Spandidos Publications style
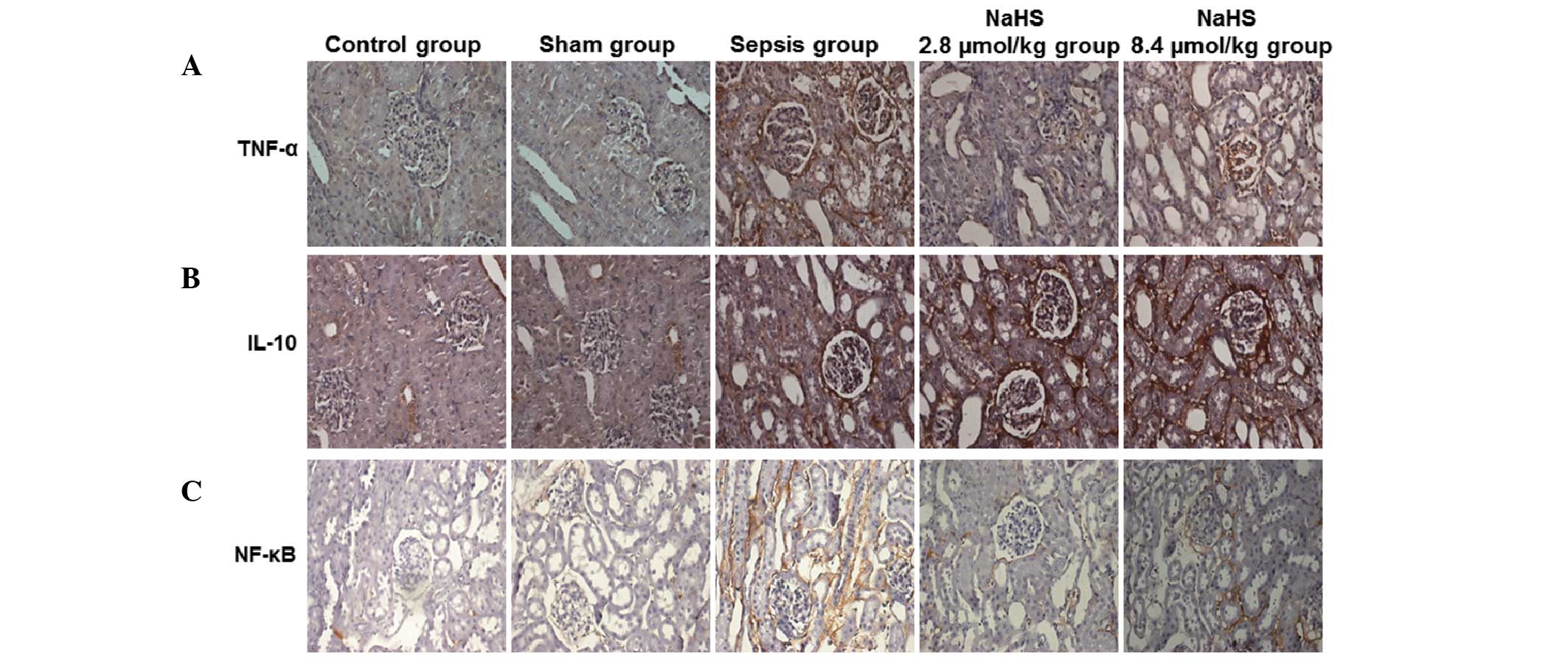
Chen X, Xu W, Wang Y, Luo H, Quan S, Zhou J, Yang N, Zhang T, Wu L, Liu J, Liu J, et al: Hydrogen sulfide reduces kidney injury due to urinary‑derived sepsis by inhibiting NF-κB expression, decreasing TNF-α levels and increasing IL-10 levels. Exp Ther Med 8: 464-470, 2014.
APA
Chen, X., Xu, W., Wang, Y., Luo, H., Quan, S., Zhou, J. ... Luo, Z. (2014). Hydrogen sulfide reduces kidney injury due to urinary‑derived sepsis by inhibiting NF-κB expression, decreasing TNF-α levels and increasing IL-10 levels. Experimental and Therapeutic Medicine, 8, 464-470. https://doi.org/10.3892/etm.2014.1781
MLA
Chen, X., Xu, W., Wang, Y., Luo, H., Quan, S., Zhou, J., Yang, N., Zhang, T., Wu, L., Liu, J., Long, X., Zhu, N., Xie, H., Luo, Z."Hydrogen sulfide reduces kidney injury due to urinary‑derived sepsis by inhibiting NF-κB expression, decreasing TNF-α levels and increasing IL-10 levels". Experimental and Therapeutic Medicine 8.2 (2014): 464-470.
Chicago
Chen, X., Xu, W., Wang, Y., Luo, H., Quan, S., Zhou, J., Yang, N., Zhang, T., Wu, L., Liu, J., Long, X., Zhu, N., Xie, H., Luo, Z."Hydrogen sulfide reduces kidney injury due to urinary‑derived sepsis by inhibiting NF-κB expression, decreasing TNF-α levels and increasing IL-10 levels". Experimental and Therapeutic Medicine 8, no. 2 (2014): 464-470. https://doi.org/10.3892/etm.2014.1781