Introduction
Ossification of the posterior longitudinal ligament
(OPLL) is recognized as a common clinical entity that results in
compression myelopathy of the cervical spinal cord. Since
conservative treatment for severe myelopathy caused by OPLL is
usually ineffective, surgical treatment is selected for the
majority of cases. Decompressive surgical procedures for
OPLL-associated cervical myelopathy are divided into those using an
anterior or a posterior approach. Iwasaki et al (1) identified that laminoplasty was
effective and safe for the majority of OPLL patients that had an
occupying ratio of OPLL <60% and with plateau-shaped
ossification. However, neurological outcomes following laminoplasty
for cervical OPLL were poor to fair in patients with an occupying
ratio of >60% and/or hill-shaped ossification (1). One of the factors associated with
poor surgical outcomes following laminoplasty for cervical OPLL is
kyphosis (1,2).
Clinical results from patients treated with the
posterior approach have been previously reported (1,2).
However, to date, there have been no studies focusing on the stress
distributions of posterior decompression for cervical OPLL and the
effects of kyphosis. In the present study, a 3-dimensional finite
element method (3D-FEM) was used to analyze the stress
distributions of posterior decompression, as well as kyphosis, in a
spinal cord with cervical OPLL and hill-shaped ossification.
Materials and methods
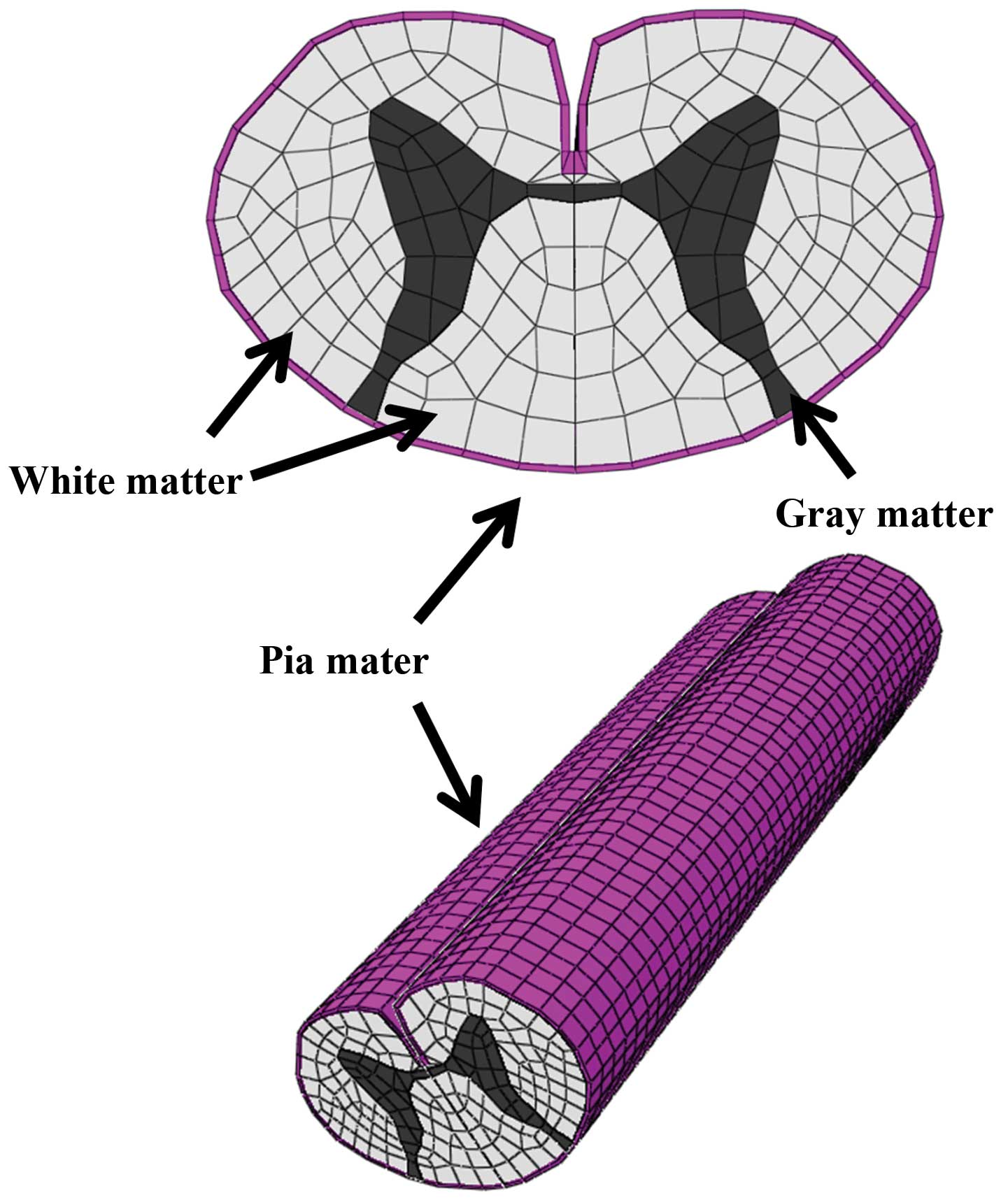
Spinal cord models
Abaqus 6.11 (Dassault Systèmes Simulia Corporation,
Providence, RI, USA) finite element package was used for FEM
simulation. The 3D-FEM spinal cord model established in this study
consisted of gray and white matter, as well as pia mater (Fig. 1). To simplify calculations in the
model, the denticulate ligament, dura and nerve root sheaths were
not included. The pia mater was included since it has been
previously identified that the spinal cord with and without this
component shows significantly different mechanical behavior
(3). The spinal cord was assumed
to be symmetrical around the mid-sagittal plane; therefore, only
half the spinal cord required reconstruction and the whole model
was integrated by mirror image. For computed tomography-myelography
(CTM) measurement, the vertical length of the spinal cord was two
vertebral bodies (~40 mm).
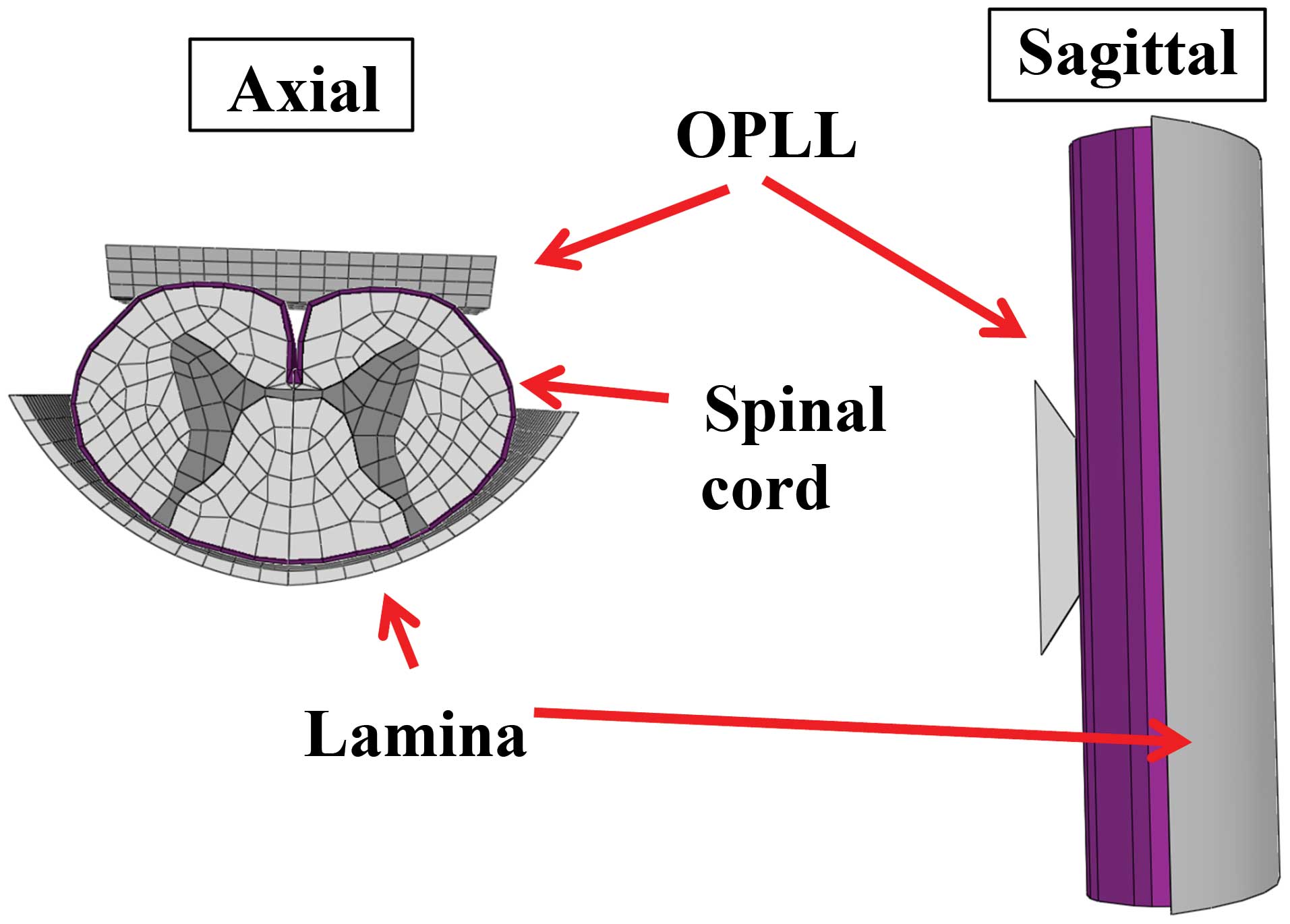
The lamina model was established by measuring CTM
and magnetic resonance imaging (MRI) and simulated cervical OPLL. A
rigid, wide trapezium body with a slope of 30° was used to simulate
cervical OPLL by measuring the MRI of paper (Fig. 2) (1).
Mechanical properties
The spinal cord consists of three distinct materials
referred to as white matter, gray matter and pia mater. The
mechanical properties (Young’s modulus and Poisson’s ratio) of the
gray and white matter were determined using data obtained by the
tensile stress strain curve and stress relaxation under various
strain rates (4,5). The mechanical properties of pia mater
were obtained from previous literature (6). The mechanical properties of
hill-shaped ossification and lamina were stiff enough for the
spinal cord to be pressed. Based on the assumption that no slippage
occurs at the interfaces of white matter, gray matter and pia
mater, these interfaces were glued together. Since there are no
data on the friction coefficient between the lamina and spinal
cord, this was assumed to be frictionless. Similarly, the
coefficient of friction between the hill-shaped ossification and
spinal cord was assumed to be frictionless at the contact
interfaces.
The spinal cord, hill-shaped ossification and lamina
model were symmetrically meshed with 20-node elements. The total
number of isoparametric 20-node elements was 11,542 and the total
number of nodes was 66,513.
Compression
In a biomechanical study of static compression of
cervical myelopathy due to OPLL, Kato et al (7) reported that a critical point may
exist between 20 and 40% compression of the anterior-posterior
diameter of the spinal cord. For the preoperative model,
compression was simulated by cervical OPLL with hill-shaped
ossification. The lamina was fixed in all directions and 30%
anterior static compression of the anterior-posterior diameter of
the spinal cord (median, 20–40%) was applied by OPLL (1,7). For
the posterior decompressive model, the lamina was shifted back to
prevent contact with the spinal cord under the application of
anterior static compression. For the kyphosis model, the spinal
cord was studied at 10, 20, 30, 40 and 50° kyphosis. The extent of
stretching the spinal cord was 20% of the length of the spinal cord
indicated in a previous study (8).
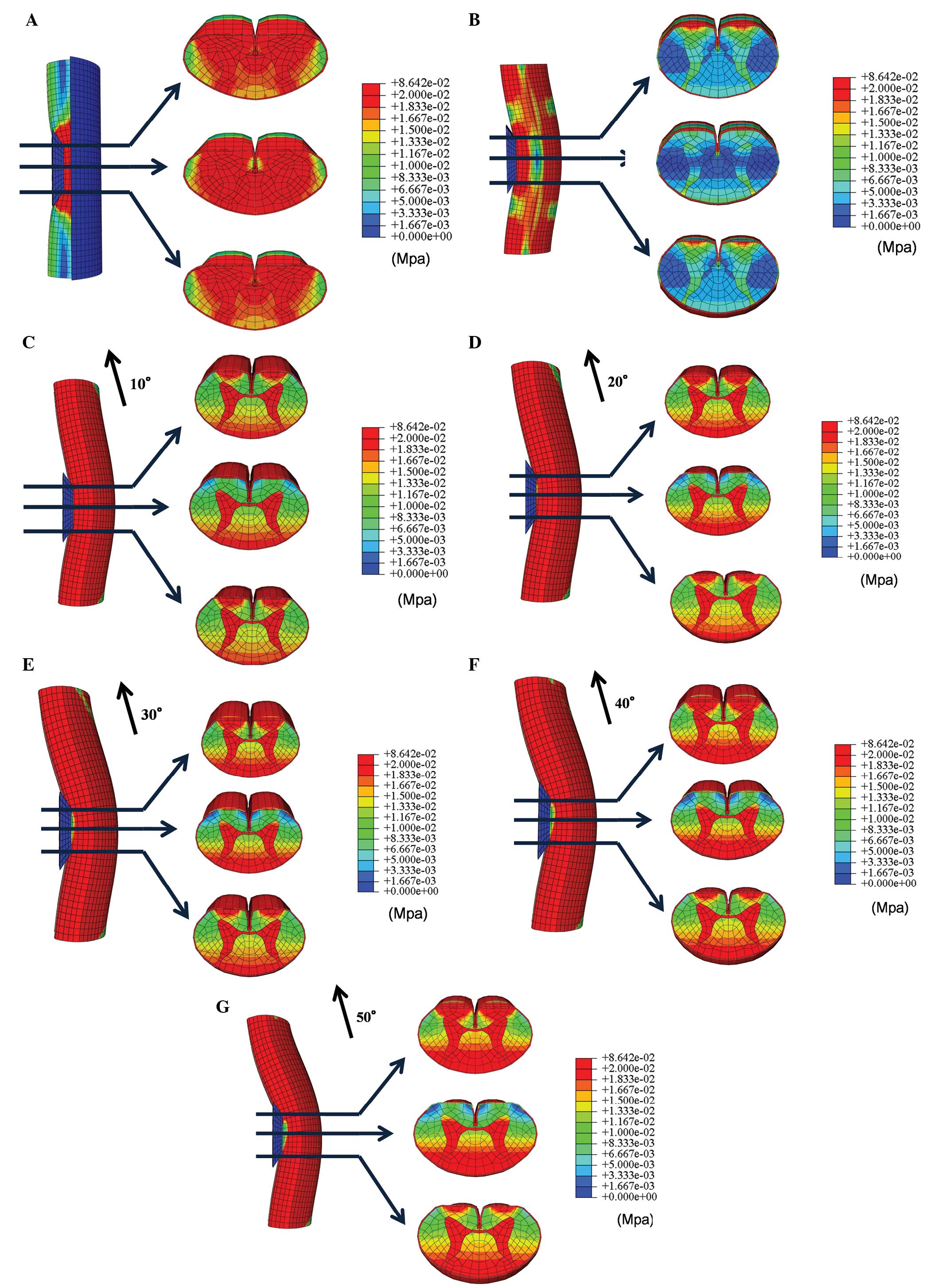
In total, seven compression combinations were
evaluated and in each cross-section the average von Mises stress
was recorded the color-coded made for each stress in the spinal
cord.
Results
Stress distribution in the three
models
In the preoperative model, high stress distributions
were observed in all axial levels of the spinal cord following
anterior static compression (30% of the anterior-posterior diameter
of the spinal cord) by cervical OPLL with hill-shaped ossification
(Fig. 3A).
In the posterior decompression model, stresses from
anterior compression of the spinal cord were lower compared with
those observed in the preoperative model. However, stresses in the
anterior funiculus slightly increased (Fig. 3B).
For the kyphosis model, stress distribution
increased in the anterior funiculus, posterior funiculus and the
gray matter in proximal and distal OPLL. The stress distribution
also increased in the posterior funiculus and the gray matter in
the center of OPLL. Furthermore, increasing the angle of kyphosis
resulted in increased stress on the spinal cord (Fig. 3C–G).
Discussion
The development of myelopathy significantly affects
the prognosis of patients with OPLL in the cervical spine. Cervical
OPLL is treated by anterior decompression and spinal fusion or
laminoplasty. Tani et al identified that postoperative
neurological deterioration occurred following posterior surgery.
The authors indicated that one of factors of neurological
deterioration affectedto decrease in the lordosis of the cervical
spine (9).
Masaki et al reported that patients with a
poor outcome following laminoplasty showed larger segmental
mobility of the vertebrae prior to and following surgery. The
authors hypothesized that laminoplasty in patients with massive
OPLL may not lead to sufficient posterior shift of the spinal cord,
resulting in persistent anterior impingement of the spinal cord by
OPLL. In cases where substantial segmental mobility remains
following surgery, it is possible that damage to the injured spinal
cord continues to progress (10).
Iwasaki et al reported that a postoperative
change in cervical alignment was observed in 18% of cases. Their
study indicated that postoperative changes in cervical alignment
may be a reflection of dynamic instability. A poor surgical outcome
following laminoplasty was indicated by newly developed cervical
kyphosis (1).
Using this prior knowledge, the present study
investigated whether the development of kyphosis of the spinal cord
following anterior compression was associated with changes in
stress distribution. The aim was to develop a 3D-FEM spinal cord
model that simulated the clinical situation and analyzed the
clinical condition of the patient. Similarly to previous studies by
Kato et al (7,11,12),
Li et al (13,14) and Nishida et al (15,16),
bovine spinal cord was used in the current analytical model since
it was impossible to obtain fresh human spinal cord. The mechanical
properties of the spinal cord used in the present study were
similar to those used in earlier studies (4–6). Li
et al identified that it was reasonable to use the
mechanical properties of the bovine spinal cord since the brain and
spinal cord of cattle and humans show similar injury changes
(14). For the purpose of the
present study, it was therefore assumed that the mechanical
properties of the spinal cord from these two species were similar.
Persson et al (3) reported
on the division of the spinal cord into pia mater and white and
gray matter. The authors demonstrated that the presence of pia
mater had a significant effect on spinal cord deformation.
Therefore, pia mater was included in the current model in order to
accurately simulate the clinical situation.
In the present study, stress distribution in the
spinal cord increased following static compression by cervical OPLL
with hill-shaped ossification. Stress distribution in the spinal
cord decreased in the posterior decompression model, demonstrating
the effectiveness of this approach. However, in the kyphosis model,
stress distribution increased with increased angles of kyphosis.
Thus, when segmental mobility remains and cervical alignment
changes following posterior decompression, damage to the spinal
cord and the progression of symptoms are likely to occur.
In conclusion, stress analyses were conducted in
models of preoperative compression, posterior decompression and
kyphosis following posterior decompression by cervical OPLL with
hill-shaped ossification.
Posterior decompression was shown to be effective,
however, stress distribution increased with the progression of
kyphosis, indicating that symptoms are likely to worsen. In cases
where kyphosis has progressed following surgery, particularly those
in which the angle of kyphosis is large, detailed follow-ups should
be conducted in case the symptoms worsen.
References
|
1
|
Iwasaki M, Okuda S, Miyauchi A, Sakaura H,
Mukai Y, Yonenobu K and Yoshikawa H: Surgical strategy for cervical
myelopathy due to ossification of the posterior longitudinal
ligament: Part 1: Clinical results and limitations of laminoplasty.
Spine (Phila Pa 1976). 32:647–653. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Chiba K, Ogawa Y, Ishii K, Takaishi H,
Nakamura M, Maruiwa H, Matsumoto M and Toyama Y: Long-term results
of expansive open-door laminoplasty for cervical myelopathy -
average 14-year follow-up study. Spine (Phila Pa 1976).
31:2998–3005. 2006.PubMed/NCBI
|
|
3
|
Persson C, Summers J and Hall RM: The
importance of fluid-structure interaction in spinal trauma models.
J Neurotrauma. 28:113–125. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ichihara K, Taguchi T, Shimada Y,
Sakuramoto I, Kawano S and Kawai S: Gray matter of the bovine
cervical spinal cord is mechanically more rigid and fragile than
the white matter. J Neurotrauma. 18:361–367. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ichihara K, Taguchi T, Sakuramoto I,
Kawano S and Kawai S: Mechanism of the spinal cord injury and the
cervical spondylotic myelopathy: new approach based on the
mechanical features of the spinal cord white and gray matter. J
Neurosurg. 99(Suppl 3): S278–S285. 2003.PubMed/NCBI
|
|
6
|
Tunturi AR: Elasticity of the spinal cord,
pia, and denticulate ligament in the dog. J Neurosurg. 48:975–979.
1978. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kato Y, Kanchiku T, Imajo Y, et al:
Biomechanical study of the effect of the degree of static
compression of the spinal cord in ossification of the posterior
longitudinal ligament. J Neurosurg Spine. 12:301–305. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Henderson FC, Geddes JF, Vaccaro AR,
Woodard E, Berry KJ and Benzel EC: Stretch-associated injury in
cervical spondylotic myelopathy: new concept and review.
Neurosurgery. 56:1101–1113. 2005.PubMed/NCBI
|
|
9
|
Tani T, Ushida T, Ishida K, et al:
Relative safety of anterior microsurgical decompression versus
laminoplasty for cervical myelopathy with a massive ossified
posterior longitudinal ligament. Spine (Phila Pa 1976).
27:2491–2498. 2002. View Article : Google Scholar
|
|
10
|
Masaki Y, Yamazaki M, Okawa A, et al: An
analysis of factors causing poor surgical outcome in patients with
cervical myelopathy due to ossification of the posterior
longitudinal ligament: anterior decompression with spinal fusion
versus laminoplasty. J spinal Disord Tech. 20:7–13. 2007.
View Article : Google Scholar
|
|
11
|
Kato Y, Kataoka H, Ichihara K, et al:
Biomechanical study of cervical flexion myelopathy using a
three-dimensional finite element method. J Neurosurg Spine.
8:436–441. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kato Y, Kanchiku T, Imajo Y, et al:
Flexion model simulating spinal cord injury without radiographic
abnormality in patients with ossification of the longitudinal
ligament: the influence of flexion speed on the cervical spine. J
Spinal Cord Med. 32:555–559. 2009.
|
|
13
|
Li XF and Dai LY: Three-dimensional finite
element model of the cervical spinal cord. Spine (Phila Pa 1976).
34:1140–1147. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Li XF and Dai LY: Acute central cord
syndrome: injury mechanisms and stress features. Spine (Phila Pa
1976). 35:E955–E964. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Nishida N, Kato Y, Imajo Y, Kawano S and
Taguchi T: Biomechanical study of the spinal cord in thoracic
ossification of the posterior longitudinal ligament. J Spinal Cord
Med. 34:518–522. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Nishida N, Kato Y, Imajo Y, Kawano S and
Taguchi T: Biomechanical analysis of cervical spondylotic
myelopathy: the influence of dynamic factors and morphometry of the
spinal cord. J Spinal Cord Med. 35:256–261. 2012. View Article : Google Scholar : PubMed/NCBI
|