Introduction
The treatment of refractory chronic skin ulcers is
challenging due to the different causes and characteristics of the
wounds. Significant efforts have been made in the development of a
variety of treatment materials and processes where multiple factors
determine the drug used, including familiarity with the products,
characteristics of the patient and the cost (1,2).
Alginate is a natural anionic polymer typically extracted from
seaweed and has been investigated and used for numerous biomedical
applications. The advantages of alginate include biocompatibility,
low toxicity, relatively low cost and mild gelation when a divalent
cation such as Ca2+ is added (3). The structural similarity of alginate
to extracellular matrices of living tissues allows wide
applications in wound healing, delivery of bioactive agents
(including, small chemical drugs and proteins) and cell
transplantation. It has previously been verified that alginate
application alone does not facilitate wound healing compared with
other traditional methods (4),
however, alginate has been used in combination with other drugs or
protein factors for the treatment of wound healing (5–11).
Human granulocyte-macrophage colony stimulating
factor (hGM-CSF) is a multifunctional growth factor and a mitogenic
agent that has been demonstrated to be involved in a number of
essential processes of wound healing (12,13).
Recombinant hGM-CSF (rhGM-CSF) has been demonstrated to promote the
healing of infected burn wounds, as well as prevent infections by
modulating immune activity and improving immune competence
(14). The first use of
locally-delivered rhGM-CSF in chronic wounds was reported in 1994
(15). Clinical studies and case
reports have demonstrated that rhGM-CSF has a positive effect on
chronic wounds with varying etiologies, including chronic venous
ulcers, pressure ulcers, erythropathy-associated ulcers, neutrophil
dysfunction-associated chronic ulcers, immunodeficiency-associated
ulcers, leprosy ulcers and refractory wounds in patients with
cancer (12). However, it has
previously been demonstrated that rhGM-CSF does not have a
significant effect on healthy wounds (16).
In order to achieve optimal results, rhGM-CSF must
be continuously present in the wound at a certain concentration. In
the present study, the combined effect of alginate and rhGM-CSF on
the treatment of refractory chronic skin ulcers was investigated.
It was hypothesized that the combination of alginate and rhGM-CSF
significantly enhances wound healing compared with the treatment of
rhGM-CSF alone.
Patients and methods
Patients
A single center, three-arm, randomized clinical
study was performed. Patients with refractory chronic skin ulcers
were enrolled between October 2009 and March 2012 from Jinan
Central Hospital (Jinan, Shandong, China). The present study was
approved by the Ethics Committee of the Jinan Central Hospital and
written informed consent was obtained from every patient. Patients
with bedsores, varicose ulcers and diabetic foot ulcers, which
persisted for >1 month following conventional and
anti-inflammatory treatments, and with a wound area >10
cm2, were selected for the present study. Patients with
the following criteria were excluded from the present study: i)
fasting plasma glucose levels >10.0 mmol/l, even following
strict control; ii) patients with severe cardiac dysfunction
(≥level III), severe renal dysfunction (≥level II), as well as
severe diseases, including cancer, tuberculosis, chronic atrophic
gastritis and systemic lupus erythematosus.
Patients were randomly assigned to one of the
following three treatment groups: group A, alginate dressing plus
rhGM-CSF; group B, rhGM-CSF only; and group C, conventional
treatment group using a vaseline gauze.
Treatment
Following cleaning the wounds with saline and drying
them with sterile cotton, rhGM-CSF paste (Changchun Jinsai
Pharmaceutical Co., Ltd., Changchun, Jilin, China) containing 100
μg rhGM-CSF/10 g, covered by alginate dressing (Smith & Nephew,
London, UK) was applied over the wound area for patients in group
A. In group B, rhGM-CSF paste covered by a vaseline gauze was
applied to the wounds, whilst in group C only a vaseline gauze was
applied. The primary dressings were covered with cotton gauzes and
bandages and the dressings were changed daily for the first 7 days
and every other day thereafter.
Wound evaluation
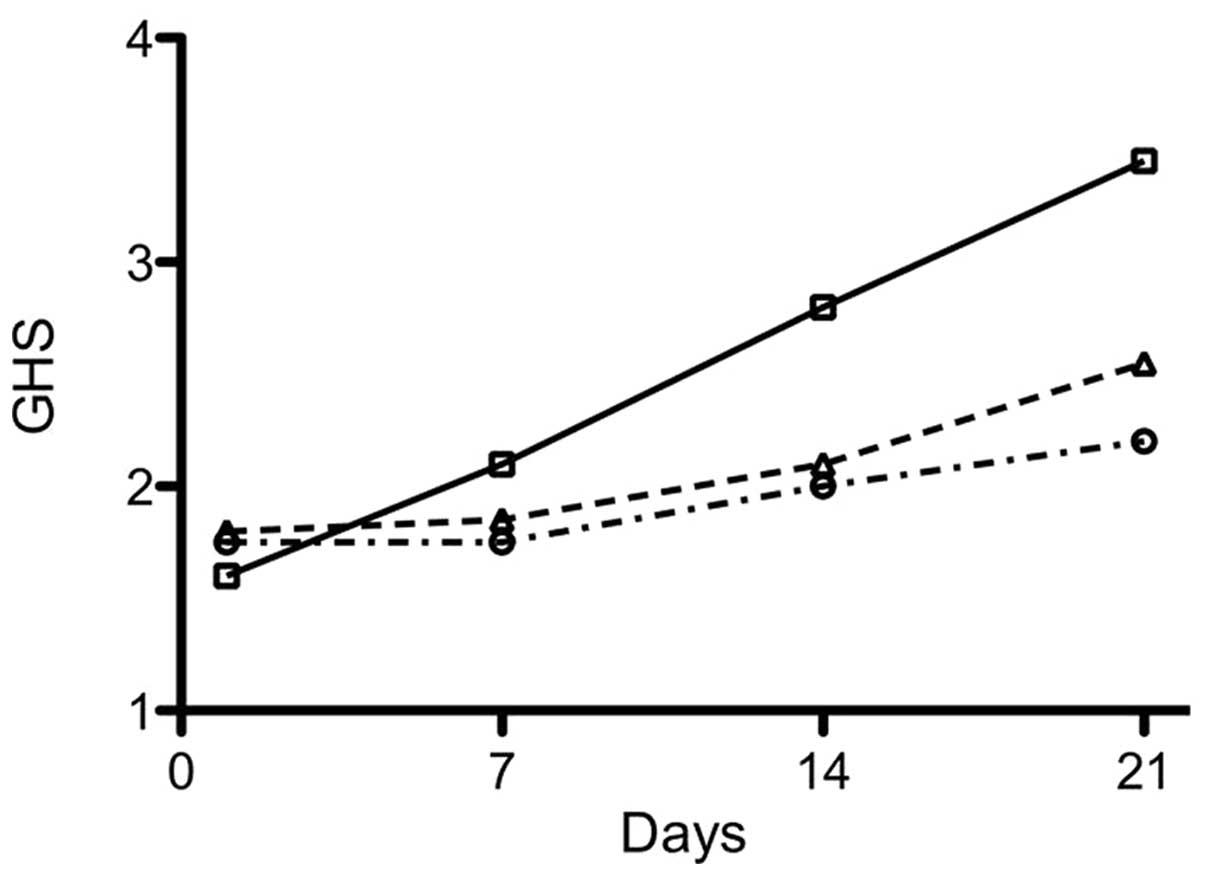
Visual observations were made on the wound color and
the growth of granulation. The physicians who performed the
evaluation were blinded to the treatment of the patients. The
evaluation criteria were determined and scored on a four-point
scale: 4 points, rosy colored wound surface and well-developed
granulation tissue; 3 points, pink wound surface with moderate
granulation tissue growth; 2 points, dark red wound surface with
light granulation tissue growth; and 1 point, pale wound surface
without granulation. The average scores for all the individuals in
each group were calculated and expressed as the group healing score
(GHS).
The wound area was measured and recorded each time
the dressing was changed. Healing was assessed as the percentage
area that was healed [(pre-treatment area - post-treatment
area)/pre-treatment area]. The ease with which the dressing was
removed was also assessed, whilst the patient scored the comfort of
the procedure. The dressing changes and treatment assessments were
performed by unbiased nurses.
Pain was assessed using the visual analogue scale
(VAS) method. A 10 cm linear score was used, where 0 indicated
painless and 10 indicated intolerable pain. Patients marked on the
line based on their pain intensity.
Statistical analysis
The data were analyzed using SPSS statistical
software (PASW statistics version 18.0; IBM, Armonk, NY, USA).
Differences in the outcome variables were analyzed on an
intention-to-treat basis. Differences in wound healing time between
the groups were examined using the Chi-square test. P<0.05 was
considered to indicate a statistically significant difference.
Results
Patient demography data and general
disease situation
A total of 60 patients were enrolled in the present
study, including 35 males and 25 females, aged between 20 and 75
years with an average age of 50.6. In total, 25 patients had
pressure sores, 15 had varicose ulcers and 20 had diabetic foot
ulcers. The ulcer area ranged between 11 and 35 cm2,
with an average size of 17.2±8.0 cm2. The duration of
the wound was 1–3.5 months, with an average time of 1.8±2.1 months
prior to the start of the study. Patients were randomly assigned
into one of the three treatment groups shown in Table I. Statistical analysis demonstrated
no significant difference between the patients in each treatment
group.
 | Table IDemographic data and medical history
of the patients. |
Table I
Demographic data and medical history
of the patients.
| Group | Number of
patients | Males/females | Age (years) | Wound duration
(months) | Pressure sores | Varicose ulcers | Diabetic foot | Ulcer area
(cm2) |
|---|
| A | 20 | 12/8 | 55.2±20.4 | 2.1±2.0 | 8 | 4 | 8 | 17.8±11.5 |
| B | 20 | 13/7 | 49.9±10.5 | 1.9±2.4 | 7 | 8 | 5 | 16.4±7.6 |
| C | 20 | 10/10 | 50.6±10.0 | 1.7±1.7 | 10 | 3 | 7 | 17.0±7.5 |
Visual observation
Pre-treatment assessment was performed on the first
day and was used as baseline for each patient. Observations were
routinely performed each time the dressing was changed by
physicians who were blinded to the treatment of the patients, and
the data are summarized in Table
II. An increase in granulation tissue growth and color changes
were observed at multiple time points in group A (alginate +
rhGM-CSF) and B (rhGM-CSF) compared with group C (vaseline only).
The GHS for each group was calculated and the results are shown in
Fig. 1. The differences between
the groups were found to be statistically significant (P<0.05;
Table II). The ease of changing
the dressing and the comfort of the patient were assessed and no
significant differences were identified among the three groups
(data not shown).
 | Table IIAssessment of wound color and
granulation at selected time points. |
Table II
Assessment of wound color and
granulation at selected time points.
| Group A | Group B | Group C |
|---|
|
|
|
|
|---|
| Time (days) | 1 | 2 | 3 | 4 | 1 | 2 | 3 | 4 | 1 | 2 | 3 | 4 |
|---|
| 1 | 11 | 6 | 3 | 0 | 9 | 9 | 2 | 0 | 8 | 9 | 3 | 0 |
| 7 | 7 | 6 | 5 | 2 | 7 | 10 | 2 | 1 | 7 | 11 | 2 | 0 |
| 14 | 2 | 5 | 8 | 5 | 5 | 9 | 5 | 1 | 5 | 10 | 5 | 0 |
| 21* | 0 | 2 | 11 | 8 | 3 | 6 | 8 | 3 | 5 | 8 | 5 | 2 |
Wound healing
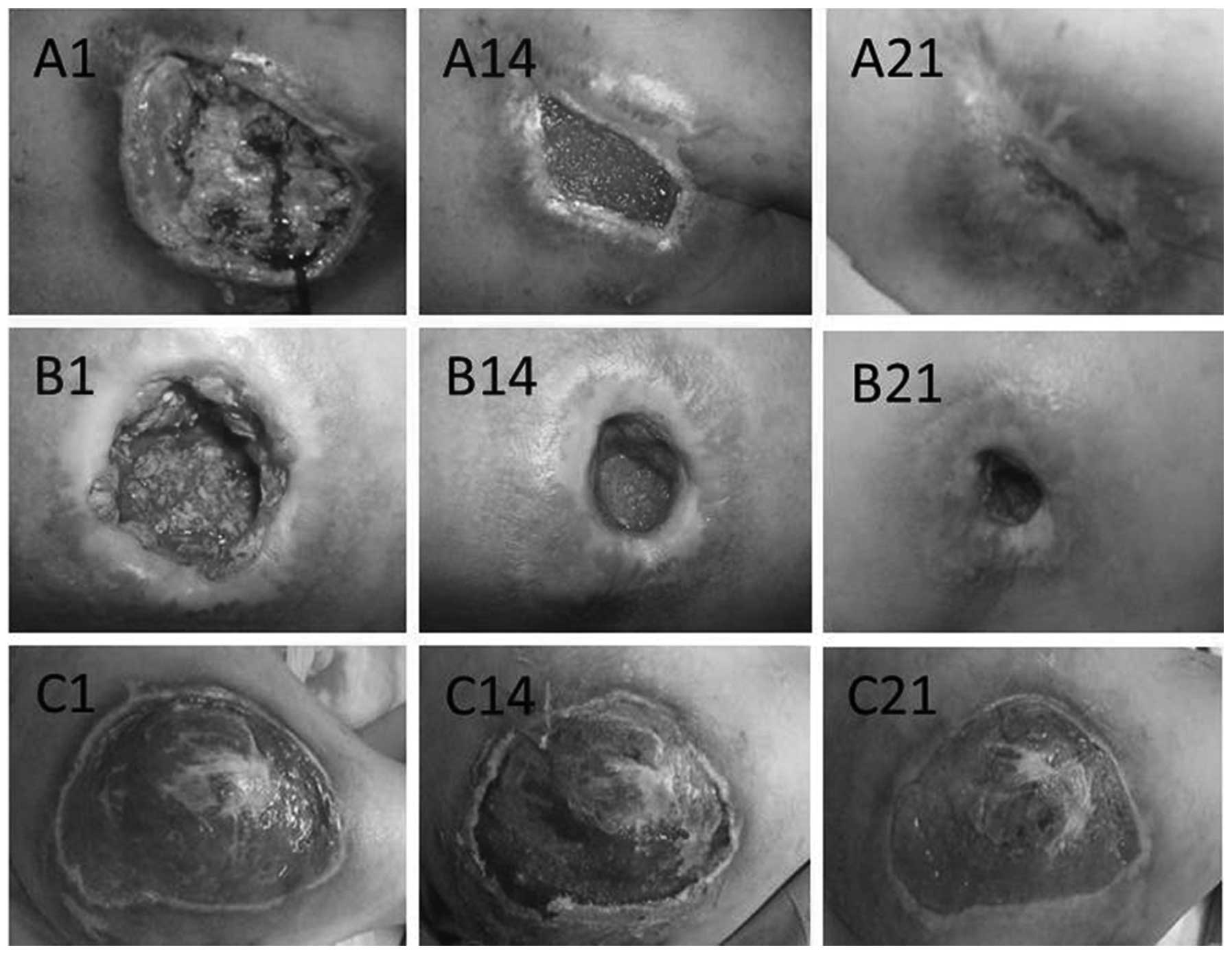
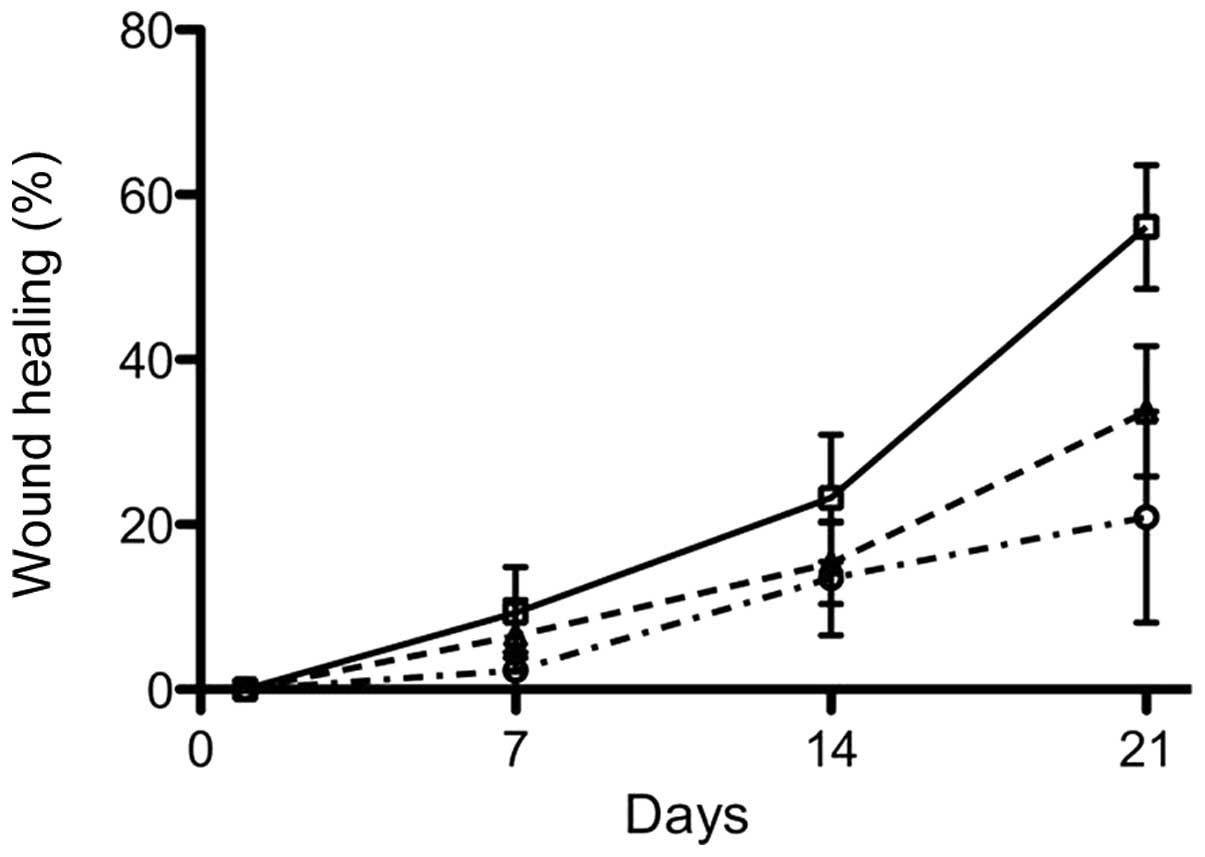
Representative cases from each group are shown in
Fig. 2 where differences between
the groups are illustrated. The wound healing rate was calculated
and the data demonstrated significant differences among the three
groups at all assessment time points. Following 3 weeks of
treatment, group A demonstrated the highest healing rate of 56%,
whilst group C and B had a healing rate of 21 and 34%, respectively
(Fig. 3). Following 7 days of
treatment, group A exhibited a rapid growth of fresh epithelium
towards the wound center and clear wound contraction and
re-epithelialization. Group B showed moderate wound contraction
compared with group A, however, this was significantly greater
compared with group C. The differences were statistically
significant among the three groups (P<0.05; Fig. 3).
Pain evaluation
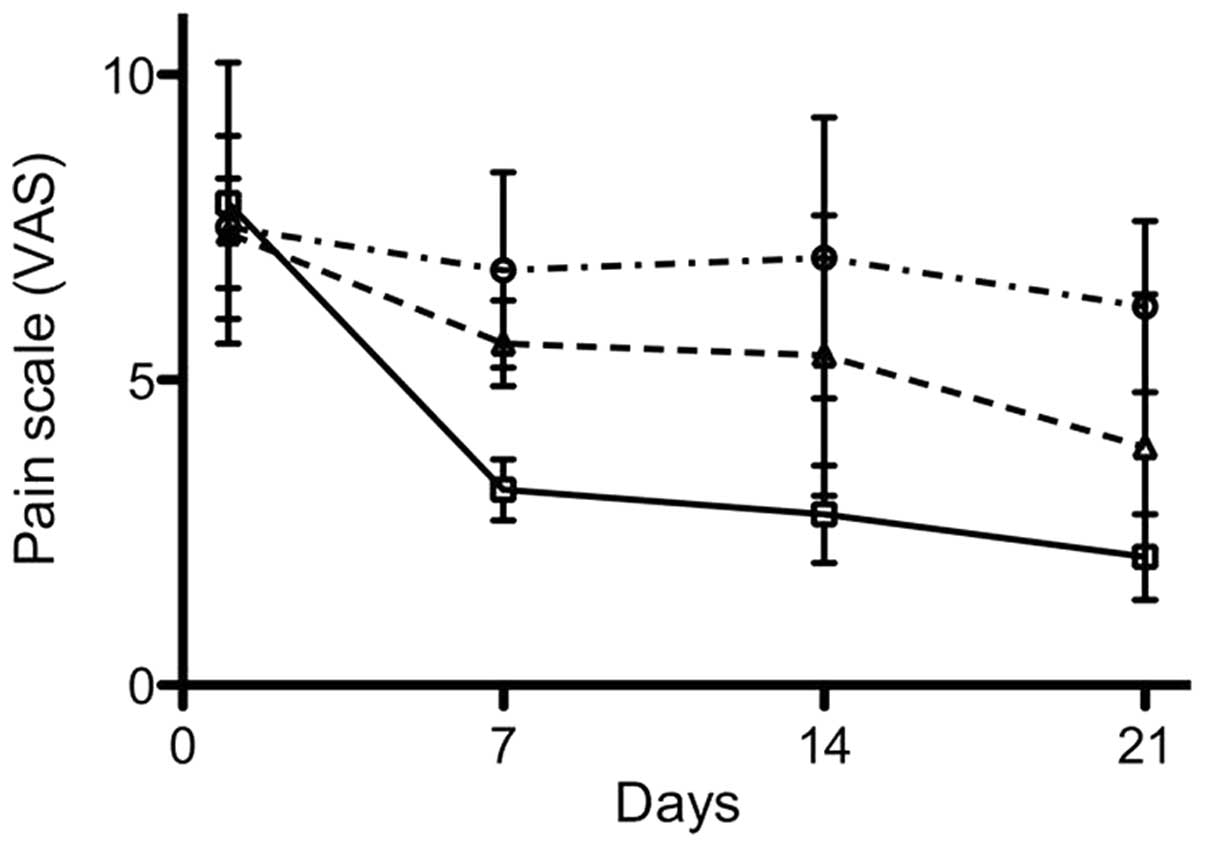
Wound pain was assessed using the VAS method on a 10
cm scale. Group A showed significantly reduced pain compared with
the other groups (Fig. 4), and the
differences among the three groups were statistically significant
(P<0.05).
Discussion
In the present study, the treatment of refractory
chronic skin ulcers using a combination therapy of rhGM-CSF with
sodium alginate was investigated. rhGM-CSF has been previously
demonstrated to be a mitotic-promoting reagent capable of promoting
wound healing. hGM-CSF was first used by da Costa et al
(15) to treat patients with
chronic refractory wounds on lower extremities and promising
results were observed. In a randomized, double-blind,
placebo-controlled trial on ulcers caused by varicose veins, it was
found that hGM-CSF treatment was significantly improved compared
with the placebo control treatment, and no adverse reactions were
observed. rhGM-CSF has also been demonstrated to be effective for
the treatment of refractory chronic wounds accompanied with
hereditary leukocyte dysfunction (17), post-surgical wounds (18) and hereditary neutrophil dysfunction
(19), as well as for the
treatment of pyoderma gangrenosum (16,20).
Alginate is used for the treatment of wounds as it
absorbs the exudate from the wound and exchanges
Na+/Ca2+ ions with the exudate, forming a gel
over the wound (21). Through the
ion exchange, insoluble calcium alginate is converted into soluble
sodium alginate. Soluble sodium alginate is capable of absorbing a
20-fold amount of its own weight of exudate (gauze absorbs 5–7
times) and forms a soft, moist, semi-solid gel-like substance, in
order to keep the wound isolated from infection or further harm. It
is known that wound healing occurs more rapidly when a gel is
formed at the wound surface and dehydration is prevented (22). Besides maintaining a moist
environment, alginate dressings possess other characteristics that
are beneficial for wound healing, including good permeability, a
lack of toxicity, stimulation and antigenicity, the ability to
prevent bleeding and promote clotting as well as the ability to
reduce water, salt and nutrient loss from the wound surface and
inhibit the growth of bacteria (23). The alginate gel also accelerates
microvessel hyperplasia and promotes granulation tissue formation
and rapid epithelialization (24).
Therefore, alginate has been widely used in various medical
conditions (25,26), even though alginate alone does not
directly enhance the wound healing process (4). The data from the present study
suggested that the combined use of alginate and rhGM-CSF reduced
the wound healing time and significantly decreased the discomfort
of the healing process. This suggests that alginate may be able to
create an improved environment so that rhGM-CSF is able to reach
its maximum effect.
Several previous studies have been performed using
rhGM-CSF with intradermal or subcutaneous injection around the
wound (20,27–31).
However, there are clear disadvantages caused by the injection,
including pain and uneven distribution of rhGM-CSF in the wound
area, which has prevented it from being widely used. Topical
application of rhGM-CSF is likely to cause loss of rhGM-CSF due to
dilution with the wound secretions. Therefore, the soft gel formed
by alginate is the ideal material to prevent this from happening.
In addition, the gel enables the continuous presence of rhGM-CSF on
the wound surface for a longer length of time, which accelerates
healing and reduces the quantity of rhGM-CSF applied to the wound
surface. Therefore, the combination of alginate dressings with
rhGM-CSF is theoretically superior to treatment with rhGM-CSF
alone, and the results from the present study support this
theory.
In the present study, patients with pressure sores,
varicose ulcers and diabetic foot ulcers were enrolled, and each
patient was randomly assigned to each group. However, statistical
analysis to assess the differences based on the type of wound was
not performed due to the limited number of cases. The results from
the present study would have been more conclusive if patients with
only one medical condition were selected. In addition, due to
certain technical reasons the wound depth was not measured and
instead the wound area was used as the sole standard for wound
healing evaluation. Thus, further studies are required to validate
the results from the present study.
In conclusion, the present study demonstrated that
alginate-rhGM-CSF dressing for refractory chronic skin ulcers
promoted the growth of granulation tissue, accelerated
re-epithelialization, whilst also effectively reducing wound pain.
These results suggest that the combination of the two may be used
for the routine treatment of refractory chronic skin ulcers.
Acknowledgements
This study was supported by the Jinan City 2009
Technology Development Program (grant no. 200918002). The authors
would like to thank Dr Sean Liu for reviewing the study.
References
|
1
|
Barnard J and Millner R: A review of
topical hemostatic agents for use in cardiac surgery. Ann Thorac
Surg. 88:1377–1383. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Niemi T, Svartling N, Syrjälä M,
Asko-Seljavaara S and Rosenberg P: Haemostatic disturbances in
burned patients during early excision and skin grafting. Blood
Coagul Fibrinolysis. 9:19–28. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wee S and Gombotz WR: Protein release from
alginate matrices. Adv Drug Deliv Rev. 31:267–285. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Groenewold MD, Gribnau AJ and Ubbink DT:
Topical haemostatic agents for skin wounds: a systematic review.
BMC Surg. 11:152011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Rabbany SY, Pastore J, Yamamoto M, Miller
T, Rafii S, Aras R and Penn M: Continuous delivery of stromal
cell-derived factor-1 from alginate scaffolds accelerates wound
healing. Cell Transplant. 19:399–408. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kolambkar YM, Dupont KM, Boerckel JD,
Huebsch N, Mooney DJ, Hutmacher DW and Guldberg RE: An
alginate-based hybrid system for growth factor delivery in the
functional repair of large bone defects. Biomaterials. 32:65–74.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lee KY, Peters MC and Mooney DJ:
Comparison of vascular endothelial growth factor and basic
fibroblast growth factor on angiogenesis in SCID mice. J Control
Release. 87:49–56. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Silva EA and Mooney DJ: Effects of VEGF
temporal and spatial presentation on angiogenesis. Biomaterials.
31:1235–1241. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Agren MS: Zinc in wound repair. Arch
Dermatol. 135:1273–1274. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Murakami K, Aoki H, Nakamura S, Takikawa
M, Hanzawa M, Kishimoto S, Hattori H, Tanaka Y, Kiyosawa T, Sato Y
and Ishihara M: Hydrogel blends of chitin/chitosan, fucoidan and
alginate as healing-impaired wound dressings. Biomaterials.
31:83–90. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wiegand C, Heinze T and Hipler UC:
Comparative in vitro study on cytotoxicity, antimicrobial activity,
and binding capacity for pathophysiological factors in chronic
wounds of alginate and silver-containing alginate. Wound Repair
Regen. 17:511–521. 2009. View Article : Google Scholar
|
|
12
|
Hu X, Sun H, Han C, Wang X and Yu W:
Topically applied rhGM-CSF for the wound healing: a systematic
review. Burns. 37:729–741. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Mann A, Breuhahn K, Schirmacher P and
Blessing M: Keratinocyte-derived granulocyte-macrophage colony
stimulating factor accelerates wound healing: Stimulation of
keratinocyte proliferation, granulation tissue formation, and
vascularization. J Invest Dermatol. 117:1382–1390. 2001. View Article : Google Scholar
|
|
14
|
Zhang L, Chen J and Han C: A multicenter
clinical trial of recombinant human GM-CSF hydrogel for the
treatment of deep second-degree burns. Wound Repair Regen.
17:685–689. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
da Costa RM, Aniceto C, Jesus FM and
Mendes M: Quick healing of leg ulcers after molgramostim. Lancet.
344:481–482. 1994.PubMed/NCBI
|
|
16
|
Ure I, Partsch B, Wolff K and Petzelbauer
P: Granulocyte/macrophage colony-stimulating factor increases
wound-fluid interleukin 8 in normal subjects but does not
accelerate wound healing. Br J Dermatol. 138:277–282. 1998.
View Article : Google Scholar
|
|
17
|
De Ugarte DA, Roberts RL, Lerdluedeeporn
P, Stiehm ER and Atkinson JB: Treatment of chronic wounds by local
delivery of granulocyte-macrophage colony-stimulating factor in
patients with neutrophil dysfunction. Pediatr Surg Int. 18:517–520.
2002.PubMed/NCBI
|
|
18
|
Jorgensen LN, Agren MS, Madsen SM,
Kallehave F, Vossoughi F, Rasmussen A and Gottrup F: Dose-dependent
impairment of collagen deposition by topical granulocyte-macrophage
colony-stimulating factor in human experimental wounds. Ann Surg.
236:684–692. 2002. View Article : Google Scholar
|
|
19
|
Breuhahn K, Mann A, Müller G, Wilhelmi A,
Schirmacher P, Enk A and Blessing M: Epidermal overexpression of
granulocyte-macrophage colony-stimulating factor induces both
keratinocyte proliferation and apoptosis. Cell Growth Differ.
11:111–121. 2000.
|
|
20
|
Jaschke E, Zabernigg A and Gattringer C:
Recombinant human granulocyte-macrophage colony-stimulating factor
applied locally in low doses enhances healing and prevents
recurrence of chronic venous ulcers. Int J Dermatol. 38:380–386.
1999. View Article : Google Scholar
|
|
21
|
Queen D, Orsted H, Sanada H and Sussman G:
A dressing history. Int Wound J. 1:59–77. 2004. View Article : Google Scholar
|
|
22
|
Winter GD: Formation of the scab and the
rate of epithelization of superficial wounds in the skin of the
young domestic pig. Nature. 193:293–294. 1962. View Article : Google Scholar
|
|
23
|
Yang Y, Wang J and Zhu L: Alginate
dressing application in plastic surgery. Journal of Chinese and
Western Medicine. 5:108–111. 2010.
|
|
24
|
Balakrishnan B, Mohanty M, Fernandez AC,
Mohanan PV and Jayakrishnan A: Evaluation of the effect of
incorporation of dibutyryl cyclic adenosine monophosphate in an in
situ-forming hydrogel wound dressing based on oxidized alginate and
gelatin. Biomaterials. 27:1355–1361. 2006. View Article : Google Scholar
|
|
25
|
Huang C, Wen X and Li G: Efficacy
observation and nursing for decubitus treated with Alginate
dressing. Modern Medicine & Health. 23:22007.
|
|
26
|
Ye Q and Chen J: Alginate dressing
application for skin graft on donor site. Zhejiang Medicine.
23:52001.
|
|
27
|
Da Costa RM, Ribeiro Jesus FM, Aniceto C
and Mendes M: Randomized, double-blind, placebo-controlled,
dose-ranging study of granulocyte-macrophage colony stimulating
factor in patients with chronic venous leg ulcers. Wound Repair
Regen. 7:17–25. 1999.PubMed/NCBI
|
|
28
|
Du S, Li Y, Mao Y, Sang X, Lu X, Wang W,
Zhang Q, Xue H, Yang X, Li S, Chi T, Zhong S and Huang J: Diagnosis
and treatment of hepatic angiomyolipoma. Hepatobiliary Surg Nutr.
1:19–24. 2012.
|
|
29
|
Kaplan G, Walsh G, Guido LS, Meyn P,
Burkhardt RA, Abalos RM, Barker J, Frindt PA, Fajardo TT and Celona
R: Novel responses of human skin to intradermal recombinant
granulocyte/macrophage-colony-stimulating factor: Langerhans cell
recruitment, keratinocyte growth, and enhanced wound healing. J Exp
Med. 175:1717–1728. 1992. View Article : Google Scholar
|
|
30
|
Siddiqui FH, Mokhashi MH and Boathman A:
Recombinant granulocyte-macrophage colony-stimulating factor in the
treatment of indolent ulcers with Klippel-Trenaunay-Weber syndrome:
a case report. J Pediatr Surg. 42:558–560. 2007. View Article : Google Scholar
|
|
31
|
Tursen U, Api H, Kaya TI, Cinel L and
Ikizoglu G: Rapid healing of chronic leg ulcers during perilesional
injections of granulocyte-macrophage colony-stimulating factor
therapy in a patient with cutaneous polyarteritis nodosa. J Eur
Acad Dermatol Venereol. 20:1341–1343. 2006. View Article : Google Scholar
|