Introduction
Alien hand syndrome (AHS) is a rare clinical
syndrome; using the Mayo Clinic Medical Records Linkage System,
Graff-Radford et al (1)
identified 150 patients with alien limbs within the Department of
Neurology between January 1, 1996, and July 11, 2011. Numerous
medical and surgical conditions can cause AHS, such as cerebral
infarction, cerebral hemorrhage, corticobasal degeneration,
epilepsia partialis continua, Alzheimer's disease, progressive
supranuclear palsy and Creutzfeldt-Jakob disease (2–9).
However, there are few reports about the pharmacologic or
rehabilitation treatment of AHS. Experience with pharmacologic
treatment of AHS has been limited to platelet aggregation
inhibitors (10,11). In addition, the rehabilitation
treatment of AHS is lacking in the literature (12–14).
Pooyania et al (14)
identified that being educated about the diagnosis of AHS and the
use of compensatory strategies (visualization, distraction of
affected limb and maintaining a slow/steady pace during activities)
decreased the frequency of patient's AHS movements (14).
AHS is a movement disorder characterized by
involuntary and autonomous movements. AHS can be divided into three
variants, including the frontal, callosal and posterior AHS
subtypes (5,15). The callosal subtype is characterized
by intermanual conflict (antagonizing movements of the two hands),
mostly due to the disconnection between the two cerebral
hemispheres (16). The blood supply
to the corpus callosum is ample; thus, infraction in this area is
rare. The present study reports a case of callosal-subtype AHS
presenting following corpus callosum infarction. In addition, the
current case was compared with a collection of 31 previously
reported cases of AHS that were caused by callosal infarction.
Case report
A 56-year-old woman presented at the Yantai
Yuhuangding Hospital (Yantai, China) in November 2011 with
involuntary and autonomous activity of the right hand that
persisted for 1 month, without apparent cause. Intermanual conflict
was the most troubling feature experienced. For instance, the
patient's right hand took off her clothing while she attempted to
dress with the left hand. The patient also reported weak right limb
and dysarthria. She had a history of hypertension, coronary artery
disease and type 2 diabetes mellitus, but no substance abuse
history, including smoking and drinking. No similar disease or
syndrome was reported for any family members. Written informed
consent was obtained from the patient.
Physical examination failed to revealed anepia,
anarthria, autotopagnosia or apraxia. No signs of meningeal
irritation were observed. In addition, an ophthalmic examination
failed to reveal any abnormalities, whereas a slightly superficial
right nasolabial fold was detected. Muscle tension was normal, with
level-5 muscle force in the right upper extremity and level-4 in
the right lower extremity (17).
Sensory, finger-to-nose and left heel-knee-shin tests were normal.
However, the heel-knee-shin test on the right side was
unsuccessful. Deep tendon reflex was normal, with no pathological
signs. The mini-mental state examination (MMSE) score was 30
(18).
Doppler color imaging demonstrated atherosclerotic
plaques in bilateral carotid arteries and increased resistance in
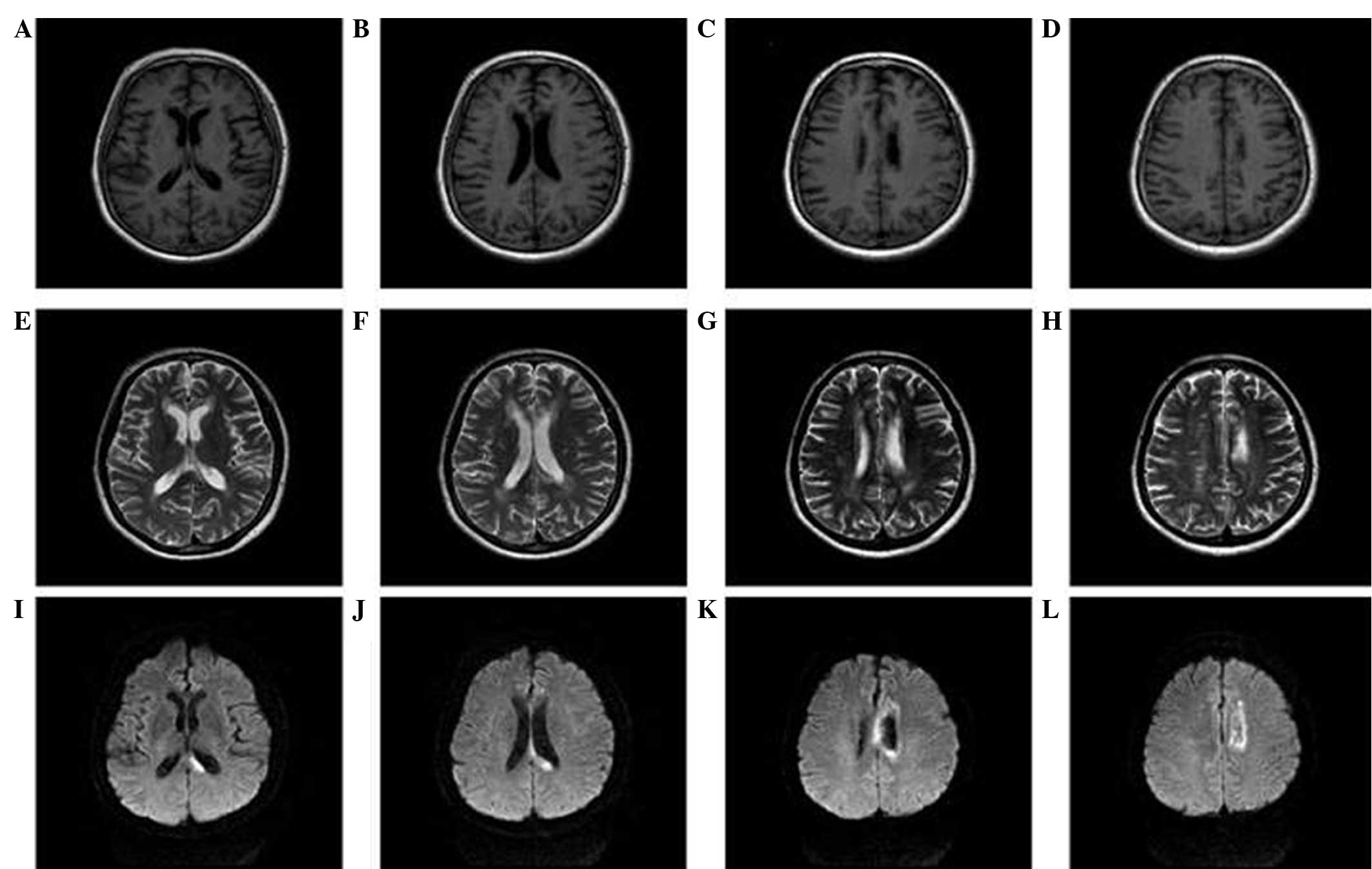
bilateral vertebral arteries. Cranial magnetic resonance imaging
(MRI) displayed long T1 and T2 signals, as well as high signals on
diffusion weighted imaging (DWI), in the body and splenium of the
left corpus callosum (Fig. 1). Brain
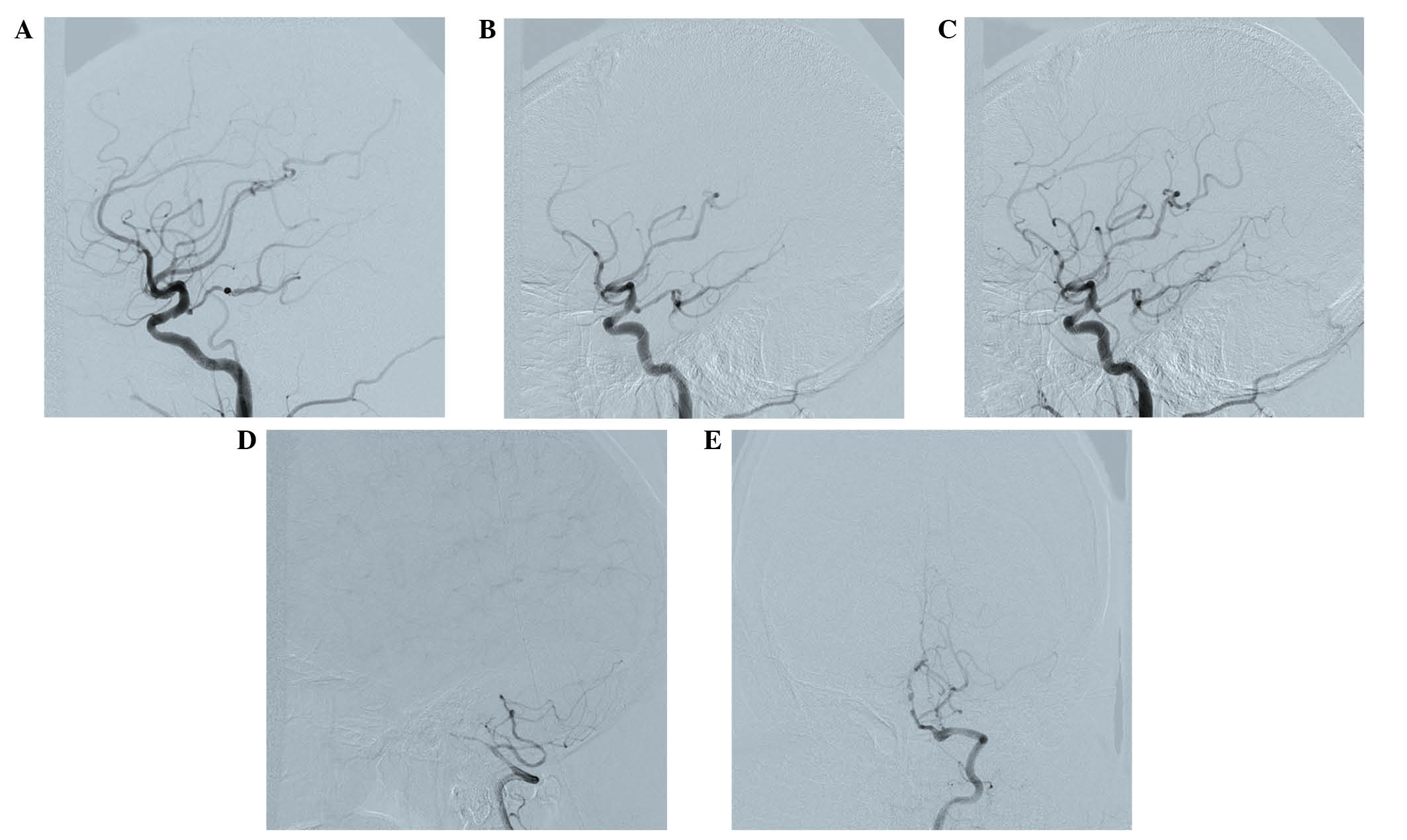
magnetic resonance angiography (MRA) 3 days following admission
revealed extensive atherosclerosis and intermittent visualization
of the basilar artery (Fig. 2A).
Cerebral digital subtraction angiography (DSA) of the right or left
internal carotid artery showed the opening of the corresponding
posterior communicating artery. Furthermore, bilateral posterior
cerebral arteries and basilar artery apex were visualized. The left
anterior cerebral artery and left pericallosal arteries appeared
faint. The right vertebral artery was narrow, and the distal
segment of the intracranial branch was occluded. In addition, the
intracranial branch of the left vertebral artery and basilar artery
was significantly narrowed (Fig. 3).
A diagnosis of callosal AHS was established based on the
aforementioned observations. The characteristic features of
callosal AHS reported in the present patient included involuntary
autonomous movement, and intermanual conflict. Infarction of the
corpus callosum was clearly demonstrated in MRI scans, while MRA
and DSA revealed multiple lesions in the feeding arteries.
The patient was treated with aspirin enteric coated
tablets (100 mg, qd; Bayer AG, Leverkusen, Germany) atorvastatin
calcium (20 mg, qn; Pfizer), amlodipine besylate tablets (5 mg, qd;
Pfizer, Inc., New York, NY, USA) and metformi (500 mg, bid;
Bristol-Myers Squibb, New York, NY, USA) during the 2-week hospital
stay, and continued to receive the same treatment until the last
visit in March 2015. No stroke recurrence was observed.
Discussion
Frontal AHS is characterized by forced grasping of
objects and impulsive reaching and groping movements toward nearby
objects within the visual field. This type of AHS is typically
caused by lesions located in the anterior corpus callosum, the
supplementary motor area, the anterior cingulate gyrus and the
medial prefrontal cortex of the dominant hemisphere. By contrast,
callosal AHS typically results from a callosal lesion and is
characterized primarily by intermanual conflict and apraxia of the
non-dominant limb (5). Posterior AHS
is characterized by the feeling of an alien hand and left
hemianesthesia, which lesions primarily in the cortex or
subcortical structures, such as the thalamus, parietal lobe and
medial temporal lobe that are supplied by the posterior cerebral
artery (10,12,13,15). The
current study reported a case with characteristic features of
callosal AHS, including involuntary autonomous movement, as well as
intermanual conflict. Infarction of the corpus callosum was clearly
demonstrated according to the imaging results.
In the present study, a search of the PubMed
database (www.ncbi.nlm.nih.gov/pubmed) was performed (keyword,
alien hand syndrome) in order to identify previous AHS cases
presenting after callosal infraction. The search yielded 23 studies
reporting 31 cases of AHS following callosal infarction between
1990 and 2014 (5,19–40).
These callosal infarction cases were divided into simple corpus
callosum infarction and complex corpus callosum infarction. Simple
corpus callosum infarction was defined as infarction occurring in
the corpus callosum alone; complex corpus callosum infarction was
defined as corpus callosum with involvement of other brain
sites.
The search yielded a total of 31 previous AHS cases,
with 7 cases of simple corpus callosum infarction (22.6%) and 24
cases of complex corpus callosum infarction (77.4%). As shown in
Table I, the corpus callosum was
affected on the left side in 10 out of the 31 cases (5,19,25–30)
and on the right side in 17 cases (20,21,25–27,31–40).
Both sides of the corpus callosum were affected in 4 cases
(20,22–24), all
of which presented simple corpus callosum infarction (Table I). In complex corpus callosum
infarction cases, the majority of lesion sites included the medial
frontal cortex (16/24; 66.7%), the anterior cingulate gyrus (7/24;
29.2%) and the supplementary motor cortex (3/24; 12.5%).
 | Table I.Summary of reported cases of alien
hand syndrome presenting following simple and complex callosal
infarction. |
Table I.
Summary of reported cases of alien
hand syndrome presenting following simple and complex callosal
infarction.
| A, Simple callosal
infarction (n=7)a |
|---|
|
|---|
| Studies |
| Nc | Symptoms | Ref. |
|---|
| Unilateral
(left) |
|
|
|
|
|
Verleger et al |
|
| IC | (19) |
| Unilateral
(right) |
|
|
|
|
|
Suwanwela and
Leelacheavasit |
| 2 | IC, PC | (20) |
|
Nicholas et al |
|
| GR, SR | (21) |
| Bilateral |
|
|
|
|
|
Muangpaisan et al |
|
| IC, agonistic
dyspraxia, mirror movement | (22) |
| Lin
et al |
|
| IC of left hand, GR
of right hand | (23) |
| Yuan
et al |
|
| IC, AH sign | (24) |
|
Suwanwela and
Leelacheavasit |
| 1 | IC, PC, mirror
movement | (20) |
|
| B, Complex callosal
infarction (n=24)b |
|
| Studies | Nc | Concurrent
infarction | Symptoms | Ref. |
|
| Unilateral
(left) |
|
|
|
|
|
Feinberg et al |
| Medial frontal
lobe | IC, GR | (5) |
|
Goldberg and Bloom | 2, 4 | Medial surface of
frontal lobe | IC and GR, or GR
only | (25) |
| Giroud
and Dumas | 7 | Centrum ovale | GR | (26) |
| Chan
and Ross | 1 | Mesiofrontal
cortex | IC | (27) |
| Biran
et al |
| Mesial frontal
cortex | IC, GR, PC | (28) |
| Jang
et al |
| Anterior portion of
left cingulate gyrus | GR, compulsive
manipulation | (29) |
| Nowak
et al | 1 | Paramedian
periventricular white matter and paramedian cortex | IC, GR | (30) |
| Nowak
et al (30) | 2 | Anterior of corpus
callosum and overlying white matter | GR | (30) |
| Unilateral
(right) |
| Tanaka
et al |
| Anterior third
cingulate gyrus, lower or medial superior frontal gyrus | IC | (31) |
|
Goldberg and Bloom | 1 | Medial frontal
gyrus | IC, GR, SR | (25) |
|
Goldberg and Bloom | 3 | Medial frontal
lobe | GR | (25) |
|
Gottlieb et al | 2 | Multiple lacunae
(both cerebral hemispheres) | IC | (32) |
| Doody
and Jankovic | 6 | Internal capsule
lacuna | LE, PE | (33) |
| Trojano
et al | 1 | Frontomesial region
extending to anterior cingulate gyrus | IC, GR, SR, AH
sign | (34) |
| Giroud
and Dumas | 8 | Internal frontal
area | GR | (26) |
| Chan
et al |
| Right anterior
cingulate gyrus, supplementary motor area, medial prefrontal
cortex | IC, GR, SR, leg
symptoms | (35) |
| Chan
and Ross | 2 | Mesial prefrontal
cortex, anterior cingulate gyrus, supplementary motor cortex | IC, GR | (27) |
| Chan
and Ross | 3 | Anterior cingulate
gyrus, prefrontal cortex, partial supplementary motor cortex | GR | (27) |
| Ay
et al |
| Thalamus,
hippocampus, inferior temporal lobe, occipital lobe | AH sign, PE | (36) |
| Ong Hai
and Odderson |
| Mesial frontal
cortex, right anterior cingulate gyrus | IC, GR, PC,
involuntary masturbation | (37) |
| Bejot
et al |
| Bilateral medial
frontal lobes | GR, involuntary
masturbation | (38) |
|
Espinosa et al |
| Parietal area | Mirror
movement | (39) |
| Park
et al | 2 | Frontal lobe | IC | (40) |
Major AHS symptoms included intermanual conflict
(19/31; 61.3%), grasp reflect (19/31; 61.3%) and alien hand signs
(3/24; 12.5%). Among the 7 patients with simple corpus callosum
infarction, intermanual conflict occurred in 6 cases (85.7%), while
grasp reflex was seen in 2 cases (28.5%). Among the 24 patients
with complex corpus callosum infarction, intermanual conflict was
reported in 13/24 (54.2%) patients, while grasp reflex was observed
in 17 cases (70.8%). Within the 17 grasp reflex patients, 14
(82.3%) had infarction at the medial frontal cortex, cingulate
gyrus or supplementary motor cortex. In addition, 2/24 (8.3%)
complex corpus callosum infarction cases were reported to
experience involuntary masturbation.
As shown in Table
II, 16 (51.6%) (19,24,25,27,30–33,
35–38) out of the 31 included cases presented
disappearance or significant alleviation of AHS symptoms during the
follow-up (between several days and 15 months), while no
improvement was observed in 4 cases (5,21,27,34)
for at least 6 months. In the remaining 11 cases (20,22,23,25,26,28,29,39,40), the
outcome was unknown.
 | Table II.Outcomes of reported cases of AHS
presenting following simple and complex callosal infarction
(n=31). |
Table II.
Outcomes of reported cases of AHS
presenting following simple and complex callosal infarction
(n=31).
| Authors | Na | Duration | AHS symptoms | Ref. |
|---|
| Feinberg et
al | 1 | 1 year | Absence | (5) |
| Verleger et
al | 1 | 15 months | Decrease | (19) |
| Suwanwela and
Leelacheavasit | 2 | N/A | N/A | (20) |
| Nicholas et
al | 1 | 8 months | Absence | (21) |
| Muangpaisan et
al | 1 | N/A | N/A | (22) |
| Lin et
al | 1 | N/A | N/A | (23) |
| Yuan et
al | 1 | 2 weeks | Decrease | (24) |
| Goldberg and
Bloom | 4 | 1 year, 7 months,
N/A | Decrease | (25) |
|
|
| N/A | N/A |
|
| Giroud and
Dumas | 2 | N/A | N/A | (26) |
| Chan and Ross | 3 | 6 and 3 months | Decrease | (27) |
|
|
| 6 months | Absence |
|
| Biran et
al | 1 | N/A | N/A | (28) |
| Jang et
al | 1 | N/A | N/A | (29) |
| Nowak et
al | 2 | 28 and 37
weeks | Decrease | (30) |
| Tanaka et
al | 1 | 7 months | Decrease | (31) |
| Gottlieb et
al | 1 | Next few
months | Decrease | (32) |
| Doody and
Jankovic | 1 | Within days | Decrease | (33) |
| Trojano et
al | 1 | 11 months | Absence | (34) |
| Chan et
al | 1 | 6 months | Decrease | (35) |
| Ay et
al | 1 | 2 weeks | Decrease | (36) |
| Ong Hai and
Odderson | 1 | 7 weeks | Decrease | (37) |
| Bejot et
al | 1 | 2 weeks | Decrease | (38) |
| Espinosa et
al | 1 | N/A | N/A | (39) |
| Park et
al | 1 | N/A | N/A | (40) |
In general, the literature search revealed that the
lesion was complex in the majority (77.4%) of cases. Intermanual
conflict was more common in simple corpus callosum infarction
patients (85.7%), and grasp reflex was more frequently reported in
complex corpus callosum infarction patients (70.8%). Involuntary
masturbation seems to be unique to infarction of the right anterior
corpus callosum (37,38). Table I
also suggests that the right hemisphere is more frequently
involved, since the right and left sides of the corpus callosum
were affected in 17 and 10 patients, respectively.
The corpus callosum is a fiber plate that conveys
information between the two cerebral hemispheres (41). Callosal AHS putatively arises from
failure in connection between the motor area and the supplementary
motor area in the two cerebral hemispheres (16,23).
Damage to the corpus callosum may manifest as frontal or callosal
AHS. Mixed AHS has been also reported following corpus callosum
infarction (24), in which the
symptoms include intermanual conflict (as in callosal AHS), feeling
of an alien hand and hemianesthesia (as in posterior AHS that
involves the thalamus, parietal lobe or medial temporal lobe)
(10,12,13,15).
Table I indicates
that infarction of the corpus callosum typically occurs with
lesions to other sites, including the medial frontal cortex,
anterior cingulate gyrus and supplementary motor cortex. Similar to
the genu and body of the corpus callosum, these regions all receive
blood supply from the anterior cerebral artery. By contrast, the
splenium of the corpus callosum receives blood from the posterior
cerebral artery (42). Infarction at
the splenium of the corpus callosum is reportedly caused by
embolism, whereas atherosclerotic cerebral infarction is the more
common form of infarction in the genu and body of the corpus
callosum (43). The corpus callosum
receives blood supply from the anterior and the posterior cerebral
arteries with extensive anastomosis, and thus is rarely affected by
infarction (42). In the present
case, MRA and cerebral angiography revealed extensive
atherosclerosis throughout the intracranial vasculature, notably in
the left anterior cerebral and the vertebral basilar arteries.
These imaging findings suggested the presence of atherosclerotic
lesions in the anterior and posterior circulation.
AHS tends to be transient in patients with partial
loss of the corpus callosum genu and splenium; in addition,
patients with unilateral callosal lesions may regain connectivity
between the two hemispheres if the remaining corpus callosum is
functional (44). Permanent AHS may
develop when the infarction involves two thirds of the anterior
corpus callosum (45). Quick
recovery was noticed following antiplatelet therapy in the present
case, suggesting that the remaining corpus callosum may have
compensated for the lesioned site, and that connectivity between
the bilateral cerebral hemispheres was re-established.
In conclusion, the present study reported a
prototypic case of callosal AHS, which was apparently caused by
compromised anterior and posterior circulation. A notable issue in
this case is insufficient blood supply of the vertebra-basilar
arteries and the left anterior cerebral artery. This finding
highlights the need for comprehensive investigation of the cerebral
vasculature in patients with AHS caused by infarction of the corpus
callosum.
Acknowledgements
The authors would like to thank the patient for her
participation in the present study. The present study was funded by
the Yantai Science and Technology Development Plan (grant no.
2013ws220).
Glossary
Abbreviations
Abbreviations:
|
AHS
|
alien hand syndrome
|
|
MRA
|
magnetic resonance angiography
|
|
MRI
|
magnetic resonance imaging
|
|
MMSE
|
mini-mental state examination
|
References
|
1
|
Graff-Radford J, Rubin MN, Jones DT,
Aksamit AJ, Ahlskog JE, Knopman DS, Petersen RC, Boeve BF and
Josephs KA: The alien limb phenomenon. J Neurol. 260:1880–1888.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Jeeves MA, Simpson DA and Geffen G:
Functional consequences of the transcallosal removal of
intraventricular tumors. J Neurol Neurosurg Pshychiatry.
42:134–142. 1979. View Article : Google Scholar
|
|
3
|
Huang Y and Jia JP: Corpus callosum
hematoma secondary to cerebral venous malformation presenting as
alien hand syndrome. Neurocase. 19:377–381. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Gibb WRG, Luther PJ and Marsden CD:
Corticobasal degeneration. Brain. 112:1171–1192. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Feinberg TE, Schindler RJ, Flanagan NG and
Haber LD: Two alien hand syndromes. Neurology. 42:19–24. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kim HY, Kim JY, Kim GU, Han HJ and Shin
DI: Alien hand syndrome after epilepsia partialis continua: FDG PET
and MRI studies. Epilepsy Behav. 23:71–73. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ball JA, Lantos PL, Jackson M, Marsden CD,
Scadding JW and Rossor MN: Alien hand sign in association with
Alzheimer's histopathology. J Neurol Neurosurg Psychiatry.
56:1020–1023. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Barclay CL, Bergeron C and Lang AE: Arm
levitation in progressive supranuclear palsy. Neurology.
52:879–882. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Rubin M, Graff-Radford J, Boeve B, Josephs
KA and Aksamit AJ: The alien limb phenomenon and Creutzfeldt-Jakob
disease. Parkinsonism Relat Disord. 18:842–846. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Marey-Lopez J, Rubio-Nazabal E,
Alonso-Magdalena L and Lopez-Facal S: Posterior alien hand syndrome
after a right thalamic infarct. J Neurol Neurosurg Psychiatry.
73:447–449. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Dolado AM, Castrillo C, Urra DG and de
Seijas E Varela: Alien hand sign or alien hand syndrome? J Neurol
Neurosurg Psychiatry. 59:100–101. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Pack BC, Stewart KJ, Diamond PT and Gale
SD: Posterior-variant alien hand syndrome: Clinical features and
response to rehabilitation. Disabil Rehabil. 24:817–818. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Pappalardo A, Ciancio MR, Reggio E and
Patti F: Posterior alien hand syndrome: Case report and
rehabilitative treatment. Neurorehabil Neural Repair. 18:176–181.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Pooyania S, Mohr S and Gray S: Alien hand
syndrome: A case report and description to rehabilitation. Disabil
Rehabil. 33:1715–1718. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kato H, Iijima M, Hiroi A, Kubo M and
Uchigata M: A case of alien hand syndrome after right posterior
cerebral artery territory infarction. Rinsho Shinkeigaku.
43:487–490. 2003.PubMed/NCBI
|
|
16
|
Geschwind DH, Iacoboni M, Mega MS, Zaidel
DW, Cloughesy T and Zaidel E: Alien hand syndrome: Interhemispheric
motor disconnection due to a lesion in the midbody of the corpus
callosum. Neurology. 45:802–808. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Shi YQ and Zhou XD: Pratical Neurology.
3rd. Shanghai Scientific and Technical Publishers; Shanghai: pp.
492004
|
|
18
|
Folstein MF, Folstein SE and McHugh PR:
Mini mental state. A practical method for grading the cognitive
state of patients for clinicians. J Psychiatr Res. 12:189–198.
1975. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Verleger R, Binkofski F, Friedrich M,
Sedlmeier P and Kömpf D: Anarchic-hand syndrome: ERP reflections of
lost control over the right hemisphere. Brain Cogn. 77:138–150.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Suwanwela NC and Leelacheavasit N:
Isolated corpus callosal infarction secondary to pericallosal
artery disease presenting as alien hand syndrome. J Neurol
Neurosurg Psychiatry. 72:533–536. 2002.PubMed/NCBI
|
|
21
|
Nicholas JJ, Wichner MH, Gorelick PB and
Ramsey MM: Naturalization of the alien hand: Case report. Arch Phys
Med Rehabil. 79:113–114. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Muangpaisan W, Srisajjakul S and Chiewvit
P: The alien hand syndrome: Report of a case and review of the
literature. J Med Assoc Thai. 88:1447–1452. 2005.PubMed/NCBI
|
|
23
|
Lin JH, Kwan SY and Wu D: Mixed alien hand
syndrome coexisting with left-sided extinction secondary to a left
corpus callosal lesion: A case report. Mov Disord. 22:248–251.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Yuan JL, Wang SK, Guo XJ and Hu WL: Acute
infarct of the corpus callosum presenting as alien hand syndrome:
Evidence of diffusion weighted imaging and magnetic resonance
angiography. BMC Neurol. 11:1422011. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Goldberg G and Bloom KK: The alien hand
sign. Localization, lateralization and recovery. Am J Phys Med
Rehabil. 69:228–238. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Giroud M and Dumas R: Clinical and
topographical range of callosal infarction: A clinical and
radiological correlation study. J Neurol Neurosurg Psychiatry.
59:238–242. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Chan JL and Ross ED: Alien hand syndrome:
Influence of neglect on the clinical presentation of frontal and
callosal variants. Cortex. 33:287–299. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Biran I, Giovannetti T, Buxbaum L and
Chatterjee A: The alien hand syndrome: What makes the alien hand
alien? Cogn Neuropsychol. 23:563–582. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Jang SH, Lee J, Yeo SS and Chang MC:
Callosal disconnection syndrome after corpus callosum infarct: A
diffusion tensor tractography study. J Stroke Cerebrovasc Dis.
22:e240–e244. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Nowak DA, Bösl K, Lüdemann-Podubecka J,
Gdynia HJ and Ponfick M: Recovery and outcome of frontal alien hand
syndrome after anterior cerebral artery stroke. J Neurol Sci.
338:203–206. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Tanaka Y, Iwasa H and Yoshida M:
Diagonistic dyspraxia: Case report and movement-related potentials.
Neurology. 40:657–661. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Gottlieb D, Robb K and Day B: Mirror
movements in the alien hand syndrome. Case report. Am J Phys Med
Rehabil. 71:297–300. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Doody RS and Jankovic J: The alien hand
and related signs. J Neurol Neurosurg Psychiatry. 55:806–810. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Trojano L, Crisci C, Lanzillo B, Elefante
R and Caruso G: How many alien hand syndromes? Follow-up of a case.
Neurology. 43:2710–2712. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Chan JL, Chen RS and Ng KK: Leg
manifestation in alien hand syndrome. J Formos Med Assoc.
95:342–346. 1996.PubMed/NCBI
|
|
36
|
Ay H, Buonanno FS, Price BH, Le DA and
Koroshetz WJ: Sensory alien hand syndrome: Case report and review
of the literature. J Neurol Neurosurg Psychiatry. 65:366–369. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Ong Hai BG and Odderson IR: Involuntary
masturbation as a manifestation of stroke-related alien hand
syndrome. Am J Phys Med Rehabil. 79:395–398. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Bejot Y, Caillier M, Osseby GV, Didi R,
Ben Salem D, Moreau T and Giroud M: Involuntary masturbation and
hemiballismus after bilateral anterior cerebral artery infarction.
Clin Neurol Neurosurg. 110:190–193. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Espinosa PS, Smith CD and Berger JR: Alien
hand syndrome. Neurology. 67:e212006. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Park YW, Kim CH, Kim MO, Jeong HJ and Jung
HY: Alien hand syndrome in stroke - case report &
neurophysiologic study. Ann Rehabil Med. 36:556–560. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Gazzaniga MS: Cerebral specialization and
interhemispheric communication: Does the corpus callosum enable the
human condition? Brain. 123:1293–1326. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Kahilogullari G, Comert A, Arslan M, Esmer
AF, Tuccar E, Elhan A, Tubbs RS and Ugur HC: Callosal branches of
the anterior cerebral artery: An anatomical report. Clin Anat.
21:383–388. 2008. View
Article : Google Scholar : PubMed/NCBI
|
|
43
|
Kasow DL, Destian S, Braun C, Quintas JC,
Kagtsu NJ and Johnson CE: Corpus callosum infarcts with atypical
clinical and radiologic presentations. AJNR Am J Neuroradiol.
21:1876–1880. 2000.PubMed/NCBI
|
|
44
|
Barbeau E, Joubert S and Poncet M: A
single case-study of diagonistic dyspraxia. Brain Cogn. 54:215–217.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Papagno C and Marsile C: Transient
left-sided alien hand with callosal and unilateral fronto-mesial
damage: A case study. Neuropsychologia. 33:1703–1709. 1995.
View Article : Google Scholar : PubMed/NCBI
|