Introduction
Bronchogenic cysts are rare congenital cystic
lesions that are induced by the abnormal budding of the primitive
tracheobronchial tube. The location of bronchogenic cysts is
dependent upon the embryonic stage of development at which abnormal
budding occurs (1,2). The majority of these cysts are located
in the mediastinum, whereas the remainder of cases predominantly
involve the lung parenchyma (1,3).
Abdominal bronchogenic cysts are very rare, particularly those
located in the gastric wall (4).
Dewing et al (5) were the
first to describe such a case in 1956. Gastric bronchogenic cysts
are threefold more common in women, in contrast with
retroperitoneal cystic masses or cutaneous bronchogenic cysts,
which appear with equal frequency in men and women (6). Most patients in previous reports were
asymptomatic (7–9), but epigastric pain, nausea and vomiting
are the most common symptoms that present. Clinical manifestations
of gastric bronchogenic cysts are usually associated with cyst
enlargement, secondary infection, perforation or compression of
adjacent tissues (10). Most gastric
bronchogenic cysts are diagnosed postoperatively (11–13), but
a number have been carefully monitored without resection (14). In the present study, a case of
abdominal bronchogenic cyst in a 17-year-old patient was presented,
and the existing literature (Table
I) was reviewed in order to analyze the clinical features of
these cysts.
 | Table I.Bronchogenic cysts of stomach. |
Table I.
Bronchogenic cysts of stomach.
| Ref. | Year | Age (years) | Gender | Size (cm) | Location | Symptoms | Preoperative
diagnosis | Intervention |
|---|
| 5 | 1956 | 56 | F | 4×3×3 | Posterior wall | Epigastric
pain | Benign tumor | Resection |
| 11 | 1956 | 46 | F | 8×6 | Greater
curvature | – | Leiomyoma or
lipoma | Resection |
| 18 | 1987 | 61 | F | 6 | Cardia | – | – | Autopsy (following
heart failure) |
| 40 | 1988 | 64 | F | 15×8 | Posterior wall | Epigasric pain,
nausea, vomiting | – | Resection |
| 20 | 1995 | 35 | F | 5.5×2.5×2.0 | Posterior wall | Epigastric pain,
nausea | – | Resection |
| 41 | 1996 | 25 | M | 6.5×5×5 | Greater
curvature | – | Benign intramural
gastric cyst | Resection |
| 22a | 2000 | 34 | M | – | Greater
curvature | – | – | Drainage +
resection |
| 42 | 2000 | 35 | M | 7×6×5 | Lesser
curvature | Epigastric
discomfort, epigastric pain | Gastric cyst,
hepatic cyst | Resection |
| 12 | 2003 | 59 | F | 7×5 | Posterior wall | – | Adrenocortica
carcinoma | Laparoscopic
converted resection |
| 13 | 2003 | 62 | M | 10×3×3 | Posterior wall | – | Lymphangioma/benign
neurogenic tumor | Resection |
| 15 | 2005 | 62 | F | 1.7 | Lesser
curvature | – | Benigh stromal
tumor | Resection |
| 43a | 2005 | 26 | M | – | Corpus | Epigastric
pain | – | Endosopic
biopsy |
| 16 | 2005 | 39 | F | 4×2.5×1 | Fundus | Rib pain | GIST | Laparoscopic
resection |
| 25 | 2006 | 38 | F | 7×5 | Cardia | – | GIST, developmental
or complicated cyst | Endoscopic
resection |
| 44 | 2006 | 63 | F | 10×7.6 | Posterior wall | Fever, abdominal
pain | – | Aspiration +
resection |
| 29 | 2007 | 60 | F | 3 | Lesser
curvature | – | – | EUS + FNA +
biopsy |
| 37 | 2007 | 37 | M | 4×4 | Lesser
curvature | Epigastric
pain | Duplication
cyst | Laparoscopic
resection |
| 45 | 2007 | 46 | F | 8×5.53 | Fundus,
gastrosplenic ligament | Loss of
conscious | – | Resection of the
cysts + splenectomy |
| 24 | 2008 | 72 | F | 2×1.5 | Lesser
curvature | – | Benign cyst of the
stomach/GIST | Resection with
adenocarcinoma |
| 23 | 2009 | 43 | M | 9×4 | Lesser
curvature | Epigastric
pain | Hepatic cyst | Resection with
adenocarcinoma |
| 7 | 2010 | 25 | F | 3×2.5×2 | Fundus | Epigastric
pain | GIST | Resection |
| 21 | 2010 | 30 | F | 6×3×3 | Posterior wall | – | Pancreatic
mass | EUS + FNA +
laparoscopic resection |
| 39 | 2010 | 67 | M | 6 | Lesser
curvature | – | – | Laparoscopic
resection |
| 46 | 2010 | 42 | M | 2.5 | Lesser
curvature | Pain in the left
lumbar region | Gastric
leiomyoma | Resection |
| 9 | 2011 | 81 | F | 2.6 | Lesser
curvature | – | Congenital
cyst | Resection |
| 47 | 2011 | 29 | M | 2 | Greater
curvature | Acute lower
quadrant abdominal pain, nausea | Gastric duplication
cyst | Resection |
| 47 | 2011 | 26 | F | 5×2.2×2 | Lesser
curvature | Epigastric
pain | Congenital
gastrointestinal duplication | Resection |
| 48 | 2011 | 76 | M | 4×4 | Lesser
curvature | – | GIST | Resection |
| 4 | 2012 | 40 | M | 1.9×1.5 | Juxtacardial | Epigastric
pain | Bronchogenic
cyst | Follow up |
| 49 | 2012 | 44 | F | 7.5×6.6×6.5 | Posterior wall | – | Benign cyst of the
pancreas/GIST | Resection |
| 10 | 2013 | 50 | M | 8×6 | Cardia | – | Retroperitoneal
mass | Resection |
| 10 | 2013 | 30 | F | 10×6 | Posterior wall | – |
GIST/lymphangioma | Resection |
| 36 | 2013 | 71 | M | 3.2 | Cardia | Throat
discomfort | Lymphangioma/benign
neurogenic tumor | Laparoscopic
resection |
| 38 | 2013 | 40 | F | 5×3.5 | Esophagastric
junction | Worsening
dysphagia | – | EUS aspiration +
laparoscopic resection |
| − b | 2013 | 17 | F | 3.5 | Cardia | Epigastric
pain | GIST | Resection |
Case report
A 17-year-old Chinese female was admitted to Lishui
Central Hospital (Lishui, China) in October 2013 suffering from
nonradiating periodic epigastric pain, without a fever. The pain
had begun 2 years previously and had increased in severity within
the 2 months prior to admission. The patient did not experience
nausea, vomiting, dysphagia, heartburn, weight loss, diarrhea,
constipation or early satiety, and had no premedical or family
history of gastric cancer. All procedures conducted in the present
study were approved by the ethics committee of Lishui Central
Hospital (Lishui, China), and written informed consent was obtained
from the patient and her father prior to participation in the
current study. Upon physical examination, no symptoms of note were
detected. Blood and stool routine examination, α-fetal protein
concentration, carcinoembryonic antigen and carbohydrate antigen CA
199 levels were all normal.
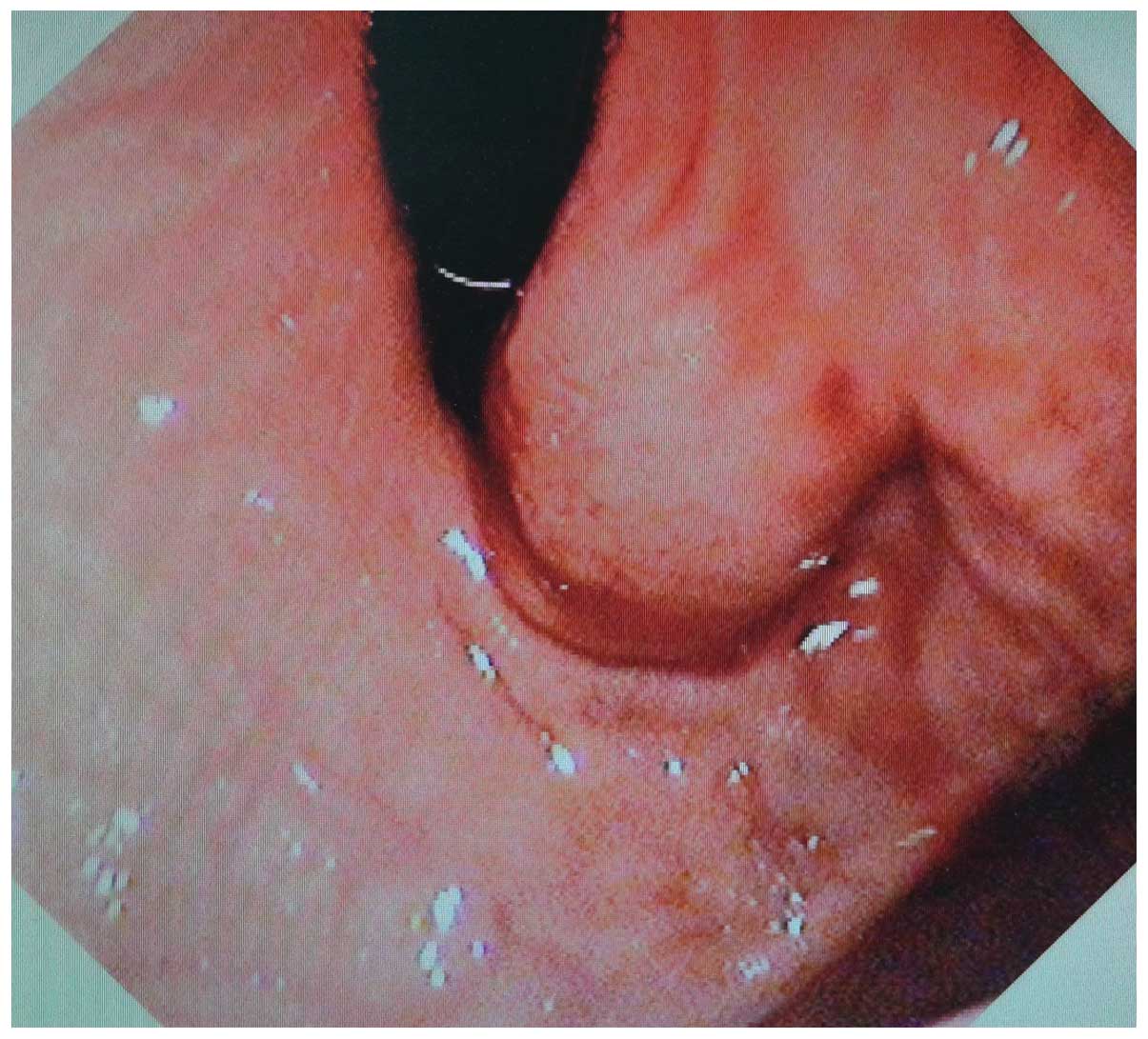
A gastroscopic examination revealed a large and
mobile submucosal lesion in the cardia, with a diameter of 3 cm
(Fig. 1). The mucosa was smooth and
the cardiac ostium of the stomach was mildly strictured, with no
evidence of bleeding or ulceration. Pinch biopsies demonstrated a
normal gastric mucosa without Helicobacter pylori infection;
therefore, gastric submucosal leiomyomatosis was suspected.
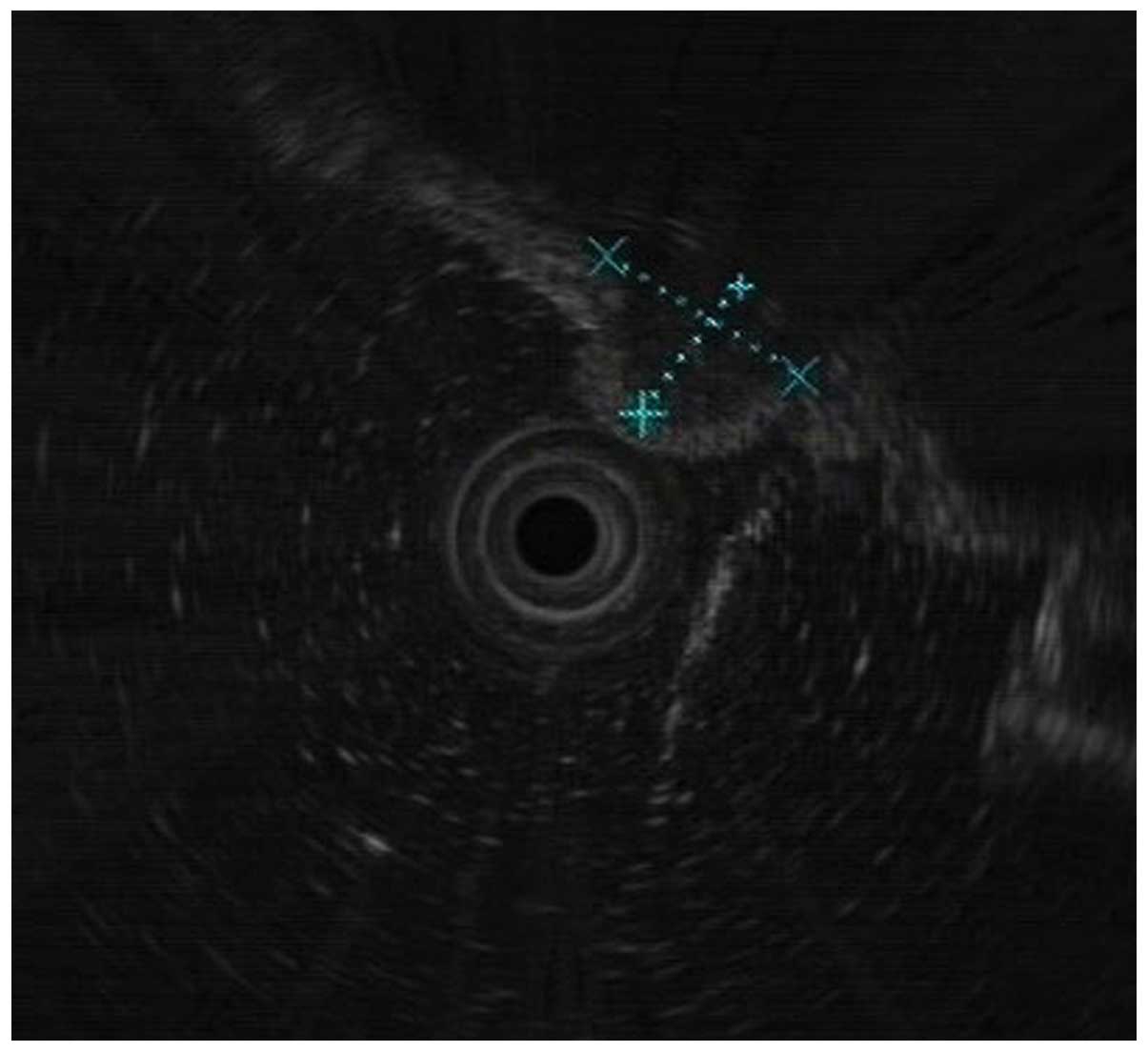
Endoscopic ultrasonography (EUS) detected a large submucosal lesion
in the cardia and the mucosa was smooth. A medium and hypoechoic
mass measuring 3 cm in diameter was detected in the muscularis
propria, which was subsequently diagnosed as a stromal tumor
(Fig. 2). Using abdominal
multi-detector-row computed tomography (CT), a quasi-circular
lesion of cystic density without enhancement was detected in the
cardia that measured 3.0×2.5 cm. No calcification or septation was
detected (Fig. 3). Subsequent
magnetic resonance imaging (MRI) demonstrated a smooth and
quasi-circular lesion with high T2 and equal T1 signal intensity
without enhancement; therefore, a cyst in the cardia of the stomach
was suspected (Fig. 4). Esophagus
barium opacification revealed that the cardia of the stomach was
compressed (Fig. 5). Based on these
results, the patient was preoperatively diagnosed with a stromal
tumor in the cardia of the stomach.
During an exploratory laparotomy, a smooth cystic
mass was detected between the submucosa and seromuscular layers,
which measured 3.0×2.5 cm. The lumen of the stomach was intact and
no discrete nodules were noted. The mass was successfully resected.
Subsequent inspection of the specimen demonstrated that it was
cystic and filled with viscous, mucoid cream-colored fluid.
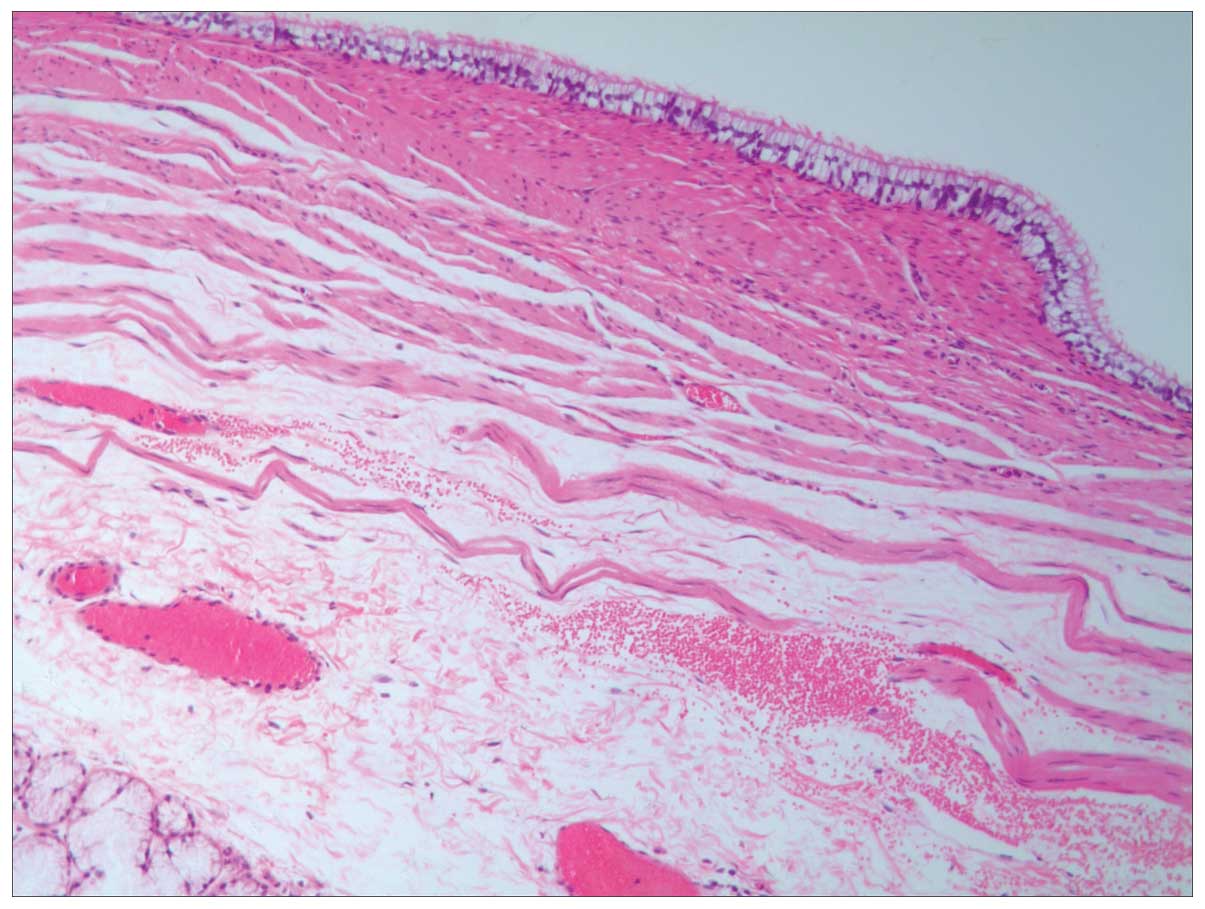
Microscopic analysis of the sections was conducted with a Microm HM
325 rotary microtome (Thermo Fisher Scientific, Waltham, MA, USA)
following hematoxylin and eosin staining (Sinopharm Chemical
Reagent Co., Ltd., Shanghai, China). This revealed that the cystic
wall of the cardia consisted of smooth muscle fibers with focal
mucous glands and ciliated columnar epithelia without any cytologic
atypia. Thus, the diagnosis of a bronchogenic cyst in the cardia of
the stomach was confirmed based on its histological appearance
(Fig. 6), in accordance with a
previous report (15).
Postoperatively, the patient recovered successfully and the
epigastric pain disappeared. At the 10 month follow-up, a total
abdominal CT revealed no recurrence of lesions. At a 12 month
follow-up, there was no evidence of recurrence and, as of the last
follow-up in December 2014, the patient had reported no symptoms
such as nausea, epigastric pain or abdominal distention.
Discussion
In order to more extensively study bronchogenic
cysts of the stomach, these were researched using the keywords
‘bronchogenic cyst of the stomach’ in Medline/PubMed (www.ncbi.nlm.nih.gov/pubmed). The final date of
data collection was in August 2014. All cases confirmed by
pathology, and cases with imaging characteristics typical of
bronchogenic cysts of the stomach were included, regardless of
patient age and gender. Cases without typical pathological or
imaging features were excluded, and this search only included
papers published in English. To the best of our knowledge, as of
August 2014, 34 cases of gastric bronchogenic cysts had been
reported under these search conditions. These cases are listed in
Table I.
Bronchogenic cysts result from a developmental
malformation in the foregut during weeks 3–7 of embryonic
development. Migration of these cysts can occur when the
attachments to the trachea or esophagus are not maintained
(16). Bronchogenic cysts are lined
with cuboida or pseudostratified ciliated epithelium and may or may
not be surrounded by elastic fibres, smooth muscle and cartilage.
The predominant locations include the hilar and middle mediastinal
area, whereas extrathoracic and subdiaphragmatic bronchogenic cysts
are rare (15). There are <100
subdiaphragmatic bronchogenic cyst cases reported in the literature
(17), but cases of cysts in the
gastric wall are rare. Gastric bronchogenic cysts exhibit a higher
prevalence in females (female to male ratio, 21:14), with a median
age of development at 43 years old. Only 1 previous case was
reported to be multifocular. Of the cases reported to date, 48.57%
(17/35) were asymptomatic and arbitrarily located (16,18);
however, a number of patients with gastric bronchogenic cysts have
presented with abdominal pain, with or without accompanying
diseases, such as peptic ulcers or cholelithiasis (15).
Gastric bronchogenic cysts are most commonly located
posterior to or on the posterolateral side of the stomach near the
gastroesophageal junction. The size of cyst can vary between 1.7 cm
and 15.0 cm in diameter. Notably, ~80% of gastric duplication cysts
do not locate to, nor interact with the mucosa (19), and only 2 cases of intramucosal cysts
have been reported (20,21). In the remainder of the identified
cases of gastric bronchogenic cysts, the cyst was continuous with
the stomach wall or surrounded by smooth muscle that is continuous
with the muscle of the stomach. With the exception of elevated CA
19–9 levels in 2 of the cases (8,22), other
tumor markers in the majority of cases were all normal, suggesting
that there are no specific tumor markers for this condition.
Postoperatively, the elevated CA 19–9 levels were found to be
normalized. Certain cases also presented with gastric carcinoma
(23,24); chronic inflammation of the gastric
mucosa resulting from the bronchogenic cyst may have caused
adenocarcinoma in the stomach (23).
The present study demonstrated that gastroscopy and imaging
examinations may be able to locate the lesion; however, they cannot
provide qualitative diagnoses. However, Lee et al (25) suggested that when a lesion is
suspected to be a solid tumor on the basis of EUS and CT
investigations and has a positive pillow sign (a surface
indentation observed upon pushing the mass with closed biopsy
forceps), the possibility of a bronchogenic cyst should be
investigated. Several of these lesions are misdiagnosed as solid
mass lesions based on CT and MRI results (26), which may be attributed to the thick
proteinaceous contents of these cysts (27).
Radiographically, bronchogenic cysts are typically
cystic in nature and compress adjacent structures (28). It is difficult to distinguish them
from other cysts solely on the basis of imaging. Ubukata et
al (9) demonstrated that far
greater clarity was achieved when using MRI, as compared with CT,
and emphasized the applicability of this method. In the present
case, the high signal intensity on T1-weighted and T2-weighted
images suggested that the mass contained mucinous or proteinaceous
fluid. EUS is not useful for demonstrating the submucosal location
of the cyst, but it may help to distinguish masses that involve the
posterior stomach from masses associated with the tail of the
pancreas or the left adrenal gland. It has previously been
demonstrated that, when clinically indicated, EUS-fine needle
aspiration (FNA) biopsy can be used in the definitive diagnosis of
gastric bronchogenic cysts (2),
particularly as EUS-FNA has a sensitivity of 93–95%, a diagnostic
rate of 82–86%, and a low complication rate of only 1–3% (29–31).
Such complications include recurrence, ulceration, infection and
hemorrhage. Clinicians should be vigilant for these complications
as they may further complicate surgical intervention due to the
associated adhesion (32). In the 35
cases analyzed in the present study, 3 cases were preoperatively
diagnosed by needle biopsy, whereas the majority of the remaining
cases were misdiagnosed as stromal tumors or other benign lesions
and one previous case was misdiagnosed due to concomitant gastric
carcinoma (23).
When a cyst is enlarged and becomes symptomatic,
surgery can be complicated and hazardous. Furthermore, it has
previously been demonstrated that gastric bronchogenic cysts are
capable of malignant transformation (33–35).
Therefore, resection is recommended once the lesion has been
identified. However, Seddik et al (4) reported a patient with an unchanged
lesion at a 3-year follow-up. Sato et al (29) demonstrated another case which was
diagnosed by endosonography-guided FNA biopsy without surgical
resection. The results of the present literature review suggest
that small and asymptomatic cases should be carefully followed up;
however, for symptomatic cases, such as the one described in the
present case report, resection is recommended. In the present case,
the epigastric pain resulted from the expanding mass pressing on
the cardia, which was misdiagnosed as a stromal tumor due to its
rarity. In order to decrease postoperative complications and
enhance recovery, laparoscopic or endoscopic surgeries remain the
first choice for treatment (36–39).
Care should be taken in order to avoid intraoperative rupture of
the cyst, particularly with infected cysts where postoperative
infectious complications are common. Since the gastric mucosa is
easily injured and anastomosis performed under laparoscopy may
result in postoperative anastomosis leakage, open surgery was
selected in the present case, as the gastric bronchogenic cyst was
located in the submucosa of the cardia.
In conclusion, gastric bronchogenic cysts are rare
and the symptoms are atypical. CT, MRI and EUS-FNA may be
selectively used for evaluation; however, the recommendation of
surgical intervention for asymptomatic cases remains
controversial.
References
|
1
|
Berrocal T, Madrid C, Novo S, Gutiérrez J,
Arjonilla A and Gómez-León N: Congenital anomalies of the
tracheobronchial tree, lung and mediastinum: Embryology, radiology,
and pathology. Radiograhis. 24:e172004.
|
|
2
|
Ko SF, Hsieh MJ, Lin JW, Huang CC, Li CC,
Cheung YC and Ng SH: Bronchogenic cyst of the esophagus: Clinical
and imaging features of seven casese. Clin Imaging. 30:309–314.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Aktoğu S, Yuncu G, Halilcolar H, Ermete S
and Buduneli T: Bronchogenic cysts: Clinicopathological
presentation and treatment. Eur Respir J. 9:2017–2021. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Seddik H, Adyoui T, Rouibaa F, El Hamdi
FZ, Aourarh A, Mahi M, Benkirane A and Zentar A: Gastric
bronchogenic cyst presenting as a submucosal mass: A case report. J
Med Case Rep. 6:262–264. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Dewing SB, Roessel CW and Olmstead EV:
Enterogenous cyst of the stomach wall, a rare benign lesion; case
report. Ann Surg. 143:131–135. 1956. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Haddadin WJ, Reid R and Jindal RM: A
retroperitoneal bronchogenic cyst: A rare cause of a mass in the
adrenal region. J Clin Pathol. 54:801–802. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Jiang L, Jiang L, Cheng N and Yan L:
Bronchogenic cyst of the gastric fundus in a young woman. Dig Liver
Dis. 42:8262010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Tan KK, Nandini CL and Ho CK: A case of
gastric bronchogenic cyst in Singapore with multiple intrigues. ANZ
J Surg. 80:286–287. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ubukata H, Satani T, Motohashi G, Konishi
S, Goto Y, Watanabe Y, Nakada I and Tabuchi T: Intra-abdominal
bronchogenic cyst with gastric attachment: Report of a case. Surg
Today. 41:1095–1100. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yang X and Guo K: Bronchogenic cyst of
stomach: Two cases report and review of the English literature.
Wien Klin Wochenschr. 125:283–287. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Gensler S, Seidenberg B, Rifkin H and
Rubinstein BM: Ciliated lined intramucosal cyst of the stomach:
Case report and suggested embryogenesis. Ann Surg. 163:954–956.
1966. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hedayati N, Cai DX and McHenry CR:
Subdiaphragmatic bronchogenic cyst masquerading as an ‘adrenal
incidentaloma’. J Gastrointest Surg. 7:802–804. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Matsubayashi J, Ishida T, Ozawa T, Aoki T,
Koyanagi Y and Mukai K: Subphrenic bronchopulmonary foregut
malformation with pulmonary sequestration-like features. Pathol
Int. 53:313–316. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Seddik H, Adioui T, Rouibaa F, El Hamdi
FZ, Aourarhz A, Mahi M, Benkirane A and Zentar A: Gastric
bronchogenic cyst presenting as a submucosal mass: A case report. J
Med Case Rep. 6:262–264. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Song SY, Noh JH, Lee SJ and Son HJ:
Bronchogenic cyst of the stomach masquerading as benign stromal
tumor. Pathol Int. 55:87–91. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Melo N, Pitman MB and Rattner DW:
Bronchogenic cyst of the gastric fundus presenting as a
gastrointestinal stromal tumor. J Laparaendosc Adv Surg Tech A.
15:163–165. 2005. View Article : Google Scholar
|
|
17
|
Liang MK, Yee HT, Song JW and Marks JL:
Subdiaphragmatic bronchogenic cysts: A comprehensive review of the
literature. Am Surg. 71:1034–1041. 2005.PubMed/NCBI
|
|
18
|
Shireman PK: Intramural cyst of the
stomach. Hum Pathol. 18:857–858. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Spivak H, Pascal RR, Wood WC and Hunter
JG: Enteric duplication presenting as cystic tumors of the
pancreas. Surgery. 121:597–600. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Laraja RD, Rothenberg RE, Chapman J,
Imran-ul-Haq and Sabatini MT: Foregut duplication cyst: A report of
a case. Am Surg. 61:840–841. 1995.PubMed/NCBI
|
|
21
|
Rubio CA, Orrego A and Willén R:
Congenital bronchogenic cyst in the gastric mucosa. J Clin Pathol.
58:3352005.PubMed/NCBI
|
|
22
|
Ikehata A and Sakuma T: Gastric
duplication cyst with markedly elevated concentration of
carbohydrate antigen 19-9. Am J Gastroenterol. 95:842–843. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Shibahara H, Arai T, Yokoi S and Hayakawa
S: Bronchogenic cyst of the stomach involved with gastric
adenocarcinoma. Clin J Gastroenterol. 2:80–84. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Murakami S, Isozaki H, Shou T, Sakai K and
Toyota H: Foregut duplication cyst of the stomach with
pseudostratified columnar ciliated epithelium. Pathol Int.
58:187–190. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Lee SH, Park DH, Park JH, Kim HS, Park SH,
Kim SJ and Oh MH: Endoscopic Mucosal resection of a gastric
bronchogenic cyst that was mimicking a solid tumor. Endoscopy.
38(Suppl 2): E12–E13. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Fazel A, Moezardalan K, Varadarajulu S,
Draganov P and Eloubeidi MA: The utility and the safety of
EUS-guided FNA in the evaluation of duplication cysts. Gastrointest
Endosc. 62:575–580. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Wiech T, Walch A and Werner M:
Histopathological classification of nonneoplastic and neoplastic
gastrointestinal submucosal lesions. Endoscopy. 37:630–634. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Sashiyama H, Miyazaki S, Okazaki Y, Kaiho
T, Nakajima Y, Hoshino T, Akai T, Nabeya Y, Funami Y, Shimada H, et
al: Esophageal bronchogenic cyst successfully excised by endoscopic
mucosal resection. Gastrointest Endosc. 56:141–145. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Sato M, Irisawa A, Bhutani MS, Schnadig V,
Takagi T, Shibukawa G, Wakatsuki T, Imamura H, Takahashi Y, Sato A,
et al: Gastric bronchogenic cyst ciagnosed by endosonographically
guided fine needle aspiration biopsy. J Clin Ultrasound.
36:237–239. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Matsui M, Goto H, Niwa Y, Arisawa T,
Hirooka Y and Hayakawa T: Preliminary results of fine needle
aspiration biopsy histology in upper gastrointestinal submucosal
tumors. Endoscopy. 30:750–755. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
O'Toole D, Palazzo L, Arotçarena R,
Dancour A, Aubert A, Hammel P, Amaris J and Ruszniewski P:
Assessment of complications of EUS-guided fine-needle aspiration.
Gastrointest Endosc. 53:470–474. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Vos CG, Hartemink KJ, Golding RP,
Oosterhuis JW and Paul MA: Bronchogenic cysts in adults: Frequently
mistaken for a solid mass on computed tomography. Wien Klin
Wochenschr. 123:179–182. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Endo C, Imai T, Nakagawa H, Ebina A and
Kaimori M: Bronchioloalveolar carcinoma arising in a bronchogenic
cyst. Ann Thorac Surg. 69:933–935. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Sullivan SM, Okada S, Kudo M and Ebihara
Y: A retroperitoneal bronchogenic cyst with malignant change.
Pathol Int. 49:338–341. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Kuraoka K, Nakayama H, Kagawa T, Ichikawa
T and Yasui W: Adenocarcinoma arising from a gastric duplication
cyst with invasion to the stomach: A case report with literature
review. J Clin Pathol. 57:428–431. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Kurokawa T, Yamamoto M, Ueda T, Enomoto T,
Inoue K, Uchida A, Kikuchi K and Ohkohchi N: Gastric bronchogenic
cyst histologically diagnosed after laparoscopic excision: Report
of a case. Int Surg. 98:455–460. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Wakabayashi H, Okano K, Yamamoto N, Suzuki
Y, Inoue H, Kadota K and Haba R: Laparoscopically resected foregut
duplication cyst (bronchogenic) of the stomach. Dig Dis Sci.
52:1767–1770. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Ballehaninna UK, Shaw JP and Brichkov I:
Subdiaphragmatic bronchogenic cyst at the gastroesophageal junction
presenting with Dysphagia: A case report. Surg Laparosc Endosc
Percutan Tech. 23:e170–e172. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Díaz Nieto R, Naranjo Torres A, Gómez
Alvarez M, Ruiz Rabelo JF, Pérez Manrique MC, Ciria Bru R, Valverde
Martínez A, de la Roldán Rúa J, Alonso Gómez J and Rufián Peña S:
Intra abdominal bronchogenic cyst. J Gastrointest Surg. 14:756–758.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Braffman B, Keller R, Gendal ES and Finkel
SI: Subdiaphragmatic bronchogenic cyst with gastric communication.
Gastrointest Radiol. 13:309–311. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Takahara T, Torigoe T, Haga H, Yosida I,
Takeshima S, Sano S, Ishii Y, Furuya T, Nakamura E and Ishikawa M:
Gastric duplication cyst: Evaluation by endoscopic ultrasonography
and magnetic resonance imaging. J Gastroenterol. 31:420–424. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Kim JH, Kim JS, Nam ES and Shin HS:
Foregut duplication cyst of stomach. Pathol Int. 50:142–145. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Rubio CA, Orrego A and Willen R:
Bronchogenic gastric cyst. A case report. In Vivo. 19:383–385.
2005.PubMed/NCBI
|
|
44
|
Cunningham SC, Hansel DE, Fishman EK and
Cameron JL: Foregut duplication cyst of the stomach. J Gastrointest
Surg. 10:620–621. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Theodosopoulos T, Marinis A, Karapanos K,
Vassilikostas G, Dafnios N, Samanides L and Carvounis E: Foregut
duplication cysts of the stomach with respiratory epithelium. World
J Gastroentero. 113:1279–1281. 2007. View Article : Google Scholar
|
|
46
|
Mardi K, Kaushal V and Gupta S: Foregut
duplication cysts of stomach masquerading as leiomyoma. Indian J
Pathol Microbiol. 53:160–161. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Khoury T and Rivera L: Foregut duplication
cysts: A report of two cases with emphasis on embryogenesis. World
J Gastroenterol. 17:130–134. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Jiang W, Zhang B, Fu YB, Wang JW, Gao SL,
Zhang SZ and Wu YL: Gastric duplication cyst lined by
pseudostratified columnar ciliated epithelium: A case report and
literature review. J Zhejiang Univ Sci B. 12:28–31. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Hosomura N, Kono H, Kawaida H, Amemiya H,
Itakura J and Fujii H: A case of foregut gastric duplication cyst
with pseudostratified columnar ciliated epithelium. Clin J
Gastroenterol. 5:82–87. 2012. View Article : Google Scholar : PubMed/NCBI
|