|
1
|
Matta A, Tandra PK, Cichowski E and
Reddymasu SC: Acute necrotising pancreatitis: a late and fatal
complication of pancreaticoduodenal arterial embolisation. BMJ Case
Rep. bcr20142041972014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Rana SS, Sharma V, Sharma R and Bhasin DK:
An unusual complication of acute necrotising pancreatitis detected
by endoscopic ultrasound. JOP. 15:276–277. 2014.PubMed/NCBI
|
|
3
|
Ambiru S, Furuyama N, Aono M, et al:
Hyperbaric oxygen therapy for the treatment of postoperative
paralytic ileus and adhesive intestinal obstruction associated with
abdominal surgery: experience with 626 patients.
Hepatogastroenterology. 54:1925–1929. 2007.
|
|
4
|
Sheikh I, Fontenot E, Waghray N, et al:
The role of nonsteroidal anti-inflammatory drugs in the prevention
of post endoscopic retrograde cholangiopancreatography
pancreatitis. JOP. 15:219–224. 2014.PubMed/NCBI
|
|
5
|
Sit M, Aktas G, Yilmaz EE, et al: Effects
of the inflammatory response on serum omentin levels in early acute
and chronic pancreatitis. Clin Ter. 165:e148–e152. 2014.PubMed/NCBI
|
|
6
|
Shalimov SA, Popov ON, Dubitskiĭ AE and
Lifshits IuZ: Direct thermometry of the pancreas in the
postoperative period. Vestn Khir Im I I Grek. 132:36–39. 1984.(In
Russian). PubMed/NCBI
|
|
7
|
Mascolo N, Izzo AA, Ligresti A, et al: The
endocannabinoid system and the molecular basis of paralytic ileus
in mice. FASEB J. 16:1973–1975. 2002.PubMed/NCBI
|
|
8
|
Elder AS, Saccone GT, Bersten AD and Dixon
DL: Evaluation of lung injury and respiratory mechanics in a rat
model of acute pancreatitis complicated with endotoxin.
Pancreatology. 12:240–247. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Fujita T: Endotoxin as a trigger of
alcoholic pancreatitis. Gastroenterology. 134:640–641. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Verma R, Dhamija R, Ross SC, Batts DH and
Loehrke ME: Symbiotic bacteria induced necrotizing pancreatitis.
JOP. 11:474–476. 2010.PubMed/NCBI
|
|
11
|
Zhang X, Tian H, Wu C, et al: Effect of
baicalin on inflammatory mediator levels and microcirculation
disturbance in rats with severe acute pancreatitis. Pancreas.
38:732–738. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Cuthbertson CM and Christophi C:
Disturbances of the microcirculation in acute pancreatitis. Br J
Surg. 93:518–530. 2006. View
Article : Google Scholar : PubMed/NCBI
|
|
13
|
Yang XN, Guo J, Lin ZQ, et al: The study
on causes of death in fulminant pancreatitis at early stage and
late stage. Sichuan Da Xue Xue Bao Yi Xue Ban. 42:686–690. 2011.(In
Chinese). PubMed/NCBI
|
|
14
|
Yuan Z, Meyerholz DK, Twait EC, et al:
Systemic inflammation with multiorgan dysfunction is the cause of
death in murine ligation-induced acute pancreatitis. J Gastrointest
Surg. 15:1670–1678. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Tsuji Y, Takahashi N, Fletcher JG, et al:
Subtraction color map of contrast-enhanced and unenhanced CT for
the prediction of pancreatic necrosis in early stage of acute
pancreatitis. AJR Am J Roentgenol. 202:W349–W356. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Garip G, Sarandöl E and Kaya E: Effects of
disease severity and necrosis on pancreatic dysfunction after acute
pancreatitis. World J Gastroenterol. 19:8065–8070. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Popa D: Treatment in severe acute
pancreatitis - still a reason of debate. J Med Life. 6:486–490.
2013.
|
|
18
|
Ge HY and Chen B: Clinical observation of
acute pancreatitis treated with acupoint application combined with
medicine. Zhongguo Zhen Jiu. 32:602–604. 2012.(In Chinese).
PubMed/NCBI
|
|
19
|
Bossi A, Romeo G and Pezzoli A:
Side-effects, structure, and H2-receptor antagonists. Lancet.
339:13661992. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Xia Q and Deng LH: Hot issues on the
treatment of severe acute pancreatitis by integrated traditional
Chinese and Western medicine. Sichuan Da Xue Xue Bao Yi Xue Ban.
44:962–965. 2013.(In Chinese).
|
|
21
|
Wan MH, Yao J, Li J, et al: The
effectiveness of purgation and electroacupuncture in extrahepatic
bile duct stone complicated with acute biliary pancreatitis:
management of biliary stone pancreatitis through traditional
Chinese medicine. Pancreas. 40:483–484. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Tang Y, Liao Y, Kawaguchi-Sakita N, et al:
Sinisan, a traditional Chinese medicine, attenuates experimental
chronic pancreatitis induced by trinitrobenzene sulfonic acid in
rats. J Hepatobiliary Pancreat Sci. 18:551–558. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
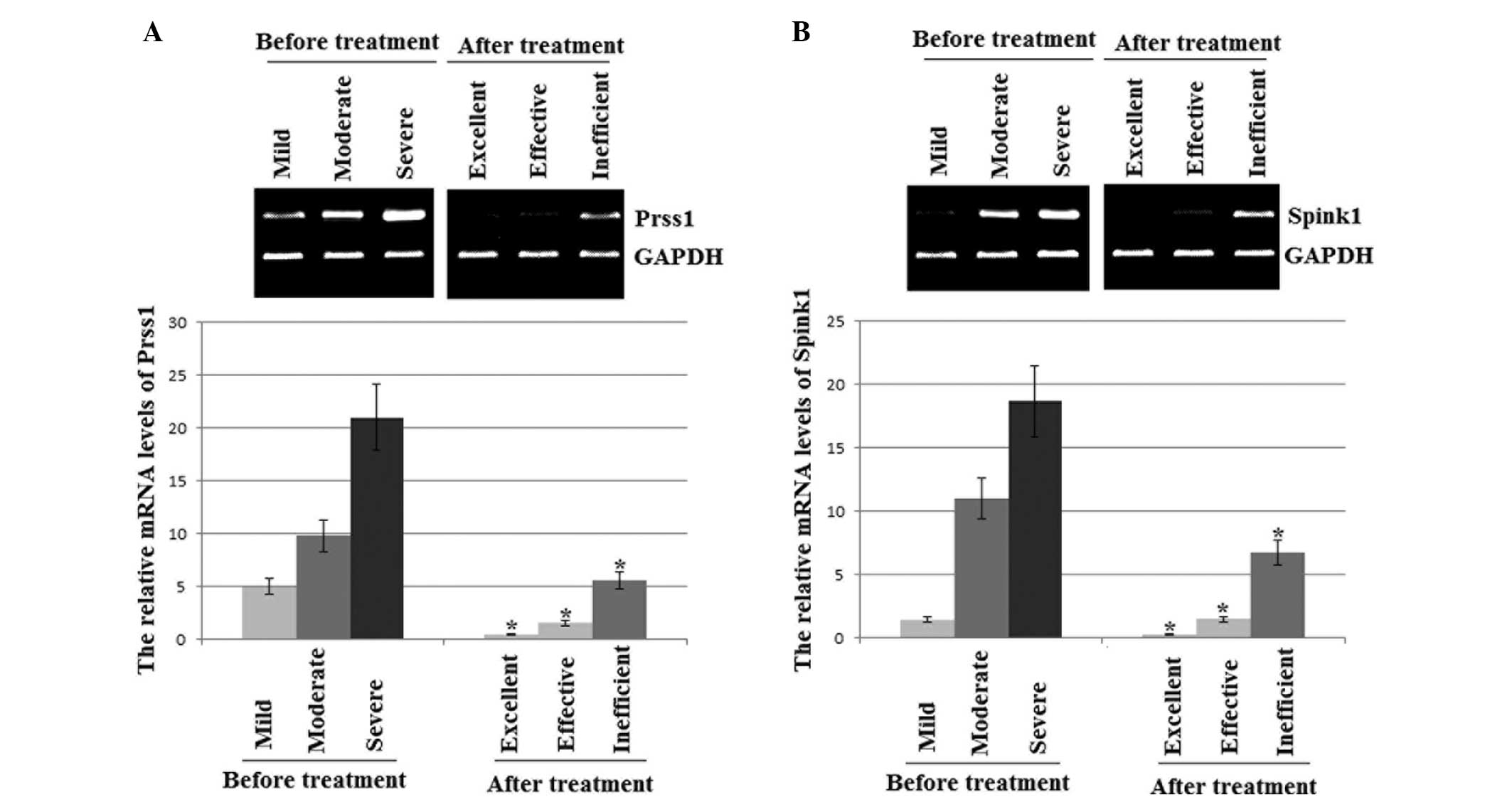
Solomon S, Whitcomb DC and LaRusch J:
PRSS1-related hereditary pancreatitis. GeneReviews®.
Pagon RA, Adam MP, Ardinger HH, et al: University of Washington;
Seattle, WA: 2012
|
|
24
|
Sánchez-Ramírez CA, Flores-Martínez SE,
García-Zapién AG, et al: Screening of R122H and N29I mutations in
the PRSS1 gene and N34S mutation in the SPINK1 gene in Mexican
pediatric patients with acute and recurrent pancreatitis. Pancreas.
41:707–711. 2012.PubMed/NCBI
|
|
25
|
Tukiainen E, Kylänpää ML, Kemppainen E, et
al: Pancreatic secretory trypsin inhibitor (SPINK1) gene mutations
in patients with acute pancreatitis. Pancreas. 30:239–242. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Lee YJ, Kim KM, Choi JH, et al: High
incidence of PRSS1 and SPINK1 mutations in Korean children with
acute recurrent and chronic pancreatitis. J Pediatr Gastroenterol
Nutr. 52:478–481. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Sobczyńska-Tomaszewska A, Bak D, Oralewska
B, et al: Analysis of CFTR, SPINK1, PRSS1 and AAT mutations in
children with acute or chronic pancreatitis. J Pediatr
Gastroenterol Nutr. 43:299–306. 2006. View Article : Google Scholar
|
|
28
|
Kiriyama S, Gabata T, Takada T, et al: New
diagnostic criteria of acute pancreatitis. J Hepatobiliary Pancreat
Sci. 17:24–36. 2010. View Article : Google Scholar
|
|
29
|
Gubergrits N, Golubova O, Lukashevich G
and Fomenko P: Elevated serum amylase in patients with chronic
pancreatitis: acute attack or macroamylasemia? Pancreatology.
14:114–116. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Wojtuń S and Gil J: Utility of amylase
serum and urine activity in acute biliary pancreatitis treated with
biliary sphincterotomy. Pol Merkur Lekarski. 22:381–384. 2007.(In
Polish).
|
|
31
|
Banks PA, Bollen TL, Dervenis C, et al;
Acute Pancreatitis Classification Working Group. Classification of
acute pancreatitis - 2012: revision of the Atlanta classification
and definitions by international consensus. Gut. 62:102–111. 2013.
View Article : Google Scholar
|
|
32
|
Li YC, Dong L, Jia A, Chang XM and Xue H:
Preparation of solid lipid nanoparticles loaded with traditional
Chinese medicine by high-pressure homogenization. Nan Fang Yi Ke Da
Xue Xue Bao. 26:541–544. 2006.(In Chinese). PubMed/NCBI
|
|
33
|
Zhuang WJ and Qian C: Treatment of
infected deciduous root canal with Samyan (traditional Chinese
medicine) paste: Clinical analysis. Shanghai Kou Qiang Yi Xue.
6:1851997.(In Chinese).
|
|
34
|
Xue QM, Li N, Xue P, Wang CW and Wen Q:
Therapeutic effects of electroacupuncture at ST36 acupoint on
sodium-taurocholate-induced severe acute pancreatitis. Chin J
Integr Med. 20:695–700. 2014. View Article : Google Scholar
|
|
35
|
Saito Y, Emura F, Matsuda T, et al: A new
sinker-assisted endoscopic submucosal dissection for colorectal
cancer. Gastrointest Endosc. 62:297–301. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Zhao J, Liao Q, Zhao Y and Hu Y: Mortality
indicators and risk factors for intra-abdominal hypertension in
severe acute pancreatitis. Int Surg. 99:252–257. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Vipperla K, Papachristou GI, Easler J, et
al: Risk of and factors associated with readmission after a
sentinel attack of acute pancreatitis. Clin Gastroenterol Hepatol.
May 9–2014.(Epub ahead of print). View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Zeng YB, Zhan XB, Guo XR, et al: Risk
factors for pancreatic infection in patients with severe acute
pancreatitis: an analysis of 163 cases. J Dig Dis. 15:377–385.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Jin J, Yu YH, Zhong M and Zhang GW:
Analyzing and identifying risk factors for acute pancreatitis with
different etiologies in pregnancy. J Matern Fetal Neonatal Med.
June 5;1–5. 2014.(Epub ahead of print). View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Tamasaki A, Nishimura Y, Kondo N, et al:
Risk factors for acute pancreatitis in patients with severe motor
and intellectual disabilities. Pediatr Int. 56:240–243. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Hong S, Qiwen B, Ying J, Wei A and
Chaoyang T: Body mass index and the risk and prognosis of acute
pancreatitis: a meta-analysis. Eur J Gastroenterol Hepatol.
23:1136–1143. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Shen HN, Wang WC, Lu CL and Li CY: Effects
of gender on severity, management and outcome in acute biliary
pancreatitis. PLoS One. 8:e575042013. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Fu P, Yuan AH, Wang CH, Li X and Wu HY:
Alcohol-induced severe acute pancreatitis followed by hemolytic
uremic syndrome managed with continuous renal replacement therapy.
BMC Nephrol. 15:12014. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Nikkola J, Räty S, Laukkarinen J, et al:
Abstinence after first acute alcohol-associated pancreatitis
protects against recurrent pancreatitis and minimizes the risk of
pancreatic dysfunction. Alcohol Alcohol. 48:483–486. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Müller S, Kaiser H, Krüger B, et al:
Age-dependent effects of UCP2 deficiency on experimental acute
pancreatitis in mice. PLoS One. 9:e944942014. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Okamura D, Starr ME, Lee EY, et al:
Age-dependent vulnerability to experimental acute pancreatitis is
associated with increased systemic inflammation and thrombosis.
Aging Cell. 11:760–769. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Akesson A, Andersen LF, Kristjánsdóttir
AG, et al: Health effects associated with foods characteristic of
the Nordic diet: a systematic literature review. Food Nutr Res.
572013.
|
|
48
|
Overby NC, Sonestedt E, Laaksonen DE and
Birgisdottir BE: Dietary fiber and the glycemic index: a background
paper for the Nordic Nutrition Recommendations 2012. Food Nutr Res.
57:2013. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Knaan T, Endevelt R and Singer P:
Evaluating the validity of the ‘categories method’: A new method
for self-report assessment of daily calorie intake: A pilot study.
Can J Diabetes. 37(Suppl 2): S2832013. View Article : Google Scholar
|
|
50
|
Pelaez-Luna M, Robles-Diaz G,
Canizales-Quinteros S and Tusie-Luna MT: PRSS1 and SPINK1 mutations
in idiopathic chronic and recurrent acute pancreatitis. World J
Gastroenterol. 20:11788–11792. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Roncati L, Gualandri G, Fortuni G and
Barbolini G: Sudden death and lipomatous infiltration of the heart
involved by fat necrosis resulting from acute pancreatitis.
Forensic Sci Int. 217:e19–e22. 2012. View Article : Google Scholar
|
|
52
|
Chen H, Li F, Jia JG, et al: Effects of
traditional Chinese medicine on intestinal mucosal permeability in
early phase of severe acute pancreatitis. Chin Med J (Engl).
123:1537–1542. 2010.
|
|
53
|
Zhang MJ, Zhang GL, Yuan WB, Ni J and
Huang LF: Treatment of abdominal compartment syndrome in severe
acute pancreatitis patients with traditional Chinese medicine.
World J Gastroenterol. 14:3574–3578. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Athwal T, Huang W, Mukherjee R, et al:
Expression of human cationic trypsinogen (PRSS1) in murine acinar
cells promotes pancreatitis and apoptotic cell death. Cell Death
Dis. 5:e11652014. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Wang J, Ohmuraya M, Suyama K, et al:
Relationship of strain-dependent susceptibility to experimentally
induced acute pancreatitis with regulation of Prss1 and Spink3
expression. Lab Invest. 90:654–664. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Corleto VD, Gambardella S, Gullotta F, et
al: New PRSS1 and common CFTR mutations in a child with acute
recurrent pancreatitis, could be considered an ‘Hereditary’ form of
pancreatitis? BMC Gastroenterol. 10:1192010. View Article : Google Scholar
|
|
57
|
Ohmuraya M and Yamamura K: Roles of serine
protease inhibitor Kazal type 1 (SPINK1) in pancreatic diseases.
Exp Anim. 60:433–444. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Rai P, Sharma A, Gupta A and Aggarwal R:
Frequency of SPINK1 N34S mutation in acute and recurrent acute
pancreatitis. J Hepatobiliary Pancreat Sci. 21:663–668. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Tremblay K, Dubois-Bouchard C, Brisson D
and Gaudet D: Association of CTRC and SPINK1 gene variants with
recurrent hospitalizations for pancreatitis or acute abdominal pain
in lipoprotein lipase deficiency. Front Genet. 5:902014. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Terlizzi V, De Gregorio F, Sepe A, et al:
Brand new SPINK1 and CFTR mutations in a child with acute recurrent
pancreatitis: a case report. Minerva Pediatr. 65:669–672.
2013.PubMed/NCBI
|
|
61
|
Jøergensen MT, Brusgaard K, Novovic S, et
al: Is the SPINK1 variant p. N34S overrepresented in patients with
acute pancreatitis? Eur J Gastroenterol Hepatol. 24:309–315. 2012.
View Article : Google Scholar
|
|
62
|
Baudry C, Rebours V, Houillier P, et al:
Recurrent acute pancreatitis caused by association of a novel
mutation of the calcium-sensing receptor gene and a heterozygous
mutation of the SPINK1 gene. Pancreas. 39:420–421. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Aoun E, Muddana V, Papachristou GI and
Whitcomb DC: SPINK1 N34S is strongly associated with recurrent
acute pancreatitis but is not a risk factor for the first or
sentinel acute pancreatitis event. Am J Gastroenterol. 105:446–451.
2010. View Article : Google Scholar
|
|
64
|
Liu XB, Jiang JM, Huang ZW, et al:
Clinical study on the treatment of severe acute pancreatitis by
integrated traditional Chinese medicine and Western medicine. J
Sichuan University (medical science edition). 35:204–208. 2004.(In
Chinese).
|