Introduction
Delayed post-traumatic vertebral collapse,
characterized by painful kyphosis that develops several weeks or
months following an injury after a symptom-free period, was first
publicly presented by the German surgeon Hermann Kümmell in 1895
(1). The development of the
disease has three phases. In the first phase, patients initially
experience back pain, which subsides and leads to an asymptomatic
period. In the second phase, the pain recurs weeks to months after
the initial incident without further apparent trauma. In the third
phase, patients develop progressive angular kyphosis. With the
advent of radiography, the progressive angular kyphosis was
attributed to a delayed post-traumatic vertebral compression
fracture. The outstanding radiological findings of Kümmell’s
disease consist of an intravertebral cleft (either intravertebral
vacuum cleft or fluid collection) combined with a collapsed
vertebra. More recently, multiple synonymous terms have been used
to describe Kümmell’s disease, including delayed post-traumatic
vertebral collapse (2,3), vertebral osteonecrosis (4,5),
intravertebral pseudarthrosis (4,6),
fracture non-union (6) and
intravertebral cleft (7). However,
whether intravertebral clefts are a pathognomonic sign of Kümmell’s
disease is controversial. Certain studies have demonstrated that
intravertebral clefts are a benign sign, whereas others have
reported that intravertebral clefts occur rarely in patients with
spinal infection and in patients with multiple myeloma (8,9).
For Kümmell’s disease with persistent pain and
without neurological symptoms, percutaneous vertebroplasty (PVP)
(4,10) or kyphoplasty (PKP) (5,6,11)
achieves good results. For patients with neurological deficits, PVP
and PKP are unsuitable. In the past, anterior decompression with
bone grafting fusion (12),
posterior decompression with pedicle subtraction osteotomy (PSO)
(2,3,13,14)
or a combined anterior and posterior approach operation (14) were used, but these procedures have
long surgery times and cause increased hemorrhage and multiple
complications. In the current study, posterior decompression and
vertebroplasty were used to treat the affected vertebrae. Pedicle
screw fixation and posterolateral bone grafts were performed at one
level above and one level below the affected vertebrae for
Kümmell’s disease with neurological deficits and improved results
were achieved. Through a review of the literature (15–18)
combined with our own study, we intend to further investigate
whether intravertebral clefts are a pathognomonic sign of Kümmell’s
disease and to determine a suitable treatment method for Kümmell’s
disease with neurological deficits.
Materials and methods
Patients
The cohort consisted of 16 patients, 7 males and 9
females, 69–82 years old (average, 74 years), admitted to Henan
Province People’s Hospital between October 2007 and August 2010.
Ten of the patients had a history of minor trauma. The duration of
their symptoms ranged from 2 to 8 months. Two patients were
undergoing long-term hormone replacement therapy. Eight patients
had hypertension and four cases had diabetes mellitus. The mean
bone mineral density was −3.65 standard deviation (SD). The treated
vertebrae were as follows: T7 (n=1), T9 (n=1), T10 (n=2), T11
(n=3), T12 (n=6), L1 (n=2) and L3 (n=1). Preoperative imaging
included standing anteroposterior and lateral radiographs, CT scans
and MRI examination. Five patients underwent stress views (standing
extension and flexion lateral radiographs) in addition to the
standard radiographs. Postoperative standing radiographs were taken
to assess the effect of the surgery. This study was conducted in
accordance with the Declaration of Helsinki and with approval from
the Ethics Committee of the Henan Province People’s Hospital.
Written informed consent was obtained from all participants.
Surgical procedure
The patients were operated on under general
anesthesia and placed in the prone position. Pillows were used to
support the upper chest and pelvis and the operating table was
adjusted to enable maximum extension of the spinal column. This
postural reduction generally restored most of the body height of
the fractured vertebrae. Using a standard posterior midline
approach, pedicle screws were placed promptly into the vertebrae
one level above and below the affected vertebra through a
distraction rod to restore the vertebral body height further. The
diseased vertebral laminae and ligamentum flavum were resected to
decompress the spinal cord. A puncture needle was driven into the
affected vertebral body to establish a working channel. A biopsy
needle was used to collect a specimen. Under fluoroscopic guidance,
bone cement was injected into the vertebral body. Intraoperative
exploration revealed no compression of the dural sac and no leakage
of bone cement in the spinal canal. Posterolateral fusion with
autogenous bone grafts from the decompression laminectomy was
performed.
Evaluation
Vertebral height was measured in millimeters along
the vertebral borders at the anterior and middle of the vertebral
body. The Cobb angle was measured as the angle between the upper
endplate of the upper vertebra of the fractured vertebra and the
lower endplate of the lower vertebra of the fractured vertebra. The
visual analog scale (VAS), which ranges from 0 (no pain) to 10
(maximal pain), was used to assess pain severity. Frankel
classification was used to assess neurological status and the
development of surgical complications was observed.
Statistical analysis
SPSS 17.0 statistical software (SPSS, Inc., Chicago,
IL, USA) was used for analysis. The data are presented as the mean
± standard deviation. One-way ANOVA was used to evaluate the
changes in the VAS, Cobb angles and vertebral body heights based on
the data obtained preoperatively, one day postoperatively and at
final follow-up. A multiple comparison was conducted using the
least significant difference test. P<0.05 was considered to
indicate a statistically significant difference.
Results
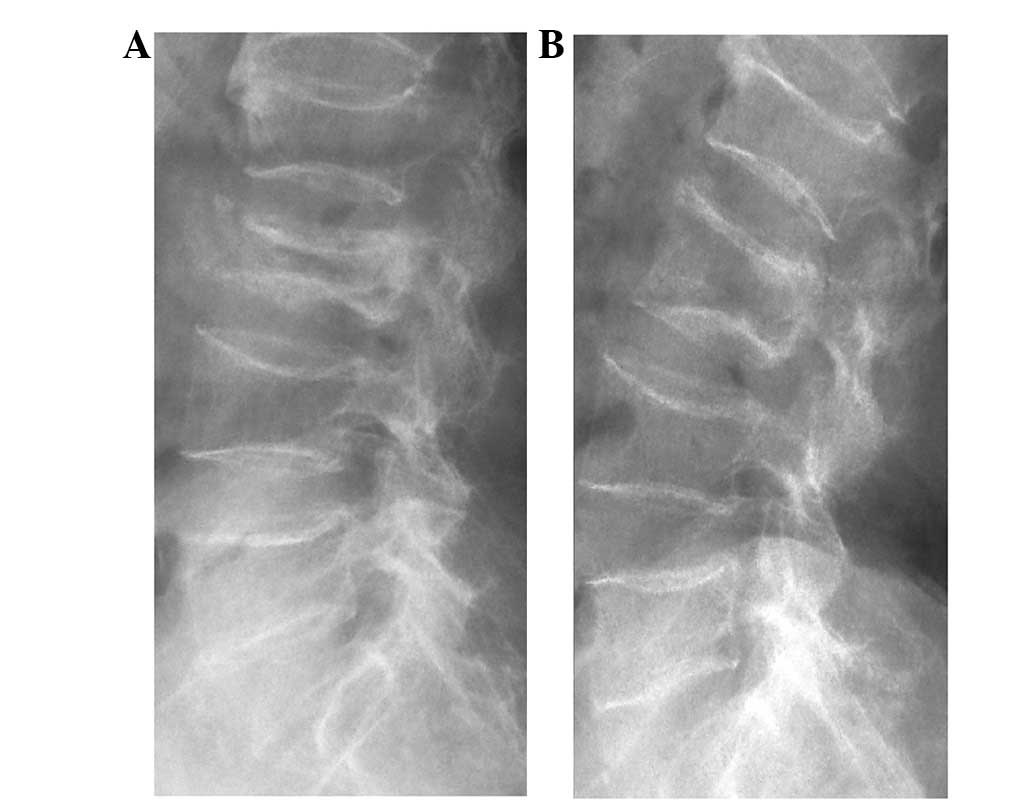
Preoperative standing lateral radiographs and
intraoperative prone position lateral radiographs, as well as
preoperative extension and flexion radiographs of five patients,
were compared and it was identified that vertebral height varied
with postural changes. Stress view radiographs showed that
vertebral height decreased with flexion and increased with
extension (Fig. 1).
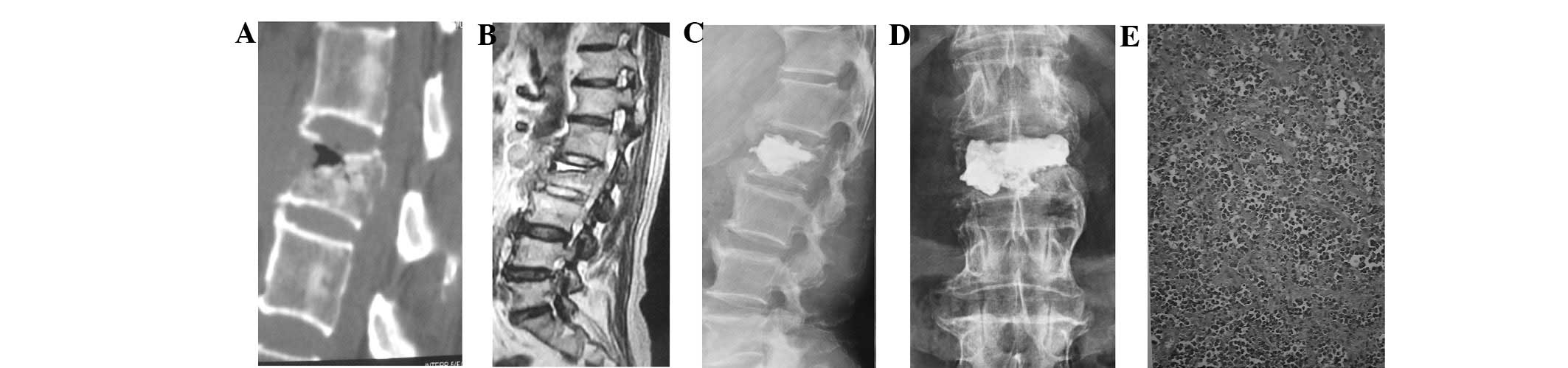
All 16 patients presented with intravertebral cleft
signs during the preoperative examination. The following
radiological patterns were identified as signs of an intravertebral
cleft: i) a gas-filled transverse band in the vertebral body on a
conventional radiograph (5 cases); ii) a gas-filled transverse band
in the vertebral body on a CT image (9 cases, 3 of which exhibited
adjacent intradiscal gas at the same time) and iii) a gas or fluid
signal on an MRI scan (preoperative MRI scans of all 16 patients).
In one case, a lumbar MRI T2-weighted image revealed mixed signals
of gas and liquid at T12. After 8 min, the thoracic MRI T2-weighted
image displayed an apparent inconsistency and a hyperintense fluid
signal at T12 (Fig. 2).
The mean surgery time was 110 min (range, 90–140
min), and the mean estimated blood loss was 250 ml (range, 150–500
ml). The mean volume of polymethylmethacrylate (PMMA) was 7.2 ml
(range, 4.5–12 ml). A spinal dural tear occurred in one case.
Intraoperative biopsies from all 16 cases reported bone necrosis
(Fig. 3). Clinically, one patient
was identified who had no neurological deficits (and so was
excluded from the group), whose CT displayed the vacuum phenomenon
(Fig. 4A) and whose MRI scan
displayed a liquid signal (Fig.
4B); the pathology report revealed non-Hodgkin’s lymphoma
(Fig. 4E).
The patients underwent follow-up after 18–42 months
(mean, 22 months). The mean VAS score, the anterior and middle
height of the affected vertebrae and the Cobb angle improved
significantly from prior to the surgery to one day postoperatively
(P<0.01). The improvement was maintained from one day
postoperatively to the final follow-up (P>0.05; Table I). No patient received a grade A
under the Frankel classification. Preoperatively, two patients were
classified as grade B, five were grade C and nine were grade D. One
day postoperatively, one patient was grade B, three were grade C,
seven were grade D and five were grade E. At final follow-up, two
patients were grade C, five were grade D and nine were grade E. The
neurological function of each patient was improved by at least one
level at the final follow-up (Table
II). One patient developed a superficial skin infection. No
obvious loosening of internal fixation, breakage or bone cement
displacement occurred.
 | Table I.Evaluation indices prior to and
following surgery. |
Table I.
Evaluation indices prior to and
following surgery.
| Cobb angle height
(cm) | Anterior vertebral
height (cm) | Middle vertebral
height (cm) | VAS score |
|---|
| Preoperative | 29.63±3.97 | 1.05±0.23 | 1.51±0.26 | 8.49±0.43 |
| One day
postoperatively | 11.34±2.25a | 2.40±0.27a | 2.47±0.29a | 2.09±0.36a |
| Final follow-up | 12.45±2.35a,b | 2.28±0.25a,b | 2.42±0.34a,b | 2.29±0.31a,b |
| F-value | 191.70 | 141.735 | 55.668 | 1601.407 |
| P-value | 0.000 | 0.000 | 0.000 | 0.000 |
 | Table II.Patient numbers prior to and following
surgery by Frankel classification. |
Table II.
Patient numbers prior to and following
surgery by Frankel classification.
| Frankel
classification (patient number)
|
|---|
| Time point | A | B | C | D | E |
|---|
| Preoperative | 0 | 2 | 5 | 9 | 0 |
| One day
postoperatively | 0 | 1 | 3 | 7 | 5 |
| Final follow-up | 0 | 0 | 2 | 5 | 9 |
Discussion
Maldague et al(19) first reported the intravertebral
vacuum cleft sign, and the authors considered gas accumulation
(vacuum cleft sign) in the vertebral body on plain X-rays as
pathognomonic of Kümmell’s disease. The vacuum phenomenon is more
evident in the extended position and may reduce or disappear in the
flexed position. The gas noted on the plain radiographs was
expected to be hypointense on both the MRI T1 and T2 sequences.
However, the majority of authors have reported either a homogeneous
fluid or gas signal on the MRI sequences of patients with the
intravertebral vacuum phenomenon. Malghem et al(8) plausibly explained this phenomenon.
Patients with the vacuum sign were serially imaged, and the MRI
demonstrated that the initially gas-filled cleft appeared
hypointense. However, following prolonged supine positioning, a
hyperintense signal appeared on the T2 sequences, indicating the
presence of fluid instead of gas. We also observed this phenomenon
in one patient. The lumbar MRI T2-weighted image showed a mixed
signal of gas and liquid at T12. After 8 min, the thoracic MRI
T2-weighted image showed a hyperintense liquid signal at T12, which
suggests that the contents (fluid and gas within the vertebral
body) are variable over time.
Whether intravertebral clefts are a pathognomonic
sign of Kümmell’s disease is controversial. Certain studies have
demonstrated that intravertebral clefts are a benign sign, whereas
others have reported that intravertebral clefts occur rarely in
patients with spinal infections and in patients with multiple
myeloma (8,9). We identified a patient (excluded from
the study) with a CT that displayed a vacuum phenomenon (Fig. 4A) and an MRI that displayed a
liquid sign (Fig. 4B). The patient
was diagnosed with Kümmell’s disease based on the clinical and
radiological signs. The vacuum cleft was filled well with PMMA
(Fig. 4C and D). However, the
pathology report revealed non-Hodgkin’s lymphoma (Fig. 4E). To the best of our knowledge, no
non-Hodgkin’s lymphoma with vacuum cleft has been reported.
Therefore, intravertebral clefts are not pathognomonic of Kümmell’s
disease, but they are highly suggestive of the disease. Thus, we
consider that it is necessary to confirm Kümmell’s disease with
bone necrosis under biopsy.
The pathogenesis of the vertebral vacuum phenomenon
remains controversial and it has been mainly theorized to involve
vertebral avascular necrosis (4,19),
vertebral fracture nonunion or pseudarthrosis (6) or intradiscal gas leakage through the
endplate fractured into the vertebral body (20). In the current study, only two
patients had factors that predispose to bone necrosis (long-term
corticosteroid application history). The remaining patients had no
other predisposing factors. The theory of vertebral avascular
necrosis alone does not explain the pathogenesis of the disease. In
the current study, nine patients exhibited a gas signal in the
affected vertebral body based on CT but only three cases had gas in
the adjacent disk. Therefore, the theory that intravertebral gas
originates from the adjacent disk alone does not explain the
intravertebral vacuum phenomenon. In addition, we compared the
preoperative standing lateral radiographs and intraoperative prone
lateral radiographs, as well as the preoperative extension and
flexion radiographs, of five patients. We found that vertebral
height varied with postural changes, in accordance with the report
by Yang et al(6). These
findings support the theory of vertebral fracture nonunion or
pseudarthrosis. Thus, we advocate the complete filling of the cleft
with cement to maximize stabilization of the pseudarthrosis. In the
current study, the mean amount of cement injected was 7.2 ml.
According to the literature, as well as our imaging results and
clinical data, the pathogenesis of the vertebral cleft phenomenon
requires a combination of avascular bone necrosis, fracture
non-healing and adjacent intradiscal gas diffusion.
The treatment strategies for Kümmell’s disease
differ between patients with neurological symptoms and those
without neurological symptoms. For patients without neurological
symptoms, the objective is to eliminate motion at the fracture site
and restore the spinal curvature. Certain authors have reported
that PVP (4,8) or PKP (5,6,9)
achieves good clinical results for Kümmell’s disease without
neurological symptoms. For neurologically impaired patients, the
aim of surgery is to decompress the spinal cord, restore the spinal
physiological curvature and maintain spinal stability. The surgical
modes include anterior, posterior or combined anterior and
posterior approaches. Anterior decompression and fusion with
intervertebral tricortical graft or ceramic glass spacers has
favorable results. These procedures are the most efficient for
decompressing the spinal cord since the locus of pathology
(deficient anterior and middle spinal columns) is directly
addressed, and they provide anterior column support. Anterior
approach surgery has a high fusion rate (95.5–100%) and the
postoperative kyphosis correction angle has a mean of 10.4–18°. At
final follow-up, the corrected degree decreased by 4.8–8°. The
drawback of the anterior approach in pleural and extrapleural
operations is that it may cause pulmonary complications in injuries
of the thoracolumbar junction, where most cases of intravertebral
vacuum occur, and it may affect gastrointestinal function in
retroperitoneal surgery. Moreover, in the anterior approach, the
stabilization of the spine may fail due to the osteoporotic bone.
Surgeries that use the posterior approach include decompression and
PSO (2,3,13,14).
The fusion rate of the posterior approach operation is 62.5–100%,
and the immediate postoperative kyphosis correction angle is
14.6–25.7°. The average loss of correction at final follow-up is
2.4–8.8°. PSO surgery often requires the fixation of the vertebral
bodies above and below the affected vertebra; thus, adjacent
vertebral disease often occurs. A combined anterior and posterior
approach has a good fusion rate (100%), with a kyphosis angle
correction of 11.2° postoperatively and a loss of 4.2° at final
follow-up. However, the surgery time is longer (351 min) and the
blood loss is higher (2892 ml) (14).
Patients with Kümmell’s disease with neurological
symptoms are often older and have a variety of diseases; thus, the
patients do not easily tolerate the aforementioned surgical
methods. Therefore, the development of a minimally invasive and
effective treatment is required. Surgeons have performed open
posterior decompression and short-segment fixation for Kümmell’s
disease with neurological symptoms, followed by vertebroplasty
(15–18) or kyphoplasty (17) under direct visualization. This
surgical method provides several advantages. Posterior
decompression relieves nerve compression with short segment
fixation and fusion reduces the fusion segment and the influence of
long segmental spinal function. Vertebral bone cement provides
anterior support to minimize posterior pedicle screw stress.
Furthermore, bone cement leakage may be avoided under direct
vision. Matsuyama et al(18) used calcium phosphate cement, which
polymerizes at lower temperatures. The results included effective
pain relief (from 8.6, preoperatively, to 2, postoperatively, on
the VAS), nerve function and kyphosis restoration (vertebral height
from 41% preoperatively to 74% postoperatively and 68% at final
follow-up). In the current study, we used PMMA for vertebroplasty
which achieved effective pain relief (the mean preoperative VAS
score of 8.49 was reduced to 2.09 one day postoperatively and 2.29
at final follow-up) and good postoperative kyphosis correction (the
anterior and central vertebral body height were enhanced by ∼1 cm
and Cobb’s angle correction was 18.29° one day postoperatively).
Follow-up examinations were conducted for ≥18 months. At the final
follow-up, a slight reduction in the vertebral height and a
kyphosis correction of 1.11° were observed compared with those at
one day after the surgery. However, these differences were not
statistically significant. The patients recovered neurologically,
and nerve function improved by least one Frankel grade at final
follow-up. The mean surgery time was 110 min (range, 90–140 min)
and the mean estimated blood loss was 250 ml (range, 150–500 ml).
Thus, posterior decompression with short-segment fixation and
fusion combined with vertebroplasty is an effective treatment for
Kümmell’s disease with neurological symptoms, especially for
patients who are not able to tolerate long surgery times and
massive blood loss. However, a previous study hypothesized that the
osteolysis rate among patients with Kümmell’s disease is greater
than the rate of bone callus formation. Following PVP or PKP,
accelerated osteolysis occurs and may displace the bone cement
(21). Two case reports have
focused on bone cement displacement following PVP (22) or PKP (23) alone for Kümmell’s disease without
neurological deficits. Therefore, greater numbers of patients and
longer follow-up times are required to verify the efficiency of
posterior decompression with short segmental pedicle screw fixation
and fusion combined with vertebroplasty for Kümmell’s disease with
neurological deficits.
References
|
1.
|
Kümmell H: Die rarefizierende Ostitis der
Wirbelkrper. Deutsche Med. 21:180–181. 1985.(in German).
|
|
2.
|
Kim KT, Suk KS, Kim JM and Lee SH: Delayed
vertebral collapse with neurological deficits secondary to
osteoporosis. Int Orthop. 27:65–69. 2003.PubMed/NCBI
|
|
3.
|
Saita K, Hoshino Y, Kikkawa I and Nakamura
H: Posterior spinal shortening for paraplegia after vertebral
collapse caused by osteoporosis. Spine (Phila Pa 1976).
25:2832–2835. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Jang JS, Kim DY and Lee SH: Efficacy of
percutaneous vertebroplasty in the treatment of intravertebral
pseudarthrosis associated with noninfected avascular necrosis of
the vertebral body. Spine (Phila Pa 1976). 28:1588–1592. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Wang GL, Yang HL, Jiang WM, et al: Balloon
kyphoplasty for osteoporotic vertebral compression fractures with
osteonecrosis. Zhonghua Wai Ke Za Zhi. 48:593–596. 2010.(In
Chinese).
|
|
6.
|
Yang HL, Wang GL, Niu GQ, et al: Diagnosis
and treatment of nonunion of osteoporotic thoracolumbar vertebral
fractures. Chin J Orthop. 27:682–686. 2007.(In Chinese).
|
|
7.
|
Pappou IP, Papadopoulos EC, Swanson AN,
Cammisa FP Jr and Girardi FP: Osteoporotic vertebral fractures and
collapse with intravertebral vacuum sign (Kümmel’s disease).
Orthopedics. 31:61–66. 2008.PubMed/NCBI
|
|
8.
|
Malghem J, Maldague B, Labaisse MA, et al:
Intravertebral vacuum cleft: changes in content after supine
positioning. Radiology. 187:483–487. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Feng SW, Chang MC, Wu HT, Yu JK, Wang ST
and Liu CL: Are intravertebral vacuum phenomena benign lesions? Eur
Spine J. 20:1341–1348. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Liang D, Jiang XB, Yao ZS, et al: The
recent effects of PVP in treatment of Kümmell’s disease on
extension position. Zhongguo Ji Zhu Ji Sui Za Zhi. 20:260–261.
2010.(In Chinese).
|
|
11.
|
Zhang XK, Liang Y, Wu WJ, et al: Kümmell’s
disease: Reports of 7 cases and review of the literature. Anatomy
and Clinics. 16:127–130. 2011.(in Chinese).
|
|
12.
|
Kanayama M, Ishida T, Hashimoto T, et al:
Role of major surgery using Kanada anterior instrumentation for
osteoporotic vertebral collapse. J Spinal Disord Tech. 23:53–56.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Mochida J, Toh E, Chiba M and Nishimura K:
Treatment of osteoporotic late collapse of a vertebral body of
thoracic and lumbar spine. J Spinal Disord. 14:393–398. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Suk SI, Kim JH, Lee SM, Chung ER and Lee
JH: Anterior-posterior surgery versus posterior closing wedge
osteotomy in post-traumatic kyphosis with neurologic compromised
osteoporotic fracture. Spine (Phila Pa 1976). 28:2170–2175. 2003.
View Article : Google Scholar
|
|
15.
|
Uchida K, Nakajima H, Yayama T, et al:
Vertebroplasty-augmented short-segment posterior fixation of
osteoporotic vertebral collapse with neurological deficit in the
thoracolumbar spine: comparisons with posterior surgery without
vertebroplasty and anterior surgery. J Neurosurg Spine. 13:612–621.
2010. View Article : Google Scholar
|
|
16.
|
Sudo H, Ito M, Abumi K, et al: One-stage
posterior instrumentation surgery for the treatment of osteoporotic
vertebral collapse with neurological deficits. Eur Spine J.
19:907–915. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Fuentes S, Blondel B, Metellus P,
Adetchessi T, Gaudart J and Dufour H: Open kyphoplasty for
management of severe osteoporotic spinal fractures. Neurosurgery.
64(5 Suppl 2): 350–354. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Matsuyama Y, Goto M, Yoshihara H, et al:
Vertebral reconstruction with biodegradable calcium phosphate
cement in the treatment of osteoporotic vertebral compression
fracture using instrumentation. J Spinal Discord Tech. 17:291–296.
2004. View Article : Google Scholar
|
|
19.
|
Maldague BE, Noel HM and Malghem JJ: The
intravertebral vacuum cleft: a sign of ischemic vertebral collapse.
Radiology. 129:23–29. 1978. View
Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Lafforgue P, Chagnaud C, Daumen-Legré V,
Daver L, Kasbarian M and Acquaviva PC: The intravertebral vacuum
phenomenon (‘vertebral osteonecrosis’). Migration of intradiscal
gas in a fractured vertebral body? Spine (Phila Pa 1976).
22:1885–1891. 1997.
|
|
21.
|
Laredo JD: Expert’s comment concerning
Grand Rounds case entitled ‘Kümmell’s disease: delayed
post-traumatic osteonecrosis of the vertebral body’ (by R. Ma, R.
Chow, F. H. Shen). Eur Spine J. 19:1071–1072. 2010.
|
|
22.
|
Wagner AL and Baskurt E: Refracture with
cement extrusion following percutaneous vertebroplasty of a large
interbody cleft. AJNR Am J Neuroradiol. 27:230–231. 2006.PubMed/NCBI
|
|
23.
|
Wang HS, Kim HS, Ju CI and Kim SW: Delayed
bone cement displacement following balloon kyphoplasty. J Korean
Neurosurg Soc. 43:212–214. 2008. View Article : Google Scholar : PubMed/NCBI
|