Introduction
Invasive mechanical ventilation (IMV) is one of the
most critical methods for determining patient outcomes in the
Intensive Care Units (ICUs) (1).
IMV is frequently used to treat patients with severe injuries,
poisoning, infectious diseases, neuromuscular diseases, chronic
obstructive pulmonary disease (COPD) and interstitial lung diseases
(2-4).
IMV is associated with a mortality rate of up to 13.1-51.0%
(5-7).
Although IMV is helpful to decrease the mortality rate, the
ultimate patient outcomes often do not change significantly. When
patients are admitted to the ICU, attending physicians must quickly
decide whether to initiate IMV, as time is of the essence. For this
purpose, the IMV Mortality Prediction Score (IMPRES) may represent
a good method to help physicians with decision-making (8,9).
IMPRES is a comprehensive index based on various clinical factors
that have been observed to be associated with the mortality rate in
ICU patients.
IMPRES considers factors such as patient age,
reasons for ICU admission, the severity of illness as measured by
scores such as the Acute Physiology and Chronic Health Evaluation
(APACHE)II or III score, and the number of days the patient has
been on mechanical ventilation (10-12).
By assessing these factors, IMPRES can provide physicians with a
valuable tool to estimate the likelihood of patient survival.
Furthermore, it helps to guide decision-making regarding treatment
options and care goals. However, the predictive value of the IMPRES
has remained to be defined. Therefore, the present study aimed to
explore the predictive value of the IMPRES and the duration of IMV
use for the mortality rate in patients with IMV use on day 28.
Patients and methods
Patients
The present study was a retrospective
cross-sectional cohort study conducted in a single medical center.
All data were obtained from the patient information database of the
Department of ICU of Renhe Hospital (Shanghai, China) between March
2018 and August 2020. A total of 129 patients were admitted to the
ICU of the hospital and received IMV over this period. The
inclusion criteria were as follows: i) Age >18 years; ii)
deterioration of the patient's condition despite being active; iii)
disturbance of consciousness; iv) aberrant breathing pattern,
including respiratory rate (RR) >35-40/min or <6-8/min,
abnormal breathing rhythm, and weak or absent spontaneous
breathing; v) severe ventilation and oxygenation disturbances
revealed by blood gas analysis or arterial partial pressure of
<50 mmHg despite full oxygen therapy; vi) progressive rise in
arterial partial pressure of carbon dioxide; and vii) progressive
decrease in blood pH. The exclusion criteria were as follows: i)
Transfer to the routine resuscitation of the intensive care
medicine department after surgery; ii) intubation for mechanical
ventilation to treat cardiac arrest; iii) patients who refused
treatment and were self-discharged. The study protocol was reviewed
and approved by the Ethics Committee of Shanghai Renhe Hospital
(Shanghai, China; approval no. KY2022-01). Written informed consent
was obtained from the patients that were willing to provide their
medical records. Data were collected following international
Conventions and guidelines on research involving human subjects,
such as the Declaration of Helsinki.
Data collection
The present study and data collection were performed
by the ICU specialists. Data were obtained from medical records,
medical histories and telephone follow-up records. They included
the anonymized name, which was recorded and given a code number,
age, sex, underlying diseases, Sequential Organ Failure Assessment
(SOFA) score (13), Acute
Physiology and Chronic Health Evaluation II (APACHEII) scores
(14) at admission and before
incubation, analgesia or sedation drugs use and vasopressor use.
The RR, heart rate (HR), oxygen saturation (SaO2),
systolic blood pressure, diastolic pressure, mean arterial pressure
(MAP) and duration of ventilator use (days) on day 28 in the ICU
were recorded.
IMPRES evaluation
After collecting the above data, the individual
IMPRES following the literature descriptions (8) was calculated based on parameters
provided in Table I.
 | Table IClinical parameters and Invasive
Mechanical Ventilation Mortality Prediction Score of patients. |
Table I
Clinical parameters and Invasive
Mechanical Ventilation Mortality Prediction Score of patients.
| Variable | Score |
|---|
| Age 70 years | 1.6 |
| Pulmonary edema | -0.5 |
| COPD | -0.6 |
| Interstitial lung
disease | 11.9 |
| Acute kidney
injury | 1.7 |
| Sepsis | 2.2 |
| Metabolic
encephalopathy | -0.3 |
| Neurodegenerative
disease | -0.2 |
| ICU-level monitoring
required | 16.7 |
| Type III pulmonary
failure | -0.3 |
| Heart failure | -0.7 |
| Lung cancer | 3.7 |
| Cardiac arrest | 1.9 |
| Lack of treatment
opportunities to prolong survival | 2.3 |
| Serious comorbidities
(at least one) | 2.3 |
| Expected survival
time is <6 months | 3 |
| Permanent organ
failure | 2.4 |
| Despite benefit from
treatment, little chance of recovery | 1.69 |
| High cost of
treatment to benefit | -0.3 |
| End stage of chronic
diseases and malignancies | 2.8 |
Outcome classification
Patients who survived for 28 days in the ICU were
assigned to the live group and those who had deceased to the dead
group. Critical factors for survival and death were determined and
compared.
Statistical analysis
Continuous variables are presented as the mean ±
standard deviation (SD) or the median with interquartile ranges
(IQR). Categorical variables are presented as percentages and
frequencies. The t-test and χ2 test were used to compare
continuous and categorical variables, respectively. Multivariate
Cox proportional hazards regression analysis was used to determine
the most impactful factors for model construction. A receiver
operating characteristic curve (ROC) analysis was performed and the
area under the ROC curve (AUC) was calculated to determine the most
impactful factors for predicting survival on day 28 in the ICU. The
Kaplan-Meier curves with the log-rank test were used to compare
overall survival (OS) on day 28 in the ICU. All statistical
analyses were performed using SPSS version 21.0 (IBM Corp.).
P<0.05 was considered to indicate statistical significance.
Results
Clinicopathological
characteristics
A total of 129 patients who received IMV treatment
in the ICU were enrolled in the present study. Their
clinicopathological characteristics are presented in Table II. This study included 70 males and
59 females. The patients were divided into dead and live groups
based on their statuses on day 28 in the ICU, and the cohort
included 56 dead and 73 live cases. The median age of the dead and
live groups was 85.0 years (range, 34-101 years) and 81.0 years
(range, 24-100 years, Table II),
respectively. Compared to the patients in the dead group, patients
in the live group had a significantly lower APACHEII score at
intubation, as well as SOFA and IMPRES scores (P<0.01). By
contrast, there were no marked differences in age, sex and APACHEII
scores at admission between the two groups (P>0.05). There were
no significant differences (P=0.058) between the intubation rate in
the live group (69.9%, 51/73) and the dead group (53.6%, 30/56) in
the first 24 h of admission. The average ICU hospitalization time
(31 days) in the live group was significantly longer than that in
the dead group (20 days; P=0.002) because of early death by day 28
in the ICU in the latter group.
 | Table IIClinicopathological characteristics of
patients receiving invasive mechanical ventilation treatment in the
ICU on day 28. |
Table II
Clinicopathological characteristics of
patients receiving invasive mechanical ventilation treatment in the
ICU on day 28.
| Variable | Dead (n=56) | Live (n=73) | z/χ2 | P-value |
|---|
| Age, years | 85.00 (75.25,
90.00) | 81.00 (69.50,
87.00) | -1.760 | 0.078 |
| APACHEII score at
admission | 29.50 (22.00,
33.75) | 26.00 (22.00,
31.50) | -1.432 | 0.157 |
| APACHEII score at
intubation | 33.00 (30.25,
36.75) | 28.00 (24.50,
32.50) | -3.901 | <0.001 |
| Sofa score | 12.00 (10.00,
15.00) | 10.00 (7.50,
12.00) | -3.025 | 0.002 |
| IMPRES | 6.30 (4.60,
8.53) | 3.80 (1.60,
5.70) | -5.548 | <0.001 |
| Male sex | 30 (53.60) | 40 (54.80) | 0.019 | 0.890 |
| Intubation in 24
h | 30 (53.60) | 51 (69.90) | 3.600 | 0.058 |
| Time at ICU,
days | 19.50 (11.50,
28.00) | 31.00 (15.50,
46.00) | -3.066 | 0.002 |
The distribution of major diseases upon ICU
admission was reviewed (Table
III). The results indicated that 69 patients (53.5%) had lung
infections when they were admitted to the ICU. The next most common
conditions were cerebral infarction (n=15, 11.6%), followed by
septic shock (n=12, 9.3%), gastrointestinal bleeding (n=8, 6.2%),
hyperosmolar coma (n=5, 3.9%), COPD (n=3, 2.3%), cerebral
hemorrhage (n=3, 2.3%), myocardial infarction (n=3, 2.3%), sleeping
pill poisoning (n=2, 1.6%) and cervical spine injury (n=2, 1.6%).
Other conditions included chest trauma, heat stroke, heart failure,
pneumothorax, lung cancer and renal failure (n=1, 0.8%).
 | Table IIIMain disease distribution on
admission to the intensive care unit. |
Table III
Main disease distribution on
admission to the intensive care unit.
| Disease | n (%) |
|---|
| Lung infection | 69 (53.5) |
| Cerebral
infarction | 15 (11.6) |
| Septic shock | 12 (9.3) |
| Gastrointestinal
bleeding | 8 (6.2) |
| Hyperosmolar
coma | 5 (3.9) |
| COPD | 3 (2.3) |
| Cerebral
hemorrhage | 3 (2.3) |
| Myocardial
infarction | 3 (2.3) |
| Sleeping pill
poisoning | 2 (1.6) |
| Cervical spine
injury | 2 (1.6) |
| Traumatic brain
injury | 1 (0.8) |
| Chest trauma | 1 (0.8) |
| Heat stroke | 1 (0.8) |
| Heart failure | 1 (0.8) |
| Pneumothorax | 1 (0.8) |
| Lung cancer | 1 (0.8) |
| Renal failure | 1 (0.8) |
Management comparison
To narrow the critical factors for predicting the
outcomes of ICU patients, their management and performances in the
ICU at day 28 were compared (Table
IV). Vasopressor use before intubation, HR, MAP at intubation,
duration of ventilator use (days) and ICU stay (days) were
significantly different between the dead and live groups
(P<0.05). By contrast, non-invasive ventilation before
intubation, analgesia and sedation before intubation,
SaO2 and RR at intubation did not differ significantly
between the two groups (P>0.05). In addition, underlying
diseases were compared and no significant differences were observed
between the two groups (Table SI).
These results revealed that vasopressor use before intubation, HR,
MAP at intubation, as well as the duration of ventilator use and
ICU stay, were the main determining factors for ICU patient
outcomes.
 | Table IVManagement and performance of
patients at the ICU on day 28. |
Table IV
Management and performance of
patients at the ICU on day 28.
| Variable | Death (n=56) | Live (n=73) |
z/χ2 | P-value |
|---|
| Intubation in 24
h | 30 (53.6) | 51 (69.9) | 3.600 | 0.058 |
| Vasopressor use
before intubation | 14 (25.0) | 7 (9.6) | 5.522 | 0.019 |
| Non-invasive
ventilation before intubation | 15 (26.8) | 19 (26.0) | 0.009 | 0.923 |
| Analgesia and
sedation before intubation | 7 (12.5) | 7 (9.6) | 0.278 | 0.598 |
| HR at intubation
(normal range, 75-128 bpm) | 97.0 (76.0,
110.8) | 105.0 (88.0,
125.0) | -2.455 | 0.014 |
| Oxygen saturation
during intubation (normal range, 95-100%) | 87.5 (71.3,
94.3) | 89.0 (72.5,
96.5) | -1.120 | 0.263 |
| RR at intubation
(normal range, 12-20 breaths/min) | 23.0 (18.0,
30.0) | 22.0 (16.0,
30.0) | -0.019 | 0.985 |
| MAP at intubation,
mmHg | 74.2 (54.4,
87.7) | 88.0 (72.3,
100.7) | -3.583 | <0.001 |
| Duration of
ventilator use, days | 8.5 (3.0,
13.0) | 13.0 (5.0,
34.5) | -2.971 | 0.003 |
| ICU time, days | 20.0 (11.5,
28.00) | 31.0 (15.5,
46.0) | -3.066 | 0.002 |
Binary logistic regression
analysis
To evaluate the critical factors for OS of ICU
patients on day 28, binary logistic regression analysis was
performed using the variables that differed significantly between
the dead and live groups. The IMPRES and duration of ventilator use
were identified as two independent factors for OS in ICU patients
on day 28 (P<0.05; Table V).
Among these two key factors, the IMPRES showed a negative
association with OS on day 28 (B=-0.417). By contrast, the duration
of ventilator use was positively associated with OS on day 28
(B=0.061). This result confirmed that the IMPRES was a critical
factor affecting OS in ICU patients receiving IMV on day 28.
 | Table VBinary logistic regression analysis
of overall survival on day 28 of patients receiving invasive
mechanical ventilation in the ICU. |
Table V
Binary logistic regression analysis
of overall survival on day 28 of patients receiving invasive
mechanical ventilation in the ICU.
| Parameter | B | S.E. | Wald | P-value | Exp (B) | 95% CI of
EXP(B) |
|---|
| SOFA score | -0.002 | 0.087 | 0.001 | 0.980 | 0.998 | 0.842-1.182 |
| IMPRES | -0.417 | 0.105 | 15.829 | 0.000 | 0.659 | 0.536-0.809 |
| Times in ICU | -0.008 | 0.014 | 0.384 | 0.536 | 0.992 | 0.966-1.018 |
| Age | -0.022 | 0.020 | 1.220 | 0.269 | 0.978 | 0.941-1.017 |
| APACHEII score at
intubation | -0.027 | 0.049 | 0.300 | 0.584 | 0.974 | 0.885-1.071 |
| Early
intubation | 0.887 | 0.527 | 2.831 | 0.092 | 2.429 | 0.864-6.828 |
| Duration of
ventilator use | 0.061 | 0.026 | 5.713 | 0.017 | 1.063 | 1.011-1.118 |
| Vasopressor | -0.455 | 0.683 | 0.443 | 0.506 | 0.635 | 0.166-2.421 |
| HR at
intubation | 0.003 | 0.010 | 0.059 | 0.808 | 1.003 | 0.982-1.023 |
| MAP at
intubation | 0.011 | 0.012 | 0.892 | 0.345 | 1.011 | 0.988-1.035 |
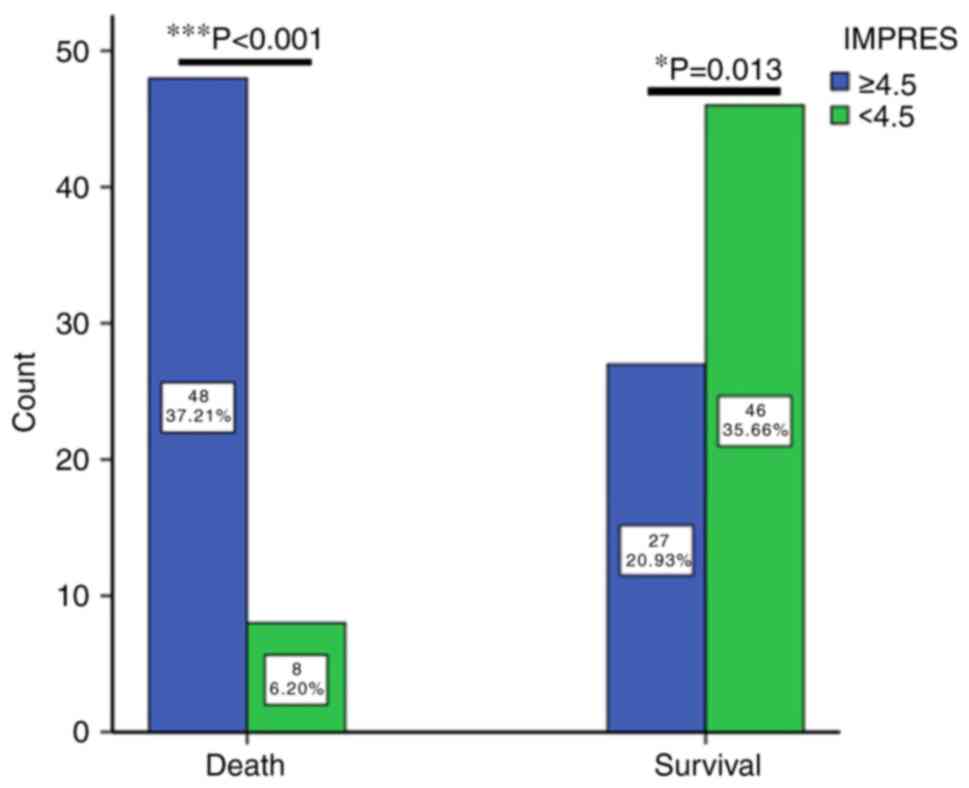
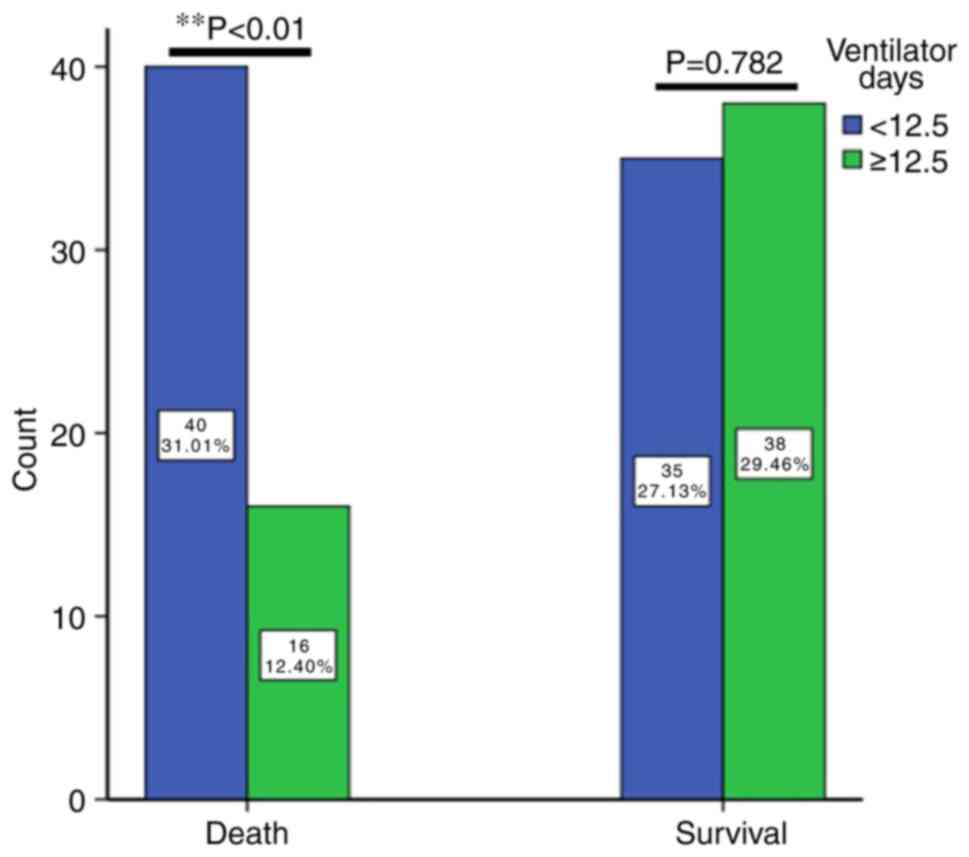
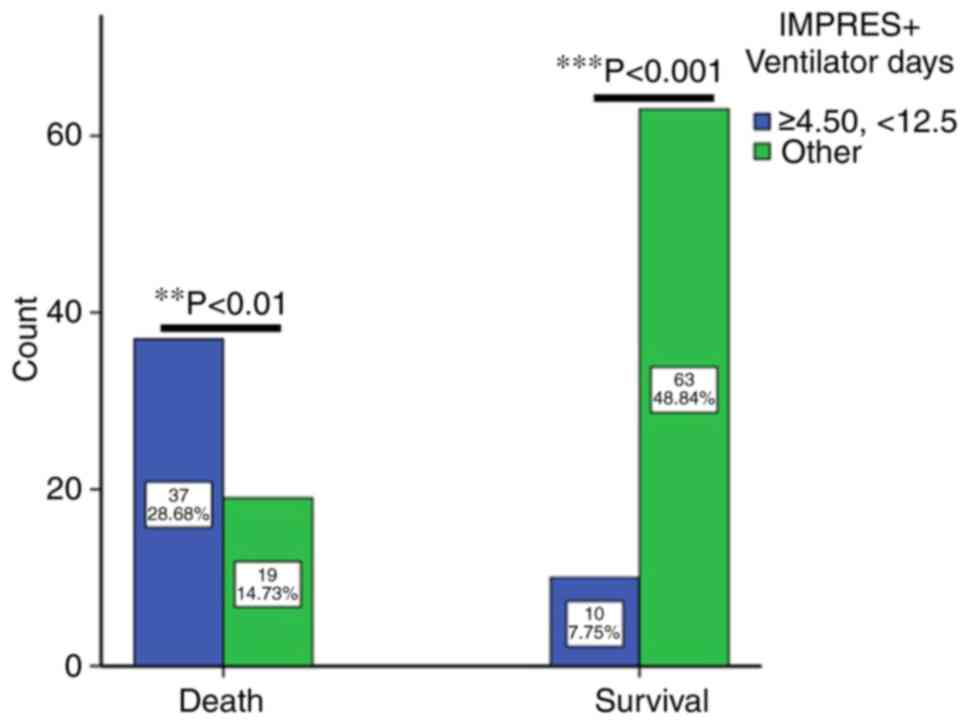
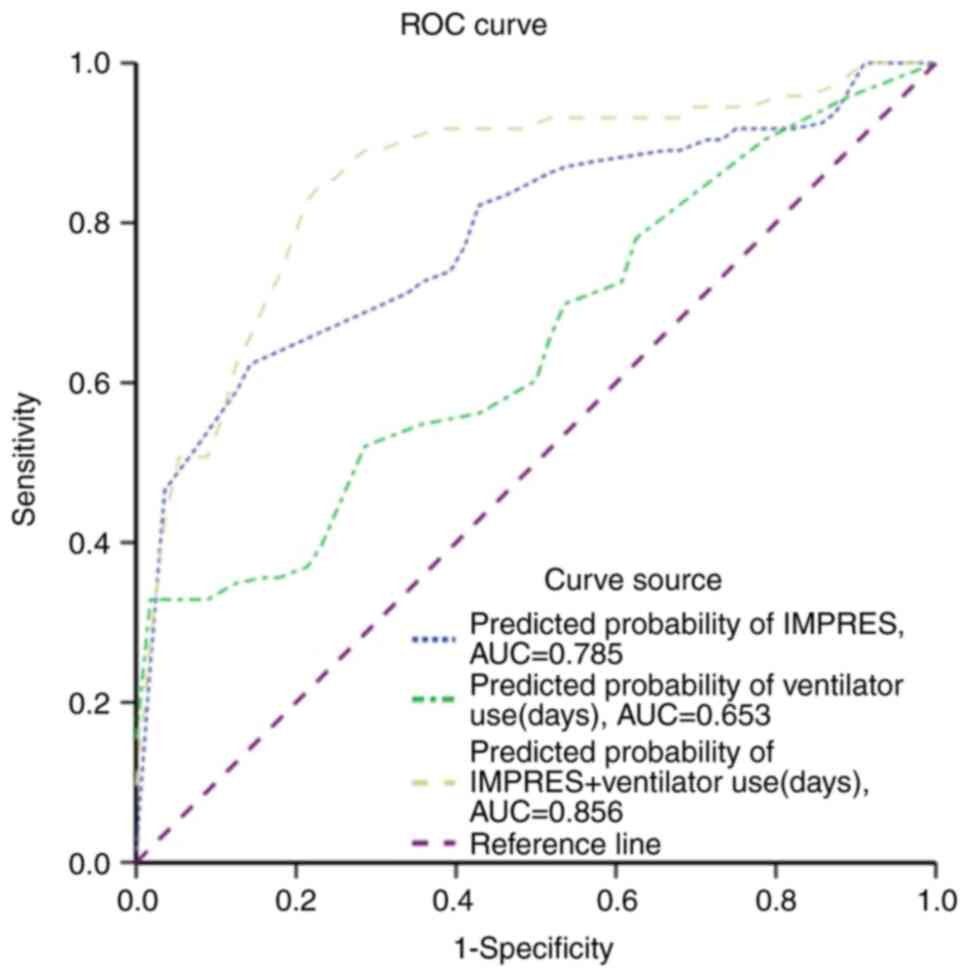
Predictive value of OS in ICU using an
independent factor combined predictive model
To more accurately predict the OS of ICU patients
with IMV on day 28, ROC curve analysis was performed and the AUC
was calculated using the two independent variables mentioned above
(Table VI). The IMPRES showed the
following results at a cut-off of 4.50: AUC, 0.785; 95% CI,
0.706-0.864; P<0.001; sensitivity, 63.0%; specificity, 85.7%;
and Youden index, 0.487. When the IMPRES score was <4.50, OS was
higher on day 28. Regarding the duration of ventilator use (days),
the results were as follows with 12.50 days as the cut-off: AUC,
0.653; 95% CI, 0.560-0.746; P=0.003 sensitivity, 52.1%;
specificity, 71.4%, and Youden index, 0.235. When the duration of
ventilator use was <12.5 days, the OS of ICU patients with IMV
was lower. The OS of ICU patients with IMV on day 28 divided into
high and low groups according to the cut-off of the IMPRES score
and duration of ventilator use is shown in Fig. 1, Fig.
2 and Fig. 3. If survival
fractions were compared in the dead and live groups using an IMPRES
of 4.5 as the cut-off, the number of patients with IMPRES 4.5 vs.
<4.5 in the dead and live groups was 48/8 (37.21 vs. 6.20%) and
27/46 (20.93 vs. 35.66%), respectively. There were significant
differences (P<0.001) in the number of patients with IMPRES 4.5
between the dead and live groups (Fig.
1). Furthermore, the number of patients at a cut-off for
ventilator time of 12.5 days in the dead and live groups was 40/16
(30.01 vs. 12.40%) and 35/38 (27.1 vs. 29.5%, P=0.782),
respectively (Fig. 2). The analysis
was then performed using the combination of an IMPRES of 4.5
combined with ventilator use for <12.5 days, and it was observed
that the number of patients with IMPRES 4.5 combined with
ventilator use <12.5 days, and the respective other group, which
included patients with IMPRES not 4.5 and ventilator use not
<12.5 days, in the dead and live groups was 37/19 (28.68 vs.
14.73%, P<0.01) and 10/63 (7.75 vs. 48.84%), respectively
(Fig. 3). By contrast, the number
(10/129, 7.75%) of patients with IMPRES 4.5 combined with
ventilator use <12.5 days in the live group was markedly lower
than number of patients in the other group (63/129, 48.84%,
P<0.001). These data indicated a strong differentiation in the
outcomes of ICU patients using the IMPRES and duration of
ventilator use with cut-off values of 4.5 and <12.5 days,
respectively.
 | Table VIComparison of AUC, Youden index,
sensitivity and specificity of independent risk factors in the ROC
analysis. |
Table VI
Comparison of AUC, Youden index,
sensitivity and specificity of independent risk factors in the ROC
analysis.
| Parameter | AUC | S.D. | P-value | 95% CI | Cut-off | Youden index | Sensitivity | Specificity |
|---|
| IMPRES | 0.785 | 0.040 | <0.001 | 0.706-0.864 | 4.50 | 0.487 | 0.857 | 0.630 |
| Duration of
ventilator use, days | 0.653 | 0.048 | 0.003 | 0.560-0.746 | 12.50 | 0.235 | 0.521 | 0.714 |
| IMPRES + duration
of ventilator use, days | 0.856 | 0.034 | <0.001 | 0.789-0.922 | 4.5 + 12.5 | 0.635 | 0.849 | 0.786 |
The parameters from the ROC curve to predict patient
survival based on the IMPRES combined with ventilator use are
provided in Tables V and VI. The results indicated a maximum AUC
(0.856) and 95% CI (0.789-0.922, P<0.01) with the combination of
the IMPRES plus the duration of ventilator use (Fig. 4). The sensitivity and specificity
were 84.9 and 78.6%, respectively. This result confirmed that the
combination of the IMPRES score and duration of ventilator use
showed the greatest efficacy for accurately predicting survival of
ICU patients.
Comparison of OS of hospitalized
patients by the Kaplan-Meier method
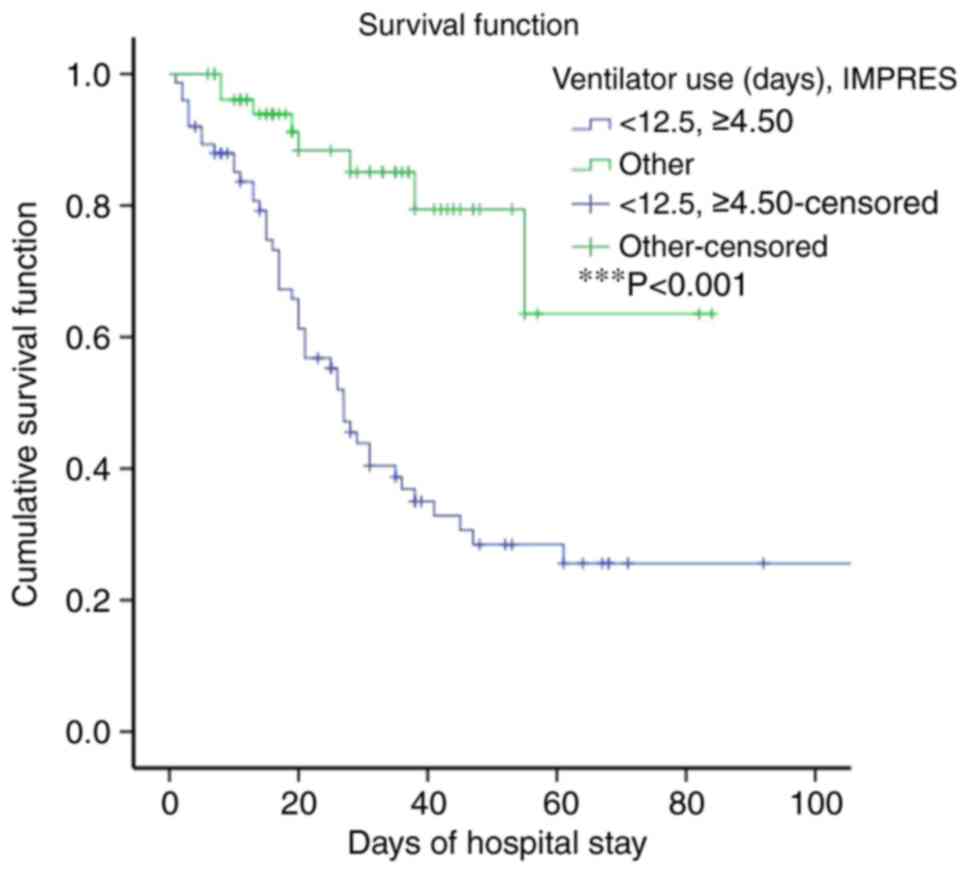
To further investigate the survival conditions at
the time of hospitalization, the follow-up period was lengthened up
to 100 days and an OS analysis was performed using the Kaplan-Meier
method, based on the number of live and dead patients (Fig. 5). The mortality rate (78.7%) of
patients with IMPRES ≥4.5 and <12.5 days of ventilator use was
much higher than that in the other groups (23.2%, P<0.001). This
result demonstrated that IMPRES ≥4.50 plus <12.5 days of
ventilator use in combination has a high predictive value for
favorable outcomes for ICU patients with IMV.
Discussion
The mortality rate of ICU patients receiving IMV is
excessively high. Predicting critical factors for patient survival
can significantly improve outcomes in this patient group. Our data
indicated that the IMPRES and the length of ventilator use (days)
were two major independent factors for ICU patient survival on day
28. Among these factors, the IMPRES is an important factor for
predicting OS. However, the IMPRES plus length of ventilator use
had a greater predictive value for ICU patient survival than either
factor alone.
The mortality rate of adult ICU patients ranges
between 10.1-45.1% and is related to acute organ dysfunctions
(15,16). By contrast, the mortality rate of
ICU patients with IMV is higher than that of patients without IMV
because IMV use is frequently associated with organ failure
(17) and prolonged intubation
markedly increases ventilator-acquired pneumonia (18). Therefore, numerous studies have
attempted to predict the mortality rate of ICU patients using
different strategies (19-21).
However, these evaluation systems have certain limitations. For
example, patients with cancer or organ transplantation have
relatively low mortality rates according to the Simplified Acute
Physiology Score 3 system (22). By
contrast, the SOFA score is more helpful for predicting the
mortality of patients with sepsis (22-24).
Currently, most physicians use the APACHE score to predict the
severity of disease. However, this score has a relatively low
predictive value in patients undergoing neurosurgery (25). Another report revealed that the
APACHEIII score and surgery type were strong predictors of
mortality in ICU patients (26).
Recently, machine learning models were used to predict the
mortality rate at 30 days after IMV use (9,27) and
higher AUC values were reported for this approach compared to
conventional scoring systems. Chan et al (27) reported on 30-day, 90-day and 1-year
mortality prediction in ICU patients, indicating higher AUC values
in short-term follow-up using independent predictive factors.
Another study showed that the intensity of oxygen exposure in ICU
patients receiving IMV were a critical factor for their outcomes on
day 28(5). Therefore, day 28 was
selected as the cut-off time in the present study. The current
study aimed to determine the critical factors for predicting
survival in ICU patients on IMV on day 28. It was observed that the
APACHEII and SOFA score were not determining factors for the
survival rate on day 28, although the APACHEII and SOFA score in
the dead group were significantly higher than those in the live
group. This bias may have occurred because all of the patients with
high APACHEII and SOFA scores underwent IMV.
To the best of our knowledge, the present study was
the first to use individual variables to evaluate the key factors
for predicting mortality in ICU patients receiving IMV on day 28.
Binary logistic regression and ROC curve analysis were used to
narrow down the critical factors related to outcomes in this
patient group. It was observed that the IMPRES and length of
ventilator use were the two most critical factors for this
application. Ozlu et al (8)
analyzed the mortality rate of 1,463 cases in 41 ICUs using the
IMPRES method, including 583 patients on IMV and 880 patients who
did not receive IMV. Their results showed that the IMPRES helped to
predict outcomes in the ICU patients on IMV. They selected 20
variables from the initial 158 variables and established evaluation
criteria using different mortality risk values. Compared to other
mortality predictive methods in the ICU patients, the IMPRES
utilizes not only available clinical data, but also takes into
account the physician's subjective anticipation. The results
provided a more accurate prediction than other methods such as the
APACHEII or SOFA scores (8). This
method may be a superior measure for short-term mortality
prediction because the physician makes a decision based on bedside
data collection for patients at the ICU receiving IMV. Their
results showed that 76.3% of patients with an IMPRES of 5.1 died.
The present study showed that patients with an IMPRES of 4.50 had a
mortality rate of 78.7% on day 28. The present result thus
confirmed that the IMPRES was a critical variable for predicting
mortality in ICU patients on IMV.
The mortality rate of ICU patients on IMV can be
impacted by various factors, such as pneumonia caused by ventilator
use (28). One study reported that
the duration of ventilator use represented another critical factor
for predicting outcomes in ICU patients on IMV, as longer
ventilator use could cause nosocomial infection, raising both
ethical and legal concerns (29).
Therefore, the optimal length of ventilator use represents another
key issue for predicting mortality in ICU patients. In the present
study, binary logistic regression and ROC curve analyses were used
to determine the critical factors affecting the outcomes of ICU
patients on IMV. The present results indicated that patients with
IMPRES <4.5 or duration of ventilator use 12.5 days have a
probability of long survival. Otherwise, patients' survival
probability was low. In addition, the combination of IMPRES and
length of ventilator use <12.5 days had a greater predictive
ability than either factor alone.
The present study had several key limitations worth
noting. First, the sample size was relatively small. Furthermore,
it was a retrospective study and certain data may have been missed.
In addition, the data were from a single center and may have been
affected by the physicians' experiences. Therefore, a prospective
study with a large sample size across multiple centers may further
confirm our observations.
In conclusion, the present study confirmed that the
IMPRES and duration of ventilator use represent two critical
factors for predicting mortality in ICU patients receiving IMV.
Those patients with an IMPRES of 4.5 or <12.5 days of ventilator
use had high mortality rates in the present study cohort. The
combination of the IMPRES and duration of ventilator use exhibited
a greater predictive power than either factor alone. This
conclusion will be helpful in assisting ICU physicians with
clinical decision-making.
Supplementary Material
Comparison of the underlying diseases
in the dead and live groups.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets are not publicly available due to
ethical restrictions but may be requested from the corresponding
author.
Authors' contributions
SZ and ZZ conceived and designed the study. SZ and
HY were responsible for data collection. HY and ZZ analyzed the
results. SZ and ZZ prepared all figures and tables. SZ wrote the
initial draft of the manuscript. Each author revised portions of
the manuscript, and all authors have read and approved the final
manuscript. SZ and ZZ checked and confirmed the authenticity of the
raw data.
Ethics approval and consent to
participate
The study protocol was reviewed and approved by the
Ethics Committee of Shanghai RenHe Hospital (Shanghai, China;
approval no. KY2022-01). Written informed consent was obtained from
the patients that were willing to provide their medical records.
Data were collected in accordance with international conventions
and guidelines on research involving human subjects, such as the
declaration of Helsinki.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Wunsch H, Linde-Zwirble WT, Angus DC,
Hartman ME, Milbrandt EB and Kahn JM: The epidemiology of
mechanical ventilation use in the United States. Crit Care Med.
38:1947–1953. 2010.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Souza SM, Quintao APC, Soares MCB, Mendes
IR, Freitas BAC, Siman AG and Toledo LV: Survival of patients with
diabetes mellitus hospitalized for acute respiratory syndrome due
to COVID-19. Rev Inst Med Trop Sao Paulo. 64(e74)2022.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Chen X, Zhang J, Yuan S and Huang H:
Remimazolam besylate for the sedation of postoperative patients
undergoing invasive mechanical ventilation in the ICU: A
prospective dose-response study. Sci Rep. 12(19022)2022.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Smith MA, Dinh D, Ly NP, Ward SL, McGarry
ME and Zinter MS: Changes in the use of invasive and noninvasive
mechanical ventilation in pediatric asthma: 2009-2019. Ann Am
Thorac Soc. 20:245–253. 2023.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Zhu Z, Zhou M, Wei Y and Chen H:
Time-varying intensity of oxygen exposure is associated with
mortality in critically ill patients with mechanical ventilation.
Crit Care. 26(239)2022.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Plotnikow GA, Gogniat E, Accoce M, Navarro
E and Dorado JH: EpVAr study group. Epidemiology of mechanical
ventilation in Argentina. The EpVAr multicenter observational
study. Med Intensiva (Engl Ed). 46:372–382. 2022.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Fialkow L, Farenzena M, Wawrzeniak IC,
Brauner JS, Vieira SR, Vigo A and Bozzetti MC: Mechanical
ventilation in patients in the intensive care unit of a general
university hospital in southern Brazil: An epidemiological study.
Clinics (Sao Paulo). 71:144–151. 2016.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Ozlu T, Pehlivanlar Kucuk M, Kaya A, Yarar
E, Kirakli SC, Sengoren Dikis O, Kefeli Çelik H, Özkan S, Bektaş
Aksoy H and Küçük AO: IMVICAP Study Group. Can we predict patients
that will not benefit from invasive mechanical ventilation? A novel
scoring system in intensive care: The IMV Mortality Prediction
Score (IMPRES). Turk J Med Sci. 49:1662–1673. 2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Kim JH, Kwon YS and Baek MS: Machine
learning models to predict 30-day mortality in mechanically
ventilated patients. J Clin Med. 10(2172)2021.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Sudarsanam TD, Jeyaseelan L, Thomas K and
John G: Predictors of mortality in mechanically ventilated
patients. Postgrad Med J. 81:780–783. 2005.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Innocenti F, Lazzari C, Paolucci E, De
Paris A, Lagomarsini A, Guerra F, Alleonato P, Casalini L, Buggea
M, Caldi F, et al: Role of prognostic scores in predicting
in-hospital mortality and failure of non-invasive ventilation in
adults with COVID-19. Intern Emerg Med. 17:2367–2377.
2022.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Liang J, Li Z, Dong H and Xu C: Prognostic
factors associated with mortality in mechanically ventilated
patients in the intensive care unit: A single-center, retrospective
cohort study of 905 patients. Medicine (Baltimore).
98(e17592)2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Vincent JL, Moreno R, Takala J, Willatts
S, De Mendonca A, Bruining H, Reinhart CK, Suter PM and Thijs LG:
The SOFA (Sepsis-related Organ Failure Assessment) score to
describe organ dysfunction/failure. On behalf of the Working Group
on Sepsis-Related Problems of the European Society of Intensive
Care Medicine. Intensive Care Med. 22:707–710. 1996.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Knaus WA, Draper EA, Wagner DP and
Zimmerman JE: . APACHE II: A severity of disease classification
system. Crit Care Med. 13:818–829. 1985.PubMed/NCBI
|
|
15
|
Depuydt PO, Benoit DD, Vandewoude KH,
Decruyenaere JM and Colardyn FA: Outcome in noninvasively and
invasively ventilated hematologic patients with acute respiratory
failure. Chest. 126:1299–1306. 2004.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Azoulay E, Mokart D, Rabbat A, Pene F,
Kouatchet A, Bruneel F, Vincent F, Hamidfar R, Moreau D, Mohammedi
I, et al: Diagnostic bronchoscopy in hematology and oncology
patients with acute respiratory failure: Prospective multicenter
data. Crit Care Med. 36:100–107. 2008.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Grasselli G, Zangrillo A, Zanella A,
Antonelli M, Cabrini L, Castelli A, Cereda D, Coluccello A, Foti G,
Fumagalli R, et al: Baseline characteristics and outcomes of 1591
patients infected with SARS-CoV-2 Admitted to ICUs of the Lombardy
Region, Italy. JAMA. 323:1574–1581. 2020.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Melsen WG, Rovers MM, Groenwold RH,
Bergmans DC, Camus C, Bauer TT, Hanisch EW, Klarin B, Koeman M,
Krueger WA, et al: Attributable mortality of ventilator-associated
pneumonia: A meta-analysis of individual patient data from
randomised prevention studies. Lancet Infect Dis. 13:665–671.
2013.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Mahmoodpoor A, Sanaie S, Saghaleini SH,
Ostadi Z, Hosseini MS, Sheshgelani N, Vahedian-Azimi A, Samim A and
Rahimi-Bashar F: Prognostic value of National Early Warning Score
and Modified Early Warning Score on intensive care unit readmission
and mortality: A prospective observational study. Front Med
(Lausanne). 9(938005)2022.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Yang J, Lim HG, Park W, Kim D, Yoon JS,
Lee SM and Kim K: Development of a machine learning model for the
prediction of the short-term mortality in patients in the intensive
care unit. J Crit Care. 71(154106)2022.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Fronczek J, Flaatten H, Guidet B, Polok K,
Andersen FH, Andrew BY, Artigas A, Beil M, Cecconi M, Christensen
S, et al: Short-term mortality of patients >/=80 years old
admitted to European intensive care units: An international
observational study. Br J Anaesth. 129:58–66. 2022.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Costa e Silva VT, de Castro I, Liano F,
Muriel A, Rodriguez-Palomares JR and Yu L: Performance of the
third-generation models of severity scoring systems (APACHE IV,
SAPS 3 and MPM-III) in acute kidney injury critically ill patients.
Nephrol Dial Transplant. 26:3894–3901. 2011.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Soares M, Silva UV, Teles JM, Silva E,
Caruso P, Lobo SM, Dal Pizzol F, Azevedo LP, de Carvalho FB and
Salluh JI: Validation of four prognostic scores in patients with
cancer admitted to Brazilian intensive care units: Results from a
prospective multicenter study. Intensive Care Med. 36:1188–1195.
2010.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Patrizio E, Zambon A, Mazzola P,
Massariello F, Galeazzi M, Cavalieri d'Oro L, Bonfanti P and
Bellelli G: Assessing the mortality risk in older patients
hospitalized with a diagnosis of sepsis: The role of frailty and
acute organ dysfunction. Aging Clin Exp Res. 34:2335–2343.
2022.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Akavipat P, Thinkhamrop J, Thinkhamrop B
and Sriraj W: Acute physiology and chronic health evaluation
(Apache) Ii score - the clinical predictor in neurosurgical
intensive care unit. Acta Clin Croat. 58:50–56. 2019.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Zhang AT, Tan SX, Pillay PS and Stewart D:
A critical decision point: Short- and long-term outcomes of older
surgical patients admitted to a Queensland intensive care unit.
Australas J Ageing. 41:e32–e40. 2022.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Chan MC, Pai KC, Su SA, Wang MS, Wu CL and
Chao WC: Explainable machine learning to predict long-term
mortality in critically ill ventilated patients: A retrospective
study in central Taiwan. BMC Med Inform Decis Mak.
22(75)2022.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Wang M, Wang W, Jia X, He Q, Zhu S, Kang
Y, Zhang R, Ren Y, Li L, Zou K, et al: Associations between
antithrombosis and ventilator-associated events, ICU stays, and
mortality among mechanically ventilated patients: A registry-based
cohort study. Front Pharmacol. 13(891178)2022.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Esteban A, Frutos-Vivar F, Muriel A,
Ferguson ND, Penuelas O, Abraira V, Raymondos K, Rios F, Nin N,
Apezteguía C, et al: Evolution of mortality over time in patients
receiving mechanical ventilation. Am J Respir Crit Care Med.
188:220–230. 2013.PubMed/NCBI View Article : Google Scholar
|