At present the incidence of contrast-induced
nephropathy (CIN) has been increasing in patients undergoing
coronary angioplasty, due to the increasing use of contrast media
(1). CIN is usually described as an
increase in serum creatinine of 0.5 mg/dl or a 25% increase from
the baseline value 48 h following the imaging procedure (2). CIN has been reported to occur in ≥14.5%
of unselected patients undergoing coronary angioplasty, and is
considered to be the third leading cause of hospital-acquired acute
renal failure (3). It is more
commonly associated with adverse clinical outcomes, increased
medical care costs, prolonged hospitalization, and increased
in-hospitality morbidity and mortality (4). The major risk factors of CIN are
reduced circulation volume, the type and volume of contrast agent,
simultaneous administration of nephrotoxic agents and pre-existing
renal dysfunction, particularly that due to diabetic nephropathy
(5–8). Since the poor prognosis of patients
with diabetic nephropathy could largely attribute to CIN, these
patients may benefit greatly from preventive interventions. The
precise mechanisms underlying the pathogenesis of CIN have not been
well established. However, it is widely speculated that the
underlying mechanism of CIN may involve an injury to the renal
medulla caused by a combination of reduced blood flow, direct
tubular toxicity and an osmotic effect (9). The direct tubular toxicity may be
associated with reactive oxygen species (ROS), which are generated
following the administration of contrast agent (10). Currently, the preventive treatments
for CIN involve reducing contrast exposure, intravenous volume
expansion with a saline hydration, and usage of low or
iso-osmolarity contrast agent; however, these may provide
incomplete prevention of CIN and thus, adjunctive pharmacotherapies
in clinical practice have emerged (11). Among these, N-acetylcysteine (NAC)
has been of interest since it was initially reported by Tepel et
al (12). NAC as a direct
scavenger of free radicals may improve blood flow via nitric
oxide-mediated pathways, and it is a precursor of glutathione
synthesis, providing vasodilation and antioxidant activity against
CIN (13). Therefore, oral NAC
therapy may be an alternative method for CIN prevention, providing
safety, low cost and few side effects (14).
It has been reported that oral NAC may more
effectively provide protection against CIN compared with
intravenous hydration alone (15).
Results of the initial study (12)
of oral NAC for the prevention of CIN were encouraging, while the
bioavailability of oral NAC may be low and exhibited mixed results;
a few trials demonstrated the reduction of CIN incidence by oral
NAC therapy (16–21), and most trials revealed no
significant CIN prevention (22–34). The
aim of the present study was to determine whether oral NAC therapy
is beneficial for CIN prevention in clinical practice, using a
meta-analysis.
A comprehensive study was performed to search all
published randomized controlled trials (RCT) until January 1, 2015
which concerned oral NAC treatment to prevent CIN in patients
undergoing coronary angioplasty, using searching engines such as
Medline (https://www.nlm.nih.gov/bsd/pmresources.html), Embase
(https://www.elsevier.com/solutions/embase-biomedical-research)
and Cochrane (http://uk.cochrane.org/). The search
terms were as follows: N-acetylcysteine, acetylcysteine, NAC,
cardiac catheterization, coronary angioplasty, coronary angiogram,
percutaneous coronary intervention, contrast-induced nephropathy,
contrast-induced nephrotoxicity, contrast-medium nephrotoxicity,
contrast medium-induced nephropathy and contrast-induced acute
kidney injury. RCTs were limited to those with human subjects. A
manual search of the results was then performed for the qualifying
trials. Abstracts alone or meeting proceedings were excluded. This
search strategy was performed comprehensively until no new
potential citations were found on review of the reference list of
retrieved papers. All of the studies published in English which met
the following inclusion criteria were included: Subjects underwent
coronary angioplasty, randomization of oral NAC and placebo, and
data regarding CIN incidence. Exclusion criteria were as follows:
<18 years of age, known allergy or hypersensitivity to NAC,
dialysis patients and those with ST-segment elevation myocardial
infarction undergoing primary angioplasty.
Two investigators (Dr Jing-Xiu Li and Dr Nan-Nan
Liu) were assigned independently to assemble the information of
each study as follows: First author name, surgery type (coronary
angiography or percutaneous coronary intervention), study design
(RCT, prospective or not), control types (placebo or not), blinding
types (double-blinding or not), NAC regimen, sample size, mean age,
percentage of males, the incidence of CIN and length of
hospitalization in each group. Disagreements were settled through
discussion and consensus.
The majority of selected trials were conducted in
randomized sequence generation and allocation concealment, and the
participants were divided randomly. All of them were considered to
be of low bias risk.
The relative risk (RR) was estimated with 95%
confidence interval (CI) for dichotomous outcomes. Heterogeneity
was reported with the I2 statistic, using a
fixed-effects model, and >50% of I2 was considered to
be statistically significant. Begg and Egger tests were performed
for presenting the publication bias, and the potential bias was
analyzed with visual inspection of the Begg funnel plots in which
the log RRS plotted against their standard errors. P<0.05 was
considered to indicate a statistically significant difference. All
statistical analyses were performed using STATA software, version
12.0 (StataCorp LP, College Station, TX, USA) and RevMan 5.2 (The
Nordic Cochrane Centre, Copenhagen, Denmark).
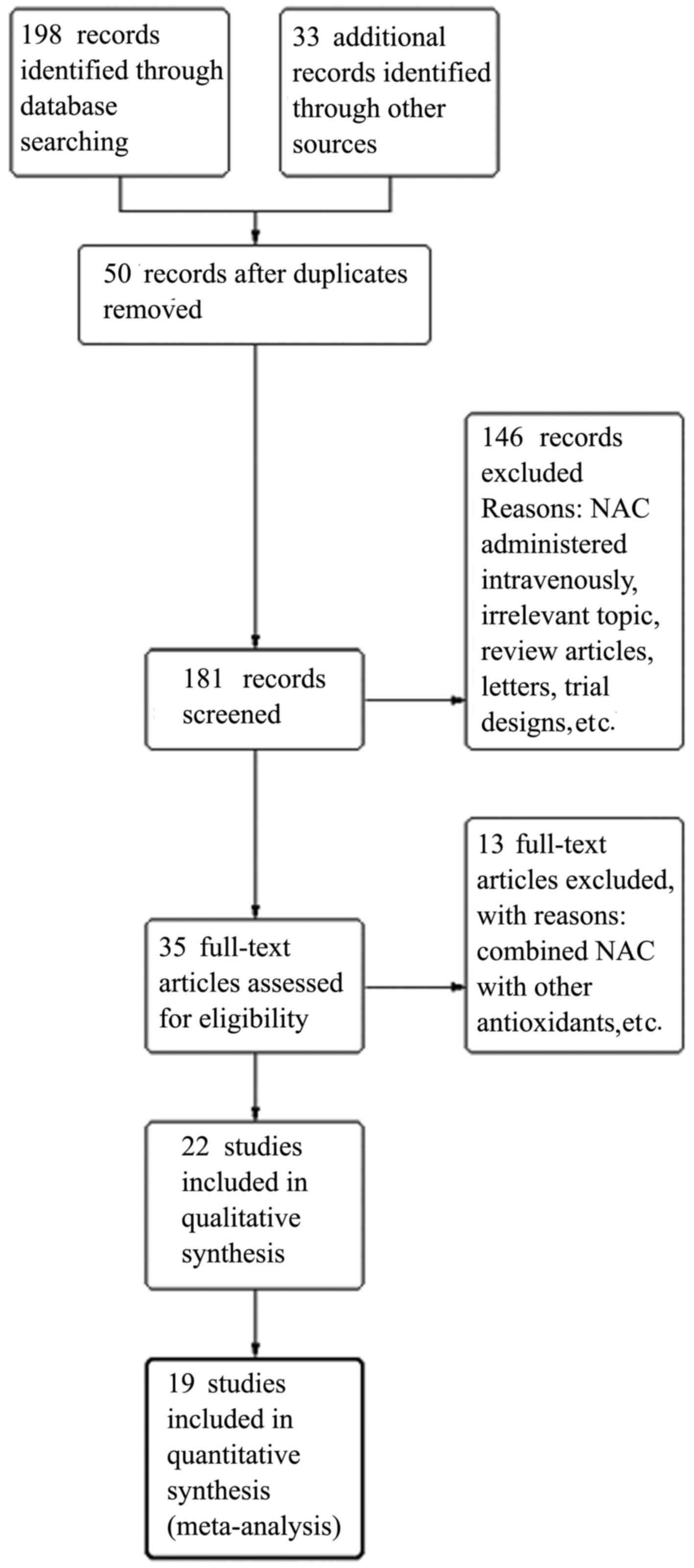
A total of 19 placebo-control RCTs were included in
this study, consisting of 4,514 patients. The flow of identified
studies through the selection process is shown in Fig. 1. The characteristics at baseline and
design of the selected studies are shown in Tables I and II. The range of participant number was
36–2,308, including men and women. The range of total NAC dosage
was 1,200–12,000 mg. The effects of oral NAC on CIN prevention were
also compared.
The selected trials in the meta-analysis were
well-designed and reasonably conducted, adequately implementing
randomized sequence generation and allocation concealment. The
participants among them were blinded. All of the selected studies
had a low risk of bias, and the details are shown in Fig. 2. Publication bias assessed by Egger's
test is shown in Fig. 3.
The baseline characteristics revealed no significant
difference between history of coexistent disease and routine
prophylactic therapies. The CIN incidence was 247 patients in the
oral NAC group (n=2,269) and 278 patients in the control group
(n=2,245), pooling all of the 19 trials. There was no statistical
significance (RR, 0.84; 95% CI, 0.65–1.10; P=0.20, Fig. 4), with no heterogeneity between
trials (I2=29%, P=0.12).
In this meta-analysis, 19 RCTs were combined in
order to evaluate the effects of oral NAC on CIN prevention in
patients undergoing coronary angioplasty. The results showed that
oral NAC treatment was not associated with a reduction of CIN
incidence, and there was no significant heterogeneity between
trials. In addition, it was found that the combined treatments of
oral NAC and sodium chloride did not provide additional benefits;
therefore, the role of oral NAC therapy is yet to be defined in CIN
prevention (11,35,36).
It has been reported that contrast-induced
nephropathy occurred in ~14.5% of unselected patients following
coronary angioplasty. CIN has been considered as the third common
cause of in-hospital acute renal failure after coronary
angiography/intervention (37). In
present studies, the commonly accepted standard for CIN is
according to the absolute or relative change in plasma creatinine
concentration (38). In the majority
of cases, CIN is defined as an increase in baseline serum
creatinine (SCr) concentration of 25% or an absolute increase of at
least 44 mmol/l within 48 h (39).
It is universally acknowledged that absolute increase in SCr is
superior threshold than a relative increase in SCr (40–43).
However, it has been shown that SCr may not be an optimal
substitute marker for glomerular filtration rate (GFR), as the
alteration in renal handling, filtration, secretion and resorption
may exert an influence on SCr levels (44). As has been noted previously (45), tubular creatinine secretion may be
decreased by contrast media itself. Thus, it may cause a transient
increase in SCr concentration, independent of the reduction in GFR.
Serum cystatin C has been proposed as a sensitive biomarker for the
diagnosis of CIN, as cystatin C has been confirmed to reflect
contrast medium-induced deterioration in kidney function in a
superior manner to serum creatinine (46). A previous study showed that oral NAC
did not significantly reduce the incidence of CIN on the basis of
the standard disease definition; however, by the cystatin C level
disease criteria it may be considered to be efficacious (47). However, at present SCr remains the
cheapest and most widely accepted standard of renal function
(48). Therefore, the change of
absolute or relative SCr concentration remains a key parameter in
the diagnosis of CIN. Intravenous saline hydration and the use of
low-osmolality contrast medium has been accepted as preventive
strategies for CIN (49–51).
In the present meta-analysis, 19 placebo-control
RCTs were included, consisting of 4,514 patients. The baseline
characteristic revealed no significant difference between history
of coexistent disease and routine prophylactic therapies. Each
randomize controlled trial utilized intravenous saline hydration.
The CIN incidence was 247 patients in the oral NAC group (n=2,269)
and 278 patients in the control group (n=2,245), pooling all of the
19 trials. There was no statistically significant difference
between the oral NAC group and the control group (RR, 0.84; 95% CI,
0.65–1.10; P=0.20), with no heterogeneity between trials
(I2=29%, P=0.12). The results showed that the oral NAC
treatment was not associated with a reduction in CIN incidence. A
previous study (52) found that
intravenous saline hydration with 0.45% saline prior to and
following coronary angiography and the proper use of nonionic low
osmolar iodine may be renoprotective. Previously, it has been
confirmed (51) that normal saline
hydration (0.9%) may be more efficacious compared with half-normal
saline (0.45%). It is generally accepted that the optimal volume of
normal saline hydration may be determined based on body weight, and
1.0–1.5 ml/kg/h is considered to be the normal range (39). In the present meta-analysis, it was
found that the combined treatments of oral NAC and sodium chloride
did not provide additional benefits, and thus the role of oral NAC
therapy not yet to be defined in CIN prevention.
The precise mechanism underlying the pathogenesis of
CIN remains unclear. It is widely considered (53–55) that
the pathogenesis of CIN may involve injury to the renal medulla
caused by reduced renal blood flow and tubular toxicity through
ROS, which occurs following the administration of contrast media
(1,56). NAC, a thiol-containing antioxidant,
has been approved for an increase in the level of plasma
glutathione, which is an oxygen-free radical scavenger (13). It has been affirmed (57) that NAC is able to prevent oxidative
stress at the location of renal post-ischemia. NAC has received
considerable attention in recent years following research by Tepel
et al (12). In the opinion
of Tepel et al, the utilization of NAC in conjunction with a
fixed volume (75 ml) of low-osmolar contrast medium in patients
undergoing computed tomography (CT), may significantly reduce
incidence of CIN. It has become increasing recognized that NAC may
result in increased nitric oxide production and intensification of
nitric oxide binding (58). It has
been demonstrated in human testing (59) that NAC treatment may significantly
improve endothelium-dependent vasodilation. In a previous study, it
was found that pretreatment of vascular smooth muscle cells with
NAC clearly reduced ROS formation and prevented the reduction of
cell viability (60). In the present
meta-analysis, the majority of the selected trials utilized a low
dose of NAC (600 mg) twice daily for 48 h in conjunction with
intravenous saline hydration. It is known the oral NAC may be
absorbed quickly, reaching the peak plasma concentration in 45 min,
and having a half-life of 2 h. Thus, pretreatment with NAC more
than a few hours prior to contrast exposure or for a prolonged
period afterward may not be essential to provide beneficial
effects.
There were a number of limitations inherent to this
study. First, the asymmetrical appearance of the funnel plot
suggests that publication bias was present. Despite the broad
searching databases and manually searching the conference
proceedings and reference lists from the identified trials, we
could not eliminate that publication bias caused overestimation of
the results from the true treatment. Second, all included studies
used the endpoint of CIN as the primary outcome. Typically, this
has been defined as an increase in baseline serum creatinine level
of 25% or an absolute increase of 44 mmol/l. It found that NAC had
no effect on preventing CIN on the basis of the standard diagnostic
definition, while it showed a preventive effect based on cystatin C
levels. Whether a newer urinary biomarker such as cystatin C may
identify kidney damage for CIN requires further research. Finally,
despite earlier studies having shown the association of CIN with
increased in-hospital morbidity and mortality, particularly in
patients that require dialysis, insufficient trials have been
designed to investigate the effect of NAC on these clinical
relevant outcomes. Thus, the present study did not identify
sufficient evidence for a meta-analysis to assess the effect of NAC
on these relatively rare, but key outcomes.
This meta-analysis of 19 placebo-controlled RCTs
indicated that oral NAC did not significantly reduce the incidence
of CIN. Also, it revealed that the combination of oral NAC and
sodium chloride may not provide additional benefits compared with
hydration with sodium chloride alone. Up to now, trials are too
inconsistent to warrant a conclusion on efficacy. Recently, it has
been found that oral NAC is able to confer a preventive effect of
CIN based on cystatin C. Therefore, further high quality RCTs are
required to confirm the safety and investigate the effect of oral
NAC on clinically relevant outcomes, such as in-hospital morbidity,
mortality and cost of medical care, particularly in patients that
require dialysis.
The present study was supported by the Science Fund
for Distinguished Young Scholars of the Fourth Affiliated Hospital
of Harbin Medical University (grant no. HYDSYJQ201504).
|
1
|
Tepel M, Aspelin P and Lameire N:
Contrast-induced nephropathy: A clinical and evidence-based
approach. Circulation. 113:1799–1806. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Thomsen HS: European Society of Urogenital
Radiology (ESUR) guidelines on the safe use of iodinated contrast
media. Eur J Radiol. 60:307–313. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
McCullough PA, Wolyn R, Rocher LL, Levin
RN and O'Neill WW: Acute renal failure after coronary intervention:
Incidence, risk factors, and relationship to mortality. Am J Med.
103:368–375. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Rihal CS, Textor SC, Grill DE, Berger PB,
Ting HH, Best PJ, Singh M, Bell MR, Barsness GW, Mathew V, et al:
Incidence and prognostic importance of acute renal failure after
percutaneous coronary intervention. Circulation. 105:2259–2264.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Nikolsky E, Mehran R, Turcot D, Aymong ED,
Mintz GS, Lasic Z, Lansky AJ, Tsounias E, Moses JW, Stone GW, et
al: Impact of chronic kidney disease on prognosis of patients with
diabetes mellitus treated with percutaneous coronary intervention.
Am J Cardiol. 94:300–305. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Bartholomew BA, Harjai KJ, Dukkipati S,
Boura JA, Yerkey MW, Glazier S, Grines CL and O'Neill WW: Impact of
nephropathy after percutaneous coronary intervention and a method
for risk stratification. Am J Cardiol. 93:1515–1519. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Mehran R, Aymong ED, Nikolsky E, Lasic Z,
Iakovou I, Fahy M, Mintz GS, Lansky AJ, Moses JW, Stone GW, et al:
A simple risk score for prediction of contrast-induced nephropathy
after percutaneous coronary intervention: Development and initial
validation. J Am Coll Cardiol. 44:1393–1399. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Parfrey PS, Griffiths SM, Barrett BJ, Paul
MD, Genge M, Withers J, Farid N and McManamon PJ: Contrast
material-induced renal failure in patients with diabetes mellitus,
renal insufficiency, or both. A prospective controlled study. N Eng
J Med. 320:143–149. 1989. View Article : Google Scholar
|
|
9
|
Rudnick MR and Goldfarb S: Pathogenesis of
contrast-induced nephropathy: Experimental and clinical
observations with an emphasis on the role of osmolality. Rev
Cardiovasc Med. 4 Suppl 5:S28–S33. 2003.PubMed/NCBI
|
|
10
|
Murphy SW, Barrett BJ and Parfrey PS:
Contrast nephropathy. J Am Soc Nephrol. 11:177–182. 2000.PubMed/NCBI
|
|
11
|
Wright RS, Anderson JL, Adams CD, Bridges
CR, Casey DE Jr, Ettinger SM, Fesmire FM, Ganiats TG, Jneid H,
Lincoff AM, et al: 2011 ACCF/AHA focused update of the Guidelines
for the Management of Patients With Unstable
Angina/Non-ST-Elevation Myocardial Infarction (Updating the 2007
Guideline): A report of the American College of Cardiology
Foundation/American Heart Association Task Force on Practice
Guidelines developed in collaboration with the American College of
Emergency Physicians, Society for Cardiovascular Angiography and
Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol.
59:1920–1959. 2011. View Article : Google Scholar
|
|
12
|
Tepel M, van der Giet M, Schwarzfeld C,
Laufer U, Liermann D and Zidek W: Prevention of
radiographic-contrast-agent-induced reductions in renal function by
acetylcysteine. N Engl J Med. 343:180–184. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Shalansky SJ, Vu T, Pate GE, Levin A,
Humphries KH and Webb JG: N-acetylcysteine for prevention of
radiographic contrast material-induced nephropathy: Is the
intravenous route best? Pharmacotherapy. 25:1095–1103. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Karimzadeh I, Khalili H, Sagheb MM and
Farsaei S: A double-blinded, placebo-controlled, multicenter
clinical trial of N-acetylcysteine for preventing amphotericin
B-induced nephrotoxicity. Expert Opin Drug Metab Toxicol.
11:1345–1355. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Baker CS, Wragg A, Kumar S, De Palma R,
Baker LR and Knight CJ: A rapid protocol for the prevention of
contrast induced renal dysfunction: The RAPPID study. J Am Coll
Cardiol. 41:2114–2118. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ochoa A, Pellizzon G, Addala S, Grines C,
Isayenko Y, Boura J, Rempinski D, O'Neill W and Kahn J: Abbreviated
dosing of N-acetylcysteine prevents contrast-induced nephropathy
after elective and urgent coronary angiography and intervention. J
Interv Cardiol. 17:159–165. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
MacNeill BD, Harding SA, Bazaril H, Patton
KK, Colon-Hernadez P, DeJoseph D and Jang IK: Prophylaxis of
contrast-induced nephropathy in patients undergoing coronary
angiography. Catheter Cardiovasc Interv. 60:458–461. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Briguori C, Manganelli F, Scarpato P, Elia
PP, Golia B, Riviezzo G, Lepore S, Librera M, Villari B, Colombo A
and Ricciardelli B: Acetylcysteine and contrast agent associated
nephrotoxicity. J Am Coll Cardiol. 40:298–303. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Diaz-Sandoval LJ, Kosowsky BD and Losordo
DW: Acetylcysteine to prevent angiography-related renal tissue
injury (the APART trial). Am J Cardiol. 89:356–358. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kay J, Chow WH, Chan TM, Lo SK, Kwok OH,
Yip A, Fan K, Lee CH and Lam WF: Acetylcysteine for prevention of
acute deterioration of renal function following elective coronary
angiography and intervention: A randomized controlled trial. JAMA.
289:553–558. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Shyu KG, Cheng JJ and Kuan P:
Acetylcysteine protects against acute renal damage in patients with
abnormal renal function undergoing a coronary procedure. J Am Coll
Cardiol. 40:1383–1388. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
ACT Investigators, . Acetylcysteine for
prevention of renal outcomes in patients undergoing coronary and
peripheral vascularangiography: Main results from the randomized
Acetylcysteine for Contrast-induced nephropathy Trial (ACT).
Circulation. 124:1250–1259. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Allaqaband S, Tumuluri R, Malik AM, Gupta
A, Volkert P, Shalev Y and Bajwa TK: Prospective randomized study
of N-acetylcysteine, fenoldopam and saline for prevention of
radiocontrast-induced nephropathy. Catheter Cardiovasc Interv.
57:279–283. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Amini M, Salarifar M, Amirbaigloo A,
Masoudkabir F and Esfahani F: N-acetylcysteine does not prevent
contrast-induced nephropathy after cardiac catheterization in
patients with diabetes mellitus and chronic kidney disease: A
randomized clinical trial. Trials. 10:452009. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Baskurt M, Okcun B, Abaci O, Dogan GM,
Kilickesmez K, Ozkan AA, Ersanli M and Gurmen T: N-acetylcysteine
versus N-acetylcysteine+theophylline for the prevention of contrast
nephropathy. Eur J Clin Invest. 39:793–179. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Oldemeyer JB, Biddle WP, Wurdeman RL,
Mooss AN, Cichowski E and Hilleman DE: Acetylcysteine in the
prevention of contrast induced nephropathy after coronary
angiography. Am Heart J. 146:E232003. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Durham JD, Caputo C, Dokko J, Zaharakis T,
Pahlavan M, Keltz J, Dutka P, Marzo K, Maesaka JK and Fishbane S: A
randomized controlled trial of N-acetylcysteine to prevent contrast
nephropathy in cardiac angiography. Kidney Int. 62:2202–2207. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Ferrario F, Barone MT, Landoni G,
Genderini A, Heidemperger M, Trezzi M, Piccaluga E, Danna P and
Scorza D: Acetylcysteine and non-ionic isosmolar contrast-induced
nephropathy - a randomized controlled study. Nephrol Dial
Transplant. 24:3103–3107. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Fung JW, Szeto CC, Chan WW, Kum LC, Chan
AK, Wong JT, Wu EB, Yip GW, Chan JY, Yu CM, et al: Effect of
N-acetylcysteine for prevention of contrast nephropathy in patients
with moderate to severe renal insufficiency: A randomized trial. Am
J Kidney Dis. 43:801–808. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Goldenberg I, Shechter M, Matetzky S,
Jonas M, Adam M, Pres H, Elian D, Agranat O, Schwammenthal E and
Guetta V: Oral acetylcysteine as an adjunct to saline hydration for
the prevention of contrast-induced nephropathy following coronary
angiography. A randomized controlled trial and review of the
current literature. Eur Heart J. 25:212–218. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Gomes VO, de Figueredo CE Poli, Caramori
P, Lasevitch R, Bodanese LC, Araújo A, Röedel AP, Caramori AP,
Brito FS Jr, Bezerra HG, et al: N-acetylcysteine does not prevent
contrast induced nephropathy after cardiac catheterisation with an
ionic low osmolality contrast medium: A multicentre clinical trial.
Heart. 91:774–778. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Kimmel M, Butscheid M, Brenner S, Kuhlmann
U, Klotz U and Alscher DM: Improved estimation of glomerular
filtration rate by serum cystatin C in preventing contrast induced
nephropathy by N-acetylcysteine or zinc - preliminary results.
Nephrol Dial Transplant. 23:1241–1245. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Ozcan EE, Guneri S, Akdeniz B, Akyildiz
IZ, Senaslan O, Baris N, Aslan O and Badak O: Sodium Bicarbonate,
N-acetylcysteine and saline for prevention of radiocontrast-induced
nephropathy. A comparison of 3 regimens for protecting
contrast-induced nephropathy in patients undergoing coronary
procedures. A single-center prospective controlled trial. Am Heart
J. 154:539–544. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Yang K, Liu W, Ren W and Lv S: Different
interventions in preventing contrast-induced nephropathy after
percutaneous coronary intervention. Int Urol Nephrol. 46:1801–1807.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Task Force on Myocardial Revascularization
of the European Society of Cardiology (ESC) and the European
Association for Cardio-Thoracic Surgery (EACTS, European
Association for Percutaneous Cardiovascular Interventions (EAPCI),
; Wijns W, Kolh P, Danchin N, Di Mario C, Falk V, Folliguet T, Garg
S, Huber K, et al: Guidelines on myocardial revascularization. Eur
Heart J. 31:2501–2555. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Stephan Windecker, Kolh P, Alfonso F,
Collet JP, Cremer J, Falk V, Filippatos G, Hamm C, Head SJ, Jüni P,
et al: 2014 ESC/EACTS guidelines on myocardial revascularization.
Rev Esp Cardiol (Engl Ed). 68:1442015.PubMed/NCBI
|
|
37
|
Nash K, Hafeez A and Hou S:
Hospital-acquired renal insufficiency. Am J Kidney Dis. 39:930–936.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Morcos SK, Thomsen HS and Webb JA:
Contrast-media-induced nephrotoxicity: A consensus report. Contrast
Media Safety Committee, European Society of Urogenital Radiology
(ESUR). Eur Radiol. 9:1602–1613. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Stacul F, van der Molen AJ, Reimer P, Webb
JA, Thomsen HS, Morcos SK, Almén T, Aspelin P, Bellin MF, Clement
O, et al: Contrast induced nephropathy: Updated ESUR contrast media
safety committee guidelines. Eur Radiol. 21:2527–2541. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Waikar SS and Bonventre JV: Creatinine
kinetics and the definition of acute kidney injury. J Am Soc
Nephrol. 20:672–679. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Thomsen HS and Morcos SK: Risk of
contrast-medium-induced nephropathy in high-risk patients
undergoing MDCT - a pooled analysis of two randomized trials. Eur
Radiol. 19:891–897. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Reddan D, Laville M and Garovic VD:
Contrast-induced nephropathy and its prevention: What do we really
know from evidence-based findings? J Nephrol. 22:333–351.
2009.PubMed/NCBI
|
|
43
|
Toprak O: What is the best definition of
contrast-induced nephropathy? Ren Fail. 29:387–388. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Ma YC, Zuo L, Chen JH, Luo Q, Yu XQ, Li Y,
Xu JS, Huang SM, Wang LN, Huang W, et al: Modified glomerular
filtration rate estimating equation for Chinese patients with
chronic kidney disease. J Am Soc Nephrol. 17:2937–2944. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Bräutigam M and Persson PB: Do iodinated
contrast media interfere with renal tubular creatinine secretion?
Radiology. 240:6152006. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Sun Z, Fu Q, Cao L, Jin W, Cheng L and Li
Z: Intravenous N-acetylcysteine for prevention of contrast-induced
nephropathy: A meta-analysis of randomized, controlled trials. PLoS
One. 8:e551242013. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Kim BJ, Sung KC, Kim BS, Kang JH, Lee KB,
Kim H and Lee MH: Effect of N-acetylcysteine on cystatin C-based
renal function after elective coronary angiography (ENABLE Study):
A prospective, randomized trial. Int J Cardiol. 138:239–245. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Molitoris BA, Levin A, Warnock DG,
Joannidis M, Mehta RL, Kellum JA, Ronco C and Shah SV; Acute Kidney
Injury Network working group, : Improving outcomes of acute kidney
injury: report of an initiative. Nat Clin Pract Nephrol. 3:439–442.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Chen Y, Hu S, Liu Y, Zhao R, Wang L, Fu G,
He Q, Su X, Zheng Y, Qi X, et al: Renal tolerability of iopromide
and iodixanol in 562 renally impaired patients undergoing cardiac
catheterisation: The DIRECT study. EuroIntervention. 8:830–838.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Stacul F, Adam A, Becker CR, Davidson C,
Lameire N, McCullough PA and Tumlin J; CIN Consensus Working Panel,
: Strategies to reduce the risk of contrast-induced nephropathy. Am
J Cardiol. 98:59K–77K. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Mueller C, Buerkle G, Buettner HJ,
Petersen J, Perruchoud AP, Eriksson U, Marsch S and Roskamm H:
Prevention of contrast media-associated nephropathy: randomized
comparison of 2 hydration regimens in 1620 patients undergoing
coronary angioplasty. Arch Intern Med. 162:329–336. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Erley CM, Duda SH, Rehfuss D, Scholtes B,
Bock J, Müller C, Osswald H and Risler T: Prevention of
radiocontrast-media-induced nephropathy in patients with
pre-existing renal insufficiency by hydration in combination with
the adenosine antagonist theophylline. Nephrol Dial Transplant.
14:1146–1149. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Sendeski M, Patzak A and Persson PB:
Constriction of the vasa recta, the vessels supplying the area at
risk for acute kidney injury, by four different iodinated contrast
media, evaluating ionic, nonionic, monomeric and dimeric agents.
Invest Radiol. 45:453–457. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Seeliger E, Sendeski M, Rihal CS and
Persson PB: Contrast-induced kidney injury: Mechanisms, risk
factors, and prevention. Eur Heart J. 33:2007–2015. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Seeliger E, Lenhard DC and Persson PB:
Contrast media viscosity versus osmolality in kidney injury:
Lessons from animal studies. Biomed Res Int. 2014:3581362014.
View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Parfrey P: The clinical epidemiology of
contrast-induced nephropathy. Cardiovasc Intervent Radiol. 28 Suppl
2:S3–S11. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Kiefer P, Vogt J and Radermacher P: From
mucolytic to antioxidant and liver protection: New aspects in the
intensive care unit career of N-acetylcysteine. Crit Care Med.
28:3935–3936. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Efrati S, Dishy V, Averbukh M, Blatt A,
Krakover R, Weisgarten J, Morrow JD, Stein MC and Golik A: The
effect of N-acetylcysteine on renal function, nitric oxide, and
oxidative stress after angiography. Kidney Int. 64:2182–2187. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Quintavalle C, Brenca M, De Micco F, Fiore
D, Romano S, Romano MF, Apone F, Bianco A, Zabatta MA, Troncone G,
et al: In vivo and in vitro assessment of pathways involved in
contrast media-induced renal cells apoptosis. Cell Death Dis.
2:e1552011. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Li JX, Shen YQ, Cai BZ, Zhao J, Bai X, Lu
YJ and Li XQ: Arsenic trioxide induces the apoptosis in vascular
smooth muscle cells via increasing intracellular calcium and ROS
formation. Mol Biol Rep. 37:1569–1576. 2010. View Article : Google Scholar : PubMed/NCBI
|