 | Table VIHeterogeneity analysis for the
initial ridge width. |
Table VI
Heterogeneity analysis for the
initial ridge width.
| Subgroup | Number of
studies | Q |
τ2 | I2 | P-value |
|---|
| OD | 5 | 10.94 | 0.04 | 72.56% | 0.01 |
| GBR | 8 | 44.185 | 0.236 | 74.11% | >0.001 |
| RS | 8 | 59.83 | 0.33 | 89.97% | >0.001 |
Means, confidence intervals and
comparison between techniques
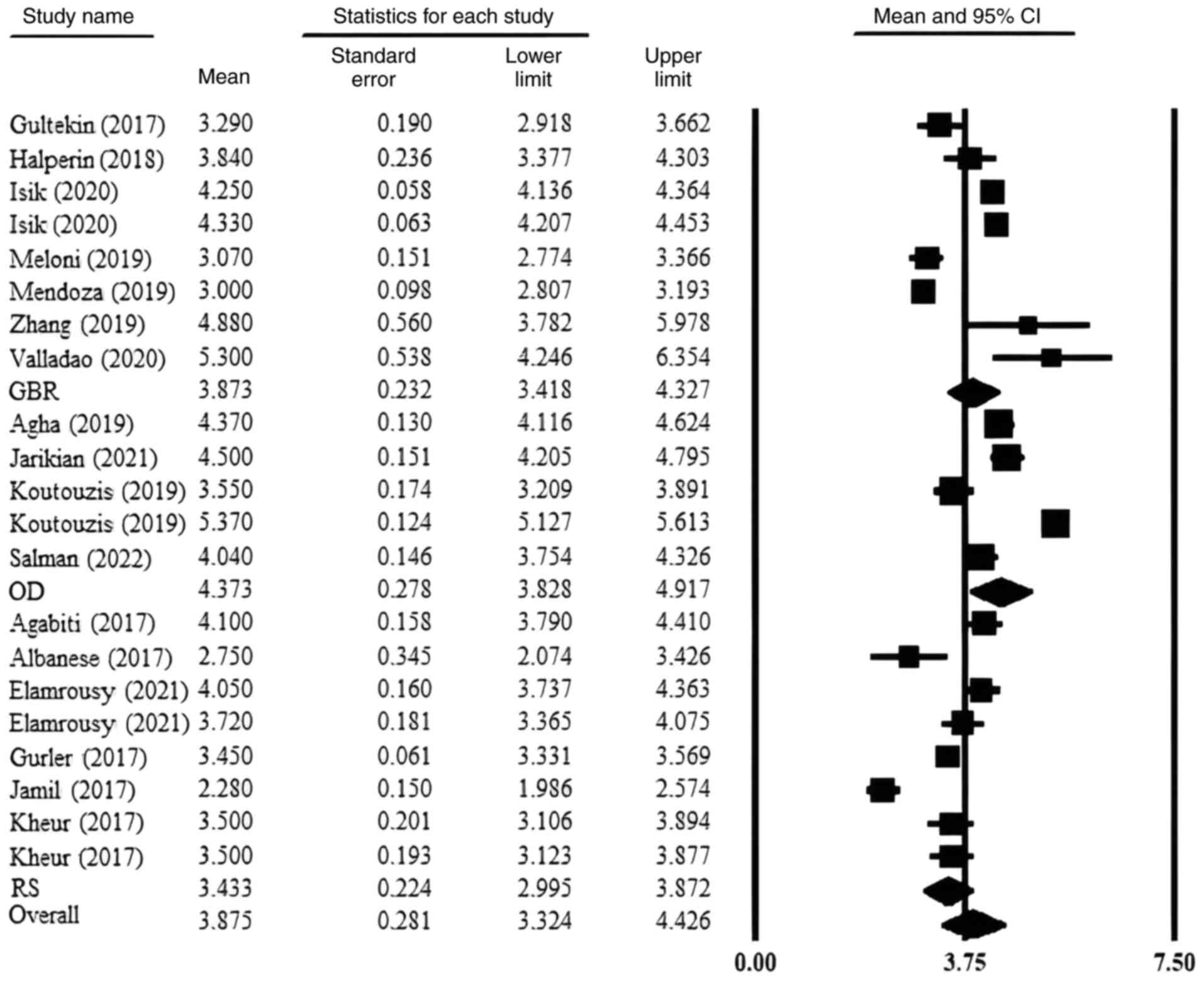
By applying the random effects model, the average
size of the edentulous ridge was determined in relation to all the
studies included in the review and grouped into OD, GBR and RS
subgroups (Fig. 9). The mean
baseline ridge diameter across the entire study group was 3.875 mm
with a 95%CI between 3.325 and 4.426 mm. For the studies on ridge
expansion via OD, the aggregate mean of the studies was 4.373 mm
with a 95%CI between 3.828 and 4.917 mm. GBR was applied in the
case of an average width ridge of 3.873 mm with a 95%CI between
3.418 and 4.327 mm, and for RS, the mean is 3.433 mm, and the 95%CI
was between 2.995 and 3.872 mm. The null hypothesis of this portion
of the statistical analysis was as follows: There is no difference
in the initial ridge size depending on the technique used. The
comparison of the three subgroups with a Cochran heterogeneity test
based on the analysis of variance (ANOVA) reports a statistically
significant P-value of 0.03, thus contradicting the null
hypothesis. However, the comparison of each of the two subgroups
separately from each other results in the following P-values: GBR
vs. ridge expansion via OD (P=0.08), GBR vs. RS (P=0.18) and RS vs.
ridge expansion via OD (P=0.001).
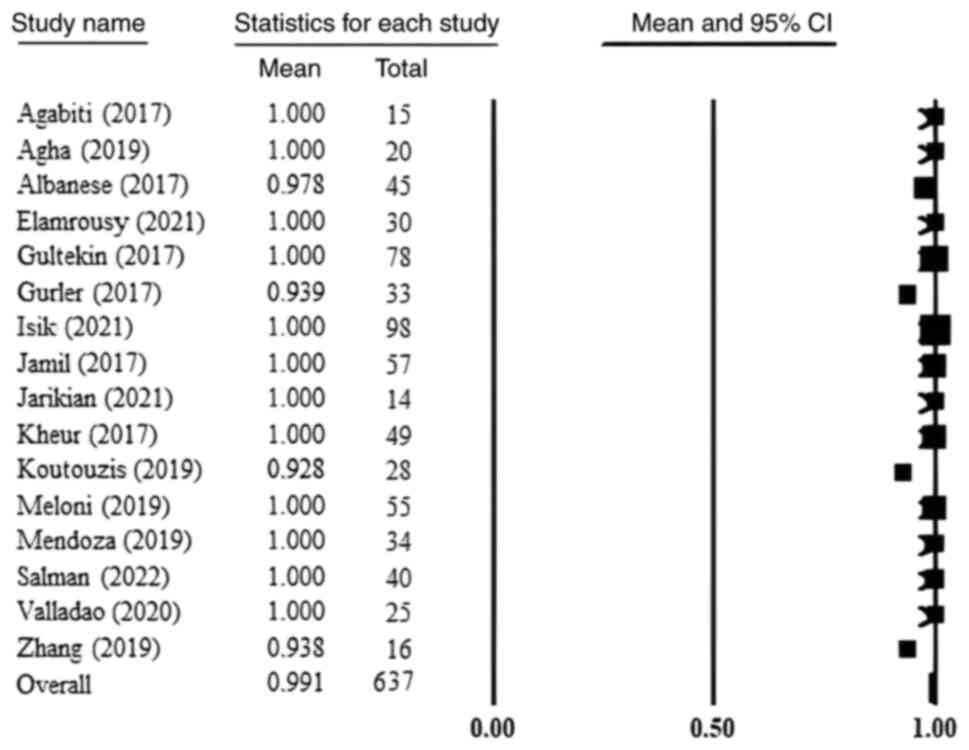
Survival rate of implants
The survival rate of implants was very high,
regardless of the technique used. The current selection of studies
had a mean survival rate of 99.1%. The six GBR studies that
reported these data had a mean of 99.7%, the six studies on RS had
a mean of 98.7% and for the four studies on ridge expansion via OD
it was 98% (Fig. 10). The
differences were not statistically relevant.
Bone gain in relation to graft
type
The graft type was used as a moderating factor in
the statistical analysis. Two studies (20,23)
were excluded from this analysis for not providing accurate data on
the number of patients or interventions requiring grafting. The
bone grafts were divided as follows:
1. N-no use of bone substitute reported
2. Aug-autologous bone or mixture (autogenous graft
and xenogeneic bone or autogenous bone and alloplastic
material)
3. Alg-allogeneic bone
4. Alp-synthetic material
5. X-xenogeneic graft
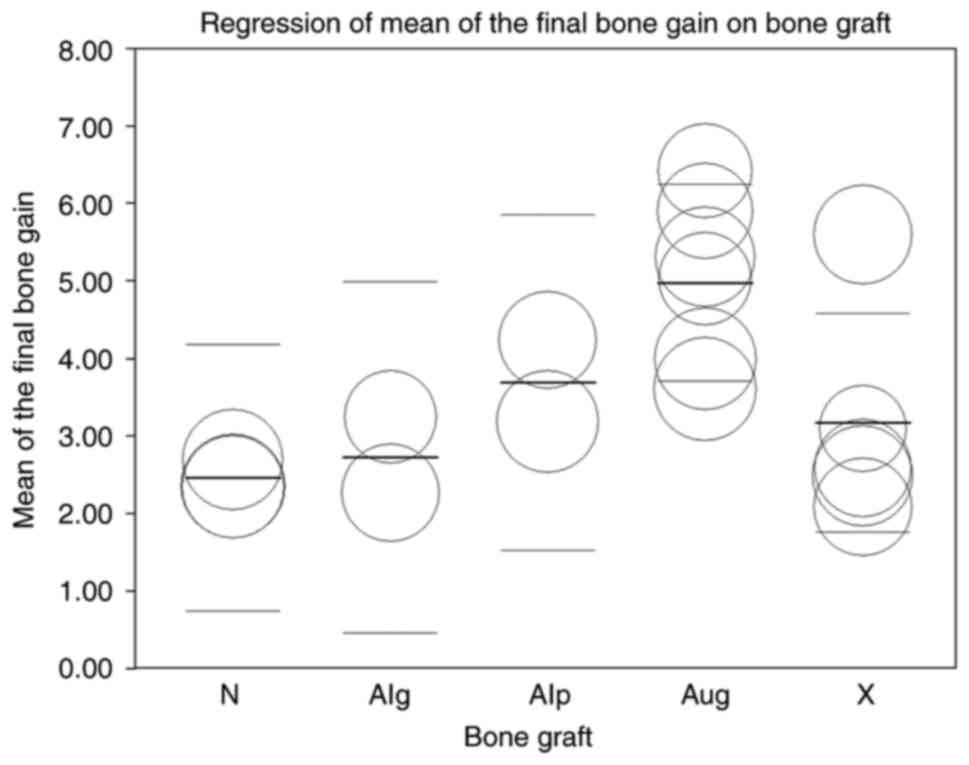
Dispersion of studies related to the
type of bone graft
A scatter plot is shown in Fig. 11 with the following
characteristics:
i) In the subgroup using animal bone grafts, the
study published by Mendoza et al (34) reported the most important bone gain
outside the confidence interval.
ii) On average, the subgroup that did not use bone
grafts at all showed the least horizontal bone gain followed by the
mean of the subgroup of allogeneic bone grafts and the mean of the
subgroup of xenogeneic bone grafts.
iii) The autologous bone subgroup reports the
largest difference in initial and final width.
iv) The subgroups of allogeneic grafts and synthetic
materials will not be considered in the statistical comparison.
v) The test group in the study published by
Elamrousy et al (30)
presented the most bone gain, part of the data reported being
located outside the CI, and the control group is placed in the area
with the least final bone gain reported.
vi) Within the subgroup of xenogeneic bone grafts,
the study published by Gurler et al (26) reported the lowest dispersion within
the study set.
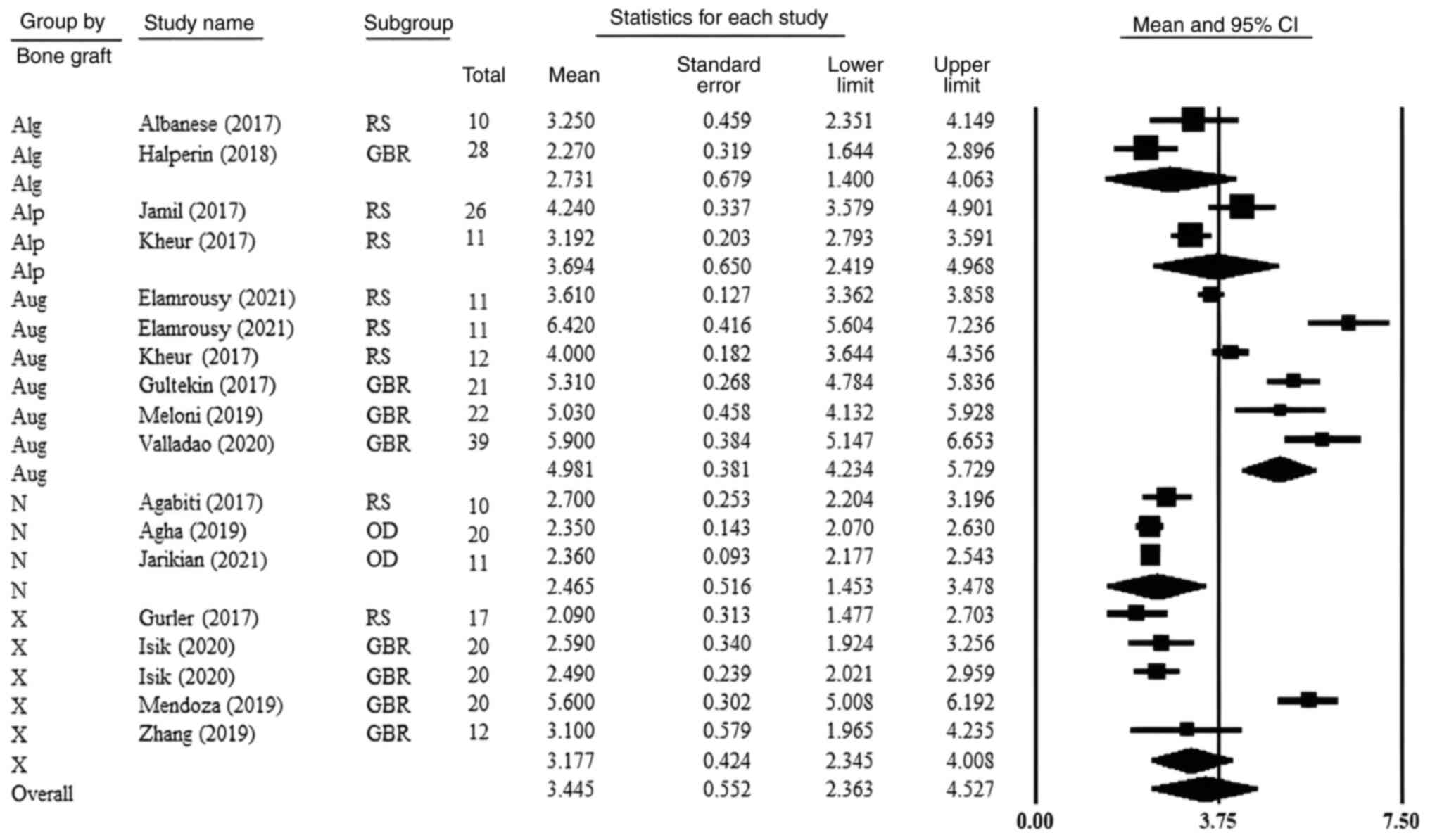
Means and CIs
For the studies describing bone augmentations
performed with xenografts, autologous bone or using no grafting,
means and CIs were calculated (Fig.
12). Studies that did not report the use of any bone graft had
a mean difference in baseline and endpoint of 2.465 mm with a 95%CI
between 1.453 and 3.478 mm. Studies in which the autologous crest
is augmented reported a mean of 4.981 mm with a 95%CI between 4.234
and 5.729 mm. The mean bone gain using xenogeneic grafts is 3.177
mm with a 95%CI between 2.345 and 4.008 mm. In the case of
subgroups of allogeneic grafts and synthetic materials, the means
are 2.731 mm (1.400-4.063 mm 95%CI) and 3.694 mm (2.419-4.968 mm
95%CI), respectively. These studies were not included in the
comparison between subgroups. In the null hypothesis, there are no
differences in bone gain depending on the type of graft. The
P-value recorded is <0.001, and the separate comparisons showed
the following: autologous bone vs. no graft (P<0.001),
autologous bone vs. xenogeneic bone (P=0.014), no graft vs.
xenogeneic bone (P=0.248).
Discussion
While there are a number of studies regarding the
long term clinically relevant results of RS and GBR (i.e., final
bone gain, resorption and recorded secondary stability), the OD
technique is not as well documented in a way that can provide long
term data so that a proper conclusion regarding the ideal surgical
technique could be drawn. A published meta-analysis on the
augmentation of horizontal ridge defects (2014) identified an
increase in ridge width of 3.31 mm (38). This result is similar to the outcome
of the present study, in which a bone gain of 3.3 mm (2.211-4.33 mm
95%CI) was identified. A systematic review conducted in
2018(19) reported bone gain values
through bone regeneration guided by 2.27±1.68 mm. The present
review included studies published from 1997 to 2014. In the present
study, the mean bone gain for studies using GBR was much higher at
4.036 mm (3.351-4.772 mm 95%CI). However, the 2018 meta-analysis
only considered studies using a xenogeneic bone substitute. The
mean bone gain in the xenogeneic graft studies included in this
meta-analysis was 3.454 mm (2.134-4.744 mm 95%CI). Another
meta-analysis published in 2015(39) showed comparable results, a mean of
3.9 mm (3.52-4.28 mm 95%CI), but this includes the onlay block
technique. Another systematic review published in 2018(7) showed 2.59±0.29 mm (standard error)
horizontal bone gain following GBR. More recent meta-analyses have
not been identified. Studies using different means of improving the
efficiency of GBR (PRF, titanium membrane, autogenous bone mixture
and xenogeneic bone) report means greater than 4 mm. It should be
taken into account that most of the studies included in these
reviews and meta-analyses use GBR as a way to restore various small
or medium post-extraction defects, unlike the studies in this
meta-analysis which aimed at the concrete dimensional growth of the
edentulous ridge. The shortcomings of the current study (high
heterogeneity, short period of time of the study), but also the
lack of recent systematized data (meta-analyses) related to this
technique, determine the difference between the mean of the current
study and those published for the time being in the literature.
Regarding the RS technique, a meta-analysis from
2015(18) estimated a mean of the
final difference at the level of the ridge of 3.19 mm (2.19-4.2 mm;
95%CI), comparable to the current study. The most recent
meta-analysis in 2017(3) noted a
horizontal increase of 3.61 mm, agreeing with the data from the
present study.
Meta-analyses that determine a mean of horizontal
bone gain through ridge expansion via OD have not been published to
date. In the present analysis, however, ridge expansion via OD
determined results comparable to the lower portion (in terms of
increasing horizontal size) of the included studies of RS and
GBR.
The current review did not consider the combination
of the techniques discussed. A single included study, Jamil et
al (27), performed the RS
technique together with GBR in certain treated cases, but this was
not included in the analysis, due to the uniqueness of the
phenomenon within the set of studies, but also to facilitate the
subsequent statistical assessment. Studies combining ridge
expansion via OD with GBR or RS with ridge expansion via OD have
not been identified as such, but the studies published by Koutouzis
et al (20) and Salman et
al (23) used bone substitute
to augment the vestibular area of the implant insertion site under
the conditions recommended by the inventors of the Versah burs and
the ridge expansion via OD technique (vestibular cortical bone ≤2
mm). The combination of techniques is, according to the authors, a
research direction that should be considered.
A very high degree of variability in the data from
the studies on GBR was observed; also evident is the overlap of the
two techniques (GBR and RS) in terms of available bone and its
horizontal growth rate, the statistical analysis determining
P-values higher than the statistical relevance threshold.
However, there is a clear delimitation between the
dimensions of the edentulous ridges to which ridge expansion via OD
can be applied, but also the bone gain that can be expected from
this technique. It should be taken into account that the main
indication of ridge expansion via OD is a jawbone with low density,
not narrow edentulous ridges. The OD technique used in order expand
the ridge horizontally is dependent on the amount of basal bone
(located at 5-10 mm from the top of the edentulous ridges), an
aspect that was not taken into account in the present study, being
highlighted only in one of the included publications. The
literature has the following minimum horizontal dimensions where
the use of different procedures are indicated: 3 mm for GBR
(40) and 2.5-3 mm for RS (41,42),
although this seems a rather arbitrary condition, as, in clinical
work, surgical options are selected by assessing a number of other
variables related to the basal bone mass including density, patient
anatomy and practitioner experience. While the current review does
not take into account every possible factor, it however reflects
the minimum horizontal dimension indications, bringing new
information on the applicability of ridge expansion via OD to
horizontal ridge defects.
Although not as effective in terms of the horizontal
growth of the edentulous ridge, ridge expansion via OD excels in
its ease of application and predictability. The application of RS
and GBR is highly dependent on the skill of the practitioner and
the management of complications and accidents. Dehiscence and
membrane exposure or bad splitting are common incidents that
jeopardize the success of lateral ridge augmentation. However,
implant survival rates are comparable for all augmentation
methods.
Relative to the type of bone substitute, the
superiority of autologous bone is further observed in the case of
the analyzed techniques (GBR and RS), the onlay block bone graft
technique not being included in the present study. Statistical
analysis by graft has been carried out as a guide only; the present
study was not intended to identify significant results in this
respect.
The present review has some limitations. First of
all, the studies included in this analysis are not ideal, as they
are not, entirely, randomized controlled studies. Some included
studies present the results of different demonstrations of changes
in the techniques of augmentation itself, making them sensitive to
a risk of bias increase. Second, the number of studies related to
each technique is not similar, there being a rather large
discrepancy between the samples identified for each method, ridge
expansion via OD being a relatively recent procedure with few
published studies as of yet. Third, the authors have not identified
studies that consider the initial width of the ridge as a
statistical variable, so the analysis and results from this data
should be interpreted with caution.
As aforementioned, there are a number of factors on
which the choice of these ways of horizontal bone augmentation
depends, the current meta-analysis taking into account a very
limited number of them. In the future, it will be necessary to
correlate these factors in a more complex statistical model by
analyzing the data of more homogeneous set of studies (from a
clinical and methodological point of view) in order to obtain the
most accurate results and to devise protocols that eliminate as
much as possible the uncertainty in the treatment of cases of
horizontal atrophy of edentulous ridges.
Taking into account the shortcomings of this
investigation, the final conclusions are as follows: i) Among the
techniques discussed, GBR reports the most bone gain, followed
closely by the RS technique and then ridge expansion via OD, ii)
the RS technique is applied to ridges with the smallest initial
size, GBR and ridge expansion via OD requiring a thicker alveolar
ridge iii) implant survival rate is very high for all the
augmentation procedures and iv) ridge expansion via OD with Versah
burs is a technique that must be considered when discussing lateral
ridge augmentation. The results are not as impressive as in the
case of GBR or RS, but its predictability and ease of application
are preferable factors for clinicians.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study are included
in the figures and/or tables of this article.
Authors' contributions
VA, SD and AP conceived and designed the present
study, which was co-ordinated by AP and SD. VA and SD were
responsible for data collection and confirm the authenticity of all
the raw data. VA, SD and AP were responsible for data management,
analysis and interpretation. VA and SD wrote the present study. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Nentwig GH: Technic of bone splitting for
alveolar recession in anterior maxillary region. Quintessenz.
37:1825–1834. 1986.PubMed/NCBI(In German).
|
|
2
|
Inchingolo AD, Inchingolo AM, Bordea IR,
Xhajanka E, Romeo DM, Romeo M, Zappone CMF, Malcangi G, Scarano A,
Lorusso F, et al: The effectiveness of osseodensification drilling
protocol for implant site osteotomy: A systematic review of the
literature and meta-analysis. Materials (Basel).
14(1147)2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Waechter J, Leite FR, Nascimento GG, Carmo
Filho LC and Faot F: The split crest technique and dental implants:
A systematic review and meta-analysis. Int J Oral Maxillofac Surg.
46:116–128. 2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Starch-Jensen T and Becktor JP: Maxillary
alveolar ridge expansion with split-crest technique compared with
lateral ridge augmentation with autogenous bone block graft: A
systematic review. J Oral Maxillofac Res. 10(e2)2019.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Schopper C, Goriwoda W, Moser D, Spassova
E, Watzinger F and Ewers R: Long-term results after guided bone
regeneration with resorbable and microporous titanium membranes.
Oral Maxillofac Surg Clin N Am. 13:449–458. 2001.
|
|
6
|
Tolstunov L: Classification of the
alveolar ridge width: Implant-driven treatment considerations for
the horizontally deficient alveolar ridges. J Oral Implantol.
40:365–370. 2014.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Elnayef B, Porta C, Suárez-López Del Amo
F, Mordini L, Gargallo-Albiol J and Hernández-Alfaro F: The fate of
lateral ridge augmentation: A systematic review and meta-analysis.
Int J Oral Maxillofac Implants. 33:622–635. 2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Huwais S and Meyer EG: A novel osseous
densification approach in implant osteotomy preparation to increase
biomechanical primary stability, bone mineral density, and
bone-to-implant contact. Int J Oral Maxillofac Implants. 32:27–36.
2017.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Pai UY, Rodrigues SJ, Talreja KS and
Mundathaje M: Osseodensification-a novel approach in implant
dentistry. J Indian Prosthodont Soc. 18:196–200. 2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Frizzera F, Spin-Neto R, Padilha V,
Nicchio N, Ghiraldini B, Bezerra F and Marcantonio E Jr: Effect of
osseodensification on the increase in ridge thickness and the
prevention of buccal peri-implant defects: An in vitro randomized
split mouth pilot study. BMC Oral Health. 22(233)2022.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Zhou L, Su Y and Wang J, Wang X, Liu Q and
Wang J: Effect of exposure rates with customized versus
conventional titanium mesh on guided bone regeneration: Systematic
review and meta-analysis. J Oral Implantol. 48:339–346.
2022.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Carini F, Longoni S, Amosso E, Paleari J,
Carini S and Porcaro G: Bone augmentation with TiMesh. autologous
bone versus autologous bone and bone substitutes. A systematic
review. Ann Stomatol (Roma). 5 (Suppl 2 to No 2):S27–S36.
2014.PubMed/NCBI
|
|
13
|
Tolstunov L, Hamrick JFE, Broumand V,
Shilo D and Rachmiel A: Bone augmentation techniques for horizontal
and vertical alveolar ridge deficiency in oral implantology. Oral
Maxillofac Surg Clin North Am. 31:163–191. 2019.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Arnal HM, Angioni CD, Gaultier F,
Urbinelli R and Urban IA: Horizontal guided bone regeneration on
knife-edge ridges: A retrospective case-control pilot study
comparing two surgical techniques. Clin Implant Dent Relat Res.
24:211–221. 2022.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Atef M, Tarek A, Shaheen M, Alarawi RM and
Askar N: Horizontal ridge augmentation using native collagen
membrane vs titanium mesh in atrophic maxillary ridges: Randomized
clinical trial. Clin Implant Dent Relat Res. 22:156–166.
2020.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Slim K, Nini E, Forestier D, Kwiatkowski
F, Panis Y and Chipponi J: Methodological index for non-randomized
studies (minors): Development and validation of a new instrument.
ANZ J Surg. 73:712–716. 2003.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Higgins JPT, Altman DG, Gøtzsche PC, Jüni
P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, et
al: The cochrane collaboration's tool for assessing risk of bias in
randomised trials. BMJ. 343(d5928)2011.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Elnayef B, Monje A, Lin GH,
Gargallo-Albiol J, Chan HL, Wang HL and Hernández-Alfaro F:
Alveolar ridge split on horizontal bone augmentation: A systematic
review. Int J Oral Maxillofac Implants. 30:596–606. 2015.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Wessing B, Lettner S and Zechner W: Guided
bone regeneration with collagen membranes and particulate graft
materials: A systematic review and meta-analysis. Int J Oral
Maxillofac Implants. 33:87–100. 2018.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Koutouzis T, Huwais S, Hasan F, Trahan W,
Waldrop T and Neiva R: Alveolar ridge expansion by
osseodensification-mediated plastic deformation and compaction
autografting: A multicenter retrospective study. Implant Dent.
28:349–355. 2019.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Agha MM and El-Mohandes WA: Evolution of
implant placement in narrow alveolar ridge using versah drills.
Al-Azhar J Dent Sci. 22:247–251. 2019.
|
|
22
|
Jarikian S, Jaafo MH and Al-Nerabieah Z:
Clinical evaluation of two techniques for narrow alveolar ridge
expansion: Clinical study. Int J Dent Oral Sci. 8:1047–1052.
2021.
|
|
23
|
Salman RD and Bede SY: The use of
osseodensification for ridge expansion and dental implant placement
in narrow alveolar ridges: A prospective observational clinical
study. J Craniofac Surg. 33:2114–2117. 2022.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Agabiti I and Botticelli D: Two-stage
ridge split at narrow alveolar mandibular bone ridges. J Oral
Maxillofac Surg. 75:2115.e1–2115.e12. 2017.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Albanese M, Ricciardi G, Luciano U,
Donadello D, Lucchese A, Gelpi F, Zangani A, De Santis D, Rizzini
A, Rossetto A and Bertossi D: Alveolar splitting with
Piezosurgery®, bone bank grafts and NobelActive implants as an
alternative to major bone grafting for maxillary reconstruction.
Minerva Stomatol. 68:3–10. 2019.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Gurler G, Delilbasi C, Garip H and
Tufekcioglu S: Comparison of alveolar ridge splitting and
autogenous onlay bone grafting to enable implant placement in
patients with atrophic jaw bones. Saudi Med J. 38:1207–1212.
2017.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Jamil FA and Al-Adili SS: Lateral ridge
splitting (expansion) with immediate placement of endosseous dental
implant using piezoelectric device: A new treatment protocol. J
Craniofac Surg. 28:434–439. 2017.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Kheur MG, Kheur S, Lakha T, Jambhekar S,
Le B and Jain V: Does graft particle type and size affect ridge
dimensional changes after alveolar ridge split procedure? J Oral
Maxillofac Surg. 76:761–769. 2018.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Mahmoud ZT, Wainwright M and Troedhan A:
Flapless piezotome crest split achieves comparable outcomes to
autologous onlay grafts with significant less patient morbidity and
complications-a randomized clinical study. J Oral Maxillofac Surg.
78:1953–1964. 2020.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Elamrousy W, Osama M and Issa DR:
Autogenous bone and bioactive glass around implants placed
simultaneously with ridge splitting for the treatment of horizontal
bony defects: A randomised clinical trial. Int J Dent.
2021(2457328)2021.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Gultekin BA, Cansiz E and Borahan MO:
Clinical and 3-dimensional radiographic evaluation of autogenous
iliac block bone grafting and guided bone regeneration in patients
with atrophic maxilla. J Oral Maxillofac Surg. 75:709–722.
2017.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Halperin-Sternfeld M, Zigdon-Giladi H,
Shapira L and Wilensky A: Lateral guided bone regeneration using a
novel synthetic bioresorbable membrane: A two center prospective
randomized controlled trial running title: A novel membrane for
ridge augmentation. J Mol Clin Med. 1:169–176. 2018.
|
|
33
|
Meloni SM, Jovanovic SA, Urban I, Baldoni
E, Pisano M and Tallarico M: Horizontal ridge augmentation using
GBR with a native collagen membrane and 1:1 ratio of particulate
xenograft and autologous bone: A 3-year after final loading
prospective clinical study. Clin Implant Dent Relat Res.
21:669–677. 2019.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Mendoza-Azpur G, de la Fuente A, Chavez E,
Valdivia E and Khouly I: Horizontal ridge augmentation with guided
bone regeneration using particulate xenogenic bone substitutes with
or without autogenous block grafts: A randomized controlled trial.
Clin Implant Dent Relat Res. 21:521–530. 2019.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Zhang T, Zhang T and Cai X: The
application of a newly designed L-shaped titanium mesh for GBR with
simultaneous implant placement in the esthetic zone: A
retrospective case series study. Clin Implant Dent Relat Res.
21:862–872. 2019.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Amaral Valladão CA Jr, Freitas Monteiro M
and Joly JC: Guided bone regeneration in staged vertical and
horizontal bone augmentation using platelet-rich fibrin associated
with bone grafts: A retrospective clinical study. Int J Implant
Dent. 6(72)2020.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Işık G, Özden Yüce M, Koçak-Topbaş N and
Günbay T: Guided bone regeneration simultaneous with implant
placement using bovine-derived xenograft with and without liquid
platelet-rich fibrin: A randomized controlled clinical trial. Clin
Oral Investig. 25:5563–5575. 2021.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Ortega-Oller I, Suárez F, Galindo-Moreno
P, Torrecillas-Martínez L, Monje A, Catena A and Wang HL: The
influence of implant diameter on its survival: A meta-analysis
based on prospective clinical trials. J Periodontol. 85:569–580.
2014.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Sanz-Sánchez I, Ortiz-Vigón A, Sanz-Martín
I, Figuero E and Sanz M: Effectiveness of lateral bone augmentation
on the alveolar crest dimension: A systematic review and
meta-analysis. J Dent Res. 94 (9 Suppl):128S–142S. 2015.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Stevens MR, Ghasemi S and Tabrizi R (eds):
Innovative perspectives in oral and maxillofacial surgery.
Springer, Cham, 2021.
|
|
41
|
Sohn DS, Lee HJ, Heo JU, Moon JW, Park IS
and Romanos GE: Immediate and delayed lateral ridge expansion
technique in the atrophic posterior mandibular ridge. J Oral
Maxillofac Surg. 68:2283–2290. 2010.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Jha N, Choi EH, Kaushik NK and Ryu JJ:
Types of devices used in ridge split procedure for alveolar bone
expansion: A systematic review. PLoS One.
12(e0180342)2017.PubMed/NCBI View Article : Google Scholar
|