1. Introduction
The landscape of cancer treatment and research has
undergone notable transformation, with the emergence of
personalized and precision medicine as groundbreaking approaches in
the management of various types of cancer, including those
affecting gynecological organs. These approaches mark a departure
from the traditional one-size-fits-all strategy, paving the way for
more targeted, efficient and effective interventions (1). In gynecological cancer, encompassing
ovarian, cervical, uterine, vaginal and vulvar cancer, precision
medicine may improve outcomes, decrease side effects and enhance
patient quality of life (2).
Personalized medicine, often used interchangeably
with precision medicine, involves customization of medical therapy
according to the unique attributes of each patient. It extends
beyond focusing on genetic profiles, encompassing a wide array of
patient-specific factors, including environmental influences,
lifestyle and unique disease pathways. The holistic approach of
personalized medicine, which views the patient as an integral part
of the treatment equation, optimizes therapeutic decisions and
practices for individual patients (3).
Precision medicine emphasizes the incorporation of
genetic, environmental and lifestyle information into the
diagnosis, treatment and prevention of disease. This approach
relies on advanced technologies and the analysis of large datasets
to identify which therapies will be beneficial for patients
depending on their genetic and molecular profiling (4). The goal is to select optimal therapies
and interventions for patients, minimizing unnecessary treatments
and focusing on those most likely to benefit the patient (5).
The present review aims to provide a comprehensive
overview of the advances in precision medicine within the context
of gynecological cancers, focusing on the challenges posed by tumor
heterogeneity, the role of genetic alterations, and the development
of targeted therapies. By discussing the current state of precision
oncology and its future directions, the present study seeks to
highlight the potential for improving patient outcomes through
personalized treatment approaches.
2. Tumor heterogeneity in gynecological
malignancy
Tumor heterogeneity, a hallmark of cancer, presents
challenges in the diagnosis, treatment and management of
gynecological malignancies. Heterogeneity manifests at multiple
levels, including histological subtype, molecular profile and
clinical behavior within gynecological cancers such as ovarian,
cervical and uterine cancers (6).
Histological and molecular
heterogeneity
Gynecological cancers, particularly ovarian cancer,
exhibit substantial histological diversity. For example, ovarian
cancer includes subtypes such as high-grade serous (HGS),
endometrioid, clear cell and mucinous carcinoma, each with distinct
genetic alterations, clinical presentations and responses to
therapy (7). Molecular
heterogeneity further complicates this landscape as tumors of the
same histological subtype may show diverse genetic mutations, gene
expression patterns and signaling pathway alterations (8). Advances in genomic technologies,
including next-generation sequencing (NGS), enable comprehensive
tumor profiling, revealing the complex molecular underpinnings and
identifying potential therapeutic targets and biomarkers (8).
Functional and epigenetic
heterogeneity
In addition to genetic variations, epigenetic
modifications such as DNA methylation and histone modification
contribute to tumor heterogeneity by regulating gene expression and
cell phenotypes, leading to treatment resistance and phenotypical
diversity (9). Phenotypical
heterogeneity is also evident in varying cell morphology,
proliferation rate and drug sensitivity, complicating treatment
strategies (10). Moreover,
functional heterogeneity arises from differences in cell
metabolism, signaling pathway activation and immune
microenvironment interactions, all of which influence tumor
aggressiveness and therapeutic resistance (11-15).
3. Challenges in current treatment
approaches and future directions
Despite advancements in understanding gynecological
cancer and developing targeted therapy, challenges persist,
particularly regarding tumor heterogeneity, treatment resistance
and disparities in access to innovative treatments (16).
Treatment resistance and
recurrence
A major challenge is the high rate of recurrence and
development of treatment resistance, especially in advanced-stage
gynecological cancer. Even with initial therapeutic success, many
patients experience disease progression and become resistant to
standard treatments, leading to poor long-term outcomes (16). This resistance often results from
the tumor molecular heterogeneity, which necessitates alternative
therapeutic strategies and development of novel targeted agents to
overcome these resistance mechanisms (17).
Lack of predictive biomarkers
Another significant hurdle is the scarcity of
reliable predictive biomarkers for selecting optimal treatment
strategies. Although biomarkers such as breast cancer (BRCA) gene
mutations in ovarian cancer have been validated for targeted
therapy, many patients lack actionable mutations, limiting their
treatment options (17). The
identification and validation of robust biomarkers that accurately
predict treatment response and guide therapeutic decisions is key
(18).
Disparities in access to
treatment
Disparities in access to genomic testing, targeted
therapy and clinical trials are particularly pronounced among
populations of developing countries. Limited access to precision
medicine exacerbates disparities in outcomes and survival rates
between demographic groups (18).
Efforts to improve access to innovative therapy and clinical trials
for all patients, regardless of socioeconomic status or
geographical location, are essential for reducing these disparities
(18).
Data interpretation and
integration
The integration of multi-omic data and the
development of computational algorithms for data analysis present
opportunities and challenges. While genomic technology has enabled
comprehensive molecular characterization of tumors, interpreting
complex genomic data and translating research findings into
clinical practice is challenging. Standardization of molecular
profiling assays, data sharing initiatives and collaboration across
research institutions are necessary to accelerate progress and
ensure effective implementation of precision medicine (19).
4. Drivers of genetic alterations in
gynecological cancer
A complex interplay of genetic alterations drives
gynecological cancer, contributing to tumorigenesis, disease
progression and treatment resistance. Understanding the key driver
mutations and signaling pathways involved in gynecological
malignancy is key for developing targeted therapy and personalized
treatment strategies.
In ovarian cancer, HGS carcinoma (HGSC), the most
common and aggressive subtype, is characterized by frequent
mutations in genes involved in DNA repair pathways, such as BRCA1
and BRCA2(20). These mutations
impair homologous recombination-mediated DNA repair, leading to
genomic instability and increased susceptibility to DNA-damaging
agents such as platinum-based chemotherapy and poly (ADP-ribose)
polymerase (PARP) inhibitors (21).
Other recurrent genetic alterations in HGSC include mutations in
TP53, which occur in nearly all cases, as well as alterations in
genes involved in the PI3K/AKT/mTOR pathway, such as
phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit α
(PIK3CA) and PTEN (22). Targeted
therapy directed against these genetic aberrations hold promise for
improving outcomes in patients with ovarian cancer.
In endometrial cancer, the most common type of
uterine cancer, molecular profiling studies have identified
distinct genomic subtypes with different etiologies, clinical
behavior and treatment responses (22-24).
For example, 20-30% of endometrial cancer cases harbor mutations in
the PTEN tumor suppressor gene, leading to dysregulated
PI3K/AKT/mTOR signaling and aberrant cell proliferation (23). Other recurrent genetic alterations
in endometrial cancer include mutations in PIK3CA, Catenin Beta 1
and TP53 genes, as well as microsatellite instability (MSI) and DNA
mismatch repair (MMR) deficiency (24). These molecular alterations serve as
potential therapeutic targets and predictive biomarkers for
targeted therapy and immunotherapy in endometrial cancer.
High-risk human papilloma virus (HPV) types,
particularly HPV16 and HPV18, which encode viral oncoproteins that
promote cell transformation and oncogenesis, primarily drive
cervical cancer (25). Integration
of HPV DNA into the host genome disrupts cellular tumor suppressor
pathways, such as the retinoblastoma and p53 pathways, leading to
uncontrolled cell proliferation and tumor formation (26). In addition to HPV infection,
cervical cancer may harbor genetic alterations in genes such as
PIK3CA, PTEN and TP53, which contribute to tumor progression and
treatment resistance (27).
Targeting HPV-associated pathways and associated genetic
alterations holds potential for improving outcomes in patients with
cervical cancer.
Vulvar and vaginal cancers are relatively rare
gynecological malignancies that are often associated with HPV
infection, similar to cervical cancer (28). However, vulvar squamous cell
carcinoma may also arise in the absence of HPV infection, with
mutations in genes such as TP53, PIK3CA and fibroblast growth
factor receptor 3 (FGFR3) implicated in tumorigenesis (28). In vaginal cancer, HPV infection is a
common risk factor, particularly in younger patients, with
mutations in TP53 and PIK3CA identified in a subset of cases
(29). Targeted therapy directed
against HPV-related pathways and genetic alterations offers
potential avenues for improving outcomes in patients with vulvar
and vaginal cancer.
5. PARP inhibitors, BRCA and homologous
recombination deficiency (HRD) in gynecological cancer
PARP inhibitors exploit synthetic lethality, in
which the simultaneous inhibition of two DNA repair pathways leads
to cell death, to selectively target cancer cells with defects in
HR-mediated DNA repair (21).
BRCA1 and BRCA2 are tumor suppressor genes involved
in the repair of double-stranded DNA breaks via the HR repair
pathway. Mutations in BRCA1 or BRCA2 impair this DNA repair
mechanism, leading to genomic instability and increased
susceptibility to DNA-damaging agents, such as platinum-based
chemotherapy and PARP inhibitors (30). PARP inhibitors, such as olaparib,
niraparib and rucaparib, block activity of PARP enzymes, preventing
the repair of single-stranded DNA breaks and leading to
accumulation of double-stranded DNA breaks in BRCA-mutated cancer
cells. This synthetic lethality results in cancer cell death,
sparing normal cells with intact HR repair pathways (31).
In addition to BRCA mutations, HRD, a measure of
genomic instability and impaired DNA repair, is a predictive
biomarker for response to PARP inhibitors in gynecological cancer
(32). HRD can result from genetic
alterations, including mutations in other DNA repair genes (such as
RAD51 Paralog C and D), genomic rearrangement and chromosomal
abnormality. Tumors with HRD are more reliant on alternative DNA
repair mechanisms, such as PARP-mediated base excision repair,
making them susceptible to PARP inhibition (32).
Clinical trials have demonstrated the efficacy of
PARP inhibitors in the treatment of gynecological cancer, including
ovarian, fallopian tube and primary peritoneal cancer (33,34).
The SOLO-1 trial investigated the use of olaparib as maintenance
therapy in patients with newly diagnosed advanced ovarian cancer
and BRCA mutation (33). The study
showed a significant improvement in progression-free survival (PFS)
with olaparib compared with placebo, leading to its approval as a
first-line maintenance therapy in this population (33). Similarly, the NOVA trial
demonstrated the efficacy of niraparib as maintenance therapy in
patients with recurrent ovarian cancer, regardless of BRCA mutation
status (34). These findings have
transformed the treatment landscape for gynecological cancer,
offering new therapeutic options and improving outcomes for
patients with BRCA mutations or HRD.
However, challenges remain in the clinical
implementation of PARP inhibitors, including development of
resistance mechanisms, optimal patient selection criteria and the
identification of predictive biomarkers beyond BRCA mutations and
HRD. Resistance to PARP inhibitors can arise through various
mechanisms, such as restoration of HR repair, upregulation of
alternative DNA repair pathways or acquisition of secondary
mutations in PARP or other DNA repair genes (35).
6. Role of PD-L1 in gynecological
cancer
Tumor and immune cells express programmed
death-ligand 1 (PD-L1), a cell surface protein that serves a
critical role in regulating the immune response and promoting
immune evasion in gynecological cancer. PD-L1 interacts with its
receptor, programmed cell death protein 1 (PD-1), on T cells,
leading to T cell exhaustion and inhibition of antitumor immune
responses (36). Immunotherapies,
such as immune checkpoint inhibitors, target the PD-1/PD-L1 axis, a
major immune checkpoint pathway for the treatment of gynecological
cancer (37).
In ovarian cancer, PD-L1 expression is associated
with aggressive disease characteristics, immune infiltration and
poor prognosis (38). PD-L1
blockade enhances antitumor immune response and inhibits tumor
growth in ovarian cancer models, providing rationale for clinical
evaluation of immune checkpoint inhibitors in this disease
(39). Clinical trials
investigating PD-1/PD-L1 inhibitors, either as monotherapy or in
combination with other agents, have shown promising results in
patients with recurrent or refractory ovarian cancer, leading to
their approval for this indication (40,41).
Similarly, PD-L1 expression has been reported in
endometrial cancer, particularly in tumors with aggressive
histological subtypes, high tumor grade and advanced-stage disease
(42). The presence of
PD-L1-positive immune cells in the tumor microenvironment is
associated with immune evasion and treatment resistance in
endometrial cancer (43). Clinical
trials evaluating efficacy of PD-1/PD-L1 inhibitors in endometrial
cancer have shown encouraging responses in patients with high
microsatellite instability (MSI-H) or MMR-deficient (dMMR) tumors
(43). These findings have led to
the approval of PD-1/PD-L1 inhibitors for treatment of advanced or
metastatic endometrial cancer refractory to standard therapy
(44).
Chronic inflammation and HPV infection in cervical
cancer upregulate PD-L1 expression, which contributes to immune
suppression and tumor immune escape. High PD-L1 expression in
cervical cancer is associated with advanced-stage disease, lymph
node metastasis and decreased survival outcomes (45). A clinical trial investigating immune
checkpoint inhibitors targeting the PD-1/PD-L1 axis in cervical
cancer has demonstrated durable responses and prolonged survival in
patients with advanced or recurrent disease (46). These findings support use of
PD-1/PD-L1 inhibitors as a treatment option for patients with
advanced or metastatic cervical cancer.
Researchers have reported PD-L1 expression in a
subset of vulvar and vaginal cancer, which is associated with
immune evasion and treatment resistance (47). Clinical trials evaluating immune
checkpoint inhibitors in vulvar and vaginal cancer are ongoing,
with preliminary results showing promising antitumor activity and
manageable safety profiles (48,49).
To elucidate the role of the PD-1/PD-L1 axis in these rare
gynecological malignancies and optimize treatment strategies,
further research is necessary.
7. Clinical trials
Clinical trials serve a pivotal role in advancing
the field of gynecological oncology by evaluating novel therapeutic
strategies, validating predictive biomarkers and improving patient
outcomes. Data from recent clinical trials has provided valuable
insight into the efficacy and safety of emerging treatments and
biomarker-driven therapy for gynecological cancers (50,51).
In ovarian cancer, several landmark clinical trials
have evaluated the role of targeted therapy and immunotherapies in
improving outcomes for patients with advanced or recurrent disease
(33,52). SOLO-1 trial showcased the efficacy
of olaparib as a maintenance treatment in newly diagnosed patients
with advanced ovarian cancer and BRCA mutation, resulting in a
notable enhancement in PFS compared with a placebo (33). Similarly, the PAOLA-1 trial
investigated the combination of olaparib and bevacizumab as
first-line maintenance therapy in patients with advanced ovarian
cancer, showing a significant improvement in PFS in the overall
population and patients with HRD (52). These findings have led to approval
of olaparib and olaparib + bevacizumab as maintenance therapies in
this population (33,52).
In endometrial cancer, KEYNOTE-146 trial evaluated
the efficacy of pembrolizumab, a PD-1 inhibitor, in patients with
advanced or recurrent disease refractory to standard therapy
(53). The study demonstrated
encouraging antitumor activity with pembrolizumab, particularly in
patients with MSI-H or dMMR tumors, leading to its approval as a
treatment option in this population (53). Similarly, the JAVELIN Solid Tumor
Trial investigated the efficacy of avelumab, another PD-L1
inhibitor, in patients with advanced or recurrent endometrial
cancer, showing promising responses and manageable safety profiles
in these patients (54).
In cervical cancer, the KEYNOTE-158 trial evaluated
the efficacy of pembrolizumab in patients with advanced or
recurrent disease refractory to standard therapy (55). The study demonstrated durable
responses and prolonged survival with pembrolizumab in a subset of
patients with PD-L1-positive tumors, leading to its approval as a
treatment option in this population (56).
Furthermore, metastatic endometrial tumors after
progression in first-line platinum-based chemotherapy are treated
with combination of immunotherapy and tyrosine kinase inhibitors
pembrolizumab and lenvatinib based on results of phase III trial
KEYNOTE-158(56). The use of this
combination is universal and does not require expression of
specific biomarkers. Additionally, the GOG-240 trial investigated
addition of the immune checkpoint inhibitor ipilimumab to standard
chemotherapy in patients with recurrent or metastatic cervical
cancer, showing improved overall survival compared with
chemotherapy-alone (57).
In vulvar and vaginal cancers, clinical trials
evaluating targeted therapies and immunotherapy are relatively
limited due to the rarity of these malignancies. However, ongoing
studies are investigating the role of immune checkpoint inhibitors,
such as pembrolizumab and nivolumab, in patients with advanced or
recurrent disease, with preliminary results showing promising
antitumor activity and manageable safety profiles (58,59).
8. Real-world studies
Zhao et al (60) investigated the efficacy and safety
of niraparib as a first-line maintenance treatment for patients
with advanced ovarian cancer in a real-world setting across
multiple centers in China. The findings revealed that niraparib
provided significant PFS benefits, with PFS rates of 87.4, 75.9 and
63.6% at 6, 12 and 18 months, respectively. Factors such as age
<65 years, BRCA mutation and successful cytoreductive surgery
(R0 status) are associated with prolonged PFS. Additionally,
starting niraparib at a 200 mg dose was effective and had
manageable safety, with the most common severe adverse events being
hematological, including decreased platelet and white blood cell
counts. The study concluded that niraparib is a valuable and safe
option for maintenance therapy in patients with advanced ovarian
cancer, particularly when using an individualized starting dose
strategy.
A retrospective cohort study in the USA evaluated
the tolerability of PARP inhibitors (olaparib, niraparib and
rucaparib) in patients with advanced ovarian cancer (61). The study included 824 patients and
analyzed clinical events of interest such as anemia, neutropenia
and nausea. The findings indicated that while PARP inhibitors are
effective as maintenance therapy, they have a significant
side-effect profile, which varies depending on the PARP inhibitor
used. The aforementioned study highlights the importance of
monitoring and managing adverse effects in real-world clinical
settings (61).
Another real-world study (62) focused on treatment patterns
following disease progression in patients with epithelial ovarian
cancer who received PARP inhibitor maintenance therapy. The
aforementioned study examined subsequent therapies and outcomes,
providing valuable data on how patients fare following disease
progression while receiving PARP inhibitors. The results emphasized
the importance of tailoring post-progression treatment based on
individual patient profiles and previous responses to therapy
(62).
Huepenbecker et al (63) aimed to describe the real-world usage
of immune checkpoint inhibitors in patients with advanced or
recurrent endometrial cancer. The aforementioned study analyzed
data from a nationwide electronic health record-derived database,
focusing on patients who received systemic treatment between
January 2014 and November 2020, followed until May 2021. The study
included 326 patients who received their first immune checkpoint
inhibitors during this period, with usage increasing significantly
over time. Pembrolizumab was the most common immune checkpoint
inhibitor, often combined with lenvatinib. Immune checkpoint
inhibitors were administered as first-, second- or later lines of
therapy, with median time to next treatment being longer when
immune checkpoint inhibitors were given earlier. The study found
regional and stage-associated differences in immune checkpoint
inhibitor usage, and ~1/3 of patients received subsequent
treatments after immune checkpoint inhibitors, with no significant
difference in demographic or clinical characteristics based on
post-immune checkpoint inhibitor treatment type. The findings
highlight the growing role of immune checkpoint inhibitors across
various treatment lines in this population (63).
Passarelli et al (23) presented a case report of a
51-year-old patient with advanced endometrioid endometrial cancer
harboring a PIK3CA mutation who showed an exceptional response to
alpelisib, a PI3K α-selective inhibitor. Despite multiple prior
treatments, including surgery, chemotherapy and hormone therapy,
the disease progressed until alpelisib was introduced. Upon
starting alpelisib, the patient experienced significant clinical
and radiological improvements, with a notable decrease in tumor
size and levels of tumor markers. This case highlights the
potential of precision medicine in treating advanced gynecological
cancers by targeting specific molecular alterations such as PIK3CA
mutations. The aforementioned study emphasizes the importance of
genomic profiling in guiding treatment decisions and suggests that
alpelisib may be a promising option for patients with similar
molecular profiles (23).
9. Role of multiple targeted mutations in
gynecological cancer
Gynecological cancer often harbors multiple genetic
mutations and molecular alterations that contribute to tumor
heterogeneity, treatment resistance and disease progression
(64). Understanding the interplay
between these targeted mutations is key for optimizing treatment
strategies and improving outcomes for patients with gynecological
malignancy.
In ovarian cancer, HGSC, the most common subtype, is
characterized by extensive genomic alterations, including mutations
in tumor suppressor genes (such as TP53 and BRCA1/2) and oncogenes
(such as PIK3CA and KRAS) (65).
The presence of multiple targeted mutations in HGSC underscores the
complexity of the disease and need for personalized treatment
approaches. For example, patients with concurrent mutations in
BRCA1/2 and HRD may benefit from PARP inhibitors, whereas those
with mutations in PIK3CA or KRAS may respond to targeted therapy
against the PI3K/AKT/mTOR or MAPK signaling pathways, respectively
(66). Comprehensive molecular
profiling of tumors is key for identifying actionable mutations and
selecting tailored treatment regimens based on the genetic makeup
of each patient.
Endometrial cancer is characterized by distinct
molecular subtypes with different genetic alterations and clinical
behavior. The Cancer Genome Atlas has identified four molecular
subtypes of endometrial cancer, including DNA polymerase epsilon
ultramutated, MSI and copy number-low and -high, each with unique
genomic features and prognostic implications (22). Patients with MSI-high tumors,
characterized by mutations in DNA MMR genes [such as DNA mismatch
repair protein (MLH1) and MSH2], may benefit from immune checkpoint
inhibitors due to increased tumor mutational burden and enhanced
antitumor immune responses (44).
Conversely, patients with copy number-high tumors, characterized by
amplifications in oncogenes such as Cyclin E1 (CCNE1) and MYC, may
respond to targeted therapy directed against these genetic
alterations (20). Integrating
molecular subtype classification with targeted mutation profiling
enables identification of personalized treatment strategies
tailored to the molecular characteristics of each endometrial
cancer subtype.
Persistent infection with high-risk HPV types,
particularly HPV16 and HPV18, drives cervical cancer by encoding
viral oncoproteins that promote cell transformation and oncogenesis
(67). In addition to HPV
infection, cervical cancer may harbor mutations in genes such as
PIK3CA, PTEN and TP53, which contribute to tumor progression and
treatment resistance (22).
Patients with concurrent HPV infection and targeted mutations may
exhibit distinct clinical behavior and treatment responses,
highlighting the importance of comprehensive molecular profiling in
guiding treatment decisions for cervical cancer.
Vulvar and vaginal cancers are relatively rare
gynecological malignancies that are less well-characterized than
other types of gynecological cancer at the molecular level.
However, mutations in genes such as TP53, PIK3CA and FGFR3 in a
subset of tumors suggest potential therapeutic targets for these
diseases (28). Additionally, HPV
infection is associated with a subset of vulvar and vaginal
cancers, particularly in younger patients, further highlighting the
role of viral oncogenesis in these malignancies (68).
10. Challenges and limitations in clinical
implementation of precision medicine in gynecological cancer
The clinical implementation of precision medicine in
gynecological cancer, while promising, faces several challenges.
These include issues associated with access to advanced genomic
testing, cost and the necessity for interdisciplinary collaboration
between healthcare providers.
Access to advanced genomic
testing
NGS and other molecular profiling techniques are key
components of precision medicine. These technologies enable the
identification of specific genetic mutations and biomarkers to
guide targeted therapy. However, the availability of advanced
diagnostic tools is not uniform across healthcare facilities. In
low-resource settings, the lack of infrastructure and expertise
required to perform comprehensive genomic analysis limits the
adoption of precision medicine. Moreover, even in well-resourced
settings, there can be notable disparities in access based on
geographical location, with urban centers typically having more
advanced diagnostic facilities compared with rural areas (1).
Cost
The high cost of genomic testing and targeted
therapies can be prohibitive for patients. For example, NGS, while
providing comprehensive genomic information, is expensive and its
costs are often not fully covered by insurance policies. This
financial burden can limit patient access to precision medicine
approaches. Additionally, targeted therapy, which is developed
based on specific genetic mutations identified by genomic testing,
tends to be more expensive than conventional treatment. The high
cost of these therapies can strain healthcare budgets and make them
inaccessible. Efforts to reduce the cost of genomic testing and
targeted therapy and to increase insurance coverage for these
services are essential to make precision medicine more accessible
(3).
Interdisciplinary collaboration
The successful implementation of precision medicine
requires interdisciplinary collaboration between various healthcare
providers, including oncologists, geneticists, pathologists and
bioinformaticians. This collaborative approach is necessary to
interpret complex genomic data accurately and integrate this
information into clinical decision-making effectively. However,
fostering such interdisciplinary collaboration can be challenging.
It requires effective communication and coordination between
diverse healthcare professionals, which can be difficult to achieve
in practice. Additionally, there is need for ongoing education and
training for healthcare providers to keep up with rapid
advancements in genomic technology and precision medicine
approaches (4).
Data interpretation and
standardization
Another challenge lies in the interpretation and
standardization of genomic data. The vast amount of data generated
by genomic testing requires sophisticated bioinformatics tools and
expertise to analyze and interpret. Variability in data
interpretation and lack of standardized protocols can lead to
inconsistent clinical recommendations. Therefore, establishing
standardized guidelines and protocols for genomic data
interpretation is key to ensure reliable and actionable insights
from genomic testing (19).
Ethical and privacy concerns
The collection and storage of genomic data raise
issues of patient privacy and data security. Ensuring that genetic
information is protected from unauthorized access and misuse is
key. Additionally, ethical considerations regarding use of genetic
information, such as potential discrimination based on genetic risk
factors, need to be addressed through robust regulatory frameworks
(5).
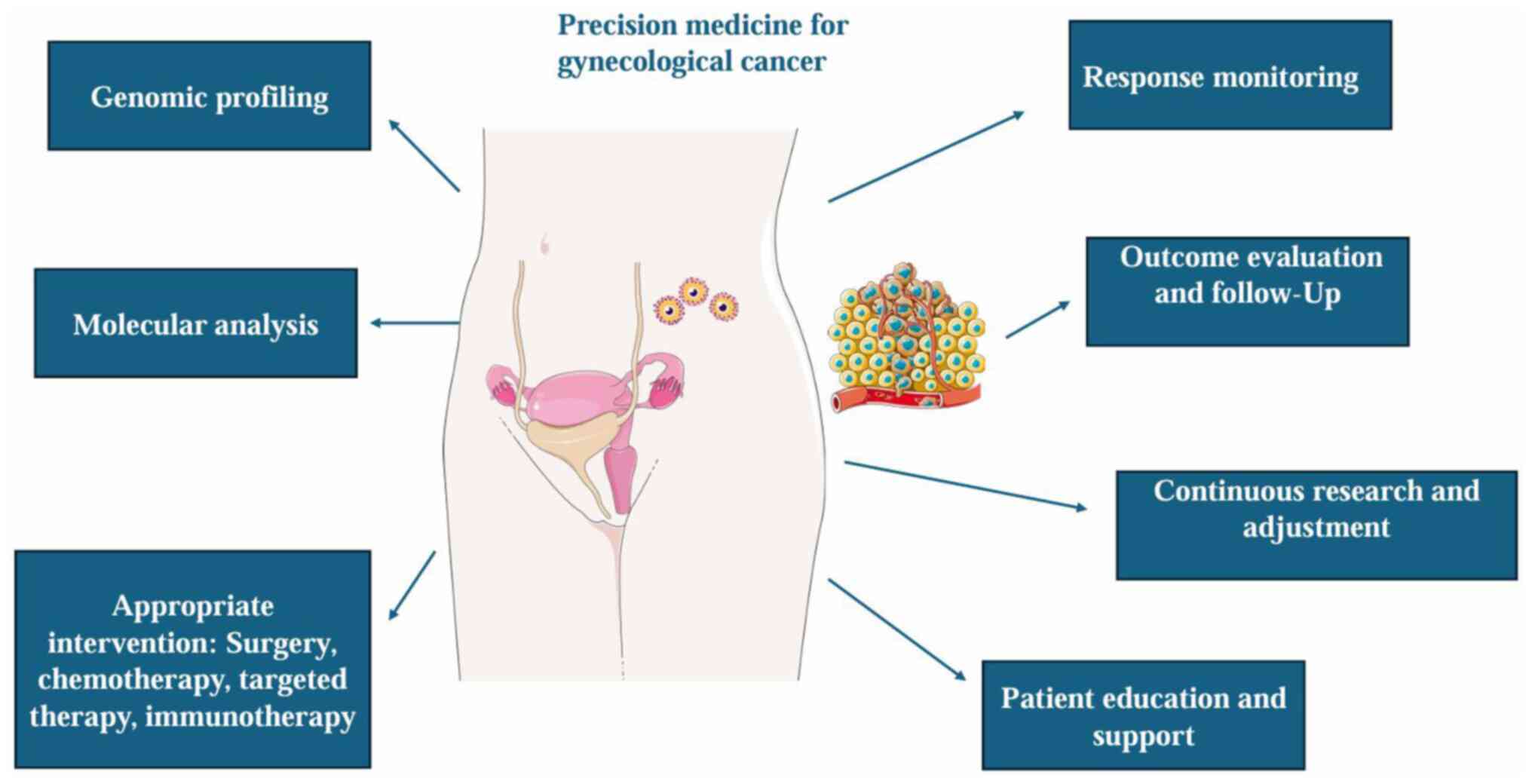
Fig. 1 provides a
schematic illustration of precision medicine in gynecological
cancer.
11. Conclusion
The transition towards personalized and precision
medicine in gynecological oncology signifies a key shift from
conventional treatment paradigms, offering new potential for
improved patient outcomes. Through the utilization of advanced
genomic technology, such as NGS, clinicians can now unravel the
complex molecular landscape of cancers affecting the gynecological
organs. This detailed molecular profiling facilitates
identification of unique genetic mutations and signaling pathways,
enabling selection of targeted therapies tailored to the individual
characteristics of each tumor.
The inherent molecular heterogeneity of
gynecological cancers, presenting a notable challenge in treatment,
is addressed by the ability of precision medicine to identify and
target specific biomarkers and molecular drivers. Successes in
ovarian, cervical and uterine cancer treatments, notably through
the use of PARP inhibitors in BRCA-mutated ovarian cancer,
exemplify the potential of precision medicine to enhance treatment
efficacy while minimizing adverse effects. Focus on molecular
profiling and development of novel targeted therapies may further
refine treatment strategies to optimize outcomes and quality of
life for patients with gynecological cancer. This underscores the
shift towards more personalized care but also highlights potential
for groundbreaking treatments in future.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
AAF and ML conceptualized the study. AAF, ML, MAD,
and VEG wrote the manuscript. ML and MAD analyzed the data and
provided critical revisions. All have read and approved the final
version of the manuscript. Data authentication is not
applicable.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Use of artificial intelligence tools
Chat GPT was used to improve the readability and
language of the manuscript; authors revised and edited the content
produced by the AI tool as necessary, taking full responsibility
for the ultimate content of the present manuscript.
References
|
1
|
Shams M, Abdallah S, Alsadoun L, Hamid YH,
Gasim R and Hassan A: Oncological horizons: The synergy of medical
and surgical innovations in cancer treatment. Cureus.
15(e49249)2023.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Wilson EM, Eskander RN and Binder PS:
Recent therapeutic advances in gynecologic oncology: A review.
Cancers (Basel). 16(770)2024.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Stefanicka-Wojtas D and Kurpas D:
Personalised medicine-implementation to the healthcare system in
europe (focus group discussions). J Pers Med.
13(380)2023.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Hassan M, Awan FM, Naz A, deAndrés-Galiana
EJ, Alvarez O, Cernea A, Fernández-Brillet L, Fernández-Martínez JL
and Kloczkowski A: Innovations in genomics and big data analytics
for personalized medicine and health care: A review. Int J Mol Sci.
23(4645)2022.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Akhoon N: Precision medicine: A new
paradigm in therapeutics. Int J Prev Med. 12(12)2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Zhang A, Miao K, Sun H and Deng CX: Tumor
heterogeneity reshapes the tumor microenvironment to influence drug
resistance. Int J Biol Sci. 18:3019–3033. 2022.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Murawski M, Jagodziński A, Bielawska-Pohl
A and Klimczak A: Complexity of the genetic background of
oncogenesis in ovarian cancer-genetic instability and clinical
implications. Cells. 13(345)2024.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Tsimberidou AM, Fountzilas E, Bleris L and
Kurzrock R: Transcriptomics and solid tumors: The next frontier in
precision cancer medicine. Semin Cancer Biol. 84:50–59.
2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Sadida HQ, Abdulla A, Marzooqi SA, Hashem
S, Macha MA, Akil ASA and Bhat AA: Epigenetic modifications: Key
players in cancer heterogeneity and drug resistance. Transl Oncol.
39(101821)2024.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Thankamony AP, Ramkomuth S, Ramesh ST,
Murali R, Chakraborty P, Karthikeyan N, Varghese BA, Jaikumar VS,
Jolly MK, Swarbrick A and Nair R: Phenotypic heterogeneity drives
differential disease outcome in a mouse model of triple negative
breast cancer. Front Oncol. 13(1230647)2023.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Cordani M, Dando I, Ambrosini G and
González-Menéndez P: Signaling, cancer cell plasticity, and
intratumor heterogeneity. Cell Commun Signal.
22(255)2024.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Goenka A, Khan F, Verma B, Sinha P, Dmello
CC, Jogalekar MP, Gangadaran P and Ahn BC: Tumor microenvironment
signaling and therapeutics in cancer progression. Cancer Commun
(Lond). 43:525–561. 2023.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Imodoye SO, Adedokun KA and Bello IO: From
complexity to clarity: unravelling tumor heterogeneity through the
lens of tumor microenvironment for innovative cancer therapy.
Histochem Cell Biol. 161:299–323. 2024.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Proietto M, Crippa M, Damiani C, Pasquale
V, Sacco E, Vanoni M and Gilardi M: Tumor heterogeneity:
Preclinical models, emerging technologies, and future applications.
Front Oncol. 13(1164535)2023.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Wang Q, Shao X, Zhang Y, Zhu M, Wang FXC,
Mu J, Li J, Yao H and Chen K: Role of tumor microenvironment in
cancer progression and therapeutic strategy. Cancer Med.
12:11149–11165. 2023.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Garlisi B, Lauks S, Aitken C, Ogilvie LM,
Lockington C, Petrik D, Eichhorn JS and Petrik J: The complex tumor
microenvironment in ovarian cancer: Therapeutic challenges and
opportunities. Curr Oncol. 31:3826–3844. 2024.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Radu MR, Prădatu A, Duică F, Micu R,
Creţoiu SM, Suciu N, Creţoiu D, Varlas VN and Rădoi VE: Ovarian
cancer: Biomarkers and targeted therapy. Biomedicines.
9(693)2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Cooper KE, Abdallah KE, Angove RSM,
Gallagher KD and Bonham VL: Navigating access to cancer care:
Identifying barriers to precision cancer medicine. Ethn Dis.
32:39–48. 2022.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Ivanisevic T and Sewduth RN: Multi-omics
integration for the design of novel therapies and the
identification of novel biomarkers. Proteomes.
11(34)2023.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Jaliffa C, Rogel U, Sen I and Singer G:
Comprehensive genomic characterization in ovarian low-grade and
chemosensitive and chemoresistant high-grade serous carcinomas.
Oncology. 1–9. 2024.PubMed/NCBI View Article : Google Scholar : (Epub ahead of
print).
|
|
21
|
Caruso G, Tomao F, Parma G, Lapresa M,
Multinu F, Palaia I, Aletti G and Colombo N: Poly (ADP-ribose)
polymerase inhibitors (PARPi) in ovarian cancer: Lessons learned
and future directions. Int J Gynecol Cancer. 33:431–443.
2023.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Rios-Doria E, Momeni-Boroujeni A, Friedman
CF, Selenica P, Zhou Q, Wu M, Marra A, Leitao MM Jr, Iasonos A,
Alektiar KM, et al: Integration of clinical sequencing and
immunohistochemistry for the molecular classification of
endometrial carcinoma. Gynecol Oncol. 174:262–272. 2023.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Passarelli A, Ventriglia J, Pisano C,
Cecere SC, Napoli MD, Rossetti S, Tambaro R, Tarotto L, Fiore F,
Farolfi A, et al: The way to precision medicine in gynecologic
cancers: The first case report of an exceptional response to
alpelisib in a PIK3CA-mutated endometrial cancer. Front Oncol.
12(1088962)2023.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Li J, Xue X, Zhang Y, Ding F, Wu W, Liu C,
Xu Y, Chen H, Ou Q, Shao Y, et al: The differences in immune
features and genomic profiling between squamous cell carcinoma and
adenocarcinoma-A multi-center study in Chinese patients with
uterine cervical cancer. Gynecol Oncol. 175:133–141.
2023.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Song Y, Bi Z, Liu Y, Qin F, Wei Y and Wei
X: Targeting RAS-RAF-MEK-ERK signaling pathway in human cancer:
Current status in clinical trials. Genes Dis. 10:76–88.
2022.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Tewari KS, Sill MW, Long HJ III, Penson
RT, Huang H, Ramondetta LM, Landrum LM, Oaknin A, Reid TJ, Leitao
MM, et al: Improved survival with bevacizumab in advanced cervical
cancer. N Engl J Med. 370:734–743. 2014.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Friedman CF, Ravichandran V, Miller K,
Vanderbilt C, Zhou Q, Iasonos A, Vivek M, Mishra P, Leitao MM Jr,
Broach V, et al: Assessing the genomic landscape of cervical
cancers: Clinical opportunities and therapeutic targets. Clin
Cancer Res. 29:4660–4668. 2023.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Jenkins TM and Mills AM: Putative
precancerous lesions of vulvar squamous cell carcinoma. Semin Diagn
Pathol. 38:27–36. 2021.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Ferrandina G, Palluzzi E, Gallotta V,
Gambacorta MA, Autorino R, Turco LC, Macchia G, Cosentino F, Gui B,
Mattoli MV, et al: Neo-adjuvant platinum-based chemotherapy
followed by chemoradiation and radical surgery in locally advanced
cervical cancer (Lacc) patients: A phase II study. Eur J Surg
Oncol. 44:1062–1068. 2018.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Pourmasoumi P, Moradi A and Bayat M:
BRCA1/2 mutations and breast/ovarian cancer risk: A new insights
review. Reprod Sci: Aug 6, 2024 (Epub ahead of print).
|
|
31
|
Qu Y, Qin S, Yang Z, Li Z, Liang Q, Long
T, Wang W, Zeng D, Zhao Q, Dai Z, et al: Targeting the DNA repair
pathway for breast cancer therapy: Beyond the molecular subtypes.
Biomed Pharmacother. 169(115877)2023.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Telli ML, Timms KM, Reid J, Hennessy B,
Mills GB, Jensen KC, Szallasi Z, Barry WT, Winer EP, Tung NM, et
al: Homologous recombination deficiency (HRD) score predicts
response to platinum-containing neoadjuvant chemotherapy in
patients with triple-negative breast cancer. Clin Cancer Res.
22:3764–3773. 2016.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Moore K, Colombo N, Scambia G, Kim BG,
Oaknin A, Friedlander M, Lisyanskaya A, Floquet A, Leary A, Sonke
GS, et al: Maintenance olaparib in patients with newly diagnosed
advanced ovarian cancer. N Engl J Med. 379:2495–2505.
2018.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Mirza MR, Monk BJ, Herrstedt J, Oza AM,
Mahner S, Redondo A, Fabbro M, Ledermann JA, Lorusso D, Vergote I,
et al: Niraparib maintenance therapy in platinum-sensitive,
recurrent ovarian cancer. N Engl J Med. 375:2154–2164.
2016.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Li X and Zou L: BRCAness, DNA gaps, and
gain and loss of PARP inhibitor-induced synthetic lethality. J Clin
Invest. 134(e181062)2024.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Guo Z, Zhang R, Yang AG and Zheng G:
Diversity of immune checkpoints in cancer immunotherapy. Front
Immunol. 14(1121285)2023.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Aravantinou-Fatorou A, Andrikopoulou A,
Liontos M, Fiste O, Georgakopoulou VE, Dimopoulos MA,
Gavriatopoulou M and Zagouri F: Pembrolizumab in endometrial
cancer: Where we stand now. Oncol Lett. 22(821)2021.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Hamanishi J, Mandai M, Ikeda T, Minami M,
Kawaguchi A, Murayama T, Kanai M, Mori Y, Matsumoto S, Chikuma S,
et al: Safety and antitumor activity of anti-PD-1 antibody,
nivolumab, in patients with platinum-resistant ovarian cancer. J
Clin Oncol. 33:4015–4022. 2015.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Wang YM, Cai W, Xue QM, Zhang JY, Zhou L,
Xiong SY and Deng H: Prognostic role of different PD-L1 expression
patterns and tumor-infiltrating lymphocytes in high-grade serous
ovarian cancer: A systematic review and meta-analysis. Front
Immunol. 14(1234894)2023.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Andrikopoulou A, Liontos M, Skafida E,
Koutsoukos K, Apostolidou K, Kaparelou M, Rouvalis A, Bletsa G,
Dimopoulos MA and Zagouri F: Pembrolizumab in combination with
bevacizumab and oral cyclophosphamide in heavily pre-treated
platinum-resistant ovarian cancer. Int J Gynecol Cancer.
33:571–576. 2023.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Pujade-Lauraine E, Fujiwara K, Ledermann
JA, Oza AM, Kristeleit R, Ray-Coquard IL, Richardson GE, Sessa C,
Yonemori K, Banerjee S, et al: Avelumab alone or in combination
with chemotherapy versus chemotherapy alone in platinum-resistant
or platinum-refractory ovarian cancer (JAVELIN ovarian 200): An
open-label, three-arm, randomised, phase 3 study. Lancet Oncol.
22:1034–1046. 2021.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Howitt BE, Shukla SA, Sholl LM,
Ritterhouse LL, Watkins JC, Rodig S, Stover E, Strickland KC,
D'Andrea AD, Wu CJ, et al: Association of polymerase e-mutated and
microsatellite-instable endometrial cancers with neoantigen load,
number of tumor-infiltrating lymphocytes, and expression of PD-1
and PD-L1. JAMA Oncol. 1:1319–1323. 2015.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Zhang C, Wang M and Wu Y: Features of the
immunosuppressive tumor microenvironment in endometrial cancer
based on molecular subtype. Front Oncol. 13(1278863)2023.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Le DT, Durham JN, Smith KN, Wang H,
Bartlett BR, Aulakh LK, Lu S, Kemberling H, Wilt C, Luber BS, et
al: Mismatch repair deficiency predicts response of solid tumors to
PD-1 blockade. Science. 357:409–413. 2017.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Heeren AM, Punt S, Bleeker MC,
Gaarenstroom KN, van der Velden J, Kenter GG, de Gruijl TD and
Jordanova ES: Prognostic effect of different PD-L1 expression
patterns in squamous cell carcinoma and adenocarcinoma of the
cervix. Mod Pathol. 29:753–763. 2016.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Frenel JS, Le Tourneau C, O'Neil B, Ott
PA, Piha-Paul SA, Gomez-Roca C, van Brummelen EMJ, Rugo HS, Thomas
S, Saraf S, et al: Safety and efficacy of pembrolizumab in
advanced, programmed death ligand 1-positive cervical cancer:
Results from the phase Ib KEYNOTE-028 trial. J Clin Oncol.
35:4035–4041. 2017.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Choschzick M, Gut A and Fink D: PD-L1
receptor expression in vulvar carcinomas is HPV-independent.
Virchows Arch. 473:513–516. 2018.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Borella F, Preti M, Bertero L, Collemi G,
Castellano I, Cassoni P, Cosma S, Carosso AR, Bevilacqua F, Gallio
N, et al: Is there a place for immune checkpoint inhibitors in
vulvar neoplasms? A state of the art review. Int J Mol Sci.
22(190)2020.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Praiss A, Navitski A, Cohen S,
Tessier-Cloutier B, Broach V and O'Cearbhaill RE: Immunotherapy for
recurrent or metastatic vulvar carcinoma: A case report and review
of current guidelines. Gynecol Oncol Rep. 41(100982)2022.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Xu Y, Xiong F, Li H, Zheng H, Jiang J, Li
Q, Li G, Zhao W, Li R, Li J, et al: Biomarker-driven targeted
therapy in patients with recurrent platinum-resistant epithelial
ovarian cancer (BRIGHT): Protocol for an open-label, multicenter,
umbrella study. Int J Gynecol Cancer. 34:1461–1465. 2024.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Lee JY, Kim BG, Kim JW, Lee JB, Park E,
Joung JG, Kim S, Choi CH and Kim HS: Korean Gynecologic Oncology
Group (KGOG) investigators. Biomarker-guided targeted therapy in
platinum-resistant ovarian cancer (AMBITION; KGOG 3045): A
multicentre, open-label, five-arm, uncontrolled, umbrella trial. J
Gynecol Oncol. 33(e45)2022.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Ray-Coquard I, Pautier P, Pignata S, Pérol
D, González-Martín A, Berger R, Fujiwara K, Vergote I, Colombo N,
Mäenpää J, et al: Olaparib plus bevacizumab as first-line
maintenance in ovarian cancer. N Engl J Med. 381:2416–2428.
2019.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Marabelle A, Le DT, Ascierto PA, Di
Giacomo AM, De Jesus-Acosta A, Delord JP, Geva R, Gottfried M,
Penel N, Hansen AR, et al: Efficacy of pembrolizumab in patients
with noncolorectal high microsatellite instability/mismatch
repair-deficient cancer: Results from the phase II KEYNOTE-158
study. J Clin Oncol. 38:1–10. 2020.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Heery CR, O'Sullivan-Coyne G, Madan RA,
Cordes L, Rajan A, Rauckhorst M, Lamping E, Oyelakin I, Marté JL,
Lepone LM, et al: Avelumab for metastatic or locally advanced
previously treated solid tumours (JAVELIN solid tumor): A phase 1a,
multicohort, dose-escalation trial. Lancet Oncol. 18:587–598.
2017.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Makker V, Taylor MH, Aghajanian C, Oaknin
A, Mier J, Cohn AL, Romeo M, Bratos R, Brose MS, DiSimone C, et al:
Lenvatinib plus pembrolizumab in patients with advanced endometrial
cancer. J Clin Oncol. 38:2981–2992. 2020.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Makker V, Colombo N, Casado Herráez A,
Santin AD, Colomba E, Miller DS, Fujiwara K, Pignata S, Baron-Hay
S, Ray-Coquard I, et al: Lenvatinib plus pembrolizumab for advanced
endometrial cancer. N Engl J Med. 386:437–448. 2022.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Tewari KS, Sill MW, Penson RT, Huang H,
Ramondetta LM, Landrum LM, Oaknin A, Reid TJ, Leitao MM, Michael
HE, et al: Bevacizumab for advanced cervical cancer: Final overall
survival and adverse event analysis of a randomised, controlled,
open-label, phase 3 trial (gynecologic oncology group 240). Lancet.
390:1654–1663. 2017.PubMed/NCBI View Article : Google Scholar
|
|
58
|
How JA, Jazaeri AA, Soliman PT, Fleming
ND, Gong J, Piha-Paul SA, Janku F, Stephen B and Naing A:
Pembrolizumab in vaginal and vulvar squamous cell carcinoma: A case
series from a phase II basket trial. Sci Rep.
11(3667)2021.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Naumann RW, Hollebecque A, Meyer T, Devlin
MJ, Oaknin A, Kerger J, López-Picazo JM, Machiels JP, Delord JP,
Evans TRJ, et al: Safety and efficacy of nivolumab monotherapy in
recurrent or metastatic cervical, vaginal, or vulvar carcinoma:
Results from the phase I/II CheckMate 358 trial. J Clin Oncol.
37:2825–2834. 2019.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Zhao M, Qiu S, Wu X, Miao P, Jiang Z, Zhu
T, Xu X, Zhu Y, Zhang B, Yuan D, et al: Efficacy and safety of
niraparib as first-line maintenance treatment for patients with
advanced ovarian cancer: Real-world data from a multicenter study
in China. Target Oncol. 18:869–883. 2023.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Simmons D, Blank S, Nagar S, Nham T, Long
G, Davis K, Wetherill G, Munley J and McLaurin K: Real-world
evaluation of PARP inhibitor tolerability in advanced ovarian
cancer: Retrospective US cohort study (2209). Gynecologic Oncology.
176 (Suppl 1):S262–S263. 2023.
|
|
62
|
Zhang N, Zheng H, Gao Y, Shu T, Wang H and
Cai Y: A real-world study of treatment patterns following disease
progression in epithelial ovarian cancer patients undergoing
poly-ADP-ribose polymerase inhibitor maintenance therapy. J Ovarian
Res. 17(55)2024.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Huepenbecker S, Meyer LA, Craft M, Chan
JK, Craggs C, Lambert P and Lin YG: Real-world use of immune
checkpoint inhibitors in advanced or recurrent endometrial cancer.
Int J Gynecol Cancer. (ijgc-2024-005541)2024.PubMed/NCBI View Article : Google Scholar : (Epub ahead of
print).
|
|
64
|
Testa U, Petrucci E, Pasquini L, Castelli
G and Pelosi E: Ovarian cancers: Genetic abnormalities, tumor
heterogeneity and progression, clonal evolution and cancer stem
cells. Medicines (Basel). 5(16)2018.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Kotnik EN, Mullen MM, Spies NC, Li T,
Inkman M, Zhang J, Martins-Rodrigues F, Hagemann IS, McCourt CK,
Thaker PH, et al: Genetic characterization of primary and
metastatic high-grade serous ovarian cancer tumors reveals distinct
features associated with survival. Commun Biol.
6(688)2023.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Lliberos C, Richardson G and Papa A:
Oncogenic pathways and targeted therapies in ovarian cancer.
Biomolecules. 14(585)2024.PubMed/NCBI View Article : Google Scholar
|
|
67
|
Pešut E, Đukić A, Lulić L, Skelin J, Šimić
I, Milutin Gašperov N, Tomaić V, Sabol I and Grce M: Human
papillomaviruses-associated cancers: An update of current
knowledge. Viruses. 13(2234)2021.PubMed/NCBI View Article : Google Scholar
|
|
68
|
Van Arsdale A, Turker L, Chang YC, Gould
J, Harmon B, Maggi EC, Meshcheryakova O, Brown MP, Luong D, Van
Doorslaer K, et al: Structure and transcription of integrated HPV
DNA in vulvar carcinomas. NPJ Genom Med. 9(35)2024.PubMed/NCBI View Article : Google Scholar
|