Introduction
Sepsis, a systemic inflammatory response induced by
severe infection, which usually leads to multiple organ dysfunction
syndromes, is a common cause of critical illness and mortality in
intensive care units (1). Although
there have been developments in sophisticated monitoring,
antibiotic therapy and glucocorticoid treatment, and advances in
the understanding of the molecular underpinnings of sepsis, a
number of its complications remain refractory to treatment
(2,3). In 2007, the severe sepsis mortality
rate was reported to range between 30 and 50%, rising to 80–90% for
patients with septic shock and multiple organ failure (4).
In the progression of sepsis, it is considered that
the hyperactive systemic inflammatory response, with a large number
of inflammatory cytokines and excessive generation of free
radicals, is one of the main causes of multiple organ injury.
Therefore, accompanying antibiotics treatment, anti-inflammation
and anti-oxidation were usually used as important therapeutic
strategies for the sepsis. In previous studies, the marked
synergetic analgesic and anti-inflammatory effects of the
combination of sodium ferulate (SF) and oxymatrine (OMT) have been
identified and reported (5–7).
Thus, it may be hypothesized that treatment with a combination of
SF and OMT will alleviate the inflammatory response and multiple
organ injury induced by sepsis.
In the present study, cecal ligation and puncture
(CLP)-induced septic mice models were used to evaluate the effects
of the combination of SF and OMT based on the anti-inflammatory and
antioxidative effects of the treatment. The survival rates and
survival times of the animals were monitored. The lung wet/dry
weight (W/D) ratio, which represents the degree of lung injury, was
calculated. The levels of serum alanine aminotransferase (ALT),
aspartate aminotransferase (AST) and lactate dehydrogenase (LDH)
were measured, which indicated the degree of injury to the organs.
Furthermore, the C-reactive protein (CRP), interleukin-6 (IL-6) and
interferon-γ (IFN-γ) levels were assayed, which reflected the
anti-inflammatory efficacy of the treatment. Also, in order to
investigate the oxidative injury, the levels of malondialdehyde
(MDA), a biomarker of oxidative injury, and superoxidase dismutase
(SOD), an important free radical scavenger in vivo, were
measured.
Materials and methods
Drugs and chemicals
SF [molecular formula:
C10H9NaO4.2H2O;
molecular weight: 252.20; CAS: 24276-84-4; high-performance liquid
chromatography (HPLC) purity: >99%] and OMT (molecular formula:
C15H24N2O2.H2O;
molecular weight: 282.38; CAS: 16837-52-8; HPLC purity: >98%)
were provided by Beijing SL Pharmaceutical Co., Ltd. (Beijing,
China). The optimal ratio (molar ratio = 1:2) of the combination of
SF and OMT was obtained by pharmaceutical and pharmacological
tests. When the molar ratio of SF and OMT was 1:2, the solution
system was the most stable with a pH value of 7.0, and the
pharmacological activity was also strongest (unpublished data).
Animals
Swiss male mice (18–22 g; Shandong Luye
Pharmaceutical Co., Ltd, Yantai, China; Quality Certificated
Number: Lu 20090013) were used. The animals were maintained under
standard conditions (12-h light/dark cycle, temperature: 23±2°C,
humidity: 55±5%) for 3–7 days for acclimatization to the
surrounding environment. The animals had access to food and water
ad libitum. Within the 12 h prior to the experiment, only
water was supplied. In accordance with the National Institutes of
Health Guide for the Care and Use of Laboratory Animals (Eighth
edition, 2012), all procedures conducted in these experiments were
approved by the Experimental Animal Management Center of Yantai
University (Yantai, China).
Model of CLP-induced sepsis
The animals were randomly divided into seven groups
with 30 mice in each group. The groups were as follows: i) Control
(saline); ii) CLP (saline); iii) SF + OMT (3.1+6.9 mg/kg); iv) SF +
OMT (6.2+13.8 mg/kg); v) SF + OMT (12.3+27.7 mg/kg); vi) SF (6.2
mg/kg); and vii) OMT (13.8 mg/kg). Following anesthetization with
chloraldurate (3%), the animals underwent surgery with reference to
the methods of Baker et al (8). Briefly, a midline incision was made
below the diaphragm to expose the cecum. The cecum was ligated
immediately below the ileocecal valve with 1-0 silk so that
intestinal continuity was maintained. Following two punctures with
a five-gauge needle, the cecum was gently compressed until fecal
matter was extruded. Subsequently, the cecum was gently returned to
the abdomen, and the incision was closed in layers with a 2-0 silk
ligature suture. The animals in the control group underwent a
laparotomy, and the cecum was manipulated, but not ligated and
perforated. At the end of the surgery, the corresponding drugs or
saline were administered intraperitoneally; the quantity of saline
administered was 20 ml/kg body weight. Following resuscitation of
the animals, food and water were provided ad libitum.
Survival rate and survival time
In each group, the survival rates and survival times
of 10 mice were monitored. Following the CLP surgery, the animals
were carefully observed for ~8 h, followed by observation every 8 h
for 24 h. The time of mortality was recorded. If an animal
succumbed between the observations at 8 and 16 h, the survival time
was recorded as 16 h, and if the animal had not succumbed by the 24
h point, the survival time was recorded as 24 h. After 24 h, the
surviving mice were sacrificed with carbon dioxide anesthesia.
Bacterial load determination
In a preliminary experiment, the animals began to
succumb at ~10 h after CLP surgery. Thus in the present study, 8 h
after the CLP surgery, 10 mice from each group were randomly
selected and blood was obtained sterilely by percutaneous cardiac
puncture, then diluted 100-fold with phosphate-buffered saline
(PBS). The bacterial load was determined with reference to the
methods of Standage et al (9). Briefly, 200 μl diluted blood from
each mouse was plated on a chocolate agar plate (Thermo Fisher
Scientific Inc., Pittsburgh, PA, USA). The plates were incubated
for 24 h at 37°C and the number of colony forming units (CFUs) was
counted.
Lung W/D ratio calculation
Following the collection of the blood for bacterial
load determination, the animals were sacrificed and the lungs were
excised immediately. The lungs of each animal (n=10) were weighed,
and then dried in an oven at 70°C for 48 h and re-weighed. The W/D
ratio was calculated using the following formula: W/D ratio = wet
weight / dry weight.
Separation of serum and preparation of
lung and liver homogenates
Blood was collected from an eyeball of each of the
10 mice remaining in each group following anesthesia with diethyl
ether. The serum was separated by centrifugation at 600 × g for 10
min and stored at −80°C for further biochemical analysis.
Subsequently, the animals were sacrificed. The lungs and livers
were excised and homogenized in PBS on ice to prepare a 10%
homogenate using a Vertishear tissue homogenizer (Virtis, Gardiner,
NY, USA). The homogenate was also stored at −80°C for further
biochemical analysis.
Biochemical analysis
The levels of ALT, AST and LDH in the serum were
measured by routine laboratory methods using a Toshiba Automatic
analyzer (TOSHIBA TBA-40FR ACCUTE, Toshiba Corporation, Tokyo,
Japan). The levels of CRP, IL-6 and IFN-γ in the serum and in the
lung and liver homogenates were measured by enzyme-linked
immunosorbent assay (ELISA) kits according to the manufacturer’s
instructions. The ELISA kits for the determination of the levels of
CRP, IFN-γ and IL-6 were produced by Groundwork Biotechnology
Diagnosticate Ltd (San Diego, CA, USA). The MDA content and SOD
activity levels in the lung and liver homogenates were measured as
described previously (10,11). Briefly, the MDA content was
detected by the thiobarbituric acid method with a maximal
absorbance at 532 nm, and the SOD activity levels were measured
based on the SOD-mediated inhibition of nitrite formation from
hydroxyammonium in the presence of O2•−
generators (xanthine/xanthine oxidase) (10). The MDA and SOD test kits were
produced by Nanjing Jiancheng Bioengineering Institute (Nanjing,
China), and have been used in numerous studies (12,13).
Statistical analysis
All data are presented as the mean ± standard error
of the mean and were analyzed by one-way analysis of variance, with
Statistical Product and Service Solutions software, version 17.0
(SPSS, Inc., Chicago, IL, USA). The χ2 test was used to
compare the differences of the survival rates between two groups.
P<0.05 was considered to indicate a statistically significant
difference.
Results
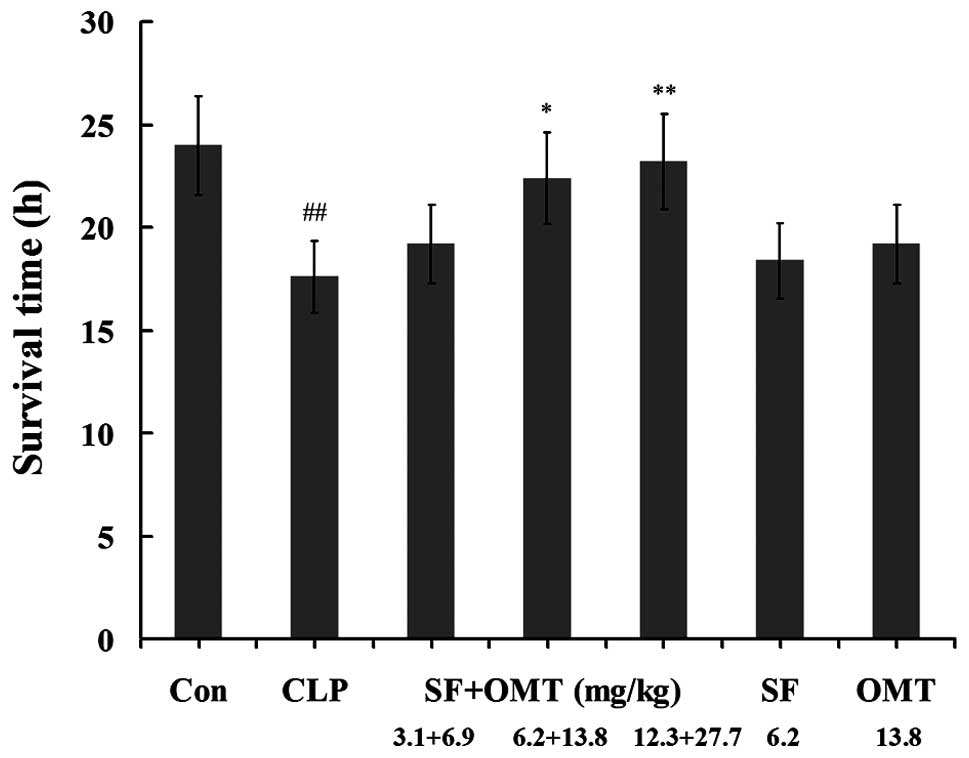
Effects of SF and OMT used in combination
or alone on the survival rate and survival time
As shown in Table
I, within 24 h after the surgery, all animals survived in the
control group. In the CLP group, the animal survival rate was 20%
at 16 h and all animals had died by 24 h. Treatment with the
combination of SF and OMT at the medium and high doses
significantly increased the survival rate and prolonged the
survival time compared with those of the CLP group (Fig. 1). At 24 h, the survival rates were
20, 40 and 50% in the SF + OMT 3.1+6.9; 6.2+13.8; and 12.3+27.7
mg/kg combination groups, respectively. Treatment with either SF
(6.2 mg/kg) or OMT (13.8 mg/kg) alone did not significantly
increase the survival rate at 24 h after the surgery (0 and 10%,
respectively), or prolong the survival time compared with those of
the combination groups.
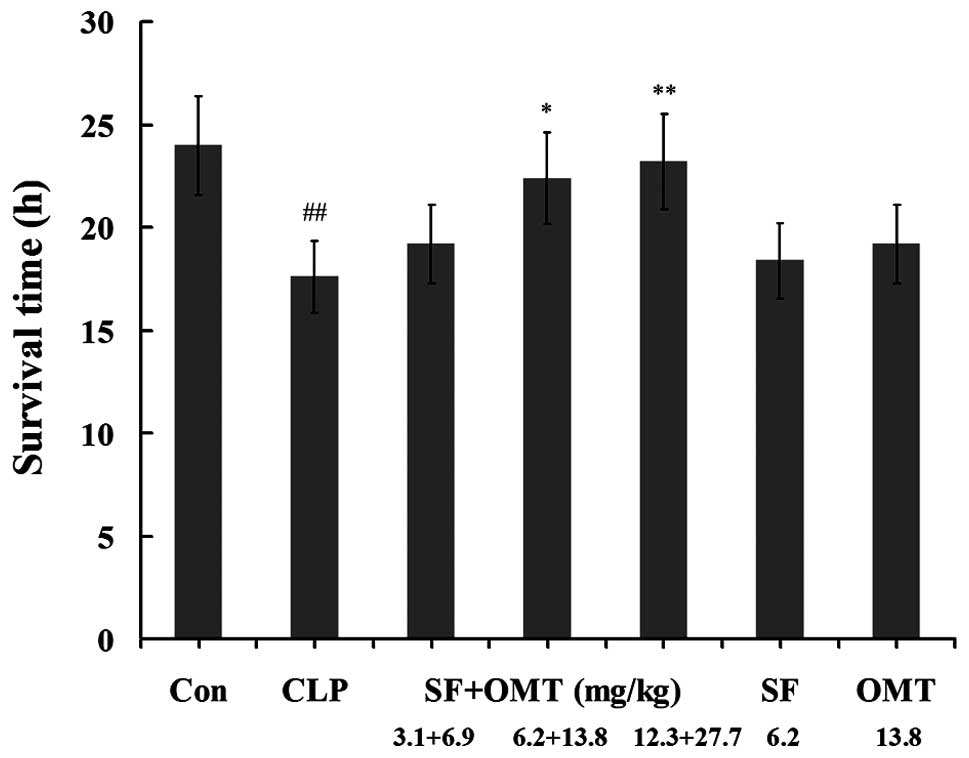 | Figure 1Effects of the combination of SF and
OMT on the survival time of CLP-induced septic mice. Con, CLP, SF
and OMT represent the control group, CLP group, SF (6.2 mg/kg) and
OMT (13.8 mg/kg) groups, respectively. SF + OMT represents the SF
and OMT combination groups. The data are expressed as the mean ±
standard error of the mean. n=10 in each group.
##P<0.01, versus the control group.
*P<0.05 and **P<0.01, versus the CLP
group. CLP, cecal ligation and puncture; SF, sodium ferulate; OMT,
oxymatrine. |
 | Table IEffects of the combination of SF and
OMT on the survival rate of CLP-induced septic mice (n=10 per
group). |
Table I
Effects of the combination of SF and
OMT on the survival rate of CLP-induced septic mice (n=10 per
group).
| | Survival rate
(%) |
|---|
| |
|
|---|
| Group | Dose (mg/kg) | 16 h | 24 h |
|---|
| Con | - | 100 | 100 |
| CLP | - | 20a | 0a |
| SF+OMT (low
dose) | 3.1+6.9 | 40 | 20 |
| SF+OMT (medium
dose) | 6.2+13.8 | 80a | 40b |
| SF+OMT (high
dose) | 12.3+27.7 | 90c | 50c |
| SF | 6.2 | 30 | 0 |
| OMT | 13.8 | 40 | 10 |
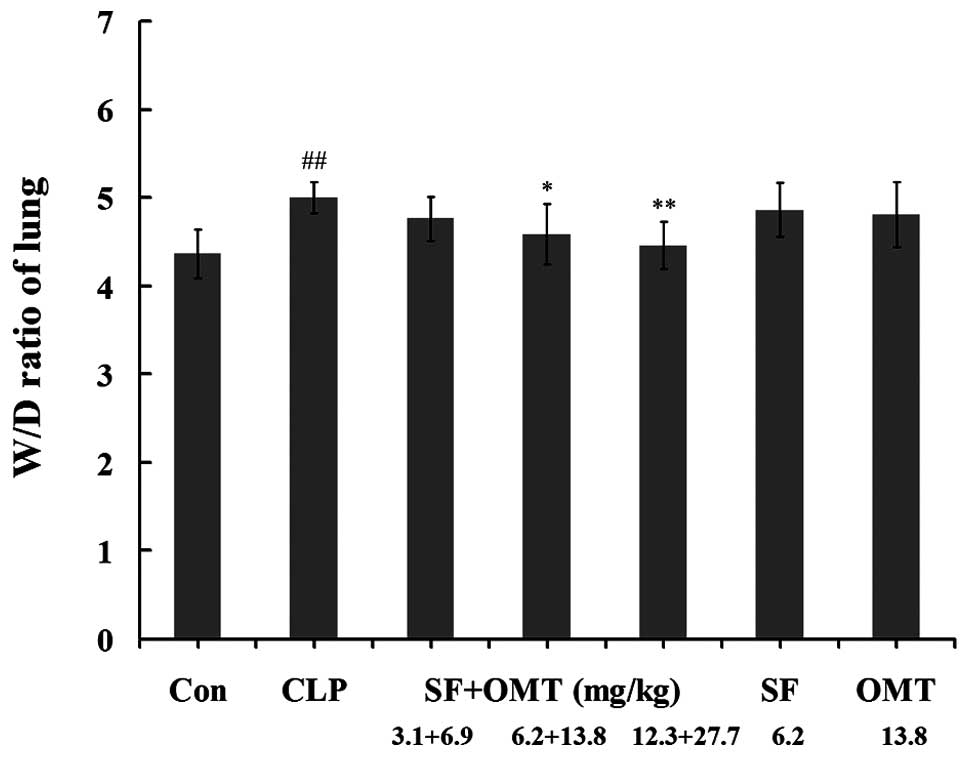
Effects of SF and OMT used in combination
or alone on the lung W/D ratio
As shown in Fig. 2,
the lung W/D ratio increased significantly in the CLP group
compared with that in the control group. The combination treatment
reduced the lung W/D ratio compared with that of the CLP group
(P<0.05 in the medium dose group; P<0.01 in the high dose
group). No significant efficacy was observed in the groups treated
with SF (6.2 mg/kg) or OMT (13.8 mg/kg) alone.
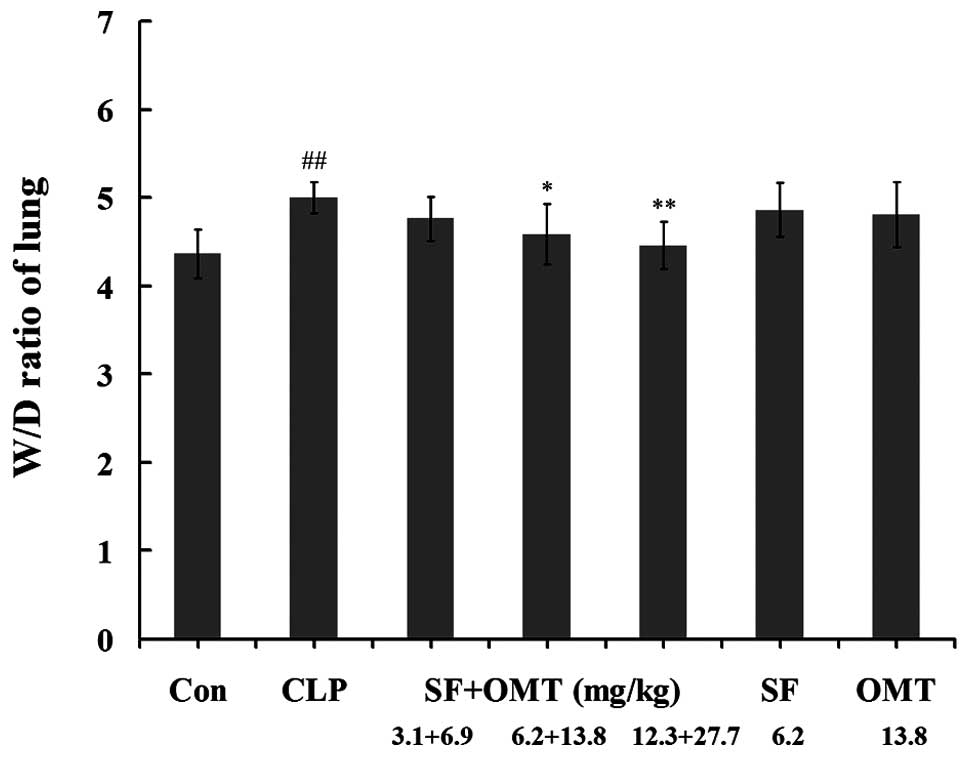 | Figure 2Effects of the combination of SF and
OMT on the lung W/D ratio of CLP-induced septic mice. Con, CLP, SF
and OMT represent the control group, CLP group, SF (6.2 mg/kg) and
OMT (13.8 mg/kg) groups, respectively. SF + OMT represents the SF
and OMT combination groups. The lung W/D ratio was determined at 8
h after the CLP surgery. The data are expressed as the mean ±
standard error of the mean. ##P<0.01, versus the
control group. *P<0.05 and **P<0.01,
versus the CLP group. W/D, wet/dry weight; CLP, cecal ligation and
puncture; SF, sodium ferulate; OMT, oxymatrine. |
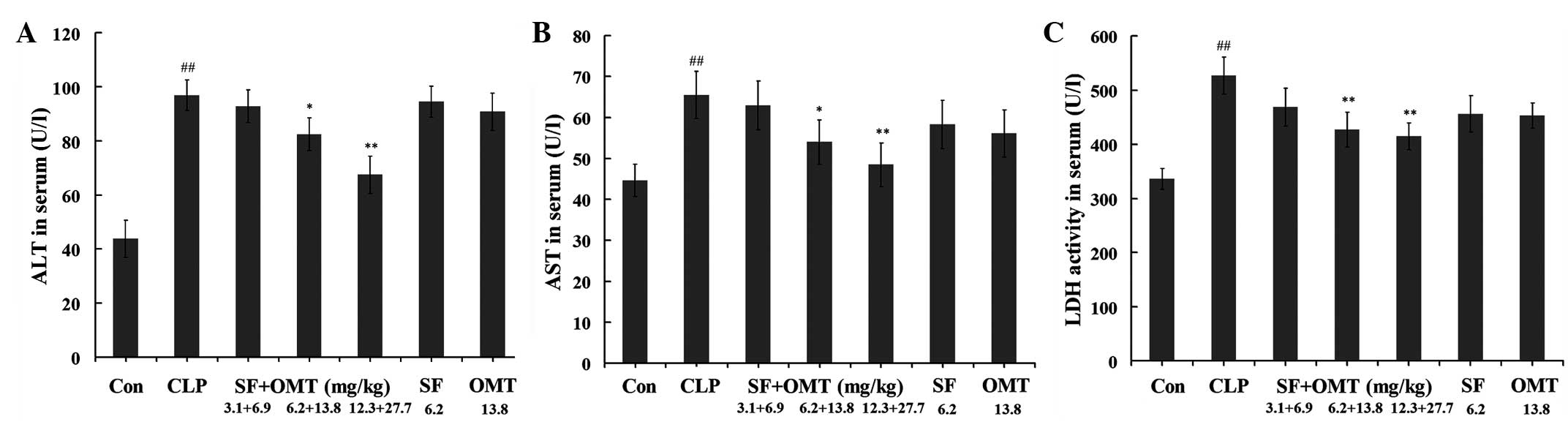
Effects of SF and OMT used in combination
or alone on the levels of ALT, AST and LDH in serum
As shown in Fig. 3,
following the CLP surgery, the serum ALT, AST and LDH levels
notably increased in the CLP group compared with those in the
control group. In the medium and high dose groups of the SF and OMT
combination treatment (SF + OMT 6.2+13.8 and 12.3+27.7 mg/kg) the
serum LDH, ALT and AST levels significantly decreased compared with
those in the CLP group. No significant inhibitory effects on serum
LDH, ALT and AST levels were observed in the groups treated with SF
(6.2 mg/kg) or OMT (13.8 mg/kg) alone.
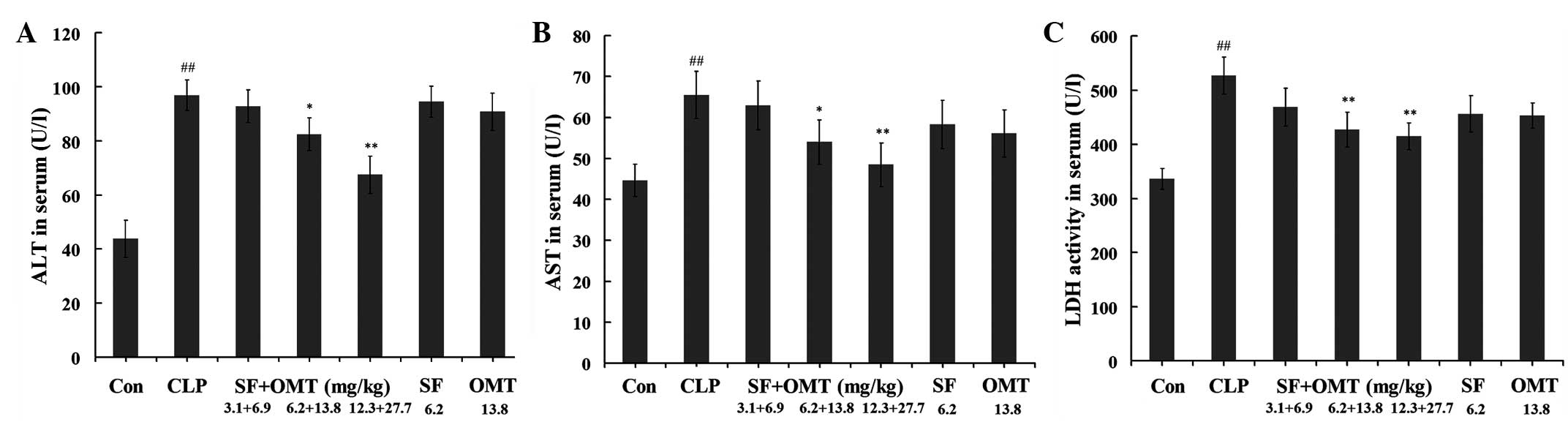 | Figure 3Effects of the combination of SF and
OMT on the levels of (A) ALT, (B) AST and (C) LDH in the serum of
CLP-induced septic mice. Con, CLP, SF and OMT represent the control
group, CLP group, SF (6.2 mg/kg) and OMT (13.8 mg/kg) groups,
respectively. SF + OMT represents the SF and OMT combination
groups. The data are expressed as the mean ± standard error of the
mean. n=10 in each group. ##P<0.01, versus the
control group. *P<0.05 and **P<0.01,
versus the CLP group. ALT, alanine aminotransferase; CLP, cecal
ligation and puncture; SF, sodium ferulate; OMT, oxymatrine; AST,
aspartate aminotransferase; LDH, lactate dehydrogenase. |
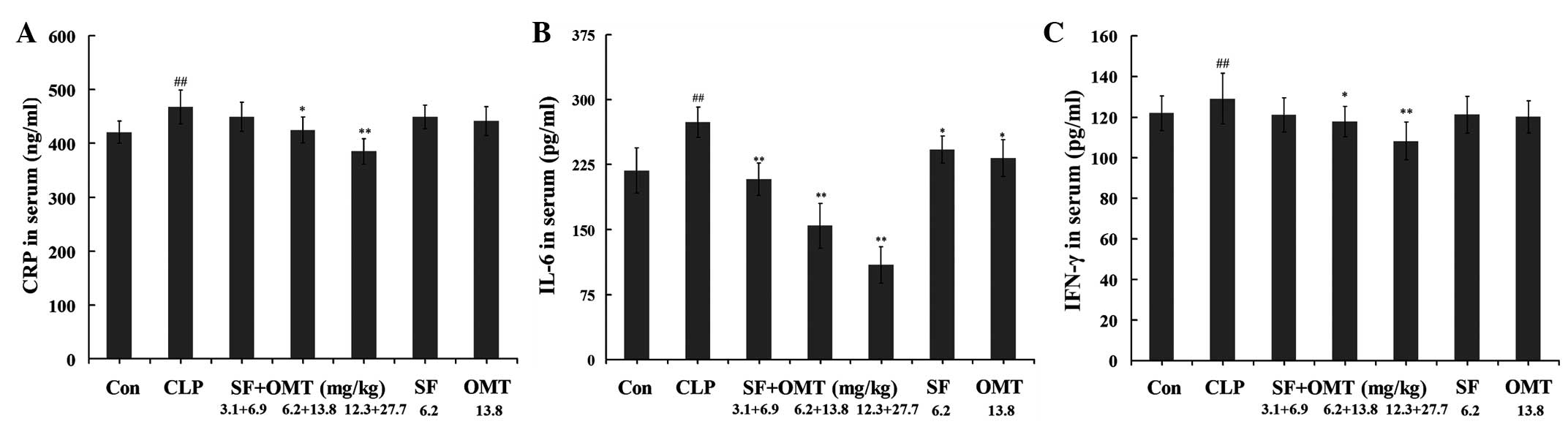
Effects of SF and OMT used in combination
or alone on the levels of CRP, IL-6 and IFN-γ in serum
Following the CLP surgery (8 h), the serum CRP, IL-6
and IFN-γ levels all significantly increased in the CLP group
compared with those in the control group (Fig. 4). In all combination treatment
groups (SF + OMT 3.1+6.9, 6.2+13.8 and 12.3+27.7 mg/kg), the levels
of IL-6 in the serum were significantly reduced in a dose-dependent
manner compared with those in the CLP group (P<0.01). The levels
of CRP and IFN-γ in the serum were significantly decreased in the
high and medium dose groups of the combination treatment compared
with those in the CLP group (P<0.05 in the medium dose group;
P<0.01 in the high dose group). With the exception of the levels
of IL-6 in the serum, which decreased significantly (P<0.05) in
the SF (6.2 mg/kg) and OMT (13.8 mg/kg) alone groups, the other
measured indices did not exhibit significant changes in the SF or
OMT alone treatment groups compared with the levels in the CLP
group.
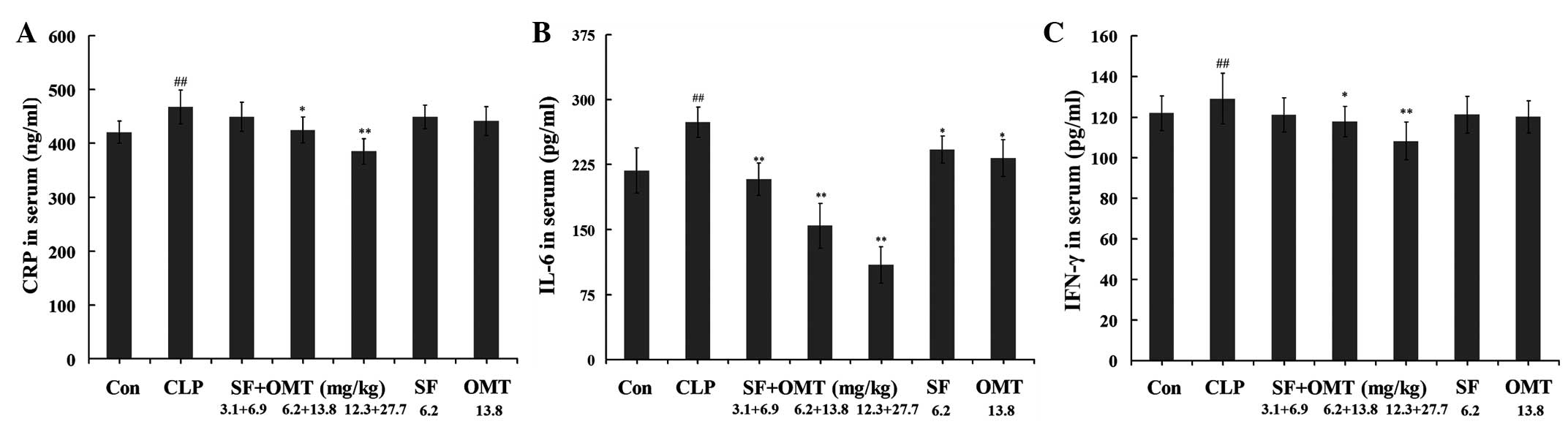 | Figure 4Effects of the combination of SF and
OMT on the levels of (A) CRP, (B) IL-6 and (C) IFN-γ in the serum
of CLP-induced septic mice. Con, CLP, SF and OMT represent the
control group, CLP group, SF (6.2 mg/kg) and OMT (13.8 mg/kg)
groups, respectively. SF + OMT represents the SF and OMT
combination groups. The data are expressed as the mean ± standard
error of the mean. n=10 in each group. ##P<0.01,
versus the control group. *P<0.05 and
**P<0.01, versus the CLP group. CRP, C-reactive
protein; CLP, cecal ligation and puncture; SF, sodium ferulate;
OMT, oxymatrine; IL-6, interleukin-6; IFN-γ, interferon-γ. |
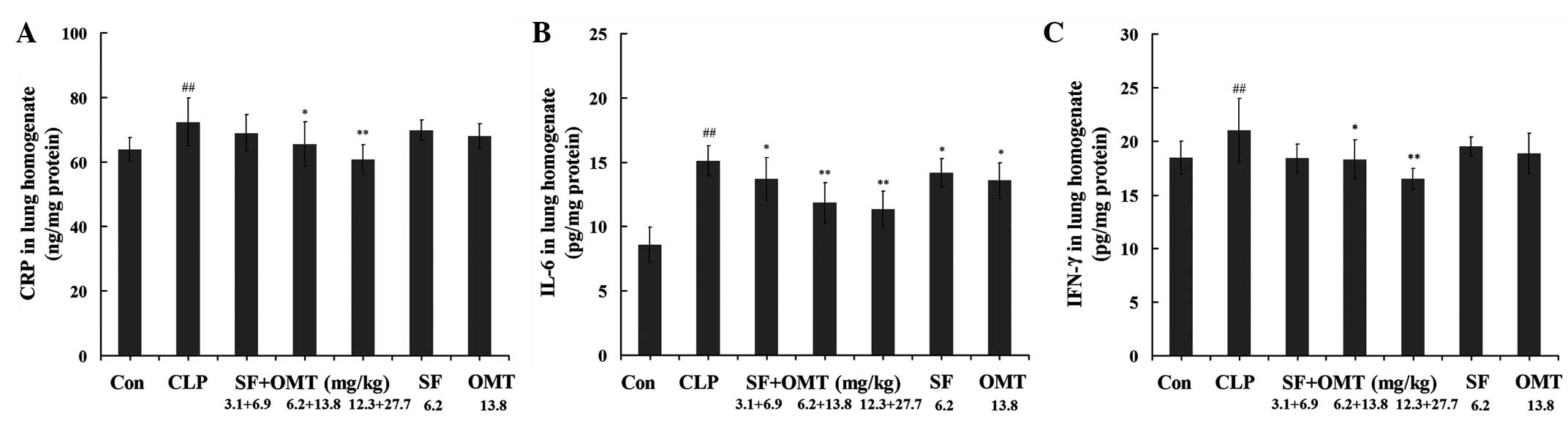
Effects of SF and OMT used in combination
or alone on the levels of CRP, IL-6 and IFN-γ in the lung
homogenate
As shown in Fig. 5,
following the CLP surgery, the levels of CRP, IL-6 and IFN-γ in
lung homogenate notably increased in the CLP group compared with
those in the control group. Treatment with the combination of SF
and OMT (SF + OMT 3.1+6.9, 6.2+13.8 and 12.3+27.7 mg/kg)
significantly reduced the levels of IL-6 compared with those in the
CLP group (P<0.05 in the low dose group; P<0.01 in the high
and medium dose groups). The CRP and IFN-γ levels in the lung
homogenate were significantly reduced in the high and medium dose
groups of the combination treatment compared with those in the CLP
group (P<0.05 in the medium dose group; P<0.01 in the high
dose group). With the exception of the levels of IL-6 in the lung
homogenate, which decreased significantly in the SF (6.2 mg/kg) and
OMT (13.8 mg/kg) groups (P<0.05), the other measured indices did
not exhibit significant changes in the SF or OMT alone treatment
groups compared with the levels in the CLP group.
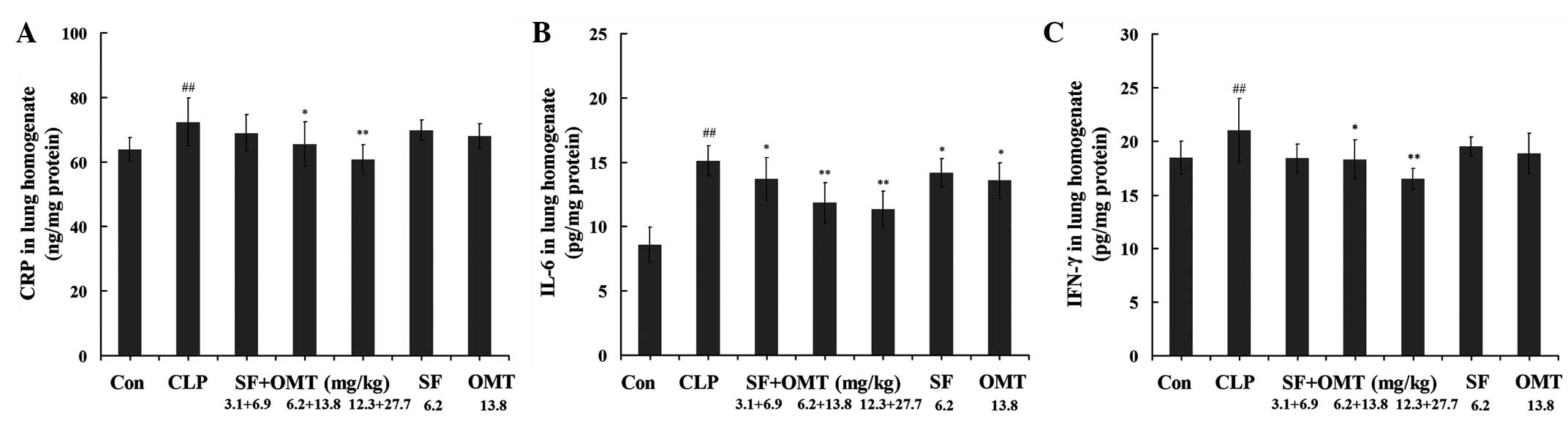 | Figure 5Effects of the combination of SF and
OMT on the levels of (A) CRP, (B) IL-6 and (C) IFN-γ in the lung
homogenates of CLP-induced septic mice. Con, CLP, SF and OMT
represent the control group, CLP group, SF (6.2 mg/kg) and OMT
(13.8 mg/kg) groups, respectively. SF + OMT represents the SF and
OMT combination groups. The data are expressed as the mean ±
standard error of the mean. n=10 in each group.
##P<0.01, versus the control group.
*P<0.05 and **P<0.01, versus the CLP
group. CRP, C-reactive protein; CLP, cecal ligation and puncture;
SF, sodium ferulate; OMT, oxymatrine; IL-6, interleukin-6; IFN-γ,
interferon-γ. |
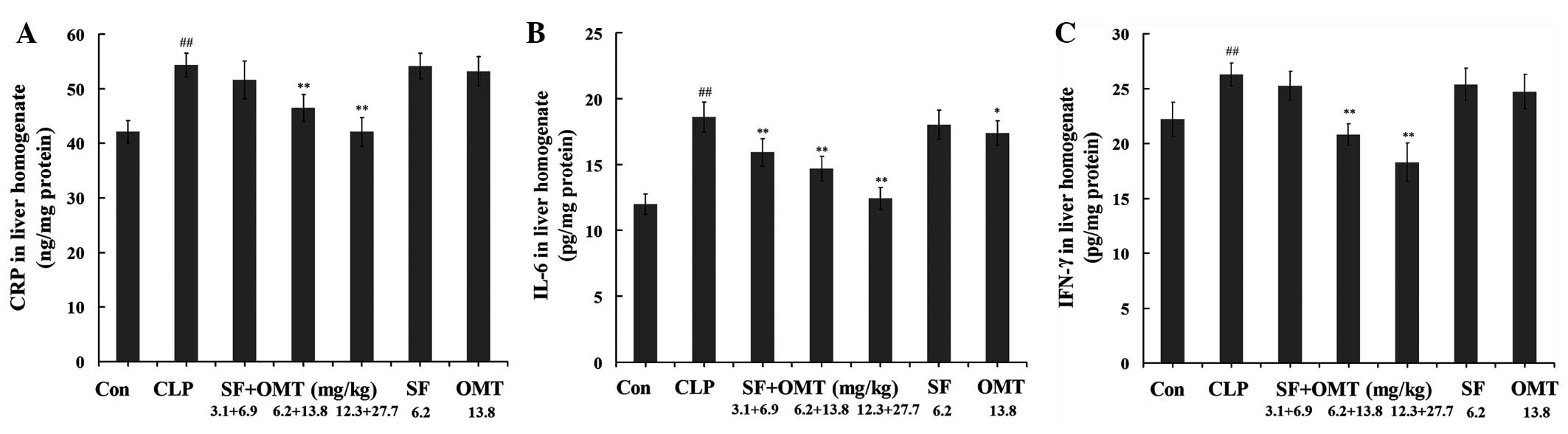
Effects of SF and OMT used in combination
or alone on the levels of CRP, IL-6 and IFN-γ in the liver
homogenate
As shown in Fig. 6,
following the CLP surgery, the levels of CRP, IL-6 and IFN-γ in the
liver homogenate notably increased in the CLP group compared with
those in the control group. Treatment with the combination of SF
and OMT (SF + OMT 3.1+6.9, 6.2+13.8 and 12.3+27.7 mg/kg)
significantly reduced the levels of IL-6 compared with those in the
CLP group (P<0.01). The CRP and IFN-γ levels in the liver
homogenate were significantly decreased in the high and medium dose
groups of the combination treatment compared with those in the CLP
group (P<0.01). With the exception of the levels of IL-6 in the
liver homogenate, which reduced significantly (P<0.05) in the
OMT (13.8 mg/kg) group, the other measured indices did not exhibit
significant changes in the SF or OMT alone treatment groups
compared with the levels in the CLP group.
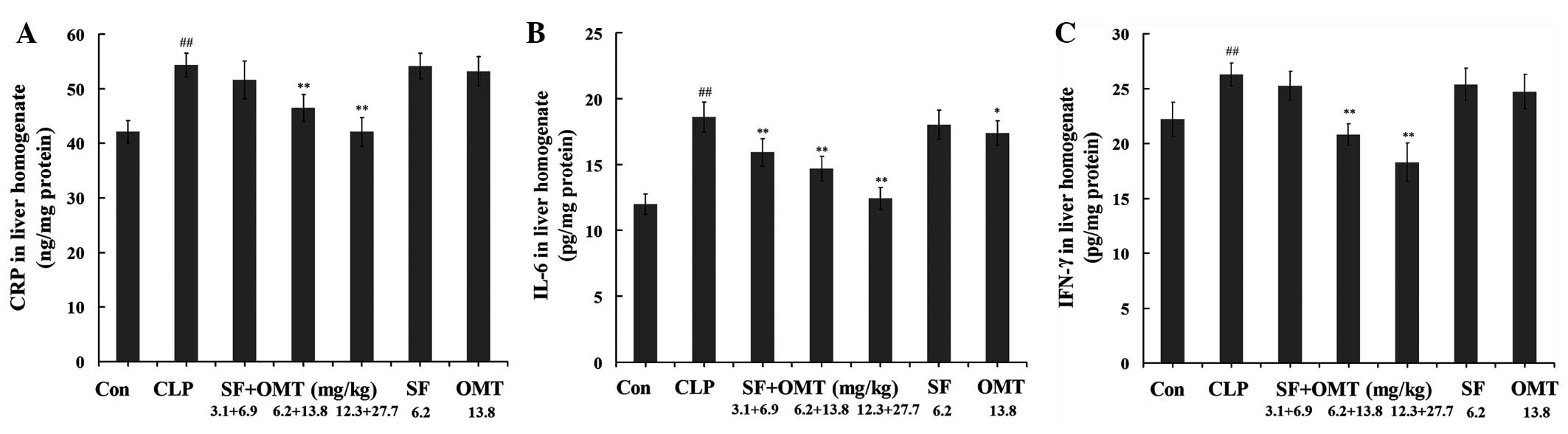 | Figure 6Effects of the combination of SF and
OMT on the levels of (A) CRP, (B) IL-6 and (C) IFN-γ in the liver
homogenates of CLP-induced septic mice. Con, CLP, SF and OMT
represent the control group, CLP group, SF (6.2 mg/kg) and OMT
(13.8 mg/kg) groups, respectively. SF + OMT represents the SF and
OMT combination groups. The data are expressed as the mean ±
standard error of the mean. n=10 in each group.
##P<0.01, versus the control group.
*P<0.05 and **P<0.01, versus the CLP
group. CRP, C-reactive protein; CLP, cecal ligation and puncture;
SF, sodium ferulate; OMT, oxymatrine; IL-6, interleukin-6; IFN-γ,
interferon-γ. |
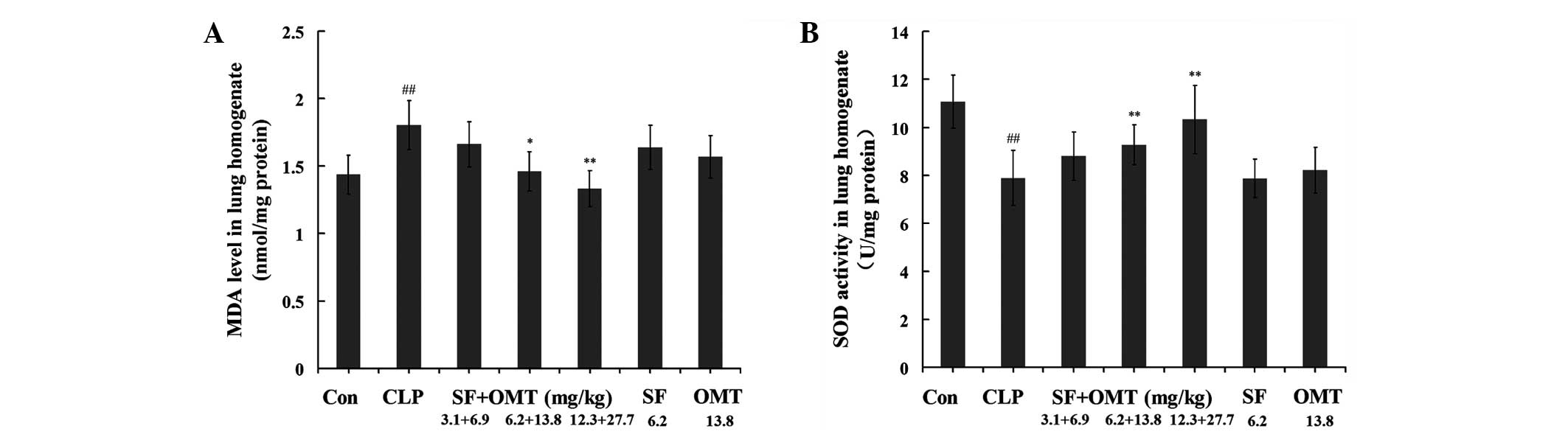
Effects of SF and OMT used in combination
or alone on the levels of MDA and SOD activity in the lung
homogenate
As shown in Fig. 7,
the CLP surgery resulted in a marked increase in the MDA levels and
reduction in the SOD activity levels in the lung homogenates of the
CLP group compared with those in the control group. Compared with
those in the CLP group, in the combination treatment groups the MDA
levels significantly decreased (P<0.05 in the medium dose group;
P<0.01 in the high dose group) and the SOD activity levels
increased (P<0.01 in the medium and high dose groups) in the
lung homogenate. In the groups treated with SF (6.2 mg/kg) or OMT
(13.8 mg/kg) alone, the MDA and SOD activity levels in the lung
homogenate did not exhibit significant changes compared with those
in the CLP group.
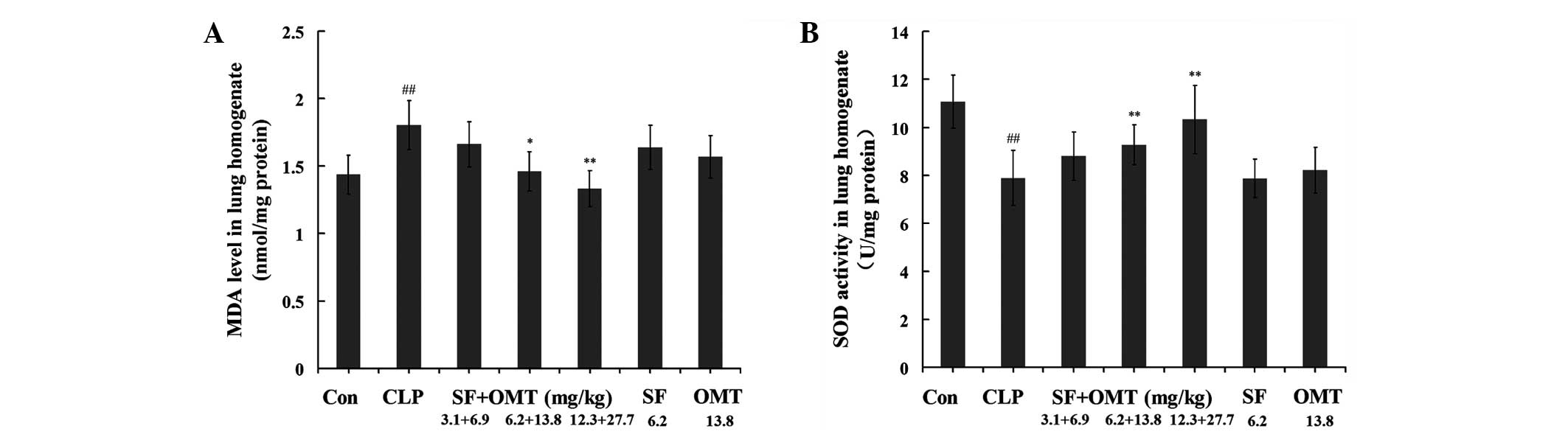 | Figure 7Effects of the combination of SF and
OMT on the levels of (A) MDA and (B) SOD activity in the lung
homogenates of CLP-induced septic mice. Con, CLP, SF and OMT
represent the control group, CLP group, SF (6.2 mg/kg) and OMT
(13.8 mg/kg) groups, respectively. SF + OMT represents the SF and
OMT combination groups. The data are expressed as the mean ±
standard error of the mean. n=10 in each group.
##P<0.01, versus the control group.
*P<0.05 and **P<0.01, versus the CLP
group. MDA, malondialdehyde; CLP, cecal ligation and puncture; SF,
sodium ferulate; OMT, oxymatrine; SOD, superoxidase dismutase. |
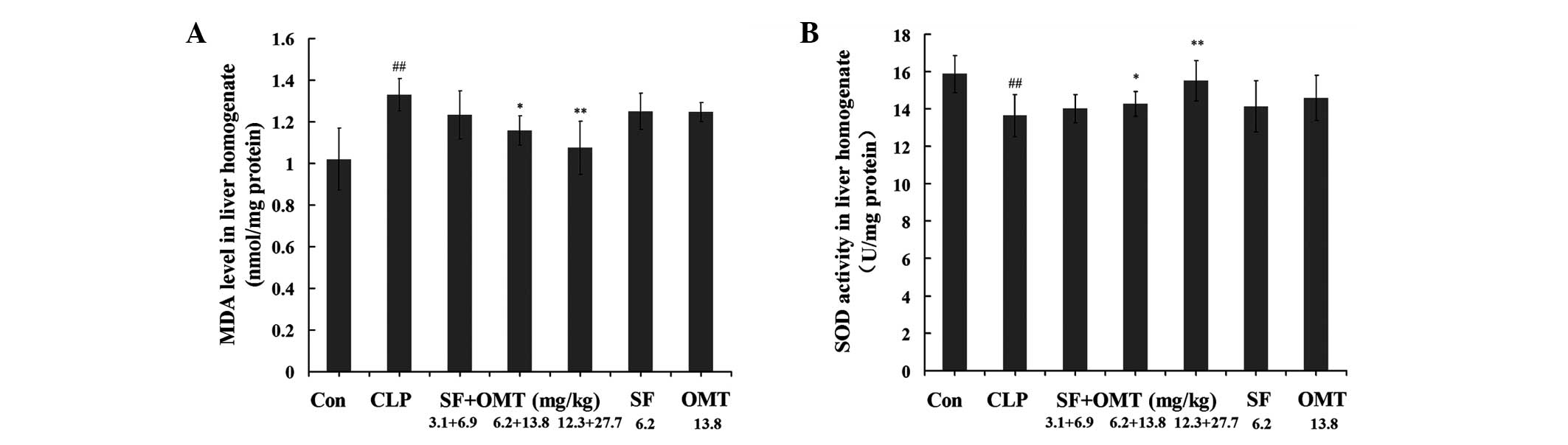
Effects of SF and OMT used in combination
or alone on the levels of MDA and SOD activity in the liver
homogenates
As shown in Fig. 8,
the CLP surgery resulted in a marked increase of the MDA levels and
reduction in the SOD activity levels in the liver homogenates in
the CLP group compared with those in the control group. Compared
with those of the CLP group, in the combination treatment groups
the MDA levels significantly decreased and the SOD activity levels
increased in a dose-dependent manner in the liver homogenate. In
the group treated with SF (6.2 mg/kg) or OMT (13.8 mg/kg) alone,
the MDA and SOD activity levels in the liver homogenate did not
exhibit significant differences compared with those in the CLP
group.
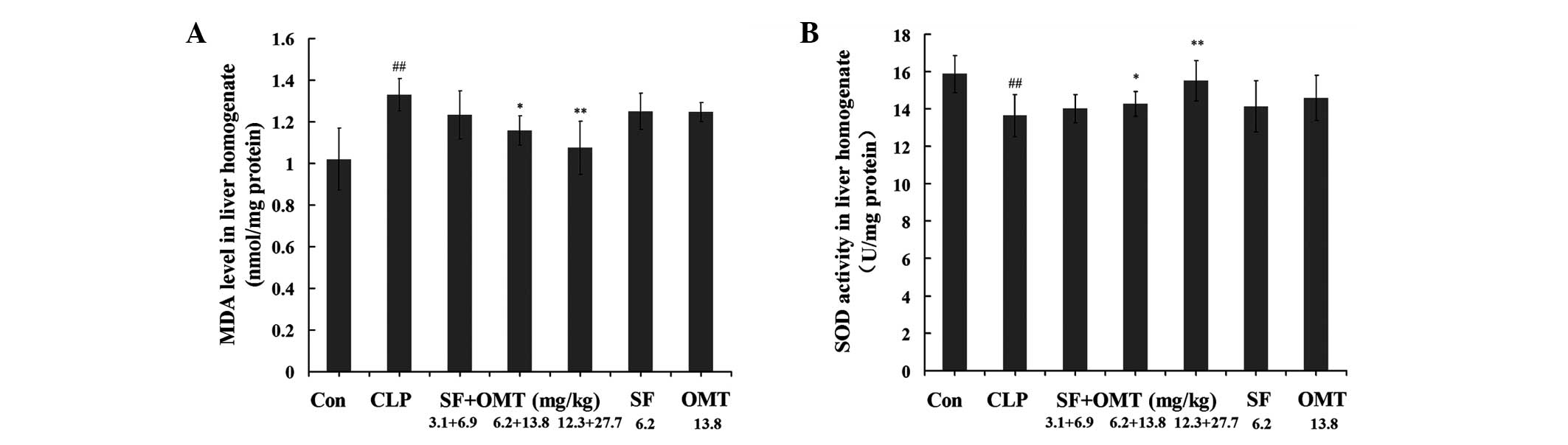 | Figure 8Effects of the combination of SF and
OMT on the levels of (A) MDA and (B) SOD activity in the liver
homogenates of CLP-induced septic mice. Con, CLP, SF and OMT
represent the control group, CLP group, SF (6.2 mg/kg) and OMT
(13.8 mg/kg) groups, respectively. SF + OMT represents the SF and
OMT combination groups. The data are expressed as the mean ±
standard error of the mean. n=10 in each group.
##P<0.01, versus the control group.
*P<0.05 and **P<0.01, versus the CLP
group. MDA, malondialdehyde; CLP, cecal ligation and puncture; SF,
sodium ferulate; OMT, oxymatrine; SOD, superoxidase dismutase. |
Effects of the combination of SF and OMT
on the bacterial load in the blood
After the CLP surgery (8 h), the bacterial load of
the blood was markedly increased compared with that in the control
group. Compared with that in the CLP group, no significant
difference in number of CFUs was detected in the combination
treatment groups (SF + OMT 3.1+6.9, 6.2+13.8 and 12.3+27.7 mg/kg),
or SF (6.2 mg/kg) and OMT (13.8 mg/kg) groups (P>0.05; data not
shown).
Discussion
SF, one of the active ingredients isolated from the
Chinese herb Radix Angelica sinensis (Oliv.) Diels, exerts
antioxidative, anti-inflammatory and platelet aggregation
inhibitory effects, and free radical-scavenging activities
(14,15). SF has been approved by the State
Food and Drugs Administration of China (Beijing, China) as a drug
for the clinical treatment of cardiovascular and cerebrovascular
diseases. OMT, a component of the Chinese herb Radix Sophora
flavescent Ait., has been widely used for the treatment of
chronic hepatitis in China, and its positive pharmacological
effects on the regulation of the immune reaction, reduction of
hypersensitive reactions and inhibition of histamine release have
been demonstrated by in vitro and in vivo studies
(16,17). Previous studies have shown that the
combination of SF and OMT has a synergistic anti-inflammatory
effect and may protect against lipopolysaccharide (LPS)-induced
lung injury (7). Therefore, the
present study used the CLP-induced model of sepsis to further
corroborate the anti-inflammatory effect of the combination of SF
and OMT and aimed to demonstrate its protective effect on
sepsis-induced organ injury.
Sepsis resulting from CLP in animals is an accepted
animal model that closely imitates the physiological changes
observed during the progression of sepsis in humans (18). This model has been shown to
accurately reproduce the sepsis sequelae with regard to the
hyperactive inflammatory process, generation of cytokines and
development of multiorgan failure that leads to mortality (19). Control of the extent of damage
resulting from cecum perforation may effectively control the
survival rate and survival time of mice. In the present study, none
of the animals died within 8 h after the CLP surgery, and of the
animals in the CLP group, 20% survived to the 16 h point and none
survived to the 24 h point. These results indicated that
CLP-induced sepsis was a suitable model to duplicate the
pathological process of acute inflammatory reactions and validate
the anti-inflammatory effect of the SF and OMT combination drug
treatment. Treatment with the combination of SF and OMT at the
medium and high doses significantly increased the survival rate and
prolonged the survival time of the mice with CLP-induced sepsis
effectively compared with those of the CLP-induced septic models
without treatment. These results supported our hypothesis
concerning the protective effect of the SF and OMT combination
treatment on CLP-induced sepsis.
Sepsis-induced multiple organ injury is the main
cause of septic shock and patient mortality, in which the lung is
the primary target organ and importantly, mortality is mainly
caused by irreversible lung injury, termed ‘shock lung’
(20). The water content of the
lung tissue, which represents the degree of lung injury, is
reflected by the lung W/D ratio. The serum ALT, AST and LDH levels
are biochemical markers for the extent of injury to the liver and
other organs and are easily measured using a routine automatic
analyzer. The increased levels of ALT, AST and LDH in serum
indicate the degree of organ injury (21,22).
Thus, following treatment with the combination of SF and OMT in the
present study, the notable reduction in the levels of ALT, AST and
LDH suggested that the cellular injury to the liver and other
organs induced by CLP was attenuated. These results exhibited the
protective effect of the combination of SF and OMT on CLP-induced
organ injury.
For modulation of a number of healing processes, the
important inflammatory mediators, including CRP, IL-6 and IFN-γ,
are rapidly induced in the early stage of the inflammatory
response. However, if overproduced, these mediators may exacerbate
the severity of multiple inflammatory diseases, particularly in
sepsis (23–26).
CRP is a type of reactive protein in the acute
inflammatory phase (27) and shows
a significant positive correlation with the extent of tissue
injury. As an indicator of the systemic inflammatory reaction, CRP
may exhibit proinflammatory effects by activating the complement
system and inducing the production of inflammatory cytokines and
tissue factor in monocytes (27,28).
CRP is a marker of inflammatory reaction and predicts the risk of
the occurrence of organ injury (29). IL-6 is an early inflammatory
mediator that is markedly upregulated in the serum of patients with
sepsis (30,31). As a proinflammatory cytokine
(32), IL-6 has numerous
biological features and plays an important role in the process of
inflammation (33). IFN-γ is a
potent proinflammatory cytokine and contributes to innate immunity.
IFN-γ is a risk factor for the occurrence of organ injury (34). A previous study showed that
following treatment with the combination of SF and OMT, the CRP,
IL-6 and IFN-γ genes were all synergistically downregulated in
LPS-stimulated RAW 264.7 cells (5). In order to confirm that the
anti-inflammatory effect of the combination of SF and OMT was
associated with the inflammatory cytokines, 10 mice in each group
of the present study were sacrificed and the levels of CRP, IL-6
and IFN-γ in serum, lung and liver homogenate were detected at 8 h
after the CLP surgery, at which point none of the animals had died.
It was detected that the levels of the inflammatory cytokines had
all increased markedly compared with those in the control group. As
the results showed, treatment with the combination of SF and OMT
significantly reduced the increased CRP, IL-6 and IFN-γ levels
induced by CLP in the serum, lung and liver homogenates. These
results were consistent with the reverse transcription-polymerase
chain reaction results published in a previous study (5) and further confirmed the
anti-inflammatory effect of the combination of SF and OMT involved
in the protective mechanism of the organs.
Sepsis is frequently associated with the generation
of a large number of free radicals and an excessive amount of free
radicals causes oxidative tissue injury, which is considered to
trigger the inflammatory response and contribute to organ injury
(35,36). One of histopathological causes of
sepsis is the overproduction of reactive oxygen species. MDA is
produced by lipid peroxidation inside cells. The MDA content of an
organism reflects the degree of lipid peroxidation (37). The MDA levels are a valuable
biomarker of oxidative injury in tissues and indirectly present the
degree of cellular injury (38,39).
SOD is an antioxidant enzyme that removes superoxide free radicals
and protects against cellular injury from free radicals (40). The enhancement of the oxidation
reaction is reflected by a reduction in the levels of SOD activity.
In the present study, the MDA levels in the lung and liver tissue
were markedly increased and the SOD activity levels were markedly
reduced by CLP, compared with those in the control group. However,
the increased MDA levels were significantly reduced and the
decreased SOD activity levels were significantly increased by the
medium and high doses of the combination SF and OMT treatment.
Thus, the results indicate that the combination treatment
alleviates the extent of the oxidative injury in the lung and liver
tissues. These results were in accordance with those of a previous
study (7), and indicated that the
combination treatment significantly attenuates the LPS-induced
reduction in the levels of SOD activity.
These observations suggest that the bacterial load
may increase due to the anti-inflammatory effect of SF and OMT.
Thus, in the present study the bacterial load in mice of all groups
was detected. No significant differences were observed between the
bacterial load of the CLP group and those of the groups treated
with a combination of SF and OMT or the drugs alone at 8 h after
the CLP surgery. This suggested that treatment with the combination
of SF and OMT did not increase the bacterial load in the early
stage of the inflammatory response. In an in vitro
experiment conducted by authors of the present study, it was
demonstrated that following treatment with the combination of SF
and OMT, neither an antibiotic effect on certain Gram-positive and
Gram-negative bacteria, nor an effect on the antibiotic effect of
penicillin and streptomycin (data not shown) were observed.
The elucidation of the anti-inflammatory effect of
the combination of SF and OMT is likely to provide potential
therapeutic approaches, for example the combination treatment may
be a substitute for the corticosteroid drugs used to treat sepsis.
To achieve this goal, further studies should be conducted, with the
aim of exploring whether the combination of SF and OMT treatment
influences the defense system of the body and its superior
advantage compared with corticosteroid drugs. The present study
only suggested that an anti-inflammatory strategy had a significant
therapeutic effect in the early stage of a serious inflammatory
disease, and that alleviation of the inflammatory response is
likely to be beneficial for organ protection, as it would provide
the time for recovery of patients. Beyond all question, antibiotic
therapy should be the first-line strategy for the treatment of
serious infectious disease.
In order to further test the synergistic
anti-inflammatory effect of the combination of SF and OMT in the
present study, SF and OMT treatment alone groups were designed as
further control groups. When used in the same doses as those in the
medium dose combination treatment group, no clear anti-inflammatory
or antioxidative effects were observed in the mice treated with SF
or OMT alone, with the exception of a slight improvement in the
IL-6 levels. These results indirectly provided more data further
confirming the synergistic effect of the SF and OMT combination
treatment. Detailed data analyzing the synergistic effect of the
combination of SF and OMT have been published in a previous study
(5,7). Also, data regarding the optimization
of the dose ratio of SF and OMT may be reported by the authors of
the present study in the future.
In conclusion, the combination of SF and OMT had
protective effects against CLP-induced sepsis in mice. The possible
mechanisms of these effects may be associated with the alleviation
of systemic inflammation, including reductions in IL-6, CRP and
IFN-γ levels, and the diminishment of oxidative injury.
Acknowledgements
The authors thank Dr Peter Zhang of Medi Alliance
Inc. (King of Prussia, PA, USA) for his valuable comments and Dr
Yujun Li for the histopathological analysis.
References
|
1
|
Mokart D, Capo C, Blache JL, Delpero JR,
Houvenaeghel G, Martin C and Mege JL: Early postoperative
compensatory anti-inflammatory response syndrome is associated with
septic complications after major surgical trauma in patients with
cancer. Br J Surg. 89:1450–1456. 2002. View Article : Google Scholar
|
|
2
|
Bollaert PE, Charpentier C, Levy B,
Debouverie M, Audibert G and Larcan A: Reversal of late septic
shock with supraphysiologic doses of hydrocortisone. Crit Care Med.
26:645–650. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Baddour LM, Yu VL, Klugman KP, et al;
International Pneumococcal Study Group. Combination antibiotic
therapy lowers mortality among severely ill patients with
pneumococcal bacteremia. Am J Respir Crit Care Med. 170:440–444.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Schlichting D and McCollam JS: Recognizing
and managing severe sepsis: a common and deadly threat. South Med
J. 100:594–600. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Yuan X, Sun Y, Miao N, et al: The
synergistic anti-inflammatory effect of the combination of sodium
ferulate and oxymatrine and its modulation on
inflammation-associated mediators in RAW 264.7 cells. J
Ethnopharmacol. 137:1477–1485. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Liu H, Sun Y, Gao Y, Chen F, Xu M and Liu
Z: The analgesic effect and mechanism of the combination of sodium
ferulate and oxymatrine. Neurochem Res. 35:1368–1375. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Yuan X, Wang Y, Du D, Hu Z, Xu M, Xu M and
Liu Z: The effects of the combination of sodium ferulate and
oxymatrine on lipopolysaccharide-induced acute lung injury in mice.
Inflammation. 35:1161–1168. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Baker CC, Chaudry IH, Gaines HO and Baue
AE: Evaluation of factors affecting mortality rate after sepsis in
a murine cecal ligation and puncture model. Surgery. 94:331–335.
1983.PubMed/NCBI
|
|
9
|
Standage SW, Caldwell CC, Zingarelli B and
Wong HR: Reduced peroxisome proliferator-activated receptor α
expression is associated with decreased survival and increased
tissue bacterial load in sepsis. Shock. 37:164–169. 2012.
|
|
10
|
Elstner EF and Heupel A: Inhibition of
nitrite formation from hydroxylammoniumchloride: a simple assay for
superoxide dismutase. Anal Biochem. 70:616–620. 1976. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ohkawa H, Ohishi N and Yagi K: Assay for
lipid peroxides in animal tissues by thiobarbituric acid reaction.
Anal Biochem. 95:351–358. 1979. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Li Y, Huang Y, Piao Y, Nagaoka K, Watanabe
G, Taya K and Li C: Protective effects of nuclear factor erythroid
2-related factor 2 on whole body heat stress-induced oxidative
damage in the mouse testis. Reprod Biol Endocrinol. 11:232013.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wei Q, Ren X, Jiang Y, Jin H, Liu N and Li
J: Advanced glycation end products accelerate rat vascular
calcification through RAGE/oxidative stress. BMC Cardiovasc Disord.
13:132013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wang BH and Ou-Yang JP: Pharmacological
actions of sodium ferulate in cardiovascular system. Cardiovascuar
Drug Rev. 23:161–172. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Srinivasan M, Sudheer AR and Menon VP:
Ferulic acid: therapeutic potential through its antioxidant
property. J Clin Biochem Nutr. 40:92–100. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Chen XS, Wang GJ, Cai X, et al: Inhibition
of hepatitis B virus by oxymatrine in vivo. World J Gastroenterol.
7:49–52. 2001.PubMed/NCBI
|
|
17
|
Xu GL, Yao L, Rao SY, Gong ZN, Zhang SQ
and Yu SQ: Attenuation of acute lung injury in mice by oxymatrine
is associated with inhibition of phosphorylated p53
mitogen-activated protein kinase. J Ethnopharmacol. 98:177–183.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Brooks HF, Osabutey CK, Moss RF, Andrews
PL and Davies DC: Caecal ligation and puncture in the rat mimics
the pathophysiological changes in human sepsis and causes
multiorgan dysfunction. Metab Brain Dis. 22:353–373. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Remick D, Manohar P, Bolgos G, Rodriguez
J, Moldawer L and Wollenberg G: Blockade of tumor necrosis factor
reduces lipopolysacharide lethality, but not the lethality of cecal
ligation and puncture. Shock. 4:89–95. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kosaka J, Morimatsu H, Takahashi T, et al:
Effects of biliverdin administration on acute lung injury induced
by hemorrhagic shock and resuscitation in rats. PLoS One.
8:e636062013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Shahshahani MM, Azizahari S, Soori T, et
al: Hepatotoxicity and liver enzyme alteration in patients with
immunobullous diseases receiving immunosuppressive therapy. J
Dermatol. 38:1153–1157. 2011. View Article : Google Scholar
|
|
22
|
Singab AN, Youssef DT, Noaman E and Kotb
S: Hepatoprotective effect of flavonol glycosides rich fraction
from Egyptian Vicia calcarata Desf. against
CCl4-induced liver damage in rats. Arch Pharm Res.
28:791–798. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Márquez-Velasco R, Martínez-Velázquez AX,
Amezcua-Guerra LM, et al: Enhanced survival from CLP-induced sepsis
following late administration of low doses of anti-IFNγ F(ab’)2
antibody fragments. Inflamm Res. 60:947–953. 2011.PubMed/NCBI
|
|
24
|
Latifi SQ, O’Riordan MA, Levine AD and
Stallion A: Persistent elevation of serum interleukin-6 in
intraabdominal sepsis identifies those with prolonged length of
stay. J Pediatr Surg. 39:1548–1552. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Imamura T, Tanaka S, Yoshida H, et al:
Significance of measurement of high sensitivity C-reactive protein
in acute pancreatitis. J Gastroenterol. 37:935–938. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Memiş D, Gursoy O, Tasdogan M, et al: High
C-reactive protein and low cholesterol levels are prognostic
markers of survival in severe sepsis. J Clin Anesth. 19:186–191.
2007.PubMed/NCBI
|
|
27
|
Ballou SP and Lozanski G: Induction of
inflammatory cytokine release from cultured human monocytes by
C-reactive protein. Cytokine. 4:361–368. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Cermak J, Key NS, Bach RR, Balla J, Jacob
HS and Vercellotti GM: C-reactive protein induces human peripheral
blood monocytes to synthesize tissue factor. Blood. 82:513–520.
1993.PubMed/NCBI
|
|
29
|
Lausevic Z, Lausevic M,
Trbojevic-Stankovic J, Krstic S and Stojimirovic B: Predicting
multiple organ failure in patients with severe trauma. Can J Surg.
51:97–102. 2008.PubMed/NCBI
|
|
30
|
Calandra T, Gerain J, Heumann D, et al:
High circulating levels of interleukin-6 in patients with septic
shock: Evolution during sepsis, prognostic value, and interplay
with other cytokines. The Swiss-Dutch J5 Immunoglobulin Study
Group. Am J Med. 91:23–29. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Gårdlund B, Sjölin J, Nilsson A, et al:
Plasma levels of cytokines in primary septic shock in humans:
correlation with disease severity. J Infect Dis. 172:296–301.
1995.PubMed/NCBI
|
|
32
|
Coyle P, Philcox JC and Rofe AM:
Metallothionein induction in cultured rat hepatocytes by arthritic
rat serum, activated macrophages, interleukin-6, interleukin-11 and
leukaemia inhibitory factor. Inflamm Res. 44:475–481. 1995.
View Article : Google Scholar
|
|
33
|
Tao JY, Zheng GH, Zhao L, et al:
Anti-inflammatory effects of ethyl acetate fraction from
Melilotus suaveolens Ledeb on LPS-stimulated RAW 264.7
cells. J Ethnopharmacol. 123:97–105. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
de Lima TH, Sass N, Mattar R, Moron AF,
Torloni MR, Franchim CS and Daher S: Cytokine gene polymorphisms in
preeclampsia and eclampsia. Hypertens Res. 32:565–569.
2009.PubMed/NCBI
|
|
35
|
Su F, Wang Z, Cai Y, Remmelink M and
Vincent JL: Beneficial effects of ethyl pyruvate in septic shock
from peritonitis. Arch Surg. 142:166–171. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Berg RM, Møller K and Bailey DM:
Neuro-oxidative-nitrosative stress in sepsis. J Cereb Blood Flow
Metab. 31:1532–1544. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Perše M, Injac R and Erman A: Oxidative
status and lipofuscin accumulation in urothelial cells of bladder
in aging mice. PLoS One. 8:e596382013.PubMed/NCBI
|
|
38
|
Gong WH, Zheng WX, Wang J, Chen SH, Pang
B, Hu XM and Cao XL: Coexistence of hyperlipidemia and acute
cerebral ischemia/reperfusion induces severe liver damage in a rat
model. World J Gastroenterol. 18:4934–4943. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Fakurazi S, Sharifudin SA and Arulselvan
P: Moringa oleifera hydroethanolic extracts effectively
alleviate acetaminophen-induced hepatotoxicity in experimental rats
through their antioxidant nature. Molecules. 17:8334–8350. 2012.
View Article : Google Scholar
|
|
40
|
Sunil C, Duraipandiyan V, Ignacimuthu S
and Al-Dhabi NA: Antioxidant, free radical scavenging and liver
protective effects of friedelin isolated from Azima
tetracantha Lam. leaves. Food Chem. 139:860–865. 2013.
View Article : Google Scholar : PubMed/NCBI
|