Introduction
Orbital deformities that occur following
enucleation, evisceration or exenteration are often corrected with
hydroxyapatite orbital implantation. Following this surgery, local
inflammation or delayed vascularization of the orbital implant may
hinder the healing of conjunctival wounds, causing conjunctival
dehiscence (1,2) and even orbital implant exposure and
prolapse. These complications are usually treated with drugs and
secondary surgery (3–5). Orbital implant exposure is currently
treated with various surgical techniques, including a dermal fat
graft (6,7), acellular dermal graft (8), palate mucosal repair (9), oral mucosal repair (10), Enduragen® graft repair (11), subconjunctival tissue flap repair
(12) and fresh amniotic membrane
repair (13). These surgical methods
are unsatisfactory, however, as they cannot eliminate local
inflammation or accelerate vascularization of the orbital implant.
Secondary surgery usually causes unsatisfactory restoration, and
patients must undergo multiple repair surgeries and sometimes
removal of the orbital implant.
It has been well established that laser therapy is
useful in several therapeutic scenarios (14,15). A
plethora of beneficial effects have been demonstrated for numerous
in vitro and in vivo test systems, including
antibacterial, antiviral, antitumor, cellular differentiation,
immunopotentiating and repair activities (16). In particular, helium-neon lasers
based on red light allow primary chromophores to act as endogenous
porphyrins (17). Although
helium-neon laser therapy has achieved satisfactory results with
regard to wound healing (18,19), its
application to hydroxyapatite orbital implant exposure has not been
reported to date.
Local helium-neon laser irradiation has been
conducted in patients with orbital implant exposure in the First
Affiliated Hospital of Nanjing Medical University (Nanjing, China)
since 2007; the present study concerns the investigation into the
clinical efficacy of the technique.
Materials and methods
Patients
A total of 70 patients (46 men and 24 women) with
hydroxyapatite orbital implant exposure were included in this study
between January 1997 and July 2014, nonconsecutively. The mean age
of the subjects was 37.6 years (range, 23–62 years). Among the
patients, 35 were treated with helium-neon laser therapy (group A):
22 men and 13 women, with a mean age of 36.5 years (range, 25–55
years). In total, 30 patients underwent orbital implantation at the
first stage and the other 5 patients that were unable to undergo
the first stage operation for various reasons were included in the
second stage. The patients in group A were followed up for 2–28
months postoperatively. The remaining 35 patients were treated with
drugs and surgery (group B): 25 men and 10 women with a mean age of
39.5 years (range, 24–60 years). A total of 22 patients underwent
orbital implantation at the first stage and the other 13 patients
at the second stage. The group B patients were followed up for 5–40
months postoperatively. The two groups had no statistically
significant differences in age or gender (P>0.05).
Animal experiment
A total of 24 New Zealand white 7-month-old rabbits
(equally male and female) weighing 2–3 kg were obtained from
Nanjing Medical University. The rabbits received 10-mm diameter
hydroxyapatite orbital implant (IOI Corp.) and were divided into
two groups. In one group, the rabbits were treated with 0.5%
levofloxacin ophthalmic solution and 21,000 IU/5 ml bFGF eye drops
(4 times per day) following surgery. The other group underwent
helium-neon laser irradiation plus the eye drops. After 2 weeks of
treatment, the hydroxyapatite orbital implants harvested from the
rabbit eyes underwent pathology examinations.
Degree of orbital implant
exposure
Orbital implant exposure of <7 mm was considered
mild, while that of 7–10 mm was moderate to severe. Patients were
excluded if their orbital implant exposure was >10 mm, the
anterior orbital implant appeared to have prolapsed or there was
orbital infection (19).
In this study, 24 patients in group A had mild
orbital exposure and 11 patients had moderate to severe exposure.
Similarly, in group B, 24 patients had mild orbital exposure and 11
had moderate to severe exposure.
Treatment
The orbital implant (20 mm diameter; IOI Corp., San
Diego, CA, USA) was wrapped with a pedicled scleral flap.
Implantation was performed following evisceration. In group A, a
helium-neon laser multifunction therapy machine (LJL40-HA; Shanghai
Institute of Laser Technology, Shanghai, China) was used as
follows: Maximum output power, 50 MW; emission wavelength, 632.8
nm; main voltage, 220±22 V; frequency, 50±1 Hz. The aperture size
was adjusted based on the conjunctival sac. Irradiation was applied
for 15 min continuously once a day for 10 days. During the
follow-up period, patients were administered 0.5% levofloxacin
ophthalmic solution [Santen Pharmaceutical (China) Co. Ltd.,
Suzhou, China] and recombinant bovine basic fibroblast growth
factor (bFGF) eye drops (21,000 IU/5 ml; Zhuhai Essex
Bio-Pharmaceutical Co., Ltd., Shenzhen, China) 4 times per day. The
patients were rechecked every 5 days postoperatively until the
conjunctival wounds had healed. In group B, patients with mild
orbital implant exposure were treated with levofloxacin ophthalmic
solution and recombinant bovine bFGF eye drops. Patients with
moderate to severe exposure underwent surgical restoration and drug
therapy if drugs alone did not diminish the exposure. Surgical
restoration included conjunctival flap transposition for a
conjunctival wound and allogeneic scleral repair for evident
implant exposure and scleral dissolution.
Statistical analysis
Data were statistically processed using SPSS
software (version 13.0; SPSS, Inc., Chicago, IL, USA). The healing
rates were compared using the χ2 test. Healing times
were compared using a two independent samples t-test. Data
expressed as the mean ± standard deviation. P<0.05 was
considered to indicate a statistically significant difference.
Results
Healing rates
In group A, all 24 patients with mild orbital
implant exposure underwent a course of helium-neon laser
irradiation, following which their conjunctival wounds had healed,
giving a 100% healing rate. The average healing time was 7.22±2.11
days. Conjunctival hyperemia was clearly attenuated, secretion was
reduced and eyelid activities were normal. The remaining 11
patients with moderate to severe exposure underwent one course of
helium-neon laser irradiation. Four patients achieved conjunctival
wound healing, and six more were completely healed following two
courses of laser therapy. There was no exudation or conjunctival
hyperemia and the eyelid moved freely. One patient with severe
conjunctival dehiscence and anterior implant exposure underwent
allogeneic scleral restoration and conjunctival flap implantation
to repair a conjunctival wound. The conjunctival wound healed
following three courses of local helium-neon laser irradiation with
no complications.
In group B, 24 patients with mild orbital implant
exposure were treated with drugs. Among them, 22 cases healed. The
healing rate was 91.67%. The average healing time was 14.33±3.20
days, which was significantly longer than that for group A
(Table I). The 11 patients with
moderate to severe exposure were treated with drugs and surgery.
Among them, 4 patients experienced healing. The healing rate was
36.36%, which was clearly lower than that in group A (90.91%).
 | Table I.Comparison of conjunctival wound
healing rates between the two groups. |
Table I.
Comparison of conjunctival wound
healing rates between the two groups.
|
| Helium-neon laser
irradiation group (group A) | Drugs and surgical
treatment group (group B) |
|---|
|
|
|
|
|---|
| Degree of
conjunctival dehiscence | N | No. of healing
cases | No. of nonhealing
cases | Healing rate, % | N | No. of healing
cases | No. of nonhealing
cases | Healing rate, % |
|---|
| Mild | 24 | 24 | 0 | 100.00 | 24 | 22 | 2 | 91.67 |
| Moderate to
severe | 11 | 10 | 1 |
90.91 | 11 | 4 | 7 | 36.36 |
| Total | 35 | 34 | 1 |
97.14 | 35 | 26 | 9 | 74.29 |
The total efficiency rate of helium-neon laser
irradiation was 97.14%, which was significantly higher than that
for the drugs plus surgery treatment (74.29%). A comparison of the
treatment outcomes between the two groups is shown in Table I.
Conjunctival healing times
The results showed that the average healing time of
conjunctival wounds was 7.22±2.11 days for the mild-exposure
patients in group A and 14.33±3.20 days for the mild-exposure
patients in group B. The difference was significant
(t=8.97>t0.05(44)=2.12, P<0.05). Patients with
moderate to severe orbital implant exposure had an average healing
time of 18.19±2.12 days in group A and 31.25±4.21 days in group B.
The difference was significant
(t=7.91>t0.05(12)=2.179, P<0.05). Helium-neon
laser irradiation clearly shortened the healing time of the
conjunctival wounds in patients with mild or moderate to severe
orbital implant exposure (Table
II).
 | Table II.Comparison of the healing times of
conjunctival wounds for the two groups. |
Table II.
Comparison of the healing times of
conjunctival wounds for the two groups.
| Exposure | Healing time in group
A (days) | Healing time in group
B (days) | t | P-value |
|---|
| Mild |
7.22±2.11 | 14.33±3.20 | 8.97 | <0.05 |
| Moderate to
severe | 18.19±2.12 | 31.25±4.21 | 7.91 | <0.05 |
Changes in hydroxyapatite orbital
implants prior to and following helium-neon laser irradiation
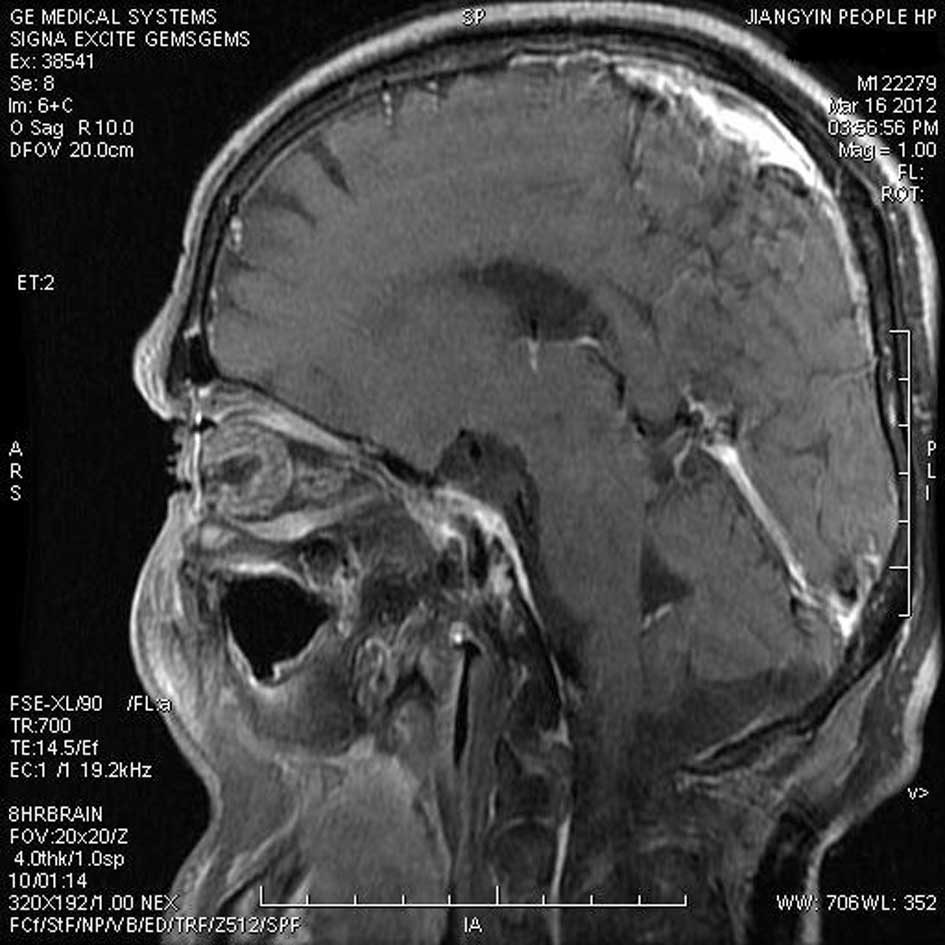
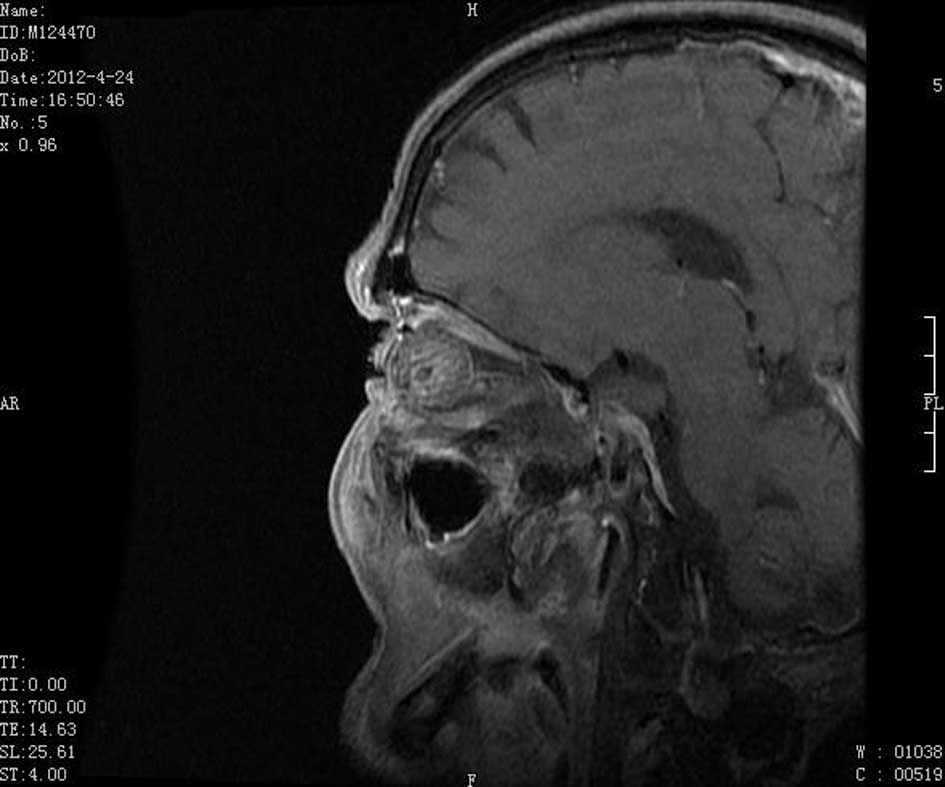
Patients with moderate to severe orbital implant
exposure underwent magnetic resonance imaging (MRI) prior to and
following helium-neon laser irradiation. The results showed that
the front part of the orbital implant was not vascularized in
patients with apparent conjunctival dehiscence (Fig. 1). By contrast, following one course
of helium-neon laser irradiation, vascularization of the front part
of the orbital implant was clearly visible (Fig. 2). The conjunctival wound was healed
with no complications. The findings indicate that helium-neon laser
irradiation significantly promotes orbital implant
vascularization.
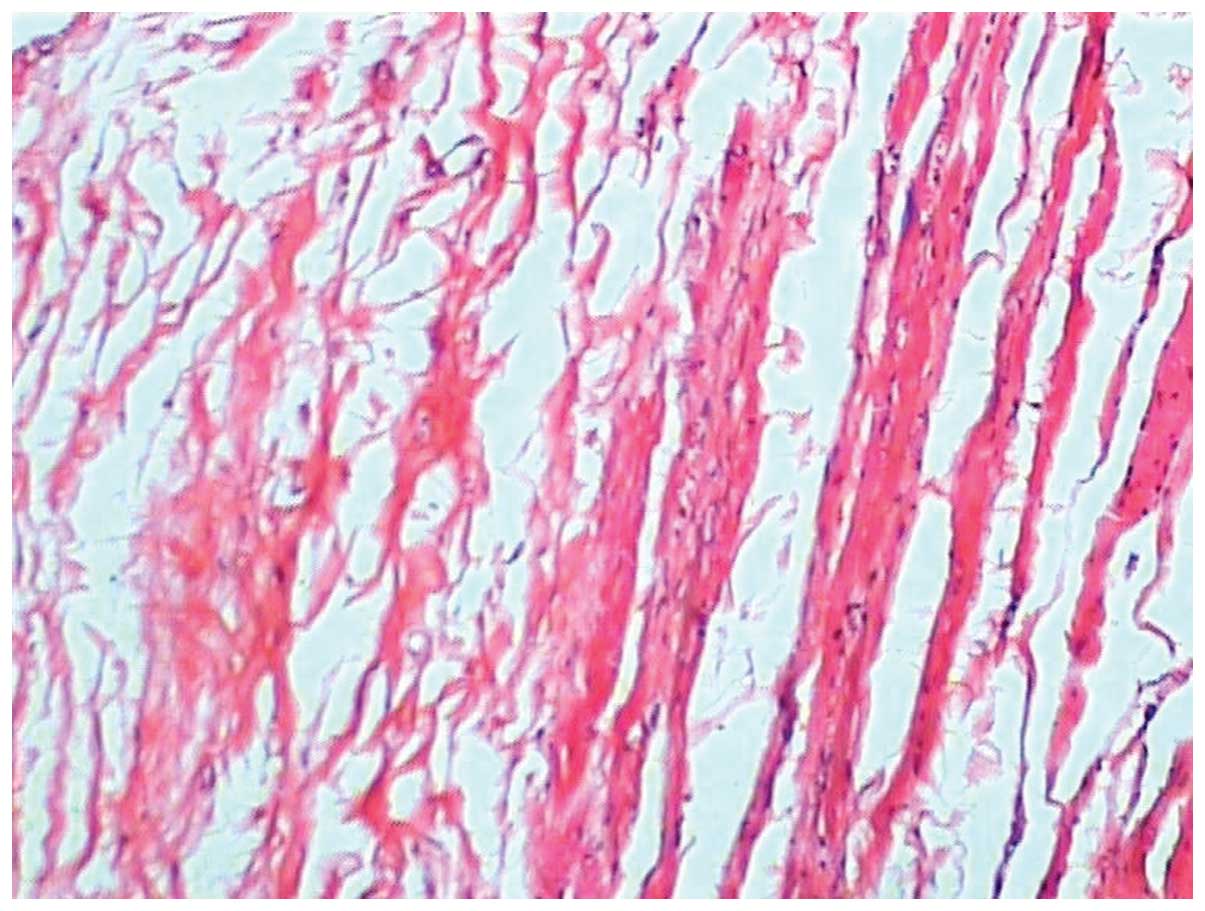
In an animal experiment, New Zealand white rabbits
were given 10-mm diameter hydroxyapatite orbital implants (IOI
Corp.) and divided into two groups. In one group, the rabbits were
treated with 0.5% levofloxacin ophthalmic solution and 21,000 IU/5
ml bFGF eye drops (4 times per day) following surgery. The other
group underwent helium-neon laser irradiation plus the eye drops.
After 2 weeks of treatment, the hydroxyapatite orbital implants
harvested from the rabbit eyes underwent pathology examinations. In
the rabbits that received eye drops alone, there was sparse fibrous
tissue around the orbital implant, only a few new blood vessels
were evident and a large number of inflammatory cells (mainly
neutrophils) and red blood cells were present. Following
helium-neon laser irradiation plus eye drops, mature and dense
fibrous tissues were noted around the implants. No inflammatory
cells were apparent. The findings indicated that, in addition to
promoting orbital vascularization, helium-neon laser irradiation
has anti-inflammatory effects.
Discussion
Orbital implant exposure is a common complication
following orbital implantation. Custer and Trinkaus (20) estimated that the total incidence of
postoperative orbital implant exposure in China was 4.9%, and the
prevalence in China reportedly ranged from 1.6 to 21.6% between
1998 and 2004 (21). The majority of
patients with mild exposure (7 mm) and conjunctival dehiscence are
healed by drugs, whereas those with moderate to severe exposure
undergo both drug and surgical treatment. The surgical treatment
may include local debridement, polishing of the orbital implant
surface and allogeneic scleral transposition for conjunctival flap
restoration (3–5,20).
Secondary surgical restoration is sometimes ineffective in patients
with severe exposure. Custer and Trinkaus (20) noted that 29% of severe cases required
removal of the orbital implant.
Conjunctival dehiscence and orbital implant exposure
following orbital implant surgery are the results of delayed
histogenesis of orbital fibrovascular tissue and local inflammatory
reactions (1,2). Tambe et al (1) found that all of the patients who failed
surgery appeared to have chronic inflammation according to
pathological sections of the exposed orbital implant. Sustained
local chronic inflammatory reactions may affect orbital implant
vascularization, delay orbital fibrous vascularization, reduce the
local anti-inflammatory reaction of the orbital implant and hinder
local wound healing, ultimately expanding a bulbar conjunctival
wound and causing apparent orbital implant exposure. Eye drops
mainly function at the conjunctiva so it is difficult for them to
reach the orbital implant. Surgical treatment can debride local
wounds and restore conjunctival wounds. Since the combination of
drugs and surgical treatment cannot prevent orbital inflammation or
promote vascularization, their use has a low success rate for
treating orbital implant exposure.
Lasers can play an important role in tissue repair.
Kazem Sakouri et al (22)
postulated that the use of lasers could enhance callus development
during the early stage of the healing process in rabbits.
Similarly, it has been suggested that low-level laser therapy may
accelerate fracture repair or cause increased callus volume and
bone mineral density, particularly during the early stages of
absorbing hematoma and bone remodeling (23). A previous study has demonstrated that
helium-neon laser therapy significantly increased the number of
blood vessels after 7 days of irradiation (24).
Helium-neon laser is red light at 632.8 nm. The
incident beam can partially reach into 15 mm of tissue, causing
local vascular dilation and accelerated blood flow. The laser thus
plays a role in reducing inflammation, has an anti-swelling effect
and promotes functional recovery. Calin and Parasca (25) found that a laser at 630–700 nm
significantly repaired injured tissue. In addition, low-energy
helium-neon lasers strengthen phagocytosis by macrophages and
promote the absorption of inflammation (26). Local helium-neon laser therapy
contributes to the prevention of the inflammatory reaction and
promotes local tissue proliferation and wound healing. These
efficacies of helium-neon laser therapy provide strong theoretical
evidence for its use in the clinical treatment of orbital implant
exposure.
In the present study, 35 patients with orbital
implant exposure were treated with helium-neon laser therapy (group
A), and 34 of them achieved complete healing. The efficacy rate was
97.14%, which was significantly higher than that for patients in
group B (74.29%), who were on a drugs plus surgery regimen. In
addition, helium-neon laser therapy markedly shortened the healing
time of the conjunctival wounds in patients with mild conjunctival
dehiscence and orbital implant exposure (Table II). Enhanced MRI scans and animal
experiments (Figs. 3 and 4) confirmed the contribution of helium-neon
lasers to the promotion of vascularization and prevention of
inflammation. These results have revealed the underlying mechanisms
of helium-neon laser therapy for treating hydroxyapatite orbital
implant exposure: The technique promotes vascularization of the
orbital implant; improves internal microcirculation of the orbital
implant; enhances the anti-infection capacity; enhances local
vasodilation, accelerating blood flow; and strengthens phagocytosis
by macrophages, promoting the absorption of inflammatory cells and
thereby promoting the healing of conjunctival wounds.
In conclusion, helium-neon laser therapy is superior
to combined drugs and surgery for treating hydroxyapatite orbital
implant exposure accompanying postoperative conjunctival
dehiscence. It can significantly increase the healing rate of
conjunctival wounds and shorten the healing time. This low-cost
method is safe and efficient and can serve as a routine
precautionary measure for patients in poor local and systemic
conditions. In summary, helium-neon laser therapy is an ideal
treatment for hydroxyapatite orbital implant exposure.
References
|
1
|
Tambe K, Pushpoth S, Mudhar HS and
Sandramouli S: A histopathologic study of orbital implant
vascularization. Orbit. 28:50–57. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Buettner H and Bartley GB: Tissue
breakdown and exposure associated with orbital hydroxyapatite
implants. Am J Ophthalmol. 113:669–673. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kuzmanović Elabjer B, Petrinović-Doresić
J, Busić M and Henc-Petrinović L: Our approach in the treatment of
exposed hydroxyapatite orbital implant. Acta Med Croatica.
60:141–144. 2006.(In Croatian). PubMed/NCBI
|
|
4
|
Lu L, Shi W, Luo M, Sun Y and Fan X:
Repair of exposed hydroxyapatite orbital implants by
subconjunctival tissue flaps. J Craniofac Surg. 22:1452–1456. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
el-Shahed FS, Sherif MM and Ali AT:
Management of tissue breakdown and exposure associated with orbital
hydroxyapatite implants. Ophthal Plast Reconstr Surg. 11:91–94.
1995. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kim HK and La TY: Treatment of intractable
orbital implant exposure with a large conjunctival defect by
secondary insertion of the implant after preceding dermis fat
graft. Int J Ophthalmol. 6:193–197. 2013.PubMed/NCBI
|
|
7
|
Lee BJ, Lewis CD and Perry JD: Exposed
porous orbital implants treated with simultaneous secondary implant
and dermis fat graft. Ophthal Plast Reconstr Surg. 26:273–276.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Jung SK, Paik JS, Sonn UH and Yang SW:
Surgical outcomes of acellular human dermal grafts for large
conjunctiva defects in orbital implant insertion. Graefes Arch Clin
Exp Ophthalmol. 251:1849–1854. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kaynak P, Karabulut GO, Ozturker C,
Perente I, Gökyiǧit B, Demirok A and Yilmaz OF: Remove, rotate and
reimplant: A novel technique for the management of exposed porous
anophthalmic implants in eviscerated patients. Eye (Lond).
28:546–552. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yoon KC, Yang Y, Jeong IY and Kook MS:
Buccal mucosal graft for hydroxyapatite orbital implant exposure.
Jpn J Ophthalmol. 55:318–320. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wu AY, Vagefi MR, Georgescu D, Burroughs
JR and Anderson RL: Enduragen patch grafts for exposed orbital
implants. Orbit. 30:92–95. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lu L, Shi W, Luo M, Sun Y and Fan X:
Repair of exposed hydroxyapatite orbital implants by
subconjunctival tissue flaps. J Craniofac Surg. 22:1452–1456. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Xie RL: Fresh amnion transplantation for
ocular prosthesis exposure. Zhonghua Yan Wai Shang Zhi Ye Bing Za
Zhi. 33:305–307. 2011.(In Chinese).
|
|
14
|
da Guarda MG, Paraguassú GM, Cerqueira NS,
Cury PR, Farias JG and Ramalho LM: Laser GaAlAs (λ 860 nm)
photobiomodulation for the treatment of bisphosphonate-induced
osteonecrosis of the jaw. Photomed Laser Surg. 30:293–297. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Sato K, Moy OJ, Peimer CA, Nakamura T,
Howard C, Ko SH, Lee TC and Nishiwaki Y: An experimental study on
costal osteochondral graft. Osteoarthr Cartilage. 20:172–183. 2012.
View Article : Google Scholar
|
|
16
|
Lan CC, Wu CS, Chiou MH, Hsieh PC and Yu
HS: Low-energy helium-neon laser induces locomotion of the immature
melanoblasts and promotes melanogenesis of the more differentiated
melanoblasts: Recapitulation of vitiligo repigmentation in vitro. J
Invest Dermatol. 126:2119–2126. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Klebanov GI, Teselkin YO, Babenkova IV,
Bashkueva TY, Chiehuk TV and Vladimirov YA: Low power laser
irradiation induces leukocyte priming. Gen Physiol Biophys.
17:365–376. 1998.PubMed/NCBI
|
|
18
|
Peccin MS, Renno AC, de Oliveira F, Giusti
PR and Ribeiro DA: Helium-neon laser improves skin repair in
rabbits. J Cosmet Laser Ther. 14:286–289. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Peccin MS, de Oliveira F, Muniz Renno AC,
Pacheco de Jesus GP, Pozzi R, Gomes de Moura CF, Giusti PR and
Ribeiro DA: Helium-neon laser improves bone repair in rabbits:
Comparison at two anatomic sites. Lasers Med Sci. 28:1125–1130.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Custer PL and Trinkaus KM: Porous implant
exposure: Incidence, management and morbidity. Ophthal Plast
Reconstr Surg. 23:1–7. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Rong L, Fang Q and Ren DY: Hydroxyapatite
ocular prosthesis implantation under double cap sclera after the
modified enucleation. Yan Ke Xin Jin Zhan. 26:592006.(In
Chinese).
|
|
22
|
Kazem Shakouri S, Soleimanpour J,
Salekzamani Y and Oskuie MR: Effect of low-level laser therapy on
the fracture healing process. Lasers Med Sci. 25:73–77. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Liu X, Lyon R, Meier HT, Thometz J and
Haworth ST: Effect of lower-level laser therapy on rabbit tibial
fracture. Photomed Laser Surg. 25:487–494. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Garavello I, Baranauskas V and da
Cruz-Höfling MA: The effects of low laser irradiation on
angiogenesis in injured rat tibiae. Histol Histopathol. 19:43–48.
2004.PubMed/NCBI
|
|
25
|
Calin MA and Parasca SV: In vivo study of
age-related changes in the optical properties of the skin. Lasers
Med Sci. 25:269–274. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Li GZ: Physical therapy for skin
diseasesClinical Dermatology in China. Zhao B: 3rd. Jiangsu Science
and Technology Press; Nanjing: pp. 231–301. 2001
|