Introduction
Proper assessment of hepatic functional reserve is
crucial to the selection of patients for hepatic surgery,
particularly in liver transplantation and the management of liver
cirrhosis. The Child-Pugh score (1,2) is
now used worldwide as the standard in the assessment of hepatic
functional reserve (3). Given the
relation between this score and survival in patients with cirrhosis
of the liver, it has recently been listed as one of the parameters
in the minimal criteria of the liver transplant waiting list
(4). The criteria are defined as a
predicted 1-year survival rate of ≤90% (4), which generally includes those with a
Child-Pugh score of ≥7, i.e., Child-Pugh Class B or C.
A number of blood biochemical tests have been used
to clinically evaluate hepatic functional reserve, including the
serum albumin test, prothrombin time test, hepaplastin test,
galactose-elimination capacity test (5), 14C-aminopyrine breath test (6), as well as testing for serum
cholinesterase activity and indocyanine green retention rate at 15
min after administration (ICGR15) (7). Although these clinical parameters are
indeed useful for assessing hepatic functional reserve,
discrepancies between them and histological findings are common,
suggesting in turn that the parameters do not always accurately
reflect hepatic functional reserve (8,9).
Reserve function is often assessed by scintigraphy, particularly in
Japan using technetium-99m-galactosyl human serum albumin
(Tc-99m-GSA), a synthetic radioligand that binds to the
asialoglycoprotein receptor on the plasma membrane of liver cells
(10–12). Tc-99m-GSA scintigraphy enables more
objective evaluation of hepatic functional reserve than the above
clinical parameters (13). Many
institutions have described methods for predicting hepatic
functional reserve by Tc-99m-GSA scintigraphy (14–17).
However, a consensus on the best method has not yet been reached
(7).
Superparamagnetic iron oxide (SPIO) is a
liver-specific particulate magnetic resonance (MR) contrast agent
taken up by Kupffer cells (KCs) in the liver. Uptake of this agent
reduces the signal-intensity of hepatic parenchyma and hepatic
tumors, such as well-differentiated hepatocellular carcinoma (HCC)
and dysplastic nodules (18) in
accordance with the phagocytic activity of KCs. Previous studies
have reported that cirrhotic tissue has a lower response to SPIO
than non-cirrhotic tissue due to the reduction of the phagocytic
activity of KCs in a cirrhotic liver (19–23).
Given the suspected close correlation between phagocytic activity
of KCs and hepatic functional reserve, we speculated that SPIO-MRI
may be suitable for the evaluation of hepatic functional reserve.
However, it is difficult to assess KC function either ex
vivo or in vivo, although morphologic evaluation of KCs
can be estimated with immunohistologic staining and supporting data
are limited.
To clarify the correlation between KC function and
hepatocye function, we aimed to analyze the correlation between the
conventional indices of hepatic functional reserve (biochemical
markers and Child-Pugh score) and both SPIO-MRI and Tc-99m-GSA
scintigraphy in patients with chronic viral hepatitis, and to
determine whether or not SPIO-MRI effectively evaluates hepatic
functional reserve.
Materials and methods
Patients
Our institutional review board approved our
retrospective study and waived the informed consent
requirement.
The inclusion criteria for the study were patients
with chronic viral hepatitis who underwent SPIO-MRI for assessment
of focal hepatic lesions and Tc-99m-GSA scintigraphy for assessment
of hepatic functional reserve before hepatic surgery or
interventional treatments for HCC. Consecutive 46 patients with
hepatic dysfunction, who had hepatitis C virus (n=43) or hepatitis
B virus infections (n=3) were enrolled in this retrospective study
during a 6-month period. There were no exclusions. The patients
were aged 46–83 years (median 70) and included 29 men and 17 women.
Twenty-nine patients were pathologically diagnosed by surgery for
HCC or diagnostic hepatic biopsy under ultrasonography with a
22-gauge core biopsy needle (cirrhosis, n=22; chronic hepatitis,
n=7). The remaining 17 patients were diagnosed based on a range of
imaging and clinical parameters, including findings on
ultrasonography, computed tomography, endoscopic examination,
biochemical markers and physical examination by two physicians
(N.O. and J.A.) blinded to radiological image information.
The Child-Pugh score is generally categorized into
three groups for evaluating hepatic functional reserve: class A,
including patients with a score of 5 or 6; class B, including
patients with a score from 7 to 9; and class C, including patients
with a score from 10 to 15 (2). In
the present study, 46 patients were classified into four groups:
chronic hepatitis (Child-Pugh score of <5; group CH, n=16);
cirrhosis with Child-Pugh class A (Child-Pugh A, n=11); and
Child-Pugh class B (n=16) or C (n=3) (hereafter, Child-Pugh B/C,
n=19).
Superparamagnetic iron oxide-magnetic
resonance imaging (MRI)
MRI was performed at a field strength of 1.0-T
(Gyroscan T10-NT; Philips, Best, Netherlands) using a body
phased-array coil. Ferumoxides (Feridex; Eiken Chemical, Tokyo,
Japan) were administered as SPIO via slow intravenous drip infusion
(median 30 min; range 25–36) at a dose of 10 μmol/kg. MRI was
performed 30 min after completion of the infusion.
T2-weighted gradient-recalled echo (GRE) images were
obtained in the transverse plane from all patients before and after
administration of SPIO. The scanning parameters on the T2-weighted
GRE sequence were as follows: repetition time = 280 msec, echo time
= 14 msec, flip angle = 30°, an 8-mm section thickness, a 1-mm gap,
a 35-cm field of view, 256 × 205 rectangular matrix, 16 sections
and one signal acquired during a 22-sec breath hold. These scanning
parameters were unchanged for T2-weighted GRE sequences before and
after administration of SPIO.
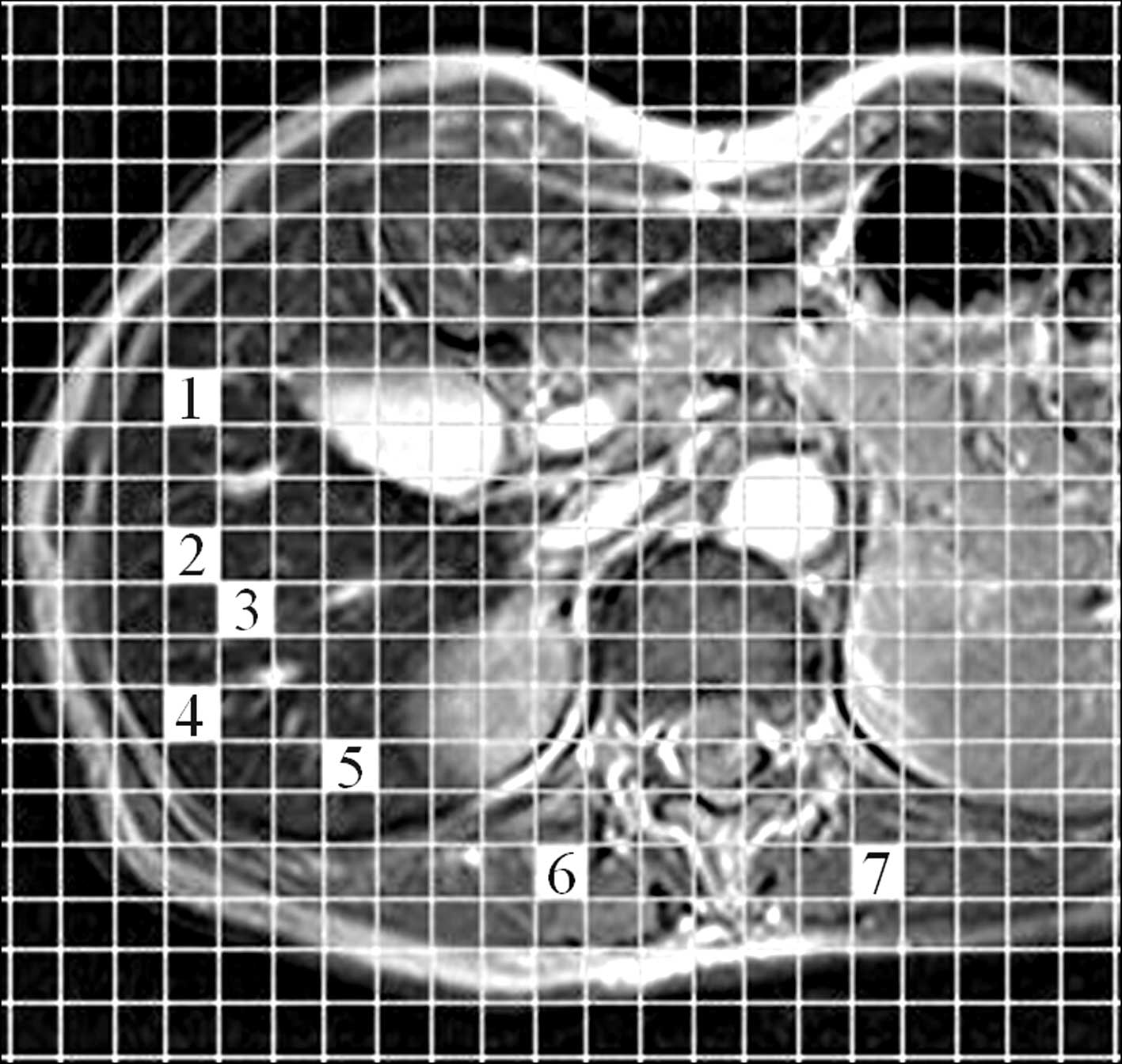
Quantitative image analysis was conducted by
measurement of signal intensities of the liver parenchyma and
paraspinous muscle. All regions of interest (ROIs) were determined
by two independent radiologists (T.T. and A.S.) using plug-in
software developed in-house by one of the authors (K.F.) (Fig. 1). Five separate ROIs were placed
over the right hepatic lobe on the T2-weighted GRE images in three
different slice sections, and liver signal intensities were
recorded as the mean values generated (liver ROI area, 500
mm2). Liver signal intensities were measured before and
after administration of SPIO, avoiding large vessels, focal hepatic
lesions or artifacts in the same locations on the images. The
procedure was repeated to measure muscle signal intensity by
placing two separate ROIs on the right and left paraspinous
muscles, avoiding the intermuscular fat on the transverse sections
used to measure liver signal intensity (muscle ROI area, 200
mm2). Liver-to-muscle signal intensity ratio (LMR) was
calculated for T2-weighted GRE images before and after
administration of SPIO (24).
To assess the effect of SPIO for each patient group,
the reduction percentage of LMR (reduction-%LMR) before and after
administration of SPIO was calculated as follows:
LMR = mean signal intensities of the liver
parenchyma/mean signal intensities of the muscle.
Reduction-%LMR (%) = (post-LMR - pre-LMR)/pre-LMR x
100, where pre-LMR is the LMR before SPIO injection and post-LMR is
the LMR after injection.
Tc-99m galactosyl human serum albumin
scintigraphy
All parameters for Tc-99m-GSA scintigraphy were
assessed by consensus of two observers (M.I. and S.M.)
independently of the previously mentioned observers. All patients
underwent hepatic imaging with Tc-99m-GSA under a γ-camera
(ZLC-7500; Shimadzu, Kyoto, Japan) placed over the chest abdominal
field. After an overnight fast, 185 MBq of Tc-99m-GSA was
administered by bolus injection. The patient was then placed in a
supine position and a dynamic image was captured. Anterior
abdominal images, including the heart and liver, were obtained
continuously for 30 min. Time-activity curves for the heart and
liver were generated from ROIs covering the whole organ.
Quantitative indices were calculated from the
time-activity curves, including the index of blood clearance (HH15
= H15/H3), which is defined as the uptake ratio of the heart at 15
min (H15) to that at 3 min (H3) after Tc-99m-GSA injection, and the
receptor index (LHL15 = L15/H15 + L15), which is defined as the
uptake ratio of the liver at 15 min to that of the liver and heart
at 15 min after injection, where L15 is the radioactivity of the
liver at 15 min after injection (Fig.
2). The index of blood clearance was calculated by dividing the
radioactivity of the heart ROI at 15 min after Tc-99m-GSA injection
by that of the heart ROI at 3 min after injection (25). The receptor index was calculated by
dividing the radioactivity of the liver ROI by that of the liver
plus heart ROIs at 15 min after the injection (25).
The median interval between SPIO-MRI and Tc-99m-GSA
scintigraphy was 10 days (range 2–18).
Statistical analysis
Skewed data were summarized for all non-parametric
methods using the median and the 25th to 75th percentile of the
interquartile range.
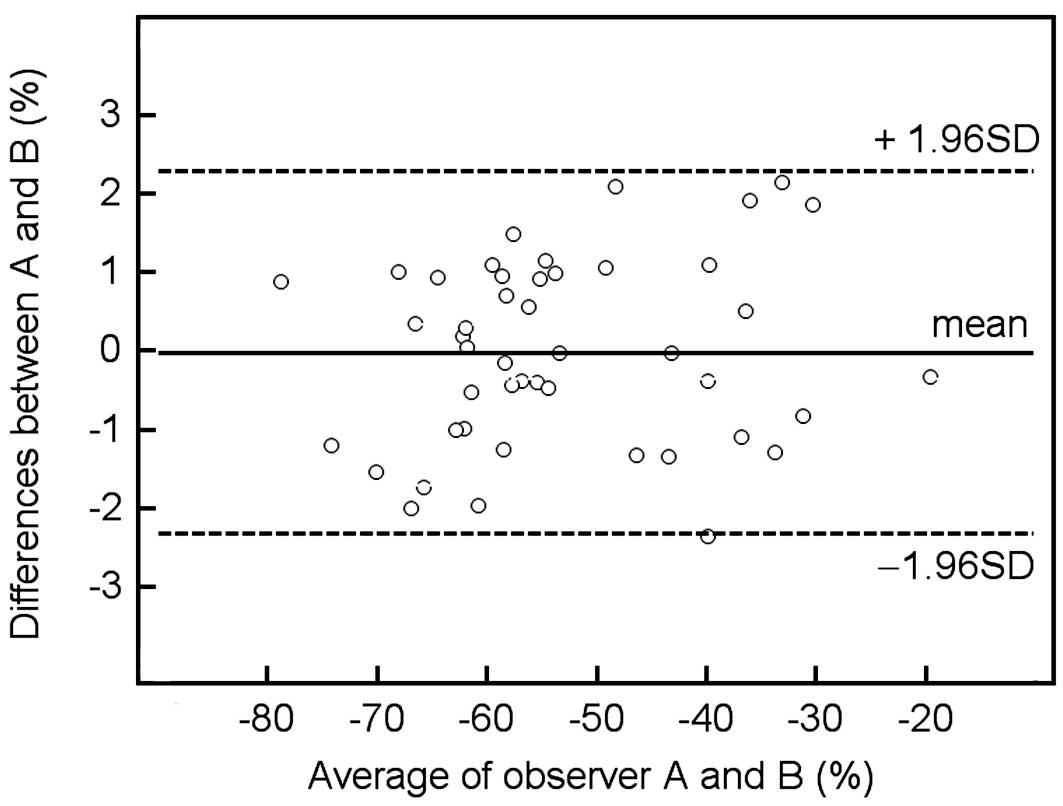
A Bland-Altman plot (26) was used to analyze inter-observer
agreement for the reduction-%LMR on T2-weighted GRE images. The
correlation of the reduction-%LMR on T2-weighted GRE images
obtained by the two observers was determined using the Pearson
correlation coefficient. Spearman's rank correlation test was used
to analyze the association between the conventional indices of
hepatic functional reserve (biochemical markers and Child-Pugh
score) with the reduction-%LMR on SPIO-MRI as well as each
Tc-99m-GSA scintigraphy parameter (i.e., HH15 or LHL15). The
Kruskal-Wallis test was used to determine the significance of
intergroup differences between reduction-%LMR, HH15 and LHL15. When
results revealed statistical significance, multiple comparisons of
each coupled combination were conducted using the Mann-Whitney U
test with Bonferroni correction.
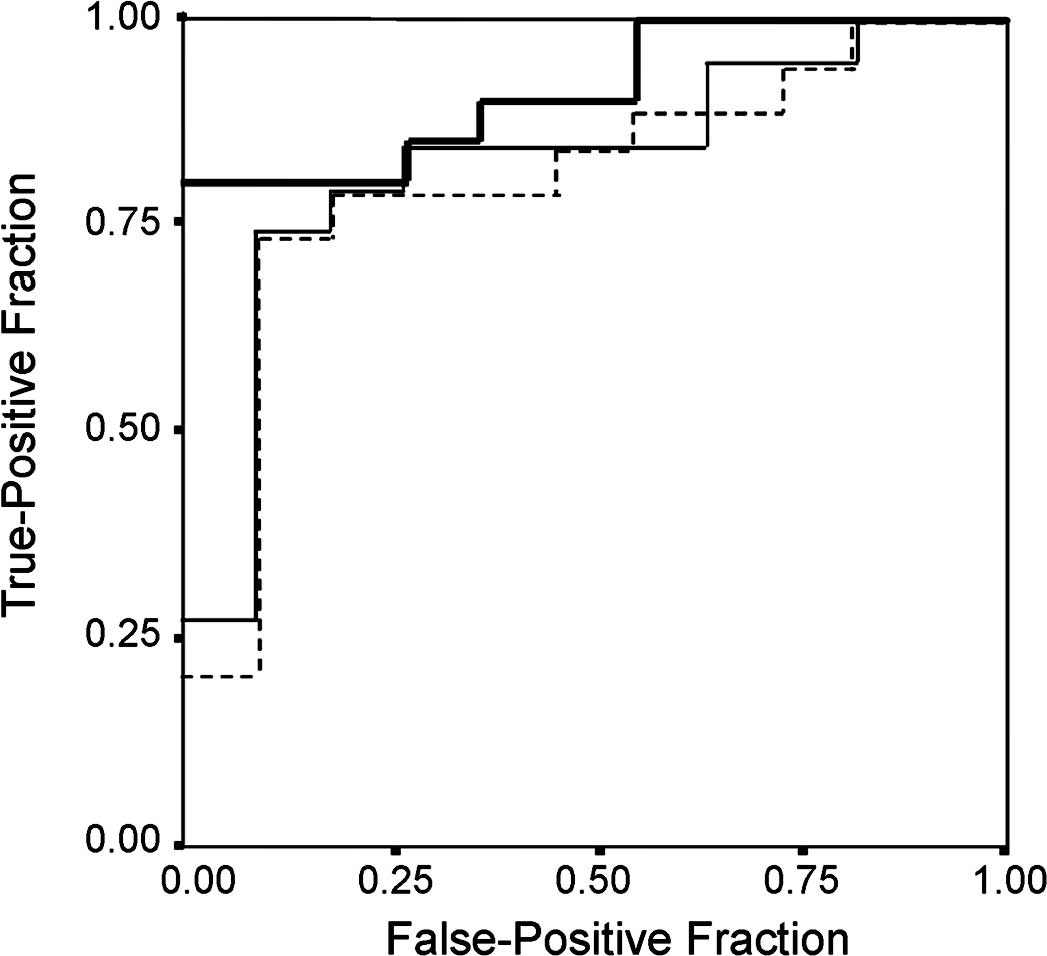
In the cirrhotic groups, receiver operating
characteristic (ROC) analysis was performed to evaluate the
usefulness of reduction-%LMR, HH15 or LHL15 as markers for
differentiating Child-Pugh A from Child-Pugh B/C when selecting
liver transplant patients from a waiting list (4). Calculations of area under the ROC
curve (AUC) found a range from 0.5 to 1.0, which increased when
diagnostic performance approached that of the reference standard
(in the present case, determination of Child-Pugh B/C).
Sensitivity, specificity, positive predictive value and negative
predictive value were calculated with standard formulas according
to the values of these indices and with varied index values that
indicated positive differentiation (i.e., threshold value).
P<0.05 was considered statistically significant.
All analyses were performed using SPSS statistical software
(version 12.0 J; SPSS, Inc., Chicago, IL, USA).
Results
Interobserver agreement for the
reduction-%LMR on T2-weighted GRE images
There was no significant difference between
measurements made by the two observers; the interclass Pearson
correlation coefficient was 0.98 (95% confidence interval,
0.97–0.99) for reduction-%LMR; the mean difference (± standard
deviation) was −0.018±1.17% and the coefficient repeatability was
2.29. The Bland-Altman plot with 95% limits of agreement is shown
in Fig. 3. There was no
proportional bias or fixed bias.
Correlation between the conventional
indices (biochemical markers and Child-Pugh score) and parameters
of each modality
Results showed the reduction-%LMR to be positively
correlated with asparatate aminotransferase (Spearman r=0.52;
P<0.001), ICGR15 (r=0.58; P<0.001), hyaluronic acid (r=0.53;
P<0.001) and Child-Pugh score (r=0.77; P<0.001). The
reduction-%LMR was found to be negatively correlated with serum
albumin level (r=−0.62; P<0.001), platelet count (r=−0.55;
P<0.001) and prothrombin time (r=−0.56; P<0.001).
Correlations between the conventional indices of hepatic functional
reserve and reduction-%LMR, HH15 and LHL15 are shown in Table I.
 | Table I.Correlation of the parameters on
SPIO-MRI and Tc-99m-GSA scintigraphy with conventional indices. |
Table I.
Correlation of the parameters on
SPIO-MRI and Tc-99m-GSA scintigraphy with conventional indices.
| SPIO-MRI
| Tc-99m-GSA
scintigraphy
|
|---|
| Reduction-%LMR | HH15 | LHL15 |
|---|
| AST (IU/l) | 0.52a | 0.59a | −0.62a |
| ALT (IU/l) | 0.19 | 0.19 | −0.21 |
| γ-GTP (IU/l) | 0.10 | 0.24 | −0.18 |
| T-Bil (mg/dl) | 0.36b | 0.57a | −0.50a |
| Alb (g/dl) | −0.62a | −0.61a | 0.64a |
| Plt
(104/μl) | −0.55a | −0.64a | 0.69a |
| PT (%) | −0.56a | −0.47b | 0.49b |
| ICGR15 (%) | 0.58a | 0.67a | −0.73a |
| HA (ng/ml) | 0.53a | 0.74a | −0.73a |
| Child-Pugh
score | 0.77a | 0.62a | 0.60a |
Significant intergroup differences for
the parameters of each modality
Significant differences were found between the four
groups for reduction-%LMR, HH15 and LHL15 (Kruskal-Wallis,
P<0.001, all comparisons). With regard to each coupled
combination, significant differences in reduction-%LMR and HH15
were found between group CH and Child-Pugh B, between group CH and
Child-Pugh C, between Child-Pugh A and Child-Pugh B, and between
Child-Pugh A and Child-Pugh C (Bonferroni test, P<0.05, all
comparisons), but no difference was found between group CH and
Child-Pugh A or between Child-Pugh B and Child-Pugh C (Table II). For LHL15, in addition to the
results mentioned above, a significant difference was found between
Child-Pugh B and Child-Pugh C (Table
II).
 | Table II.Multiple comparisons of each group
coupled combination for reduction-%LMR, HH15 and LHL15. |
Table II.
Multiple comparisons of each group
coupled combination for reduction-%LMR, HH15 and LHL15.
| SPIO-MRI
| Tc-99m-GSA
scintigraphy
|
|---|
| Group according to
hepatic function reserve | Reduction-%LMR | HH15 | LHL15 |
|---|
| CH (n=16) | −62.1 (−67.7,
−58.6)a | 0.51 (0.59,
0.43)a | 0.92 (0.94,
0.88)a |
| Class A (n=11) | −57.7 (−62.0,
−54.7)a | 0.58 (0.63,
0.51)b | 0.88 (−0.91,
0.84)b |
| Class B (n=16) | −41.5 (−53.2,
−36.1)a | 0.75 (0.78,
0.61)a,b | 0.78 (0.84,
0.75)a,b |
| Class C (n=3) | −33.7 (−39.9,
−25.0)a | 0.85 (0.85,
0.84)a,b | 0.62 (0.65,
0.49)a,b |
ROC analysis for the parameters of each
modality in cirrhotic groups
Reduction-%LMR [AUC=0.91; 95% confidence interval
(CI) 0.80–1.00, P<0.001] was a more useful parameter in
differentiating Child-Pugh A from Child-Pugh B/C than HH15
(AUC=0.80; 95% CI 0.64–0.98) or LHL15 (AUC=0.82; 95% CI 0.66–0.98)
(Fig. 4). ROC analysis indicated
that the −50% threshold level for reduction-%LMR was suitable for
differentiating Child-Pugh A from Child-Pugh B/C. Based on the
threshold values of −50%, the sensitivity, specificity, positive
predictive and negative predictive values for reduction-%LMR were
0.79, 0.91, 0.94 and 0.71, respectively (Table III).
 | Table III.Diagnostic rates of reduction-%LMR
according to cutoff value for differentiation of Child-Pugh class A
and class B/C. |
Table III.
Diagnostic rates of reduction-%LMR
according to cutoff value for differentiation of Child-Pugh class A
and class B/C.
| Diagnostic rate
(95% confidence interval)
|
|---|
| Variablea | Liver cirrhosis
(n=30) | P-valueb | Sensitivity | Specificity | PPV | NPV |
|---|
| Reduction-%LMR | | | | | | |
| < −50% | 16 | <0.001 | 0.79
(0.54–0.94) | 0.91
(0.59–0.99) | 0.94
(0.70–0.99) | 0.71
(0.42–0.92) |
| ≥50% | 14 | | | | | |
Discussion
In the present study, we demonstrated that SPIO-MRI
was a useful non-invasive method for evaluating hepatic functional
reserve. Furthermore, reduction-%LMR, as a surrogate parameter of
phagocytic activity of KCs, was found to be well correlated with
Child-Pugh score and also with biochemical markers, particularly
serum albumin, prothrombin time and ICGR15 in patients with chronic
viral hepatitis (Table I). These
findings support the hypothesis that phagocytic activity of KCs is
closely correlated with hepatocyte function in patients with
chronic viral hepatitis (27,28).
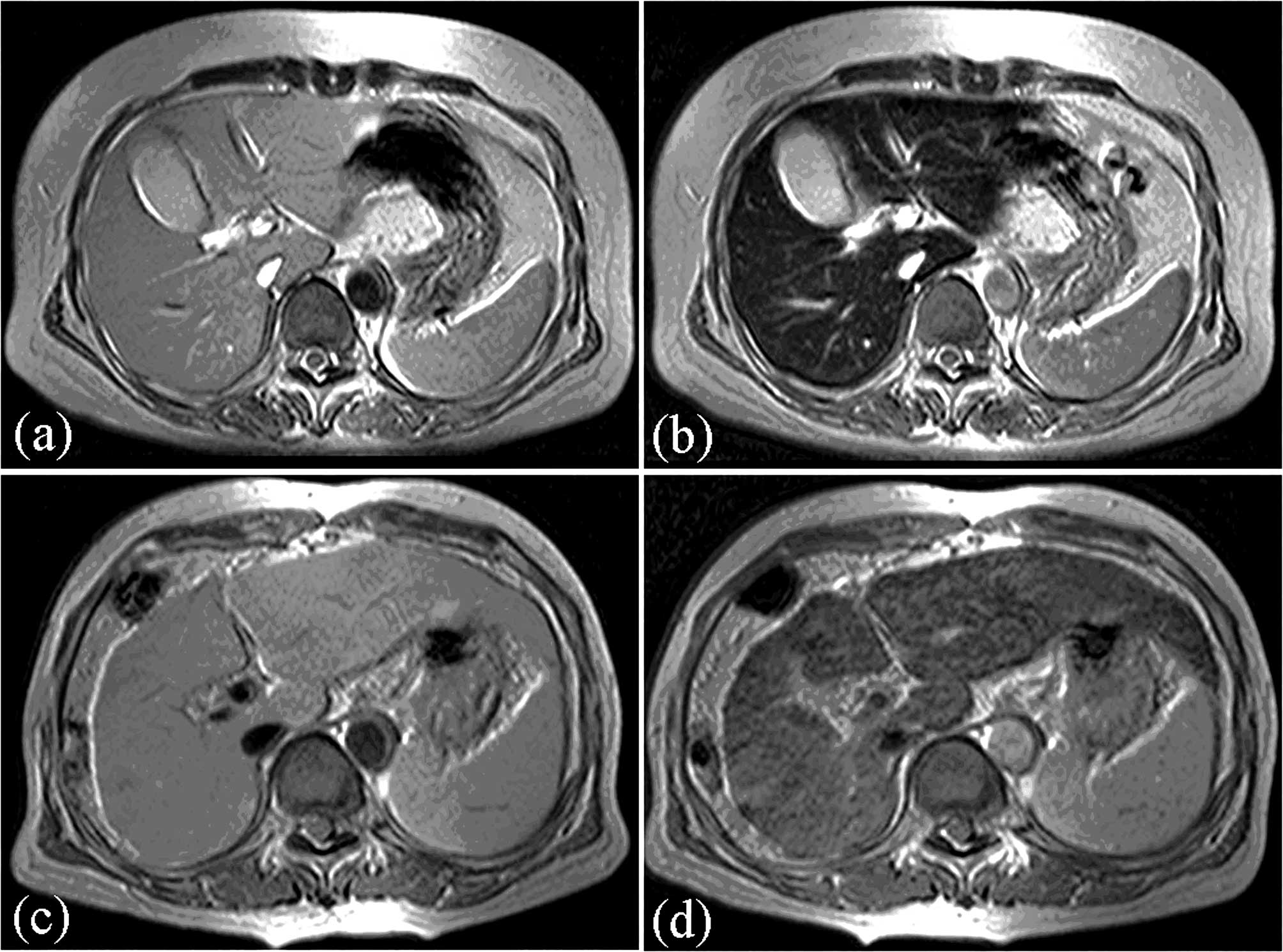
Pathologically, hepatic cirrhosis is defined as an
irreversible diffuse fibrosis or scarring of the liver. Cirrhosis
causes a decrease in hepatic function reserve and is a common
endpoint for many chronic liver diseases. Previous studies have
reported that the decrease in signal intensity in SPIO-produced
liver parenchyma is not as great in patients without cirrhosis as
in those with cirrhosis (19–23)
(Fig. 5).
SPIO-produced signal intensity is dependent on both
the number of sinusoidal KCs per unit volume of hepatic parenchyma
(KC density) and the level of activity in each KC (22). Namely, it has been considered to
represent the phagocytic activity of KCs. However, recent studies
have reported that impairment of KC phagocytic activity is
dependent on the level of activity in each KC and is not dependent
on a reduction in the total number of KCs in studies of animal
models of non-alcoholic steatohepatitis (29,30).
Reduction-%LMR on SPIO-MRI may, therefore, reflect
the level of activity in each KC in chronic viral hepatitis. In
other words, the level of activity in each KC may be closely
correlated with hepatocyte function.
With regard to the evaluation of hepatic functional
reserve by biochemical markers, several authors have reported that
markers, such as serum albumin level and prothrombin time, do not
accurately reflect hepatic functional reserve, since these
parameters are affected by the blood product supplements used to
treat liver cirrhosis. Furthermore, these studies also reported
that the ICGR15 does not allow for reserve measurement in patients
with elevated bilirubin levels and portosystemic shunts (11,12).
On the other hand, several methods have been
reported for calculating hepatic Tc-99m-GSA uptake in order to
ensure maximum clinical efficacy in the evaluation of reserve by
Tc-99m-GSA scintigraphy (10–12).
Previous studies reported that Tc-99m-GSA scintigraphy is able to
evaluate the decrease in hepatic functional reserve caused by
portosystemic shunts more precisely than biochemical markers
(31,32).
In the present study, there were significant
differences among groups for HH15 and LHL15 (Table II). We also found that these
parameters were well correlated with the Child-Pugh score and with
biochemical markers, as well as with the results of previous
studies on Tc-99m-GSA scintigraphy (10–12,25).
However, in comparison to SPIO-MRI with scintigraphy, our results
showed that Child-Pugh score and prothrombin time are closely
correlated with reduction-%LMR on SPIO-MRI rather than HH15 and
LHL15 on Tc-99m-GSA scintigraphy.
Several authors have investigated the efficacy of
SPIO-MRI for the detection of hepatic fibrosis in patients with
chronic liver disease (33,34);
their results showed that SPIO-MRI was useful for evaluating
hepatic fibrosis. In the present study, there was statistical
correlation between SPIO-MRI and hyaluronic acid, which is used
widely as a marker of hepatic fibrosis (35,36).
This result also supports that reduction-%LMR on SPIO-MRI may be
useful for evaluating hepatic fibrosis, potentially allowing for
more accurate evaluation of hepatic functional reserve.
Liver transplantation is now firmly established as a
general treatment for patients with terminal liver disease.
Generally, the minimal criteria for liver transplantation are those
established by the American Society of Transplant Physicians and
American Association for the Study of Liver Disease in 1997,
regardless of etiology (4). The
criteria are defined as a predicted 1-year survival rate of ≤90%
(4), which generally includes
those with a Child-Pugh class B/C. In the present study, ROC curve
analysis showed that reduction-%LMR was a more useful parameter in
differentiating Child-Pugh A from Child-Pugh B/C than HH15 or LHL15
(Fig. 4). Furthermore, the cutoff
value of less than −50% of reduction-%LMR indicated high
specificity and was suitable for diagnosing Child-Pugh B/C in
patients with cirrhosis (specificity 0.91 and positive predictive
value 0.94) (Table III).
Therefore, SPIO-MRI may be useful to predict early cirrhosis in
patients with chronic viral hepatitis and may be a suitable
technique which supports evaluation of hepatic functional reserve
by Child-Pugh score in the selection of liver transplant patients
from a waiting list.
Several limitations of the present study warrant
mention. First, the study was conducted under a retrospective
design and the sample size was small. Second, some bias may have
arisen from patient selection, since histopathological diagnosis
was performed in 29 of the 46 patients, whereas the remaining 17
were clinically diagnosed by two physicians. Third, the T2-weighted
GRE images in the present study were designed for a 1.0-T MRI
unit.
In conclusion, SPIO-MRI may be a useful non-invasive
method suitable for the evaluation of hepatic functional reserve,
suggesting that KC phagocytic activity is closely correlated with
hepatocyte function in patients with chronic viral hepatitis.
Abbreviations:
|
SPIO,
|
superparamagnetic iron oxide;
|
|
Tc-99m-GSA-scintigraphy,
|
scintigraphy using
technetium-99m-labelled galactosyl human serum albumin;
|
|
GRE,
|
gradient-recalled echo;
|
|
ROIs,
|
regions of interest;
|
|
%LMR,
|
percentages of liver-to-muscle signal
intensity ratio;
|
|
H15,
|
uptake ratio of the heart at 15 min
after Tc-99m-GSA injection;
|
|
H3,
|
uptake ratio of the heart at 3 min
after Tc-99m-GSA injection;
|
|
HH15,
|
index of blood clearance = H15/H3;
|
|
L15,
|
radioactivity of the liver at 15 min
after Tc-99m-GSA injection;
|
|
LHL15,
|
the receptor index = L15/(H15 +
L15);
|
|
ICG15,
|
indocyanine green retention rate at 15
min;
|
|
ROC analysis,
|
receiver operating characteristic
analysis
|
References
|
1.
|
Child CG and Turcotte JG: Surgery and
portal hypertension. Major Probl Clin Surg. 1:1–85. 1964.
|
|
2.
|
Pugh RNH, Murray-Lyon IM, Dawson JL,
Pietroni MC and Williams R: Transection of the oesophagus for
bleeding oesophageal varices. Br J Surg. 60:646–649. 1973.
View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Schneider PD: Preoperative assessment of
liver function. Surg Clin North Am. 84:355–373. 2004. View Article : Google Scholar
|
|
4.
|
Lucey MR, Brown KA, Everson GT, et al:
Minimal criteria for placement of adults on the liver transplant
waiting list. Transplantation. 66:956–962. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Tygstrup N: The galactose elimination
capacity in control subjects and in patients with cirrhosis of the
liver. Acta Med Scand. 175:281–289. 1964. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Hepner GW and Vesell ES: Assessment of
aminopyrine metabolism in man by breath analysis after oral
administration of 14C-aminopyrine. N Engl J Med. 291:134–147.
1975.PubMed/NCBI
|
|
7.
|
Kawamura H, Kamiyama T, Nakagawa T, et al:
Preoperative evaluation of hepatic functional reserve by converted
ICGR15 calculated from Tc-GSA scintigraphy. J Gastroenterol
Hepatol. 8:1235–1241. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Moody FG, Rikkers LF and Aldrete JS:
Estimation of the functional reserve of human liver. Ann Surg.
180:592–598. 1972. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Yamanaka N, Okamoto E, Kuwata K and Tanaka
N: A multiple regression equation for prediction of posthepatectomy
liver failure. Ann Surg. 200:658–663. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Fujioka H, Kawashita Y, Kamohara Y, et al:
Utility of technetium-99m-labeled-galactosyl human serum albumin
scintigraphy for estimating the hepatic functional reserve. J Clin
Gastroenterol. 28:329–333. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Sasaki N, Shiomi S, Iwata Y, et al:
Clinical usefulness of scintigraphy with 99mTc-galactosyl-human
serum albumin for prognosis of cirrhosis of the liver. J Nucl Med.
40:1652–1656. 1999.
|
|
12.
|
Kawamura E, Shiomi S, Ishizu H, et al:
Natural course of change in hepatic functional reserve in patients
with chronic liver disease evaluated by scintigraphy with GSA.
Hepatol Res. 27:129–135. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Shiomi S, Kuroki T, Kuriyama M, et al:
Evaluation of fluminant hepatic failure by scintigraphy with
technetium-99m-GSA. J Nucl Med. 38:79–82. 1997.PubMed/NCBI
|
|
14.
|
Hakawa SK and Tanaka Y: A quantitative
model of technetium-99m-DTPA-galactosyl-HSA for the assessment of
hepatic blood flow and hepatic binding receptor. J Nucl Med.
32:2233–2240. 1991.PubMed/NCBI
|
|
15.
|
Sugai Y, Komatani A, Hosoya T and
Takahashi K: Analysis of the early blood kinetics of 99mTc-GSA and
its verification: new one-compartment model and regression
equation. Nucl Med Commun. 22:773–778. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Sugahara K, Togashi H, Takahashi K, et al:
Separate analysis of asialoglycoprotein receptors in the right and
left hepatic lobes using Tc-GSA SPECT. Hepatology. 38:1401–1409.
2003.PubMed/NCBI
|
|
17.
|
Nanashima A, Yamaguchi H, Shibasaki S, et
al: Relationship between indocyanine green test and technetium-99m
galactosyl serum albumin scintigraphy in patients scheduled for
hepatectomy: clinical evaluation and patient outcome. Hepatol Res.
28:184–190. 2004. View Article : Google Scholar
|
|
18.
|
Tonan T, Fujimoto K, Azuma S, et al:
Evaluation of small (< or =2 cm) dysplastic nodules and
well-differentiated hepatocellular carcinomas with
ferucarbotran-enhanced MRI in a 1.0-T MRI unit: utility of
T2-weighted gradient echo sequences with an intermediate-echo time.
Eur J Radiol. 64:133–139. 2007.
|
|
19.
|
Elizondo G, Weissleder R, Stark DD, et al:
Hepatic cirrhosis and hepatitis: MR imaging enhanced with
superparamagnetic iron oxide. Radiology. 174:797–801. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Clement O, Frija G, Chambon C, et al:
Liver tumors in cirrhosis: experimental study with SPIO-enhanced MR
imaging. Radiology. 180:31–36. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
21.
|
Kato N, Ihara S, Tsujimoto T and Miyazawa
T: Effect of resovist on rats with different severities of liver
cirrhosis. Invest Radiol. 222:661–666. 2002.PubMed/NCBI
|
|
22.
|
Tanimoto A, Yuasa Y, Shinmoto H, et al:
Superparamagnetic iron oxide-mediated hepatic signal intensity
change in patients with and without cirrhosis: pulse sequence
effects and Kupffer cell function. Radiology. 222:661–666. 2002.
View Article : Google Scholar
|
|
23.
|
Hundt W, Petsch R, Heimberger T and Reiser
H: Signal changes in liver and spleen after Endorem administration
in patients with and without liver cirrhosis. Eur Radiol.
10:409–416. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
24.
|
Gandon Y, Olivié D, Guyader D, et al:
Non-invasive assessment of hepatic iron stores by MRI. Lancet.
31:357–362. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
25.
|
Kudo M, Todo A, Ikekubo K, et al:
Functional hepatic imaging with receptor-binding
radiopharmaceutical: clinical potential as a measure of functioning
hepatocyte mass. Gastroenterol Jpn. 26:734–741. 1991.
|
|
26.
|
Bland JM and Altman DG: Statistical
methods for assessing agreement between two methods of clinical
measurement. Lancet. 1:307–310. 1986. View Article : Google Scholar
|
|
27.
|
Waxman AD: Scintigraphic evaluation of
diffuse hepatic disease. Semin Nucl Med. 12:75–88. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
28.
|
Klingensmith WC III, Fritzberg AR, Zerbe
GO and Koep LJ: Relative role of Tc-99m-diethyl-IDA and
Tc-99m-sulfur colloid in the evaluation of liver function. Clin
Nucl Med. 5:341–346. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
29.
|
Asanuma T, Ono M, Kubota K, et al: Super
paramagnetic iron oxide MRI shows defective Kupffer cell uptake
function in non-alcoholic fatty liver disease. Gut. 59:258–266.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
30.
|
Tsujimoto T, Kawaratani H, Kitazawa T, et
al: Decreased phagocytic activity of Kupffer cells in a rat
nonalcoholic steatohepatitis model. World J Gastroenterol.
14:6036–6043. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
31.
|
Kira T, Tomiguchi S, Kira M, Ohyama Y and
Takahashi M: Quantitative evaluation of the hepatic functional
reserve using technetium-99m DTPA-galactosyl human serum albumin
before and after transjugular intrahepatic portosystemic shunt. Eur
J Nucl Med. 24:1268–1272. 1997. View Article : Google Scholar
|
|
32.
|
Osada H, Honda N, Takahashi T, et al:
Relationship between (99m)Tc-GSA scintigraphic indices of liver
function reserve and portal circulation in patients with chronic
liver disease. Ann Nucl Med. 21:245–249. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
33.
|
Aguirre DA, Behling CA, Alpert E,
Hassanein TI and Sirlin CB: Liver fibrosis: noninvasive diagnosis
with double contrast material-enhanced MR imaging. Radiology.
239:425–437. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
34.
|
Lucidarme O, Baleston F, Cadi M, et al:
Non-invasive detection of liver fibrosis: Is superparamagnetic iron
oxide particle-enhanced MR imaging a contributive technique? Eur
Radiol. 13:467–474. 2003.PubMed/NCBI
|
|
35.
|
Engström-Laurent A, Laurent UB, Lilja K
and Laurent TC: Concentration of sodium hyaluronate in serum. Scand
J Clin Lab Invest. 45:497–504. 1985.
|
|
36.
|
Tsukamoto T, Yamamoto T, Ikebe T, et al:
Serum markers of liver fibrosis and histologic severity of fibrosis
in resected liver. Hepatogastroenterology. 51:777–780.
2004.PubMed/NCBI
|