Introduction
Isthmocele, also referred to as a scar niche from a
caesarean section, is characterized by an indentation exceeding 2
mm, representing myometrial discontinuity at the site of the
previous C-section scar, in the anterior wall of the lower uterine
segment (1).
Based on the most recent statistics regarding C
section rates in the world, Romania is the 3rd leading country,
with a rate of 443.2 caesarian sections per 1,000 live births
(2). Official data from 2010
indicate a rate of 338.2 C-sections per 1,000 live births,
indicating an increase of 31.05% (2). The prevalence of isthmocele has
increased in tandem with the rise in deliveries by caesarean
section.
Considering the implications of having an isthmocele
and the rising number of births by C-section, a great number of
individuals are exhibiting long-term effects (3). This has underscored the significance
of diagnosing isthmoceles, which has become more accessible and
essential than in the past (3).
Knowledge about what to look for has streamlined the diagnostic
process (3). The diagnosis can be
made by transvaginal ultrasound, MRI or hysterosalpingography, by
observing the extension of the contrast substance at the site of
the defect (1). The estimated
prevalence of isthmocele is as high as 70%, with ~30% of the
patients experiencing symptoms (4).
Risk factors associated with the development of a
niche are lower uterine incision, the presence of cervical dilation
>5 cm, C-section after labor with a duration of more than 5 h
(5,6). Furthermore, several factors related to
surgical technique have been investigated, such as the number of
myometrial layers used for the uterine closure (7), the use of locking sutures, non-locking
sutures or interrupted sutures, the anatomical approximation of the
myometrial margins with the suture of the whole layer, including
the decidua (5,8-10).
Additionally, certain risk factors have been identified that
increase the likelihood of isthmocele development, including the
position of the uterus, high number of C-sections in the past and
high BMI (5).
The prevalent gynecological complications associated
with the presence of an isthmocele are pelvic adhesions, chronic
pelvic pain, menometrorrhagia and subfertility or even infertility
(3,11). Additionally, secondary amenorrhea
has been documented in medical literature (6).
Regarding secondary infertility, it is considered to
stem from diminished mucus quality during the follicular phase,
impacting sperm mobility and implantation (12). Additionally, fertility challenges
are attributed in part to an inflammatory response, resembling the
impact of chronic inflammation and oxidative stress observed in
conditions such as endometriosis (5,13).
Menometrorrhagia is likely a result of blood
accumulation at the site of the defect, leading to persistent
spotting (12). The lymphocytic
infiltration, anatomical distortion and abnormal continuous
contraction of the myometrium with the purpose of emptying the
niche, are part of the etiopathogenesis of the chronic pelvic pain
(12).
In addition to the aforementioned gynecological
complications, the presence of an isthmocele during subsequent
pregnancies can be associated with various issues, including
ectopic pregnancy with implantation in the uterine scar, placenta
previa potentially accompanied by spectrum accreta, or uterine
rupture (3,11).
Considering the diverse aspects of isthmocele, there
are a few classification systems that could be used, although none
of them are standardized (4,12). One
possible classification is based on ultrasound measurements,
grading the niche by the ratio between its depth and the residual
myometrium thickness, with a ratio >50% indicating a severe
niche (12). Additionally, the
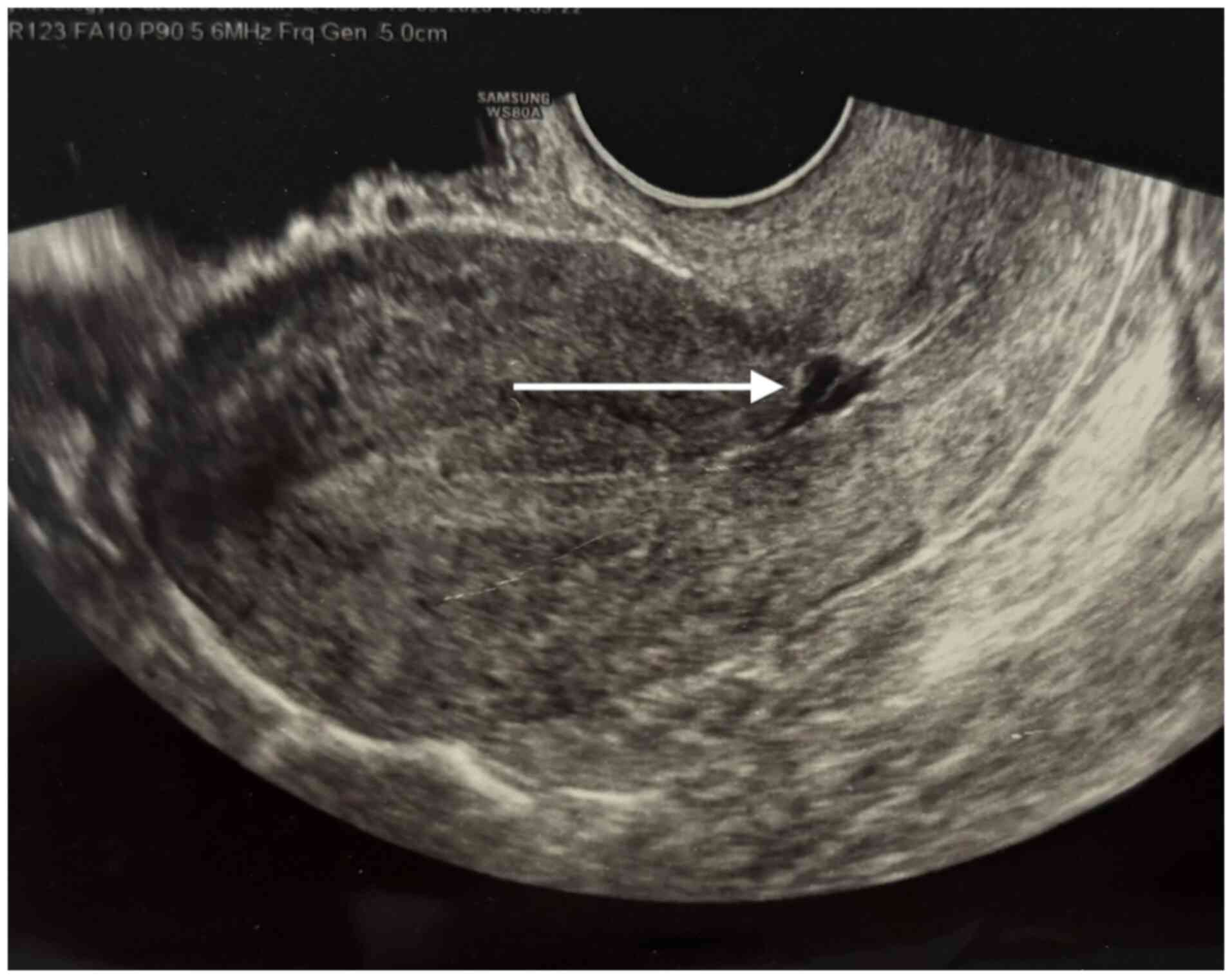
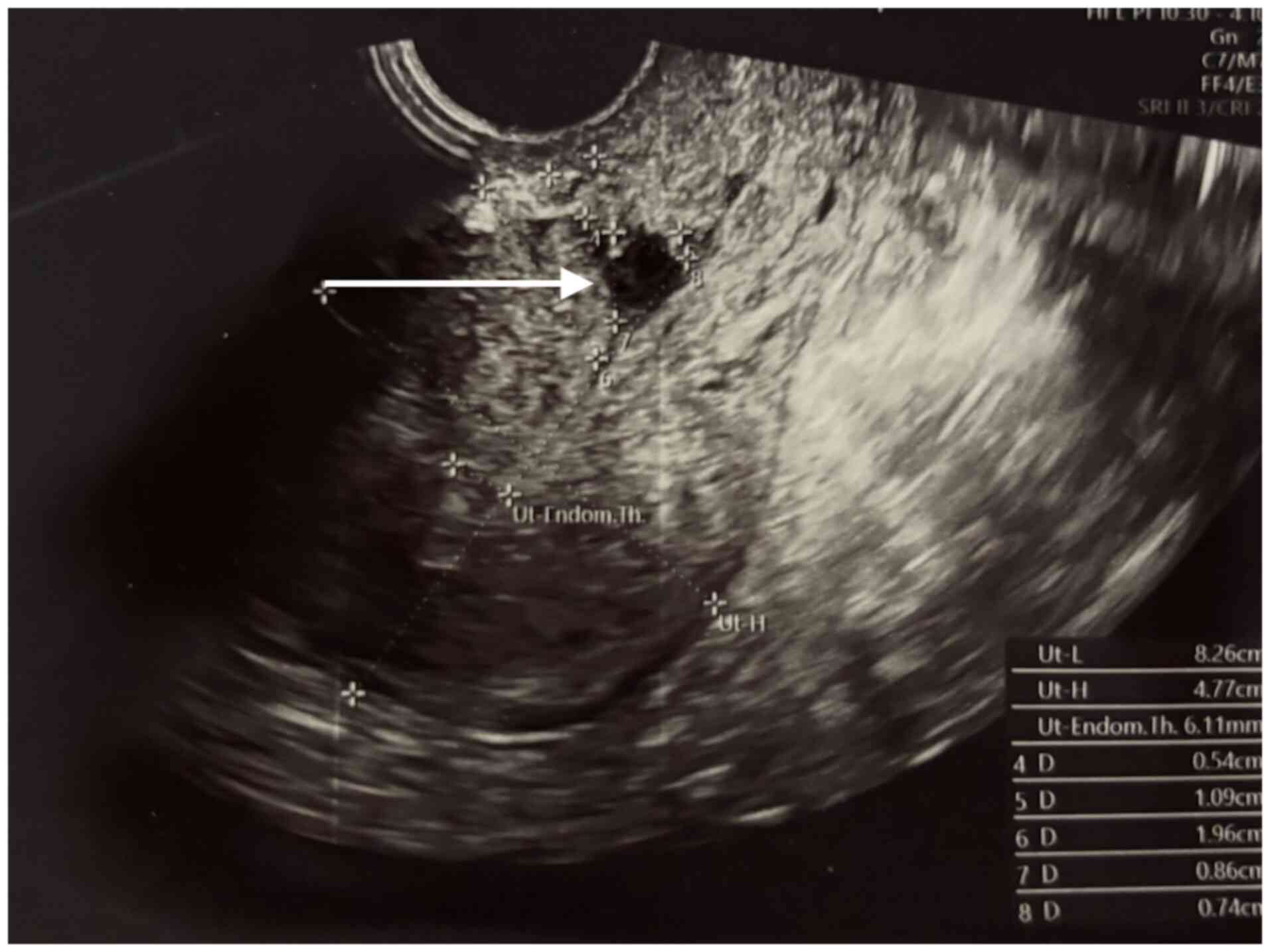
isthmocele can be classified by its shape-triangular (as observed
in Figs. 1 and 2), semicircular (as observed in Figs. 3 and 4), rectangular, droplet or inclusion
cysts, with the first two being the most common (4,14).
The decision to treat an isthmocele is based on a
few factors, including the size of the niche, the severity of the
symptoms, the presence of secondary infertility and whether the
patient wishes to obtain a pregnancy (12). Routine treatment is not recommended
for patients incidentally diagnosed with an asymptomatic niche, who
do not wish to conceive (4).
The surgical treatment can be performed by
hysteroscopy, transabdominally (laparotomy, laparoscopy or
robot-assisted), vaginally or a combination of hysteroscopy and
laparoscopy (4,15). Hysterectomy stands as a definitive
treatment for gynecological symptoms caused by the presence of the
isthmocele (4).
Materials and methods
The present study constitutes a prospective analysis
involving 52 women who were assessed 6 weeks postpartum after
delivery via caesarian section at the Saint Pantelimon Emergency
Clinical Hospital (Bucharest, Romania). The data collection period
spanned from April 1, 2022 to April 1, 2023. The primary evaluation
methods in the present study involved transvaginal ultrasound
examinations and comprehensive anamnestic assessments. All patients
signed written informed consent for the use of their data and
associated images in research upon admission to the Obstetrics and
Gynecology department (Bucharest, Romania).
The hypothesis of the present study posited that
certain types of hysterorraphy associate more frequently with the
development of the niche. With their purpose to confirm the
hypothesis, these specific objectives were formulated: (i) The
identification of anamnestic characteristics and uterine anatomy,
through detailed anamnesis and transvaginal ultrasound; (ii) the
evaluation of the niche and its ultrasound associated
characteristics, such as depth, total myometrial thickness,
residual myometrial thickness, severity degree (depth/total
myometrial thickness ratio); (iii) the evaluation of the shape of
the niche; (iv) the selection of patients with severe niches
(ratio>50%); and (v) the evaluation of hysterorraphy type based
on number of layers, type of suture (continuous locking, continuous
non-locking or interrupted), the thickness of the thread and
presence or absence of peritonization.
The inclusion criteria for patient selection were as
follows: Individuals aged 18 years or older, patients who had
undergone a caesarean section at ‘Saint Pantelimon’ Hospital
(Bucharest, Romania) within the specified timeframe, patients who
attended the 6-week postpartum medical examination, and patients
who provided informed consent to participate in the present
study.
The exclusion criteria encompassed individuals
younger than 18 years old, those who had a vaginal birth, patients
who had a C-section at a different hospital, patients for whom
surgical technique information was unavailable, and patients who
refused to participate in the present study.
To construct the database, a complementary document
was utilized to record all pertinent information. In addition to
this documentation, the physician had access to the patient's
medical records, the birth registry and the C-section registry. The
elements of descriptive statistics included the following: (i)
Quantitative variables-age (in years completed), number of previous
births by C-sections and the presence of labor prior to surgery;
(ii) Qualitative dichotomous variables-presence of niche-yes/no;
presence of peritonization-yes/no; presence of homogenous
myometrium- yes/no; and (iii) qualitative nominal variables-anatomy
(position of the uterus and size), depth of niche, the thickness of
the residual myometrium, total thickness of the myometrium, ratio
depth/myometrial total thickness, niche shape, number of layers
during uterine closure, type of suture of the first layer +/- type
of suture of the second layer.
After collecting the data, all information was
integrated in Excel, for the statistical analysis using SPSS
Statistics for Windows, version 29.0 (IBM Corp.). Continuous
variables were expressed using mean value, median, standard
deviation, minimum and maximum, while the categorial variables were
presented as absolute frequency and percentage. The association
between categorical variables was analyzed using the
cross-tabulation table and the chi-square test. In cases where the
chi-square test results were significantly altered, the Fisher's
exact test was used. For comparing the means based on dichotomous
variables in the study, the independent samples t-test was used. To
compare three or more means of groups, the ANOVA test was used,
followed by a Bonferroni post hoc test. P<0,05 was considered to
indicate a statistically significant difference.
Results
The initial segment of the results focused on
descriptive analysis. The first variable examined was the age of
the patients. The mean age was 30,42 years, with values ranging
from 20 to 46 years old. This seemingly higher mean age in the
present study could be attributed to the tendency of younger
patients to bypass prenatal and postpartum check-ups more
frequently, compared with those who are older, resulting in a
skewed average age.
Based on the presence of previous births by
C-section, 26.9% of patients had only one previous caesarean
section. Also, only 9.6% of the patients were in labor prior to the
C-section.
In terms of uterine anatomy and position, the
present study examined the positioning of the uterus. In two thirds
of cases, the uterus was found to be in anteversion, while 19.2% of
the patients had a retroverted uterus and 13.5% of them had the
uterus in an intermediate position.
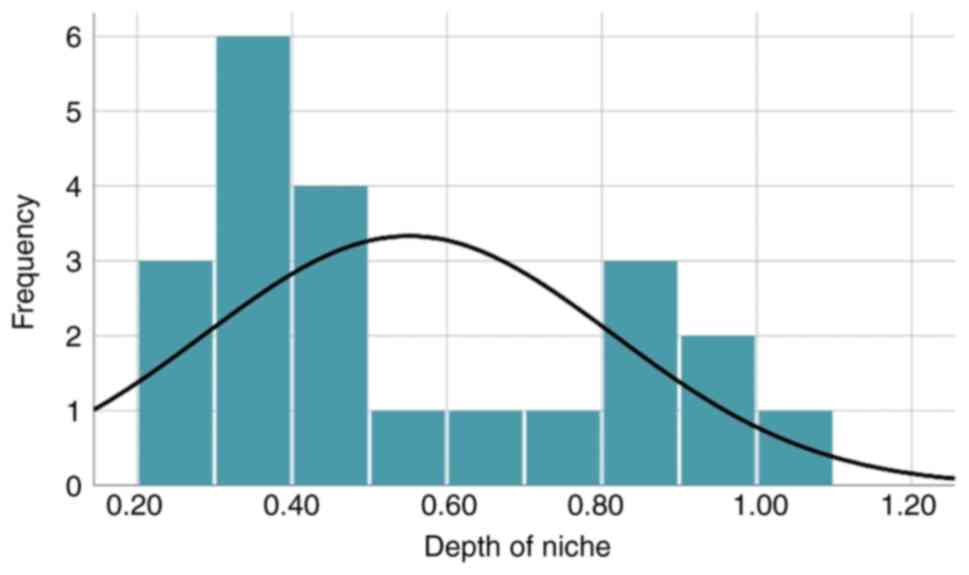
Out of the 52 patients included in the present
study, 22 patients were observed to have an isthmocele, resulting
in a prevalence of 42.3%. The results indicated that the mean depth
of the niches was 0.55 cm and the maximum depth found in the
present study was 1.01 cm. The distribution of patients included in
the present study according to the depths of the niches is
demonstrated in Fig. 5. These data
are presented in Table SI, as
supplementary data.
The thickness of the residual myometrium revealed a
mean of 0.84 cm, with a median of 0.86 cm. When analyzing the
patients with respect to the overall thickness of the myometrium,
the mean was calculated to be 1.46 cm.
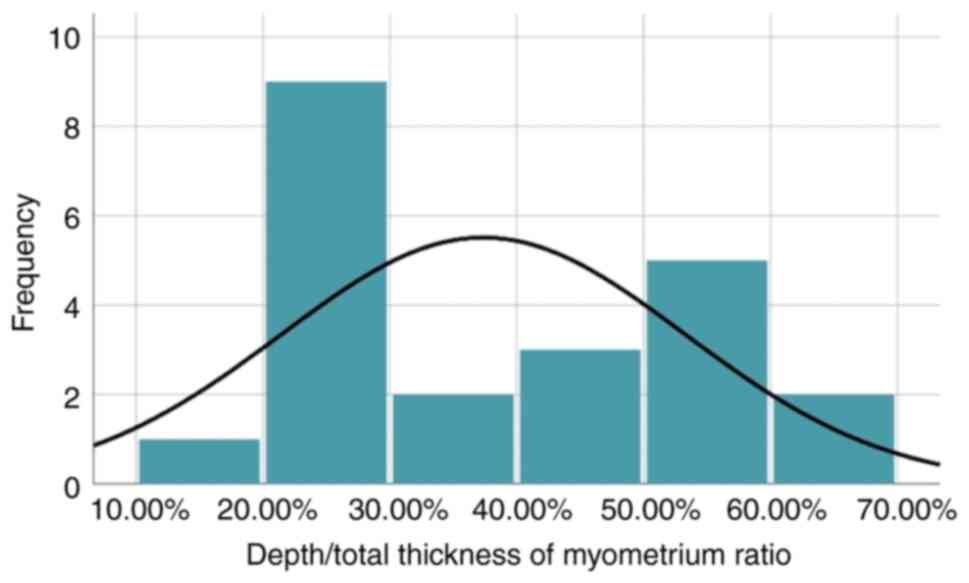
The mean ratio depth/total thickness of the
myometrium was 37.6%, with a minimum ratio of 16% and a maximum
ratio of 66%. The distribution of the patients according to the
depth/total thickness ratios is presented in Fig. 6, while supplementary data is
presented in Table SII. A ratio
exceeding 50% indicates that the niche can be classified as
severe.
Based on the identified shapes of niches in the
present study, 45.5% are triangular, 36.4% are semicircular while
the rest are inclusion cysts and droplet type.
In the analysis of the types of sutures used during
uterine closure, it was determined that 48.1% of patients received
a single layered suture, while 51.9% of patients had a double
layered suture.
During the hysterorraphy, the first layer involved a
continuous locking suture in 48.1% of patients, while continuous
non-locking suture and interrupted sutures were used in the
remaining cases.
In the final segment of the descriptive analysis,
the present study examined the number of patients in whom the
visceral peritoneum was closed during surgery. It was observed that
this was the case for 61.5% of the patients.
The association between the type of
suture and the presence of a niche
Analyzing Table I,
it can be noted that single layered closure of the uterus was
observed in 40% of cases with no isthmocele and 59.1% of cases with
isthmocele. For testing the relationship between the presence of
niche and the number of layers, chi-square test was used. Bivariate
chi-square test revealed no significant association
(χ2=1.853; df=1, P=0.173).
 | Table IAssociation between number of layers
and the presence of niche. |
Table I
Association between number of layers
and the presence of niche.
| | Number of layers | |
|---|
| | | | 1 | 2 | Total |
|---|
| Niche yes/no | No | Frequency | 12 | 18 | 30 |
| | | % | 40.0% | 60.0% | 100.0% |
| | Yes | Frequency | 13 | 9 | 22 |
| | | % | 59.1% | 40.9% | 100.0% |
| Total | | Frequency | 25 | 27 | 52 |
| | | % | 48.1% | 51.9% | 100.0% |
| Chi-square test |
| | Value | df | P-value | | |
| Pearson
Chi-Square | 1.853 | 1 | 0.173 | | |
| Cramer's V | 0.189 | 0.173 | | | |
| Number of
cases | 52 | | | | |
The results of Fisher's exact test confirm a
significant association between the presence of the niche and the
type of suture of the first layer (P=0.00560733). Based on the
findings presented in Table II,
when non-locking continuous suture was used, the absence of niche
was observed in most cases (60% of cases), while using the locking
continuous suture was associated with niches (63.6%).
 | Table IIAssociation between the first layer
type of suture and isthmocele. |
Table II
Association between the first layer
type of suture and isthmocele.
| | First layer | |
|---|
| | | | Continuous
locking | Continuous
non-locking | Interrupted
sutures | Total |
|---|
| Niche yes/no | No | Frequency | 11 | 18 | 1 | 30 |
| | | % | 36.7% | 60.0% | 3.3% | 100.0% |
| | Yes | Frequency | 14 | 4 | 4 | 22 |
| | | % | 63.6% | 18.2% | 18.2% | 100.0% |
| Total | | Frequency | 25 | 22 | 5 | 52 |
| | % | 48.1% | 42.3% | 9.6% | 100.0% | |
| | | | | Exact
probability | | |
| Fisher's exact
test | | | | 0.00560733 | | |
The association between the number of
layers and the thickness of the residual myometrium in patients
with isthmocele
The mean thickness of the residual myometrium was
0.86 cm when hysterorrhaphy was performed in a single layer, while
the mean thickness observed in patients with double-layered closure
was 0.8211 cm. Because the results of the t test had a P=0.753, as
demonstrated in Table SIII, it was
concluded that the relationship between the two variables was not
significant.
The association between the number of
layers and the total thickness of the myometrium in patients with
isthmocele
The total thickness of both types of sutures was
also compared, with a t-test result that revealed no statistically
significant difference [t(20)=-0.233; P=0.818]. These results are
presented in Table SIV.
The association between the type of
suture and the thickness of the residual myometrium in patients
with niche
For finding out whether there is a significant
association between the type of suture and the residual myometrial
thickness, one-way ANOVA analysis was used.
The thickness of the residual myometrium was not
significantly different (P=0.475) based on the type of suture, even
though results in Table III
revealed that when non-locking continuous suture was used, the mean
thickness of the residual myometrium was 1.00 cm, while in other
cases the residual myometrial thickness was 0.8. Even though these
results were observed and analyzed in Table III, the difference is not
statistically significant.
 | Table IIIRelationship between the type of
suture and the thickness of the residual myometrium. |
Table III
Relationship between the type of
suture and the thickness of the residual myometrium.
| | N | Mean | Standard
deviation | Minimum | Maximum |
|---|
| Cont. locking | 14 | 0.8029 | 0.25644 | 0.40 | 1.30 |
| Cont.
non-locking | 4 | 1.0025 | 0.41291 | 0.65 | 1.60 |
| Interrupted
suture | 4 | 0.8325 | 0.23472 | 0.49 | 1.02 |
| Total | 22 | 0.8445 | 0.28084 | 0.40 | 1.60 |
| ANOVA |
| Thickness of
residual myometrium |
| | df | F | P-value | | |
| Between groups | 2 | 0.774 | 0.475 | | |
The association between the type of
suture and the total thickness of the myometrium in patients with
niche
The total thickness of the myometrium in patients
with niche is not statistically significant different based on the
type of suture used (P=0.607), with Table IV illustrating these results.
 | Table IVRelationship between the type of
suture and total thickness of the myometrium in patients with
niche. |
Table IV
Relationship between the type of
suture and total thickness of the myometrium in patients with
niche.
| | N | Mean | Standard
deviation | Minimum | Maximum |
|---|
| Cont. locking | 14 | 1.4693 | 0.33790 | 0.86 | 1.89 |
| Cont.
non-locking | 4 | 1.5675 | 0.39911 | 1.21 | 2.10 |
| Interrupted
suture | 4 | 1.3350 | 0.15264 | 1.20 | 1.54 |
| Total | 22 | 1.4627 | 0.31936 | 0.86 | 2.10 |
| ANOVA |
| Total thickness of
myometrium |
| | df | F | P-value | | |
| Between groups | 2 | 0.513 | 0.607 | | |
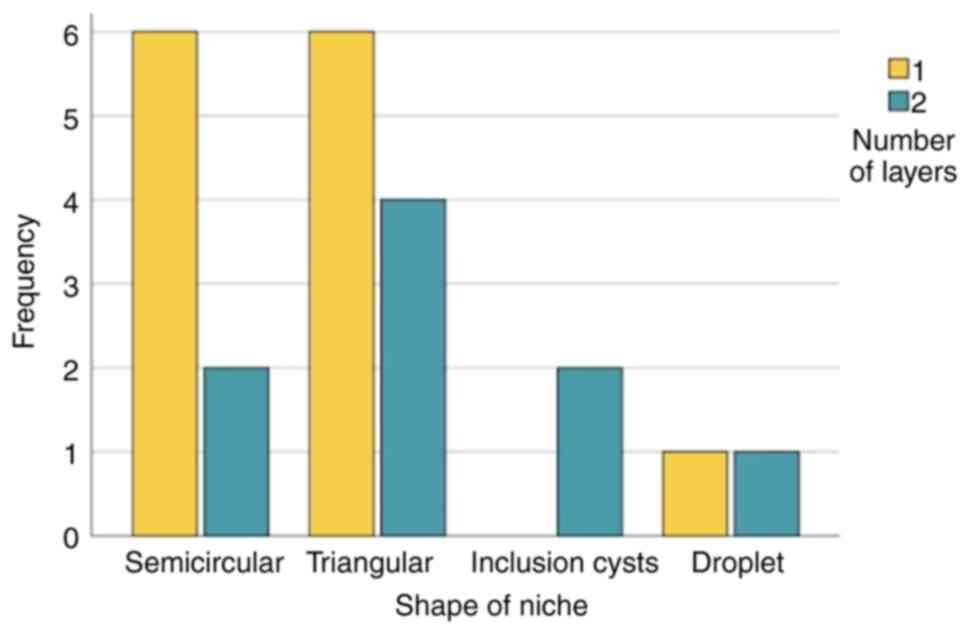
The association between the shape of
the niche and the number of layers used in patients with
isthmocele
For testing the relationship between the shape of
the niche and the number of layers used, Fisher's exact test was
used. Judging by the results that are illustrated in Fig. 7 and Table SV, there was no significant
association between the two variables (P=0.63800905).
The results regarding the inclusion cysts and
droplet type were ignored, because their number was extremely
low.
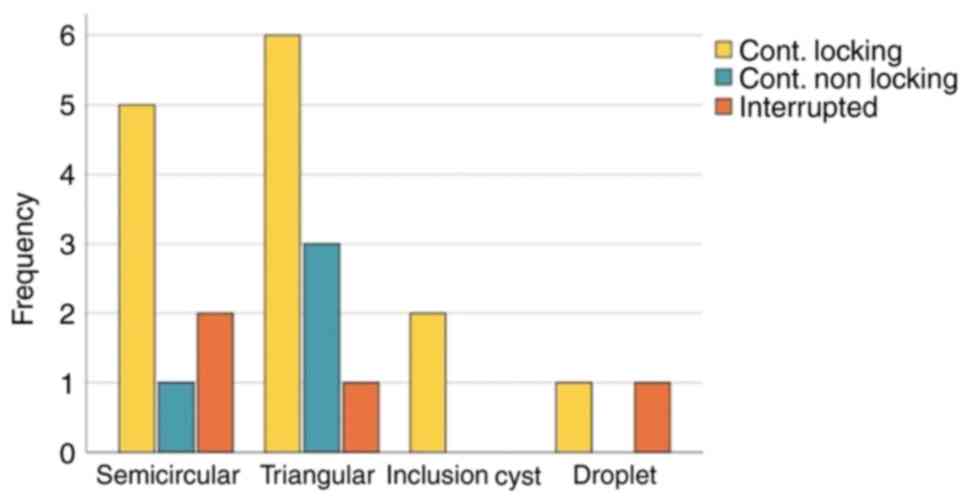
The association between the shape of
niche and type of suture
The result of Fisher's exact test revealed that
there was not statistically significant association (P=0.67420814)
between the shape of niche and the type of suture. No matter the
shape of the niche, in most cases continuous locking suture was
used for the first layer. The association between the shape of
niche and type of suture are demonstrated in Fig. 8 and Table V. The results regarding inclusion
cysts and droplet were ignored as they were in an extremely small
number.
 | Table VAssociation between the shape of
niche and type of suture. |
Table V
Association between the shape of
niche and type of suture.
| | First layer | |
|---|
| | | | Cont. locking | Cont.
non-locking | Interrupted | Total |
|---|
| Shape | Semicircular | Frequency | 5 | 1 | 2 | 8 |
| | | % | 62.5% | 12.5% | 25.0% | 100.0% |
| | Triangular | Frequency | 6 | 3 | 1 | 10 |
| | | % | 60.0% | 30.0% | 10.0% | 100.0% |
| | Inclusion cyst | Frequency | 2 | 0 | 0 | 2 |
| | | % | 100.0% | 0.0% | 0.0% | 100.0% |
| | Droplet | Frequency | 1 | 0 | 1 | 2 |
| | | % | 50.0% | 0.0% | 50.0% | 100.0% |
| Total | | Frequency | 14 | 4 | 4 | 22 |
| | | % | 63.6% | 18.2% | 18.2% | 100.0% |
| | | | Exact
probability | | | |
| Fisher's exact
test | | | 0.67420814 | | | |
The association between the number of
layers and severity of niche
Among all patients with a niche, 68.2% had a depth
of niche/total myometrial thickness <50% (non-severe niche),
while 31.8% of them had a ratio >50% (severe niche). These
results are displayed in Table
SVI.
With the use of single-layered uterine closure, the
percentage of severe niches was 30.8%, while with the use of
double-layered closure, the percentage was 33.3%. Based on the
findings presented in Table VI,
the difference is not statistically significant (P=0.9638).
 | Table VIAssociation between number of layers
and severity of niche. |
Table VI
Association between number of layers
and severity of niche.
| | Depth/total
thickness ratio | |
|---|
| | | | <50% | >50% | Total |
|---|
| Number of
layers | 1 | Frequency | 9 | 4 | 13 |
| | | % | 69.2% | 30.8% | 100.0% |
| | 2 | Frequency | 6 | 3 | 9 |
| | | % | 66.7% | 33.3% | 100.0% |
| Total | | Frequency | 15 | 7 | 22 |
| | | % | 68.2% | 31.8% | 100.0% |
| | | | Exact
probability | | |
| Fisher's exact
test | | | 0.9638 | | |
The association between the type of
suture used for the first layer and the severity of niche
With the use of continuous locking suture for the
first layer, the percentage of severe niches was 50%, while the
other two types of suture (continuous non-locking or interrupted
suture), there were no cases of severe niche (with a ratio
>50%). In Table VII, the
association between the type of suture of the first layer and the
severity of niche can be observed.
 | Table VIIAssociation between the type of
suture of first layer and the severity of niche. |
Table VII
Association between the type of
suture of first layer and the severity of niche.
| | Depth/total
myometrial thickness ratio | |
|---|
| | | | <50% | >50% | Total |
|---|
| First layer | Cont. locking | Frequency | 7 | 7 | 14 |
| | | % | 50.0% | 50.0% | 100.0% |
| | Cont.
non-locking | Frequency | 4 | 0 | 4 |
| | | % | 100.0% | 0.0% | 100.0% |
| | Interrupted
suture | Frequency | 4 | 0 | 4 |
| | | % | 100.0% | 0.0% | 100.0% |
| Total | | Frequency | 15 | 7 | 22 |
| | | % | 68.2% | 31.8% | 100.0% |
| | | | Exact
probability | | |
| Fisher's exact
test | | | 0.05661882 | | |
Despite P=0.05661882, it is plausible to consider a
statistically significant difference between the continuous locking
suture and the other two types, regarding the risk of developing a
severe niche. It's crucial to note that the relatively small sample
size might account for this value. With larger groups and increased
statistical power, a more pronounced association would likely
become evident.
The association between niche and
closure of the visceral peritoneum
In the cases presenting with niche, peritonization
was performed in 63.6% of cases, while in the cases without niche,
peritonization was observed in 60% of patients, as observed in
Table SVII. Considering this, the
difference between the two groups is not statistically significant
(P=0.790).
Furthermore, a comparison was made between the depth
of the isthmocele in patients without peritonization and those with
peritonization. Based on the results included in Table SVIII, where similar means were
observed, no significant difference was identified between the two
groups.
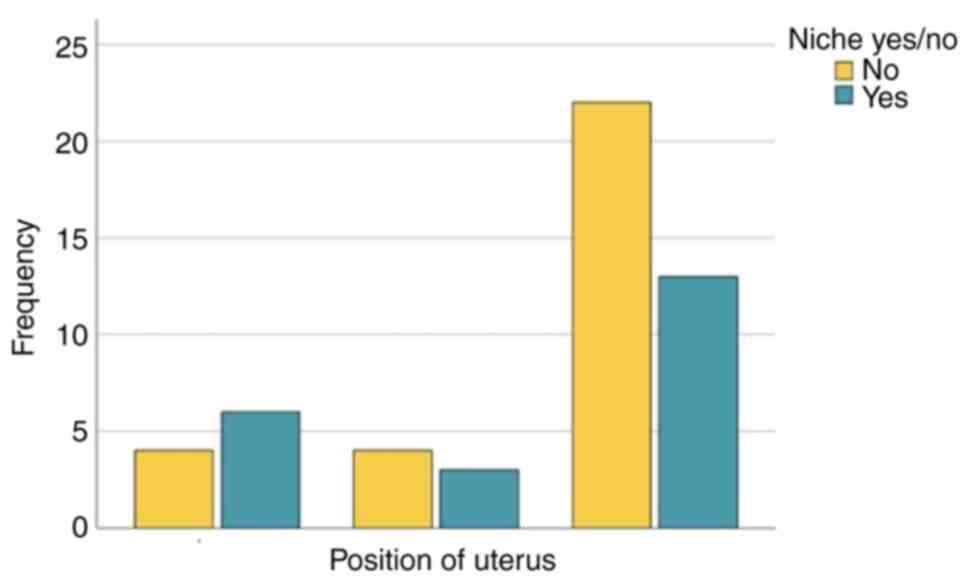
The association between the niche
presence and position of uterus
The analyzed data displayed in Table VIII revealed no statistically
significant association between the presence of the niche and
position of uterus (P=0.43952477). This association is visually
represented in Fig. 9.
 | Table VIIIAssociation between niche and
position of uterus. |
Table VIII
Association between niche and
position of uterus.
| | Niche yes/no | |
|---|
| | | | No | Yes | Total |
|---|
| Position of
uterus | Retroverted | Frequency | 4 | 6 | 10 |
| | | % | 40.0% | 60.0% | 100.0% |
| | Intermediate | Frequency | 4 | 3 | 7 |
| | | % | 57.1% | 42.9% | 100.0% |
| | Anteverted | Frequency | 22 | 13 | 35 |
| | | % | 62.9% | 37.1% | 100.0% |
| Total | | Frequency | 30 | 22 | 52 |
| | | % | 57.7% | 42.3% | 100.0% |
| | | Exact
probability | | | |
| Fisher's exact
test | | 0.43952477 | | | |
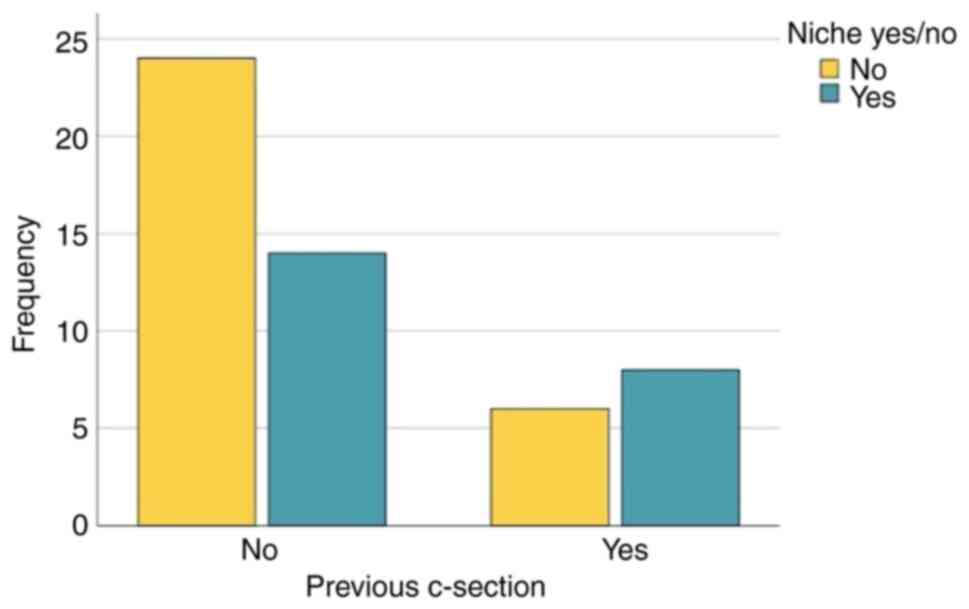
The association between the presence
of previous C-sections and niche development
The percentage of niche appearance in patients with
previous C-sections, revealing an elevated incidence of niche in
this group, is demonstrated in Fig.
10.
The association between a homogenous
myometrium and the presence of niche
Although it was observed that in the presence of
fibromatosis or adenomyosis, the niche was developed in 71.4% of
cases, while the percentage of niche was 37.8% in patients without
fibroids or adenomyosis, the result of the statistical analysis
observed in Table SIX
(P=0.11884797) revealed no statistically significant
association.
Discussion
Based on the results presented in the descriptive
and statistical analysis, a comprehensive discussion can be
initiated. Interestingly, in contrast to the lower mean age of
patients who underwent C-section at Saint Pantelimon Emergency
Clinical Hospital (Bucharest, Romania) during the specified period,
which typically tends to be younger, the present study reported a
mean age of 30.42 years. This deviation could be attributed to the
fact that a portion of the patients who gave birth via C-section
were younger women who tended to avoid prenatal care. Consequently,
the mean age in the present study might have been influenced by the
absence of adequate prenatal and postpartum medical visits of these
patients.
Based on the position of the uterus, 67.3% of the
patients had an anteverted uterus, the others presenting with
retroverted uterus or in intermediate position. Despite previous
studies suggesting a retroverted uterus a risk factor for
isthmocele development, the present statistical analysis did not
establish a significant association in the present study. However,
upon reviewing the database, it was evident that the most severe
niches were observed in patients with a retroverted uterus or in
intermediate position, as indicated by their depth to total
myometrial thickness ratios (66 and 63%, respectively).
The ultrasound appearance of the niche was observed
in 22 patients out of the 52 participants in the present study,
resulting in a prevalence of 42.3%. It's worth noting that
international studies have reported a broader range of prevalence,
reaching up to 70%. This variance in prevalence underscores the
importance of considering regional and population-specific factors
that might contribute to these differences in isthmocele
occurrence.
The shapes of the niches exhibited variability,
including triangular, semicircular, inclusion cysts and droplet
shapes. Among these, triangular and semicircular shapes were the
most prevalent, accounting for 45.5 and 36.4% respectively.
Interestingly, the present study found that associations between
the shape of the niche and factors such as the number of layers or
the type of suture used did not demonstrate any statistically
significant relationships.
Although previous studies had extensively explored
and dismissed a connection, the present study deliberately examined
the relationship between the number of layers in uterine closure
and the presence of an isthmocele. Following statistical analysis,
it was determined that there were no discernible differences in
niche development between single-layered and double-layered uterine
closures. Moreover, the present study delved in the relationship
between the number of layers and both the total myometrial
thickness and residual myometrial thickness in patients with an
isthmocele. However, the results indicated to statistically
significant differences in this regard.
The present study explored the association between
the type of suture used and both the total myometrial thickness and
the residual myometrial thickness. Notably, when utilizing a
continuous non-locking suture, the mean thickness of the residual
myometrium was found to be 1 cm, whereas in other types of suture,
the mean thickness was 0.8 cm. However, despite these variations,
the results did not demonstrate statistical significance.
In the present study, a statistically significant
association was identified between the type of suture used for the
first layer and the presence of an isthmocele (P=0.006). Notably,
the continuous non-locking suture was predominantly utilized when
the isthmocele was absent, whereas the continuous locking suture
was more prevalent in cases where the isthmocele was present. This
observed effect could likely be attributed to hypoxia induced by
the ischemia-inducing suture and subsequent vicious scarring.
In the analysis of the present study, among all
cases with an isthmocele, 31.8% had a depth-to-total myometrial
thickness ratio exceeding 50%, which is the criterion for
categorizing the niche as severe. The potential association between
the severity of the niche and the number of layers was examined,
however this did not yield significant results. However, the link
between the type of suture used for the first layer and the
severity of the niche was further investigated, and the results
indicated a significant difference. Specifically, there was a
notable distinction in the development of a severe niche when
comparing uterine closure with a continuous locking suture vs. the
other two types of sutures.
The potential association between the development of
an isthmocele and the presence of fibroids or adenomyosis in
patients was investigated. Interestingly, 71% of patients with
fibroids or adenomyosis developed an isthmocele, whereas among
those without this pathology, only 37.8% presented with a niche.
However, despite the observed differences, the association between
the presence of fibroids or adenomyosis and the development of an
isthmocele did not reach a statistical significance.
In the present study, the potential association
between the closure of the visceral peritoneum and the development
of an isthmocele was explored. Historically, it was considered that
the lack of peritoneal closure could be a risk factor for
isthmocele development due to potential adhesion formation. There
was no association found between peritonization and the presence of
niche, nor any difference was observed between the depths of niches
in patients with closure of the peritoneum vs. those without
it.
The present study's limitations revolve around its
exclusive focus on a single institution and the relatively small
sample size. The second limitation was primarily driven by the
challenge of recruiting research participants, which stemmed from
difficulties related to accessing postnatal care due to refusal by
some patients. In addition, another limit of the present study was
the fact that potentially confounding variables, such as uterine
position, body mass index and surgical technique were not
controlled. There is a statistically significant association
between the suture of the first uterine layer with continuous
locking suture and the presence of the niche, which could be
attributed to ischemia. Furthermore, there is also significant
association between the closure of the first layer with continuous
locking suture and the development of a severe niche. Further
research and analysis may be needed to delve deeper into this
aspect and its potential impact on isthmocele formation.
The present study did not find any significant
differences in the rate of isthmocele development based on the
number of layers used during uterine closure. Whether a
single-layer or double-layer closure was performed did not appear
to influence the likelihood of isthmocele development in the
present study. Moreover, no significant associations were found
between the number of layers used for hysterorraphy and the
severity of the isthmocele.
Although the most severe niches in the present study
were observed in patients with retroverted uterus or in
intermediate position, the statistical analysis of the present
study did not reveal a significant association between the niche
development and the position of uterus, which is recognized as a
significant factor in isthmocele development. It is important to
acknowledge that the limited sample size may have contributed to
the inability to establish a statistically significant
association.
The present study noted that there were no
significant associations found between the shape of the isthmocele
and either the number of layers used, or the type of suture used
for the first layer of uterine closure. There is no statistically
significant association between the development of niche and
absence of visceral peritoneal closure, as well as there are no
differences in the depths of patients with niches based on the
presence or absence of peritonization. Additionally, the presence
of fibroids or adenomyosis was not found to be associated with an
increased risk of developing an isthmocele.
These findings emphasize the potential impact of
suture technique on isthmocele formation and severity, highlighting
the importance of further research in this area.
Supplementary Material
Values of the depths of the
niche.
Depth/total thickness ratio.
Association between the number of
layers and the residual myometrial thickness in patients with
niche.
Association between the number of
layers and the total thickness of the myometrium in patients with
niche.
The association between the shape of
the niche and the number of layers used.
Distribution of niches.
Association between niche and
peritonization.
Association between peritonization and
depth of niche.
Association between homogenous
myometrium and niche.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
GZ collected the data, analyzed and interpreted the
results, and prepared the draft of the manuscript. BN collected the
data and prepared the draft of the manuscript. IP analyzed and
interpreted the results, and prepared the draft of the manuscript.
AN analyzed and interpreted the results, wrote, reviewed and edited
the manuscript. CAI designed the research, wrote, reviewed and
edited the manuscript, and supervised the present study. All
authors have critically reviewed, read and approved the final
version of the manuscript and are responsible for the content and
similarity index of the manuscript. GZ and BN confirm the
authenticity of all the raw data.
Ethics approval and consent to
participate
The present study was approved (approval no.
21/20.03.2022) by the Ethics committee of the Saint Pantelimon
Emergency Clinical Hospital (Bucharest, Romania).
Patient consent for publication
Informed oral consent was obtained from all
patients. All patients signed written informed consent for the use
of their data and associated images in research upon admission to
the Obstetrics and Gynecology department of the Saint Pantelimon
Emergency Clinical Hospital (Bucharest, Romania).
Competing interests
The authors declare that they have no competing
interests.
Use of artificial intelligence tools
During the preparation of this work, artificial
intelligence tools were used to improve the readability and
language of the manuscript or to generate images, and subsequently,
the authors revised and edited the content produced by the
artificial intelligence tools as necessary, taking full
responsibility for the ultimate content of the present
manuscript.
References
|
1
|
Rupa R, Kushvaha S and Venkatesh K:
Uterine isthmocele-a frequently overlooked complication of cesarean
sections. Indian J Radiol Imaging. 31:601–604. 2021.PubMed/NCBI View Article : Google Scholar
|
|
2
|
C-Section Rates by Country 2024.
https://worldpopulationreview.com/country-rankings/c-section-rates-by-country.
|
|
3
|
Nguyen AD, Duong GTT, Do DT, Nguyen DT,
Tran DA, Phan TTH, Nguyen TK and Nguyen HTT: Primary cesarean
section rate among full-term pregnant women with non-previous
uterine scar in a hospital of Vietnam. Heliyon.
8(e12222)2022.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Kulshrestha V, Agarwal N and Kachhawa G:
Post-caesarean niche (isthmocele) in uterine scar: An update. J
Obstet Gynecol India. 70:440–446. 2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Iannone P, Nencini G, Bonaccorsi G,
Martinello R, Pontrelli G, Scioscia M, Nappi L, Greco P and
Scutiero G: Isthmocele: From risk factors to management. Rev Bras
Ginecol Obstet. 41:044–052. 2019.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Al-Ghotani B, Martini N, Alabdallah E,
Alawad I and Hussien K: A large post-caesarean Niche (Isthmocele)
with amenorrhea, a symptom that was not reported in the medical
literature: A rare case report. Int J Surg Case Rep.
109(108528)2023.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Di Spiezio Sardo A, Saccone G, McCurdy R,
Bujold E, Bifulco G and Berghella V: Risk of cesarean scar defect
following single- vs double-layer uterine closure: Systematic
review and meta-analysis of randomized controlled trials.
Ultrasound Obstet Gynecol. 50:578–583. 2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Yıldız E and Timur B: Comparison of
classic single-layer uterin suture and double-layer purse-string
suture techniques for uterus closure in terms of postoperative
short-term uterine isthmocele: A prospective randomized controlled
trial. Turk J Obstet Gynecol. 20:206–213. 2023.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Turan GA, Gur EB, Tatar S, Gokduman A and
Guclu S: Uterine closure with unlocked suture in cesarean section:
Safety and quality. Pak J Med Sci. 30:530–534. 2014.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Vervoort AJMW, Uittenbogaard LB, Hehenkamp
WJK, Brölmann HAM, Mol BWJ and Huirne JAF: Why do niches develop in
caesarean uterine scars? Hypotheses on the aetiology of niche
development. Hum Reprod. 30:2695–702. 2015.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Setubal A, Alves J, Osório F, Guerra A,
Fernandes R, Albornoz J and Sidiroupoulou Z: Treatment for uterine
isthmocele, a pouchlike defect at the site of a cesarean section
scar. J Minim Invasive Gynecol. 25:38–46. 2018.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Hosseini E, Aghajanpour S, Zameni N and
Hafezi M: Isthmocele-a neglected cause of secondary infertility and
implantation failure: A case report. Clin Case Rep.
10(e05853)2022.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Scutiero G, Iannone P, Bernardi G,
Bonaccorsi G, Spadaro S, Volta CA, Greco P and Nappi L: Oxidative
stress and endometriosis: A systematic review of the literature.
Oxid Med Cell Longev. 2017(7265238)2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Bij de Vaate AJM, Brölmann HAM, van der
Voet LF, van der Slikke JW, Veersema S and Huirne JAF: Ultrasound
evaluation of the cesarean scar: Relation between a niche and
postmenstrual spotting. Ultrasound Obstet Gynecol. 37:93–99.
2011.PubMed/NCBI View
Article : Google Scholar
|
|
15
|
Setúbal A, Alves J, Osório F and
Sidiropoulou Z: Demonstration of isthmocele surgical repair. J
Minim Invasive Gynecol. 28:389–390. 2021.PubMed/NCBI View Article : Google Scholar
|