Introduction
Mediastinal syndromes are a group of disorders
characterized by infiltration, entrapment or compression of
mediastinal structures. The mediastinum is anatomically divided
into the anterior, medium and posterior regions. Symptoms of the
syndromes are associated with the anatomic structures involved; the
compression of the trachea results in dyspnea and respiratory
insufficiency, whereas compression of the esophagus results in
dysphagia. The superior vena cava (SVC) and nerves can become
trapped, resulting in vein distention, edema of the face or upper
extremities, and nervous system symptoms (1). Mediastinal syndrome can be due to
malignant or non-malignant conditions. Malignant health conditions
generally include lymphomas, thymomas, germ cell tumors, thyroid
neoplasms and metastases from serous or mucinous tumors, as ovary,
gastrointestinal tract or small cell lung cancer (1,2).
Non-malignant causes include goiter and large aortic aneurisms.
Generally, 3–6% of mediastinal anterior masses are represented by
intrathoracic goiter and 5–17% are carcinomas (1). Superior vena cava syndrome is the most
severe complication of mediastinal syndromes and is considered to
be a medical emergency (1,2). In addition, pulmonary cancer is the
most common cause of mediastinal syndrome. Treatment of mediastinal
syndrome involves chemotherapy and radiation, radiation alone or
surgery according to the etiology. Supportive therapies may help
manage this syndrome, however, the prognosis, depending on the type
of malignancy, is poor in the majority of cases (1,2). A total
of 40% of patients diagnosed with lung cancer have signs and
symptoms of mediastinal syndrome (3). Furthermore, lung cancer accounts for
46–75% of all cases of SVC obstruction (4). In the present study, three rare causes
of mediastinal syndrome in three respective cases are
discussed.
Case report
Case 1
A 85-year-old female was transferred on the 14th of
January, 2014 to the Department of Clinical Medicine and
Rheumatology, Campus Bio-Medico University of Rome (Rome, Italy)
with acute respiratory failure and pneumonia. Arterial blood gas
(ABG) analysis showed the following: pH, 7.43; pO2, 54
mmHg; pCO2, 40 mmHg; and HCO3, 28 mmol/l, and
pneumonia. Venous blood tests demonstrated the following:
Hemoglobin (Hb), 11.6 g/dl; platelets, 166,000 cells/µl; white
blood cell (WBC), 6,490 cells/µl (neutrophils, 4,860 cells/µl;
lymphocytes, 860 cells/µl); and creatinine, 0.84 mg/dl. Following
admission, oxygen therapy using a Venturi mask (40%) at 8 l/min and
antibiotic therapy using piperacilline/tazobactam (4.5 g three
times a day) were administered intravenously. The patient's medical
history included several years of follow-up for a thyroid goiter;
however, computed tomography (CT) analysis of the neck demonstrated
a multinodular goiter in the mediastinum with severe compression of
the tracheal lumen that appeared markedly reduced in size and was
deformed in a way that it resembled a mouse tail (Fig. 1). In addition, a sliding gastric
hiatal hernia resulted in compression of the anterior-medial part
of the left inferior lobe. This induced marked dilation of the
esophageal lumen with ‘air-fluid level’.
Due to the severe clinical condition of the patient,
surgical aspiration of the goiter was performed without any
complications. Clinical conditions improved a few days after the
surgery. ABG analysis at discharge demonstrated the following: pH,
7.44; pO2, 85 mmHg; pCO2, 26 mmHg; and
HCO3, 24 mmol/l. Oxygen therapy was reduced and
subsequently discontinued, and the patient was discharged on the
2nd of February, 2014 and referred to a long-term care
provider.
Case 2
A 21-year-old male was admitted on the 17th of
April, 2014 to the Department of Clinical Medicine and
Rheumatology, Campus Bio-Medico University of Rome with fatigue,
fever and a voluminous painless neck mass. The patient was referred
on May 2, 2014 to hematologists. Venous blood tests showed the
following: Hb, 12.6 g/dl; platelets, 428,000 cells/µl; WBC, 12,460
cells/µl (neutrophils, 10,370 cells/µl; lymphocytes, 690 cells/µl;
macrophages, 1,240 cells /µl) and erythrocyte sedimentation rate,
120 mm/h. CT examination identified a voluminous solid mass with
spiculated margins and internal necrosis, localized on the left
anterior superior mediastinum. This mass caused severe compression
of the left lung apex and jugular vein (Fig. 2). Subsequent echocardiography
demonstrated pericardial effusion. A biopsy of the mass was
performed with a menghini needle (Hepafix, B. Braun, Melsungen,
Germany). The specimen was formalin-fixed and paraffin-embedded; 3
mm thick sections were cut and stained with H&E and observed
with a BX51 light microscope (Olympus Corporation, Tokyo, Japan).
Histochemical and immunophenotypic analyses were performed on
additional sections. Histological examination revealed an
unclassifiable B-cell lymphoma, with features that were indicative
of diffuse large B-cell lymphoma and classical Hodgkin's lymphoma
stage IIB (5). The patient was
subsequently referred to hematologists on May 13th and began a
bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine,
procarbazine and prednisone chemotherapy regimen. The patient had
four cycles of chemotherapy, and the control positron emission
tomography comparison demonstrated a reduction of the mediastinal
mass.
Case 3
A 63 year-old male, suffering from an operated
gastric tumor, was admitted on 21st of November, 2013 to the
Department of Clinical Medicine and Rheumatology, Campus Bio-Medico
University of Rome with lobar pneumonia of the right lung, and
bilateral pleural effusions. In addition, the patient presented
with severe dyspnea and edema of the neck and the face. ABG
analysis demonstrated the following: pH, 7.45; pO2, 53
mmHg; pCO2, 34 mmHg; sO2, 88%; and
HCO3, 25 mmol/l. Venous blood tests results were as
follows: Creatinine, 1.5 mg/dl; Hb, 17.2 g/dl; WBC, 12,120
cells/µl, neutrophils, 10,740 cells/µl; lymphocytes, 589 cells/µl;
and platelets, 189,000 cells/µl.
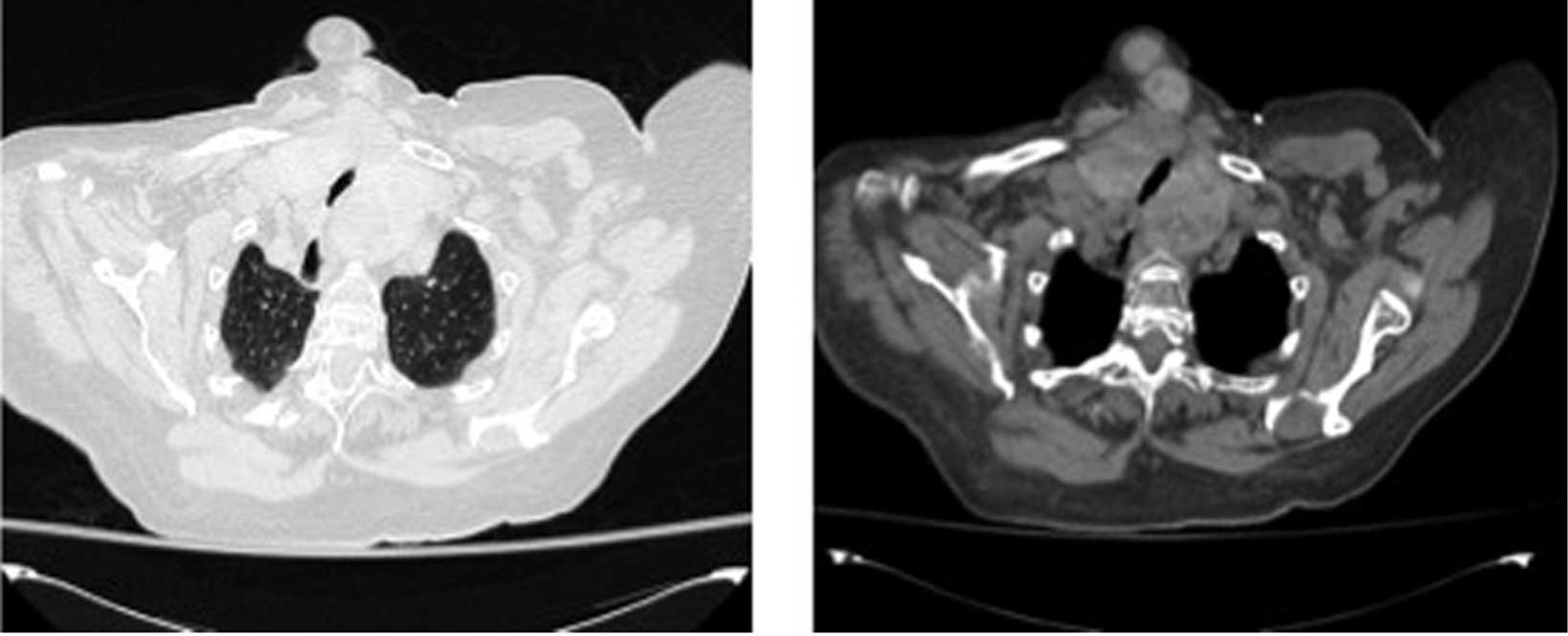
CT examination showed multiple mediastinal lymph
nodes with internal liquefactive necrotic phenomena;
lymphadenopathy was extended to the bronchovascular structures and
to the esophagus, causing a significant reduction in the diameter
of the tracheal lumen on the superior mediastinum (Fig. 3). In addition, CT indicated
compression of the SVC, infiltration of the right pulmonary artery,
moderate pericardial effusion and bilateral pleural effusion
(Fig. 3). The patient was
administered palliative care, including physiologic salt solution,
and morphine (4 mg; Mundipharma Pharmaceuticals srl, Milan, Italy)
and methylprednisolone (40 mg; Pfizer srl, Milan, Italy)
intravenously. The patient succumbed to acute respiratory failure
after 4 days.
Discussion
Mediastinal syndromes include a group of syndromes
characterized by the compression of mediastinal structures. Causes
of mediastinal syndromes are classified according to the anatomic
division of the mediastinum, including the anterior, medium and
posterior regions (Table I)
(1,2). Typically, 3–6% of mediastinal anterior
masses are represented by intrathoracic goiter, and 5–17% are
carcinomas (1). The most severe
complication of mediastinal syndrome is SVC syndrome (6), which affected the patient in case
3.
 | Table I.Causes of mediastinal syndrome based
on anatomical divisions of the mediastinum. |
Table I.
Causes of mediastinal syndrome based
on anatomical divisions of the mediastinum.
| Anterior
mediastinum | Medium
mediastinum | Posterior
mediastinum |
|---|
| Aneurysm | Bronchogenic
cyst | Aneurysm |
| Angiomatous
tumor | Bronchogenic
tumor | Bronchogenic
tumor |
| Goiter | Lymph node
hyperplasia | Esophageal
diverticular |
| Lipoma | Lymphoma | Esophageal tumor |
| Lymphoma | Pleuropericardial
cyst | Neurogenic tumor |
| Morgagni hernia | Vascular masses | Parathyroid
tumor |
| Pericardial cyst |
|
|
| Teratoma |
|
|
| Thymoma |
|
|
| Thyroid tumor |
|
|
As observed in case 1, intrathoracic goiter is
typically a multinodular benign disease (thyroid cancer is only
identified in 2.5–16% of cases) (7)
that may become a life-threatening condition when it causes the
obstruction of respiratory and neurovascular structures (1). It is understood that 80% of
intrathoracic goiters are located in the anterior mediastinum, as
was observed in case 1, whereas 10–15% are situated in the
posterior mediastinum (8). In case
1, mediastinal syndrome was life threatening due to severe tracheal
lumen compression, which lead to acute respiratory insufficiency.
Following thyroidectomy, the patient experienced rapid clinical
benefit, and dyspnea and respiratory insufficiency ceased. In this
case, a surgical approach was the preferable option, particularly
in the absence of contraindications, as intrathoracic goiter can
represent an emergency. Short-term complications of intrathoracic
goiter include the development of severe acute respiratory failure
that may require intubation, whereas long-term complications
include the development of thyroid cancer (8).
Case 2 described a young male affected by lymphoma.
Hodgkin's lymphoma predominantly affects the mediastinum in 50–70%
of patients, compared with 20% of those with non-Hodgkin's lymphoma
(2,9). If the lymphoma is bulky, it compresses
the trachea, heart, esophagus and large vessels (2); therefore, symptoms are dependent on the
anatomical structures involved (2).
Histological analysis of the patient in case 2 resulted in a
diagnosis of bulky unclassifiable B-cell lymphoma, with features
intermediate between diffuse large B-cell lymphoma and classical
Hodgkin's lymphoma. Initially, the neoplasm had compressed the
jugular and subclavian veins and the pulmonary apex, and may have
caused Bernard Horner Syndrome and SVC syndrome. Since the
treatment for these tumors depends on etiology, in this case a
chemotherapeutic regimen was administered; the volume of the mass
rapidly reduced and the patient's clinical condition improved.
In case 3, the patient presented with mediastinal
syndrome complicated by SVC syndrome. SVC syndrome is considered a
medical emergency. The vena cava is easily compressible, and prompt
and aggressive therapy should be commenced as soon as possible. The
severity of the emergency depends on how fast the obstruction of
the vessels occurs; if the development of the obstruction is slow,
collateral circulation may develop (10).
Malignant etiology is observed in 70–90% of cases of
SVC syndrome, whereas a non-malignant etiology is demonstrated in
10–30% of cases (11). Common
malignancies include bronchogenic cancer, large cell Hodgkin's
lymphomas, thymoma, lung cancer, germ cell tumor and metastatic
tumors, particularly from breast cancer (2,7).
Non-malignant diseases are caused by intravascular devices
(2), goiter, aspergilloma, large
ascending aortic aneurysm, pacemakers or internal defibrillators
(2,7,8).
The clinical presentation of SVC syndrome may be
acute or chronic, depending on the etiology. Clinical symptoms can
be due to passive venous congestion and elevated upper venous
pressure, leading to dyspnea, cough, orthopnea, and edema of upper
extremities and the face (2,12). In addition, muscle weakness caused by
Lambert-Eaton myasthenic syndrome may be present (13).
Regardless of whether a life-threatening condition
is present, such as acute respiratory insufficiency, neurological
dysfunction or acute cardiac insufficiency, treatment of SVC
syndrome should be commenced as soon as possible. However, it is
necessary to identify the type of cancer prior to administering
antineoplastic therapy (10).
Clinicians should evaluate the advantages and disadvantages of
performing a biopsy, due to the high risk of bleeding as a result
of the elevated central venous pressure (10). Mediastinoscopy or thoracotomy may be
considered for diagnosis or de-bulking treatment (10).
Therapeutic management of SVC syndrome caused by
malignant diseases includes the treatment of the cancer and the
relief of symptoms, even if prognosis is poor (10). Initial management includes supportive
measures, such as elevating the head of bed, and the use of
diuretics, oxygen and steroids for the treatment of symptoms.
Treatment depends on the etiology, therefore, radiotherapy and
chemotherapy are used in in tumours that are sensitive to these
treatments (1,2). Cancers sensitive to radiation, such as
lymphomas, should be treated promptly (10). The patient in case 3 developed SVC
syndrome due to lymph nodes metastasis of a gastric cancer. This
was the only patient who was diagnosed with a vena cava syndrome;
however, this co-morbidity may have been undiscovered in cases 2
and 3. In case 3, palliative treatment to alleviate acute
respiratory insufficiency and provide symptom relief was
administered. Radiotherapy and surgery were contraindicated, in
this case, due to very poor clinical conditions, and the patient
succumbed to acute respiratory failure after 4 days.
In conclusion, mediastinal syndrome is a life
threatening condition typically caused by tumors. Notably, in 40%
of cases, mediastinal masses are asymptomatic and are incidentally
discovered by routine chest radiographs (14). To date, improved interpretation of
radiographic signs has ameliorated the detection and localization
of the mediastinal masses, which has increased the treatment
options available. It is crucial that a diagnosis is reached as
soon as possible and that treatment commences quickly in order to
avoid emergency treatment and improve the prognosis. Treatment may
be curative, depending on the etiology and the capacity for rapid
diagnosis. Therefore, clinicians should appreciate the urgency of
the situation.
Glossary
Abbreviations
Abbreviations:
|
ABG
|
arterial blood gas
|
|
CT
|
computed tomography
|
|
Hb
|
hemoglobin
|
|
WBC
|
white blood cell
|
References
|
1
|
Shahrzad M, Le TS, Silva M, Bankier AA and
Eisenberg RL: Anterior mediastinal masses. AJR Am J Roentgenol.
203:W128–W138. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Petersdorf SH and Wood DE:
Lymphoproliferative disorders presenting as mediastinal neoplasms.
Semin Thorac Cardiovasc Surg. 12:290–300. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Collins LG, Haines C, Perkel R and Enck
RE: Lung cancer: diagnosis and management. Am Fam Physician.
75:56–63. 2007.PubMed/NCBI
|
|
4
|
Van Houtte P, De Jager R, Lustman-Maréchal
J and Kenis Y: Prognostic value of the superior vena cava syndrome
as the presenting sign of small cell anaplastic carcinoma of the
lung. Eur J Cancer. 16:1447–1450. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Campo E, Swerdlow SH, Harris NL, Pileri S,
Stein H and Jaffe ES: The 2008 WHO classification of lymphoid
neoplasms and beyond: evolving concepts and practical applications.
Blood. 117:5019–5032. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kishi K, Sonomura T, Mitsuzane K, Nishida
N, Yang RJ, Sato M, Yamada R, Shirai S and Kobayashi H:
Self-expandable metallic stent therapy for superior vena cava
syndrome: Clinical observations. Radiology. 189:531–535. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Andrade MA: A review of 128 cases of
posterior mediastinal goiter. World J Surg. 1:789–797. 1977.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Xu J, Shen B, Li Y and Zhang T: Enormous
goiter in posterior mediastinum: Report of 2 cases and literature
review. J Formos Med Assoc. 108:337–343. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Strollo DC, Rosado-de-Christenson ML and
Jett JR: Primary mediastinal tumors: Part II. Tumors of the middle
and posterior mediastinum. Chest. 112:1344–1357. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Markman M: Diagnosis and management of
superior vena cava syndrome. Cleve Clin J Med. 66:59–61. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Aroor AR, Prakasha SR, Seshadri S, S T and
Raghuraj U: A study of clinical characteristics of mediastinal
mass. J Clin Diagn Res. 8:77–80. 2014.PubMed/NCBI
|
|
12
|
Cheng S: Superior vena cava syndrome: A
contemporary review of a historic disease. Cardiol Rev. 17:16–23.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zhang K, Liu W, Li Y, Zhang K, Gao X and
Wang J: Mediastinal small cell cancer associated with Lambert-Eaton
myasthenic syndrome: A case report. Exp Ther Med. 10:117–120.
2015.PubMed/NCBI
|
|
14
|
Davis RD Jr, Oldham HN Jr and Sabiston DC
Jr: Primary cysts and neoplasms of the mediastinum: Recent changes
in clinical presentation, methods of diagnosis, management, and
results. Ann Thorac Surg. 44:229–237. 1987. View Article : Google Scholar : PubMed/NCBI
|