Introduction
Chronic myelocytic leukemia (CML), which is also
known as chronic granulocytic leukemia, is a relatively rare
malignant tumor that affects blood and bone marrow. CML is most
common in older adults and among men. Based on the cases reported
between 2009 and 2013, the number of new cases of CML was
1.8/100,000 individuals per year, whereas the number of deaths was
0.3/100,000 individuals per year (1). These rates are age-adjusted, and the
mortality rates from CML are highest among individuals aged 75–84
(1). Adequate supportive care and
the initiation of imatinib mesylate have been essential in securing
the recent favorable prognosis of patients with CML (2). CML is a clonal myeloproliferative
disorder of hematopoietic stem cells characterized by the
reciprocal translocation t (9; 22) (q34; q11), termed the
Philadelphia chromosome (Ph) (3).
The resulting breakpoint cluster region-abelson 1 (BCR-ABL1)
oncogene has deregulated tyrosine kinase activity (3), which produces a constitutive
proliferative signal that is responsible for the transformed
phenotype of CML cells. CML is estimated to account for 15–20% of
adult leukemias (1). The
age-adjusted annual incidence rate is 1.6 cases per 100,000
individuals, and the median age at diagnosis is 65 years, with a
slight male predominance (1). CML is
characterized by the generation of a large number of immature white
blood cells that accumulate inside the bone marrow, and suppress
the normal hematogenesis of bone marrow. In addition, the
aforementioned cells are able to diffuse into the entire body
through the blood circulation, leading to anemia, easy bleeding,
infection and organ infiltration; thus, patients frequently present
with such systemic manifestations, such as fever, fatigue, anemia
and hepatosplenomegaly, as the initial symptoms. Consequently, the
current case involving a patient with CML initially treated for
visual impairment in the Department of Ophthalmology at the Rizhao
People's Hospital (Rizhao, China), required the ophthalmologists to
be familiar with the ocular manifestations of such diseases as CML,
particularly the appearance of fundus lesions. Thus,
ophthalmologists should be able to identify such diseases in order
to reduce the rate of misdiagnosis and missed diagnosis of diseases
in clinical work. The current authors treated a patient with CML
with fundus lesion on December 4th 2011, and the diagnosis and
treatment are reported herein.
Case report
The current study was conducted in accordance with
the declaration of Helsinki, and was conducted with approval from
the Ethics Committee of Rizhao People's Hospital. Written informed
consent was obtained from the patient. A male patient, 23
years-of-age, visited the Department of Ophthalmology at the Rizhao
People's Hospital as a result of a dark shadow in the front of the
right eye, accompanied with blurred vision for 3 days, on December
4th, 2011. The patient had a history of occasional gingival
bleeding for the previous 2 years, and a recurrent upper
respiratory tract infection for 1 year; the latter of which was
present 1 week prior to the patient's hospital visit. The patient's
symptoms were improved following the oral administration of
Bufferin caplets (0.5 mg; Bristol-Myers Squibb Co., New York City,
NY, USA); however, the patient still felt malaise. Systemic
examination revealed mild anemia, and the skin and mucous membranes
of the entire body indicated no jaundice or bleeding spots;
however, several enlarged lymph nodes were palpable in the
bilateral neck, and the liver could not be felt under the ribs. In
addition, the spleen displayed swelling that reached four fingers
under the rib. The remaining examinations indicated no concerning
results. Eye examination provided the following results: Visual
acuity of the right eye, 0.4, J3; visual acuity of left eye, 0.6,
J2. The results of the intraocular pressure (IOP) assessment were
as follows: Right eye, 19.6 mmHg (1 mmHg = 0.133 kPa); left eye,
18.5 mmHg. The extraocular condition of both eyes was normal.
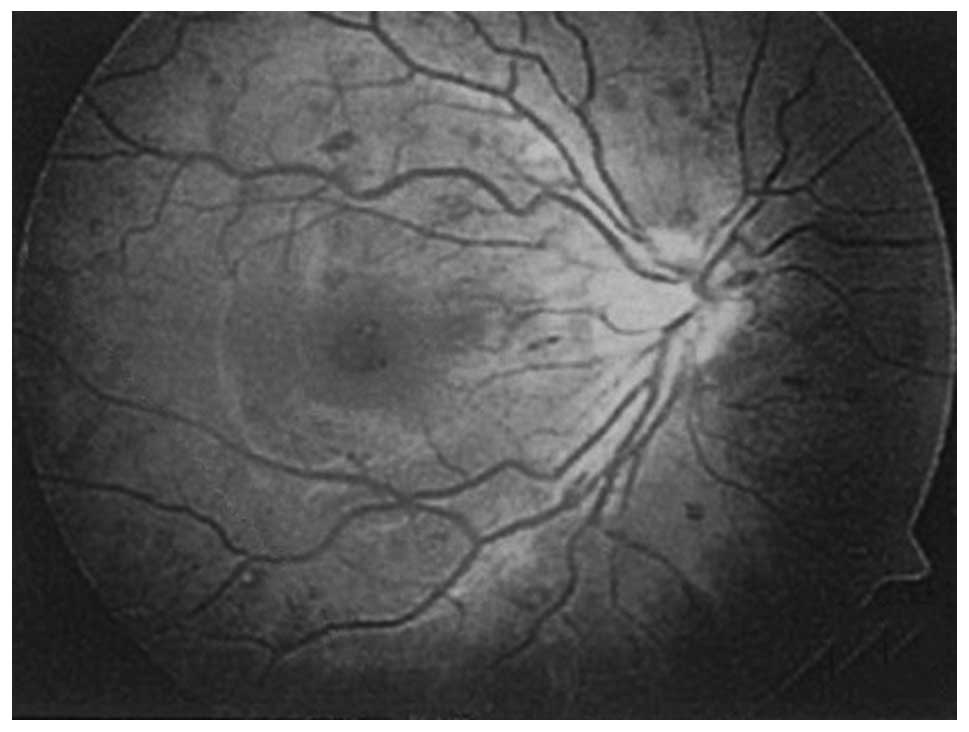
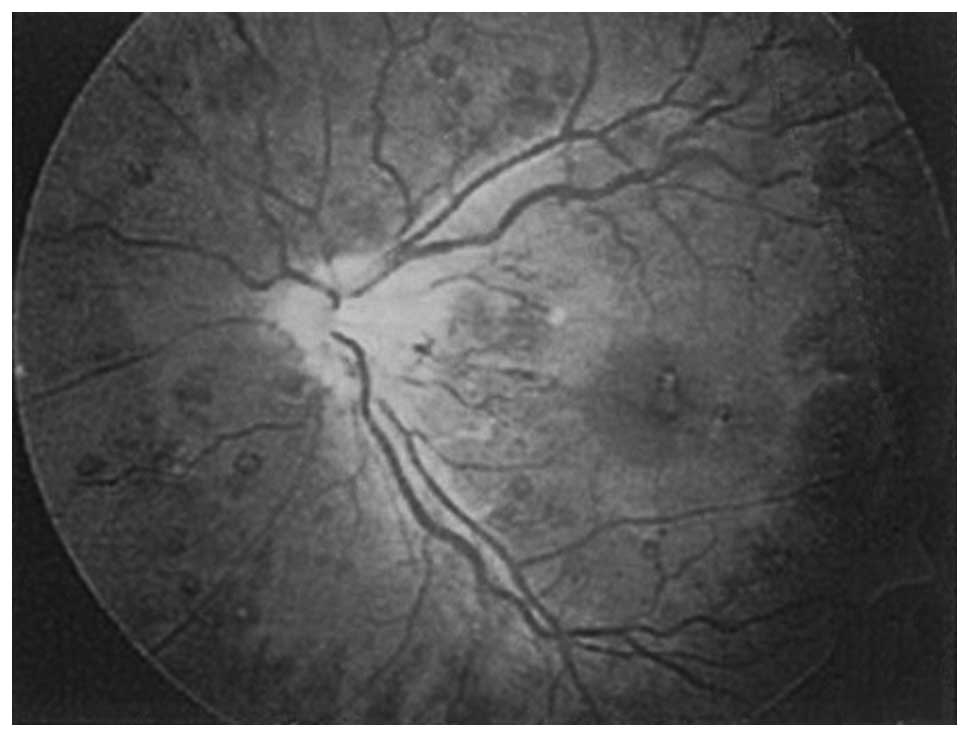
Fundus examination revealed the following: Mild binocular papillary
edema; the optic papilla boundary was less clear; the cup/disc
ratio was 0.4; the retinal arteries exhibited no abnormalites; the
veins were dilated tortuously; artery: vein = 1:2; the central
fovea of macula exhibited yellow patches and bleeding spots; the
light reflex of the central fovea disappeared; and the entire
retina exhibited a large quantity of scattered dark red bleeding
spots, which were uneven in size, the smallest of which was equal
to the vessel diameter, while the largest one was ~1/4 of the optic
nerve's diameter. White spots were present in the center of
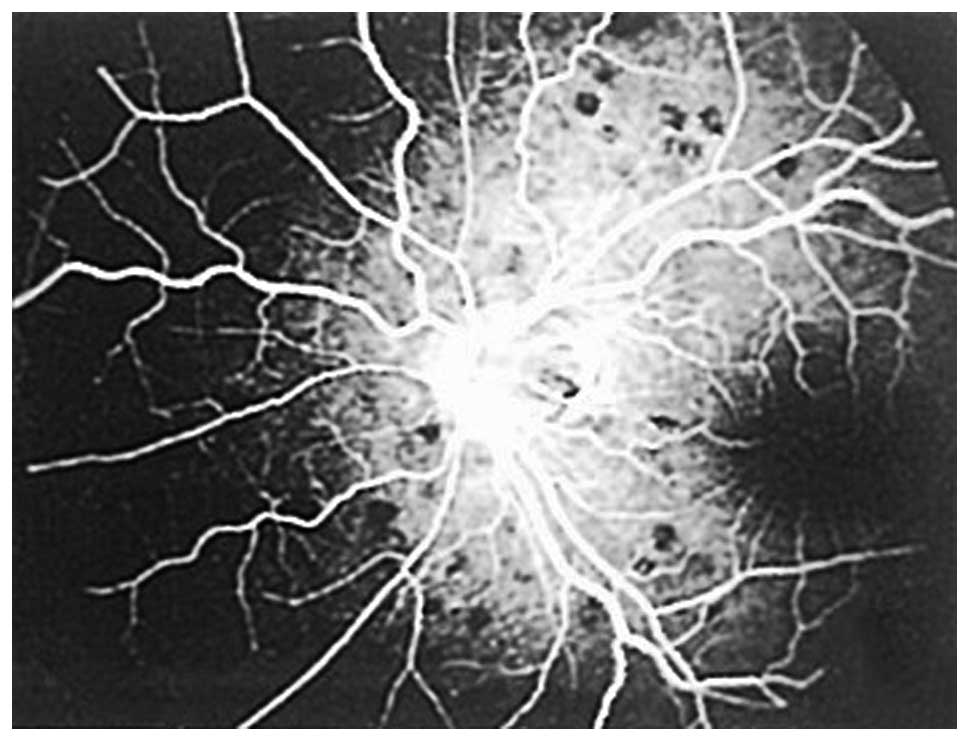
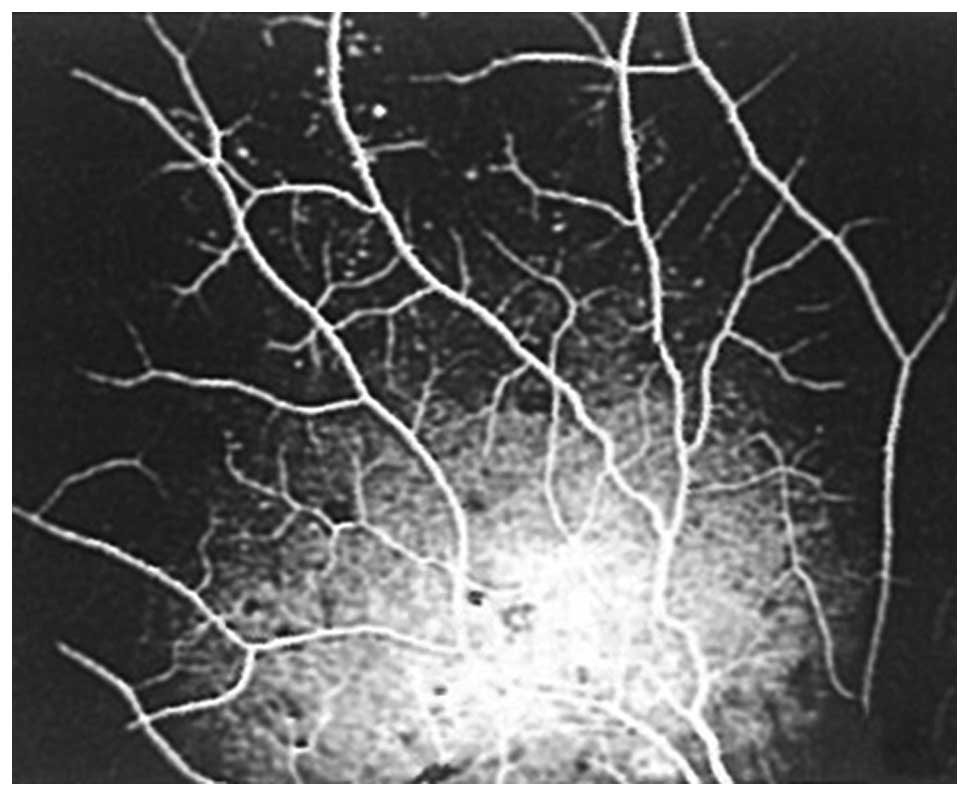
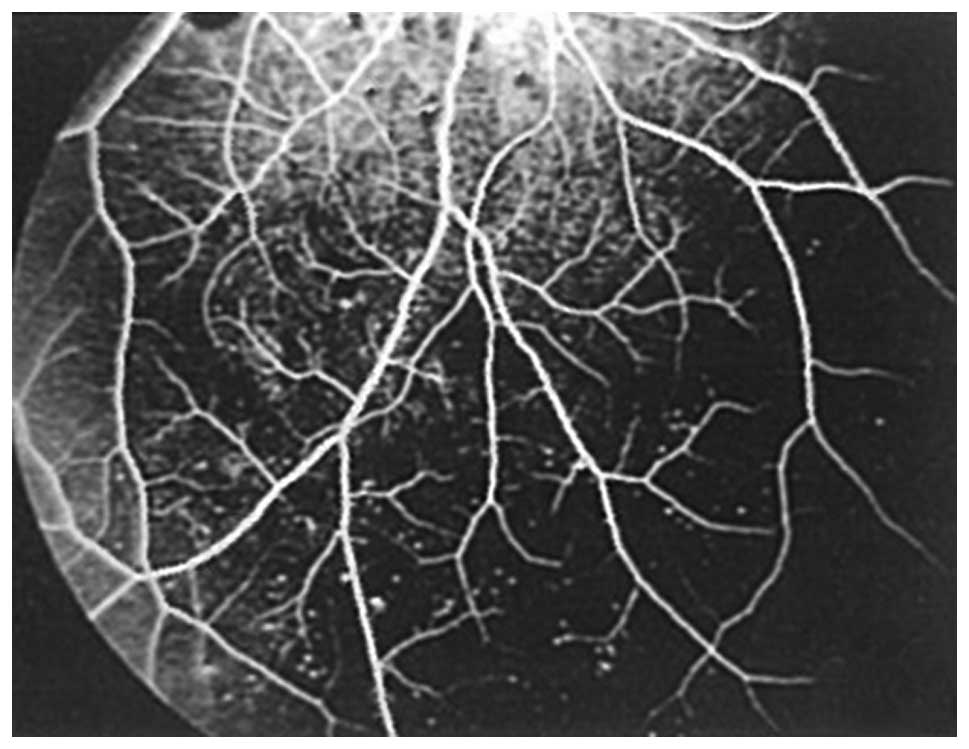
bleeding spots, and exhibited the typical Roth spots (Figs. 1 and 2). Fundus fluorescein angiography
identified the following: Numerous scattered bleeding spots on the
binocular retina that covered the fluorescence; the center of the
bleeding spots exhibited highly-fluorescent pale white spots
(Figs. 3 and 4); the binocular midperiphery and the
surrounding area had scattered capillary hemangioma-like high
fluorescent spots (Figs. 5 and
6); the retinal veins were tortuous
and dilated; and the macula lutea exhibited leakage of fluorescein.
The results of laboratory assessments were as follows: White blood
cell count, 420×109/l; rod neutrophils, 13%; segmented
neutrophils, 49%; promyelocytes, 2%; myelocytes, 30%;
metagranulocytes, 2%; hemoglobin, 84 g/l; platelet count,
544×109/l, hematocrit, 0.242; sedimentation rate of
erythrocyte, 18 mm/h; and lactate dehydrogenase, 860 IU/l.
Thus, following the confirmation of a
leukemia-caused fundus lesion, the patient was transferred to the
Department of Hematology at the same institution for subsequent
treatment. Abdominal ultrasound examination indicated that the left
lobe of the liver was 8.5 cm, the right lobe of the liver was 13.5
cm, the echo was uniform and the vascular textures were clear; the
spleen was obviously enlarged, with a spleen thickness of 7.0 cm,
and a length of 4.2 cm under the ribs. Bone marrow biopsy revealed
that the proliferation of bone marrow cells was hyperactive, and
the ratio of myeloid and erythroid cells was 37.8:1. The total
number of myeloblasts was 92.5%, among which the original
myeloblasts accounted for 2%, the promyelocytes accounted for 8%,
eosinophils accounted for 8%, basophils accounted for 0.5% and
myelocytes accounted for 22.5%. Other cell types were inhibited;
megakaryocytes demonstrated hyperactive proliferation, with 5%
being mature cells, and platelet aggregation was also observed.
The patient was diagnosed with CML, and therefore,
was admitted into the Department of Hematology for treatment with
interferon (3×106 IU/m2/d; Beijing Kawin
Technology Co., Ltd., Beijing, China) via intramuscular injection
thrice a week, oral hydroxyurea (30 mg/kg; Qilu Pharmaceutical,
Co., Ltd., Shandong, China) twice a week, and imatinib mesylate
(400 mg; Chia Tai Tianqing Pharmaceutical Group Co., Ltd., Hong
Kong, China) once daily. After 1 week the patient's condition was
markedly improved, and a blood re-examination revealed the
following: White blood cell count, 10×109/l; rod
neutrophils, 12%; segmented neutrophils, 53%; myelocytes, 2%;
metagranulocytes, 2%; hemoglobin, 84 g/l; and platelet count,
198×109/l. Fundus examination revealed that the small,
sporadic and patch-like bleeding on the binocular eyeground had
been removed, while a number of larger Roth spots remained. The
patient remains in a stable condition under treatment with imatinib
mesylate, although his dosage has decreased to 300 mg once daily.
Blood examinations, including routine blood analysis and hepatic
and renal function are performed once a month. Bone marrow biopsy
for bone marrow smear, and tests for the mutation in BCR-ABL kinase
domain and chromosome are performed every 3–4 months. To date, the
findings of these tests have demonstrated that the patient is in a
stable condition.
Discussion
The natural history of CML in the absence of
treatment is characterized by a triphasic course comprising of a
chronic phase (CP)-CML, followed by an accelerated phase and
invariably, progression to a final fatal blastic phase of an
undefined duration of time (4). The
prompt recognition of the patient's ocular fundus symptoms and
early referral to oncologists for adequate management may have been
a primary factor in determining the long-term outcome, as patients
with CP-CML at the time of diagnosis have the best long-term
prognosis with treatment (4).
Previously, CML was incurable with conventional
chemotherapy. However, the treatment strategies for CML have
undergone revolutionary developments in the previous decade,
predominantly due to an increased understanding of its molecular
pathogenesis. The BCR-ABL1 fusion protein has been the target for
drug design and therapies for CML, which have enabled the
development of effective tyrosine kinase inhibitors (TKIs) that
have the potential to eradicate the Ph chromosome-positive clone
(2). Imatinib mesylate is a first
generation TKI approved by the United States Food and Drug
Administration in 2001, and has become the initial treatment of
choice for the majority of patients with CML (2), as it results in a marked increase in
the long-term survival and preservation of an acceptable quality of
life (5).
Patients with leukemia typically present with fever,
fatigue, anemia and hepatosplenomegaly as the initial symptoms, and
eye-related symptoms are uncommon (6). Therefore, identification of leukemic
patients is seldom a result of ocular inspections. The fundus of
patients with leukemia may have lesions, which are generally more
common in acute myelocytic leukemia (7). Abu el-Asrar et al (8) reported 74 cases of acute leukemia,
which included 32 patients with retinopathy, accounting for 43%
(8). A further study reported the
prevalence as 35% (9). Thus,
patients with the binocular tortuous and dilated retinal veins, and
those with numerous Roth plaques, should be assessed for the
possibility of leukemia. In the present study, the white spots in
the patient's bleeding center were small, whereas had a greater
quantity of blood been present, the patient may have been
misdiagnosed with non-ischemic retinal vein occlusion. A case of
leukemia-induced retinal vein occlusion has also been reported
(10). Compared with the
aforementioned case (leukemia-induced retinal vein occlusion), and
the symptoms of the disease remitted subsequent to treatment,
preventing the occurrence of retinal vein occlusion, the patient in
the present study was identified to have CML at an earlier stage.
It has been reported that the occurrence of central retinal vein
thrombosis in patients with CML is not associated with an increase
of blood viscosity, but is associated with the increase of
anti-cardiolipin antibodies (10).
This is notable as, although central retinal vein thrombosis is not
a common symptom in CML, the fundal appearance of CML in the
present case was similar to the appearance of central retinal vein
thrombosis; therefore, comparable cases may be misdiagnosed as
non-schemic retinal vein occlusion.
Roth spots are considered to be the characteristic
pathological change of subacute bacterial endocarditis. Bleeding
spots with a white center are a non-specific symptom caused by the
rupture of retinal capillaries and the aggregation of fibrins and
platelets. Clinically, numerous diseases are associated with the
presence of Roth spots, which are predominantly detected in
patients with subacute bacterial endocarditis, septicemia,
toxoplasmosis, AIDS, leukemia, diabetes, hypertension, vasculitis
and traumatic brain injuries in infants. Therefore, upon the
detection of Roth spots, clinicians must perform further
assessments to identify the relevant disease (11–14).
The occurrence of retinal hemorrhage in patients
with leukemia is associated with a significant reduction in
hemoglobin and hematocrit, while an increase in the number of
leukocytes is significantly associated with the appearance of Roth
spots (8). The patient in the
present case exhibited hemoglobin levels of 84 g/l, whilst the
hematocrit decreased to 0.242, and the white blood cell count
increased to 420×109/l. In addition, the binocular
retina had a large number of bleeding spots, and all bleeding spots
had a white center. Specchia et al (15) reported that patients with leukemia
who had retinopathy exhibited an increased level of blood lactate
dehydrogenase, with an average of 812 IU/l, whilst patients who did
not have retinopathy displayed a mean blood lactate dehydrogenase
level of 607 IU/l. The blood lactate dehydrogenase level of the
current patient was increased to 860 IU/l (normal range, 100–300
IU/l), which was consistent with the literature (15). With regards to the prognosis of CML,
certain studies have reported that acute leukemic patients over 40
years-of-age with cotton wool spots in the fundus had a worse
prognosis, and the impact of cotton wool spots was greater than
that of age in terms of prognosis (9). Retinopathy is an important clinical
manifestation that determines poor prognosis in patients in the
remission period. The complete remission rate and survival rate of
young patients who do not have retinopathy are significantly higher
than those of older patients with retinopathy (15). CML in the patient in the current
study was detected at an early stage, and no cotton wool spots were
observed in the fundus. Subsequent to treatment, the retinal
hemorrhage was reduced, the white blood cell count was
significantly decreased and the systematic symptoms were
significantly improved. This indicates a good prognosis.
In summary, ophthalmologists should consider a
thorough systemic evaluation of patients with binocular tortuous
and dilated retinal veins, in addition to those with several Roth
plaques, as this may be an initial indicator of CML. As a
corollary, the authors suggest to clinicians that all patients with
newly diagnosed leukemia of any type be referred for ocular
examination, regardless of whether they are symptomatic. A timely
diagnosis, adequate supportive care and the initiation of imatinib
mesylate have been essential for securing a favorable prognosis in
the current patient.
References
|
1
|
Howlader N, Noone AM, Krapcho M, Neyman N,
Aminou R, Waldron W, Altekruse SF, Kosary CL, Ruhl J, Tatalovich Z,
et al: SEER Cancer Statistics Review, 1975-2009 (Vintage 2009
Populations). National Cancer Institute; Bethesda, MD:
(seer.cancer.gov/csr/1975_2009_pops09/). Accessed. September.
2013
|
|
2
|
Baccarani M, Cortes J, Pane F,
Niederwieser D, Saglio G, Apperley J, Cervantes F, Deininger M,
Gratwohl A, Guilhot F, et al: Chronic myeloid leukemia: An update
of concepts and management recommendations of European Leukemia
Net. J Clin Oncol. 27:6041–6051. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Quintás-Cardama A and Cortes J: Molecular
biology of bcr-abl1-positive chronic myeloid leukemia. Blood.
113:1619–1630. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Cortes J: Natural history and staging of
chronic myelogenous leukemia. Hematol Oncol Clin North Am.
18:569–584. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
GambacortiPasserini C, Antolini L, Mahon
FX, Guilhot F, Deininger M, Fava C, Nagler A, Della Casa CM, Morra
E, Abruzzese E, et al: Multicenter independent assessment of
outcomes in chronic myeloid leukemia patients treated with
imatinib. J Natl Cancer Inst. 103:553–561. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Huang PK and Sanjay S: Visual disturbance
as the first symptom of chronic myeloid leukemia. Middle East Afr J
Ophthalmol. 18:336–338. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Vrcek I, Finnerty K, Ford P, Hogan RN and
Mancini R: Relapsing acute lymphoblastic leukemia presenting with a
rapidly enlarging and vision-threatening orbital mass. Int
Ophthalmol. 35:257–260. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Abuel-Asrar AM, Al-Momen AK, Kangave D,
Harakati MS and Ajarim DS: Correlation of fundus lesions and
hematologic findings in leukemic retinopathy. Eur J Ophthalmol.
6:167–172. 1996.PubMed/NCBI
|
|
9
|
Abuel-Asrar AM, Al-Momen AK, Kangave D and
Harakati MS: Prognostic importance of retinopathy in acute
leukemia. Doc Ophthalmol. 91:273–281. 1995-1996. View Article : Google Scholar
|
|
10
|
AlAbdulla NA, Thompson JT and La Borwit
SE: Simultaneous bilateral central retinal vein occlusion
associated with anticardiolipin antibodies in leukemia. Am J
Ophthalmol. 132:266–268. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Fred HL: Little black bags, ophthalmoscopy
and the Roth spot. Tex Heart Inst J. 40:115–116. 2013.PubMed/NCBI
|
|
12
|
Ling R and James B: White centered retinal
haemorrhages (Roth spots). Postgrad Med J. 74:581–582. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Falcone PM and Larrison WI: Roth spots
seen on ophthalmoscopy: Diseases with which they may be associated.
Conn Med. 59:271–273. 1995.PubMed/NCBI
|
|
14
|
Reddy SC and Jackson N: Retinopathy in
acute leukaemia at initial diagnosis: Correlation of fundus lesions
and haematological parameters. Acta Ophthalmol Scand. 82:81–85.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Specchia G, Albano F, Guerriero S,
Buquicchio C, Pomes L, Pastore D, Carluccio P, Delle Noci N and
Liso V: Retinal abnormalities in newly diagnosed adult acute
myeloid leukemia. Acta Haematol. 105:197–203. 2001. View Article : Google Scholar : PubMed/NCBI
|