Introduction
Coronary heart disease (CHD) is one of the most
common diseases and has a serious impact on human health and safety
(1). It has become one of the top
causes of mortality in China. The prevalence of CHD is increasing
and sudden mortality is often due to this sudden disease. Detecting
CHD as early as possible before clinical symptoms appear is
important. Selective X-ray coronary angiography (SCA) is one of the
standard tests for CHD; however,it has several disadvantages,
including high-cost, invasive diagnosis and the performance of the
procedure necessitates considerable time and skill of highly
trained physicians. In the past few years, non-invasive diagnosis
of CHD has made great progress. With the improvement of
computerized tomography (CT) hardware and software technology,
64-multislice spiral CT (64-MSCT) CT angiography (CTA) has become a
common, non-invasive diagnostic method. In this study, we assessed
the clinical application of 64-MSCT CTA compared with SCA, based on
previous randomized studies (2,3).
Patients and methods
Patient characteristics
A total of 95 patients with suspected obstructive
coronary artery disease received 64-MSCT. Of these, 67 patients
were identified to have coronary stenosis. There were 43 males and
24 females, aged 41–81 years (average age, 65 years) with regular
sinus rhythm. For patients with a fast heart rate, the rhythm could
be controlled below 70 bpm, without Betaloc allergy effects. The
study was conducted in accordance with the Helsinki Declaration II
and was approved by the Institutional Review Board of Harbin
Medical University. All patients provided written informed consent
which was signed by the patient or their families.
Methods
The heart cover area was set at 120 mm with a fast
rotation speed of 0.35 sec per rotation. The mean pitch of the
heart scan was 0.23. The detector width was 64×0.625 mm and the
time of the heart scan was 4.57 sec. The blood circulation time was
evaluated by a test bolus. The injection rate of the contrast media
was 5 ml/sec. The range of the scan covered the whole heart. The
patient was instructed to maintain an inspiratory breath hold. The
whole process was performed by an interventional cardiologist.
Results
All 95 patients received 64-MSCT. All the main blood
vessels and major branches were smooth and there was no stenosis in
18 patients. Coronary myocardial bridge (CMB) was detected in 10
patients. Among the 67 patients with coronary stenosis, we detected
mild coronary stenosis (<50%) in 19 patients, moderate coronary
stenosis (50–70%) in 26 patients and severe coronary stenosis
(>75%) in 22 patients. Of the 18 patients without coronary
stenosis 11 presented symptoms, including chest distress and chest
pain. The SCA results revealed no coronary stenosis. In addition, 4
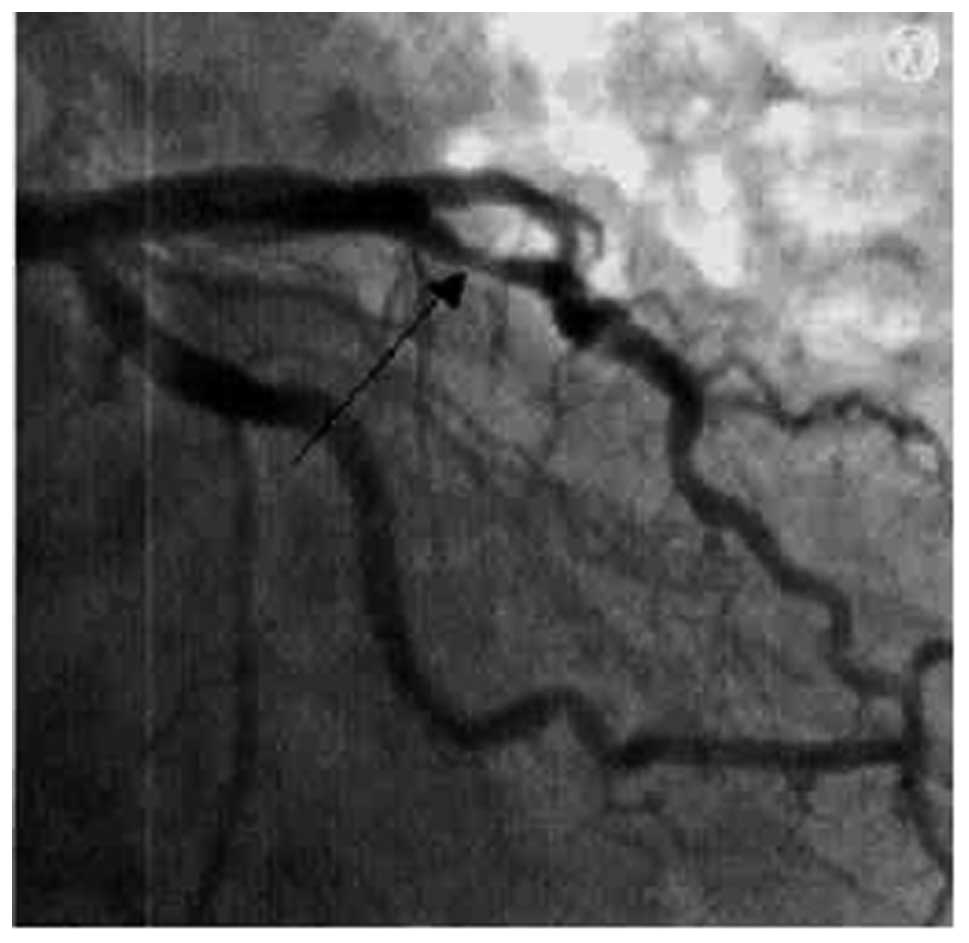
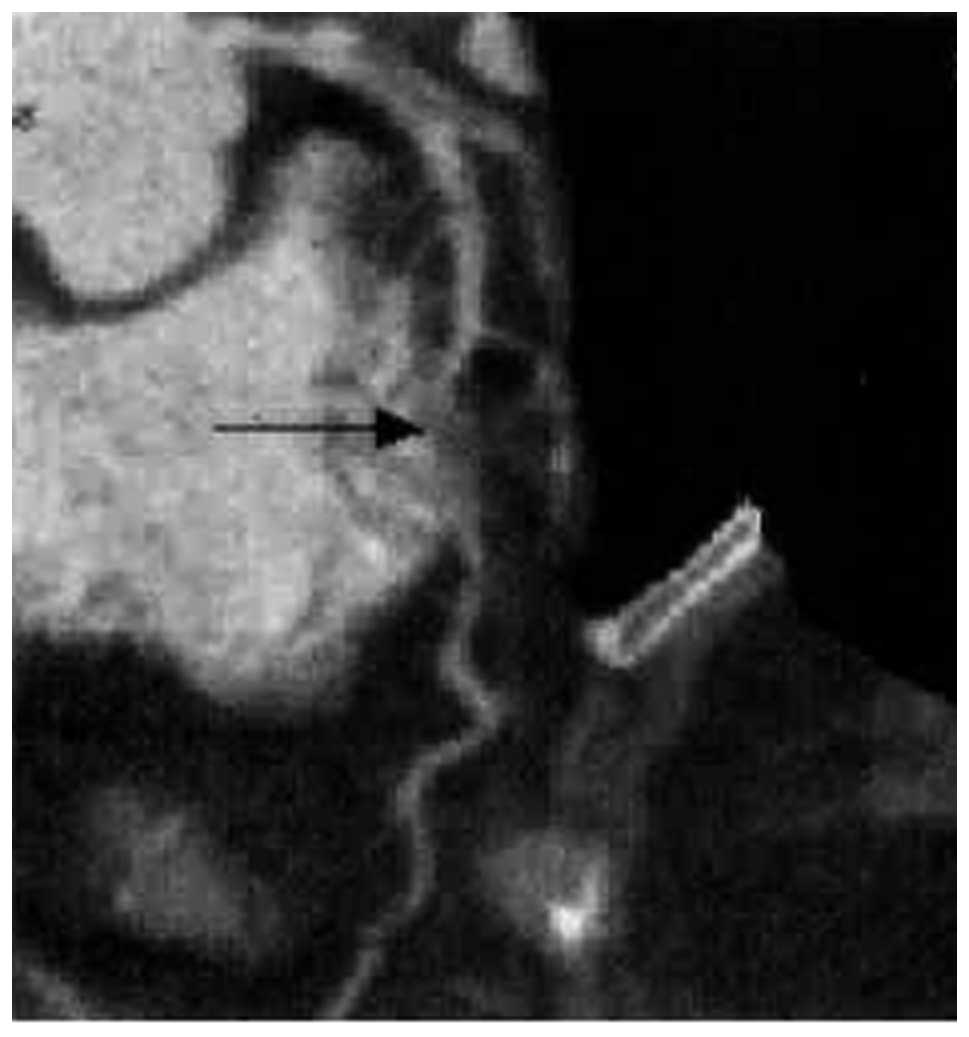
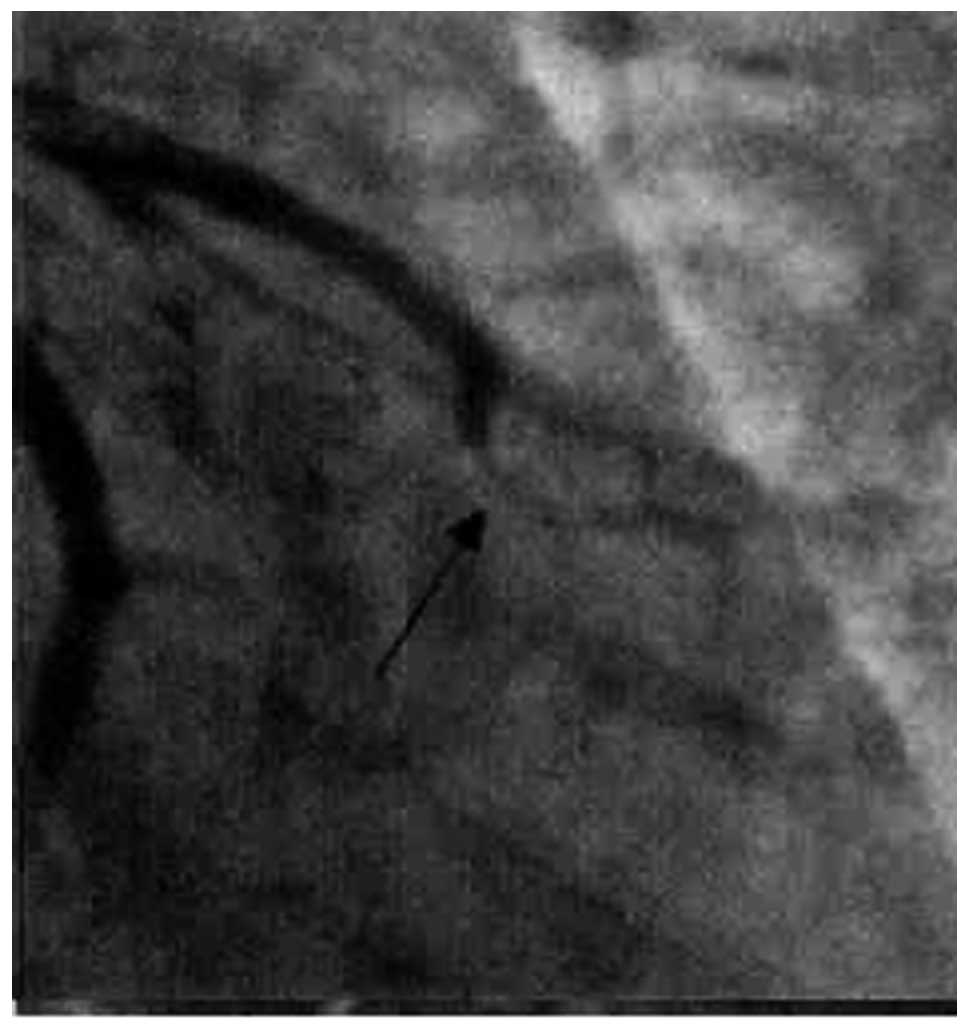
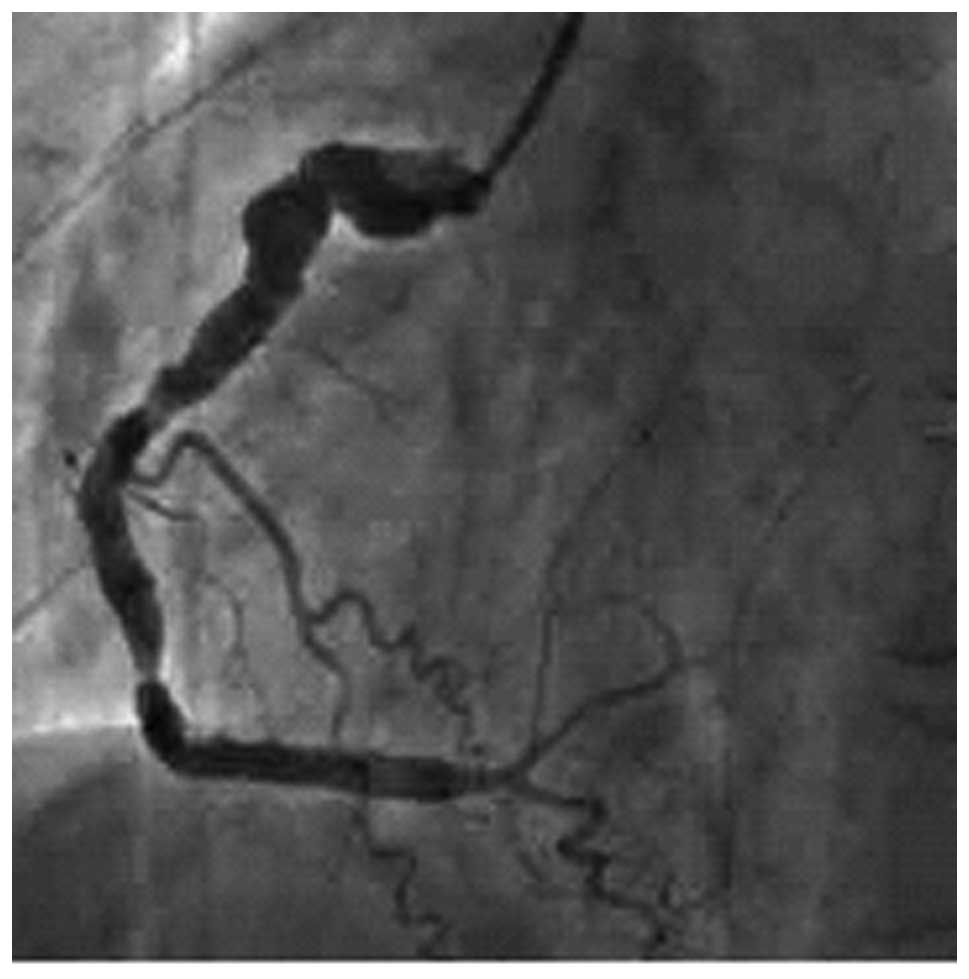
of the 5 CMB patients were diagnosed with SCA (Figs. 1 and 2) and 1 patient was diagnosed with severe
coronary stenosis (Figs. 3 and
4).
Among the patients with coronary stenosis, the SCA
results of 5 patients with mild coronary stenosis revealed that the
level of coronary stenosis was ∼30, 60, 30, 30 and 30%,
respectively. In 9 of the 26 patients with moderate coronary
stenosis the SCA results were consistent with the 64-MSCT results.
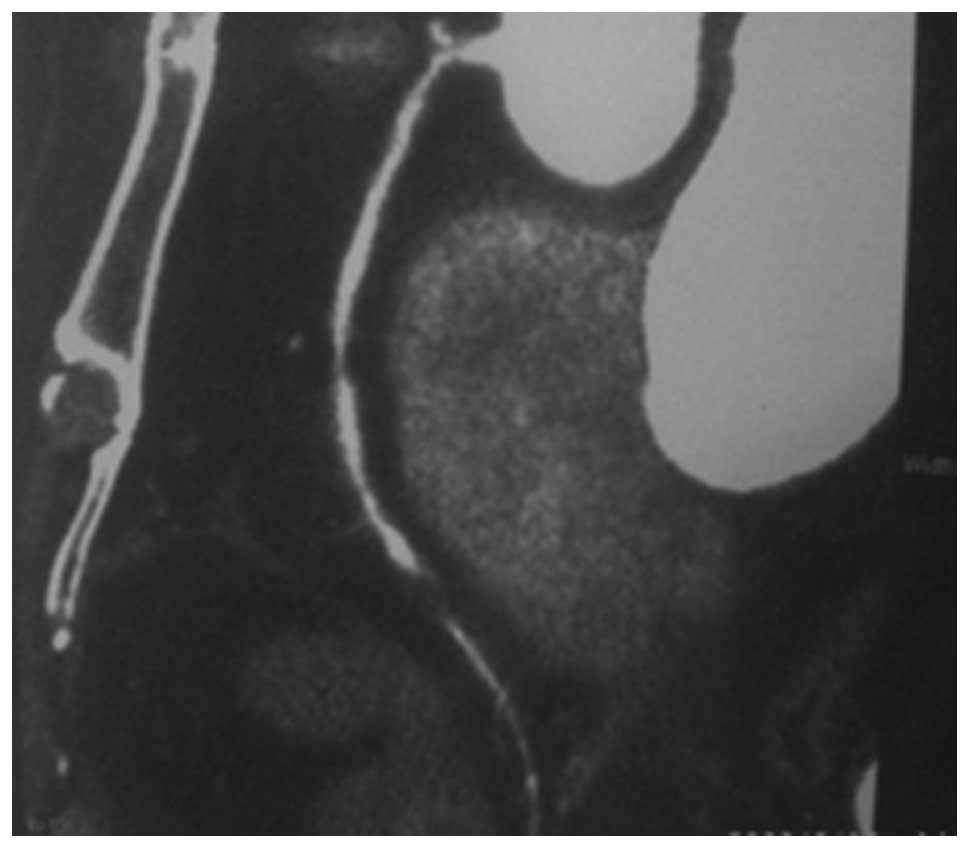
However, 17 patients had severe coronary stenosis and percutaneous
transluminal coronary intervention treatment confirmed the main and
major branch of the diseased blood vessel for these patients with
severe coronary stenosis (Figs. 5
and 6).
Discussion
CHD is one of the main factors threatening human
health and it is also one of the main causes of mortality in China.
Diagnosing coronary stenosis as early as possible and initiating
treatment helps to prevent disease progression. The most common
clinical methods for coronary stenosis are 64-MSCT CTA and SCA, and
SCA is more accurate at this stage. SCA is not only used for
diagnosis, but also for intervention therapy. However, the conduit
method has certain risks due to the invasive property, particularly
for patients who are not suitable for intervention therapy.
Additionally, SCA often increases the financial burden and certain
risks. Therefore, the reliable noninvasive 64-MSCT CTA has
attracted attention. In the past few years, the 64-MSCT hardware
has improved, the scanning time has reduced dramatically and the
time and spatial resolution have increased rapidly. In addition,
the breath artifact is avoided when the heart rate is <70 bpm
and the heart motion artifact is avoided. It also provides an
improved image quality, which clearly shows the coronary artery.
Therefore, 64-MSCT CTA is a common and popular technique (4).
In 64 patients with CHD, 64-MSCT CTA was performed
and the results on coronary stenosis reveal no difference when
compared with SCA diagnosis. Therefore, 64-MSCT CTA may be used
clinically to identify a true negative value when the symptoms of
CHD do not agree with the electrocardiogram (ECG) diagnosis
(5). A CMB is a band of heart
muscle that lies on top of a coronary artery, instead of underneath
it. With a CMB, part of a coronary artery dips into and underneath
the heart muscle and then comes back out again (6). The band of muscle that lies on top of
the coronary artery is called a bridge. With research on anatomy,
pathology and blood hemodynamics, it was identified that a CMB may
cause myocardium ischemia under certain conditions. The diagnosis
and therapy of CMB is becoming increasingly important. SCA is a
classic method for diagnosis, which shows a milking-like effect,
where the CMB is squeezed by contraction of surrounding muscle and
the constriction disappears during diastole. The 64-MSCT CTA method
displays the coronary artery and surrounding myocardial area;
therefore, it has a better diagnostic result than SCA on CMB.
Furthermore, 64-MSCT CTA avoids a false positive diagnosis. CMB is
often misdiagnosed as lumen stenosis and stent implantation is
applied; however, this may cause the lumen to break. Therefore,
64-MSCT CTA has become a better option for diagnosing CMB (7,8).
In this controlled study, we compared 64-MSCT CTA
and SCA diagnostic results and identified that SCA is capable of
diagnosing a mild or moderate coronary stenosis and 64-MSCT CTA
detects a mild coronary stenosis. We suggest that when 64-MSCT CTA
detects a mild coronary stenosis with typical symptoms and the ECG
shows no clear evolvement, a conservative therapy should be
performed and the patient’s condition strictly monitored during the
therapy. Then, SCA should only be performed when necessary.
In this study, when comparing moderate coronary
stenosis detected by 64-MSCT CTA with SCA diagnosis for the same
patients, SCA revealed that more than half of the patients had
severe coronary stenosis and required coronary stent therapy.
Therefore, we suggest that SCA is performed when a moderate
coronary stenosis is detected by 64-MSCT CTA, to prevent delay in
treatment and possible heart infarction. For severe coronary
stenosis, detected by 64-MSCT CTA, we observed a clear agreement
between 64-MSCT CTA and SCA diagnosis (9). In summary we suggest that 64-MSCT CTA
is used at the early stages for those with no CHD symptoms, mild
symptoms or no significant variation in ECG results. It is not
necessary to perform a check with SCA if nothing shows up from the
64-MSCT CTA diagnosis. For those patients who have clear symptoms,
significant variation in ECG results and 64-MSCT CTA diagnosis
reveals moderate to severe coronary stenosis, a further SCA check
is necessary. A stent implantation therapy should be performed when
the coronary stenosis level reaches ≥70% (10).
Further development is required for 64-MSCT CTA to
improve the time resolution and spatial resolution. This enables an
advanced CT detector to reach an equal quality with SCA
(0.2×0.2×0.2mm) (11). With the
development of tube rotation speed and re-build technology, the
non-invasive CTA is considered the next generation method of
SCA.
References
|
1.
|
Schroeder S, Kopp AF, Baumbach A, et al:
Noninvasive detection and evaluation of atheroscleotic coronary
plaques with multislice computed tomography. J Am Coll Cardiol.
37:1430–1435. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Li P, Xu K, Li S, et al: Impact of heart
rate on image quality of 16-slice spiral CT coronary angiography
and optimization of image reconstruction window. Chin J Interv
Imaging Ther. 3:18–22. 2006.(In Chinese).
|
|
3.
|
Nieman K, Cademartiri F, Lemos PA, et al:
Reliable noninvasive coronary angiography with fast submillimeter
multislice spiral computed tomography. Circulation. 106:2051–2054.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Wang ZQ, Yang ZQ, Zhu H, et al: Detection
of coronary artery stenoses using 16-slice spiral CT: comparison
with quantitative coronary angiography. J Comput Tomogr. 3:7–11.
2003.
|
|
5.
|
Xue H, Zhang Z, Jin Z, Lin S, Zhao W,
Zhang L and Zhang S: Recommended orientations of the MSCT coronary
angiography. Chinese J Med Imaging. 12:324–327. 2004.(In
Chinese).
|
|
6.
|
Konen E, Goitein O, Sternik L, et al: The
prevalence and anatomical patterns of intramuscular coronary
arteries: a coronary computed tomography angiographic study. J Am
Coll Cardiol. 49:587–593. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Zhang G, Qian J, Fan B, et al: The impact
of myocardial bridge on coronary flow reverse. Chin J Cardiol.
30:279–281. 2002.(In Chinese).
|
|
8.
|
Zhang G and Ge J: Status of clinical
research ofmyocardial bridge. Chin J Intervent Cardiol. 10:52–54.
2002.(In Chinese).
|
|
9.
|
Heuschmid M, Kuettner A, Schroeder S, et
al: ECG-gated 16-MDCT of the coronary arteries: assessment of image
quality and accuracy in detecting stenoses. AJR Am J Roentgenol.
184:1413–1419. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Xu Y and Lv J: Analysis of 106 cases with
CTA 64-MSCT. Chinese Med J Metallurg Ind. 23:1012006.(In
Chinese).
|
|
11.
|
Morgan-Hughes GJ, Roobottom CA, Owens PE
and Marshall AJ: Highly accurate coronary angiography with
submillimetre, 16 slice computed tomography. Heart. 91:308–313.
2005. View Article : Google Scholar : PubMed/NCBI
|