Introduction
Protrusion of lumbar intervertebral disc is one of
the most common diseases seen in department of orthopaedics with a
morbidity of 20–35% for people older than 50 years (1–3). Risk
factors include age, sex, bearing load for longtime (manual
labour), gestation and trauma. Symptoms range from lower limb ache
of different degrees, limb activity disorder, nerve injury and
nerve sweeny, and ~40–60% of patients need operative treatment
(4). As for the traditional surgery,
it combines the lumbar discectomy and fusion together and the
patient needs to stay in bed for a long time which can result in
complications such as bedsores, pneumonia and deep venous
thrombosis in the lower limbs. Microendoscopic discectomy (MED) has
the advantage of broad operation view, easier operation, minimal
damage to the tissue surrounding (5). However, the operation levels are
higher. The operative route and the operative process are similar
to traditional excision which has limited minimal invasion.
Percutaneous endoscopic lumbar discectom (PELD) combines the
endoscope technique and radiofrequency technique organically and
has the advantage of minimal invasion, minimal bleeding, easier
anesthesia and faster postoperative recovery. As a result, it has
been applied more widely in clinical use. In this study, PELD and
MED were administered for patients with protrusion of lumbar
intervertebral disc to analyze the safety and efficiency (6).
Patients and methods
Sample selection
We summarized 60 cases of patients with protrusion
for lumbar intervertebral disc at the Department of Spine Surgery
at first diagnosis and operative treatment retrospectively and the
inclusion criteria were: i) Diagnosis through computed tomography
(CT), magnetic resonance imaging (MRI) or contrast examination for
intervertebral disc; ii) patients with pain of different degrees in
the waist and lower limb and the results being positive for femoral
nerve stretch test or sciatic nerve streth test; and iii) patients
with indications of operation and the operative treatment being
expected to be effective. The exclusion standards were: i) Patients
with primary spinal stenosis, instraspinal neoplasm, spine trauma,
intervertebral disc compression fracture; ii) patients complicated
with underlying diseasessuch as organ dysfunction of heart, liver,
lungs, kidney, brain which cannot stand the risk of operation and
anesthesia; and iii) patients without enough clinical
information.
This study was approved by the Ethics Committee of
the Tongde Hospital and the written and signed informed consent was
obtained from the patients or their relatives. We divided the
patients into two groups, PELD and MED, according to the treatment
methods. The baseline information of the two groups were not
different as shown in Table I.
 | Table I.Comparison of the baseline information
of the two groups. |
Table I.
Comparison of the baseline information
of the two groups.
| Groups | PELD (n=30) | MED group (n=30) | t/χ2
test | P-value |
|---|
| Male/female | 16/14 | 17/13 | 0.067 | 0.795 |
| Age (years) | 54.8±6.5 | 53.6±6.4 | 0.233 | 0.724 |
| Course of disease
(months) | 3.2±1.3 | 3.3±1.4 | 0.256 | 0.681 |
| Protrusion of lumbar
intervertebral disc of central type | 6 (20.0) | 7 (23.3) | 0.269 | 0.874 |
| Side central
type | 16 (53.3) | 14 (46.7) |
|
|
| Extreme lateral
type | 8 (26.7) | 9 (30.0) |
|
|
| Lesion segments
L5-S1 | 12 (40.0) | 13 (43.3) | 0.299 | 0.960 |
| L4-5 | 6 (20.0) | 5 (16.7) |
|
|
| L2-4 | 5 (16.7) | 6 (20.0) |
|
|
|
T12-L2 | 7 (23.3) | 6 (20.0) |
|
|
| Radiating pain of
lower limb | 18 (60.0) | 16 (53.3) | 0.271 | 0.602 |
| Cauda equine
injury | 4 (13.3) | 6 (20.0) | 0.480 | 0. 488 |
| Lower limb activity
disorder | 10 (33.3) | 9 (30.0) | 0.077 | 0.781 |
Study methods
This study was completed by the same operating and
nursing team according to the standard medical process. Continuous
epidural anesthesia was given for the MED group and local
anesthesia for the PELD group.
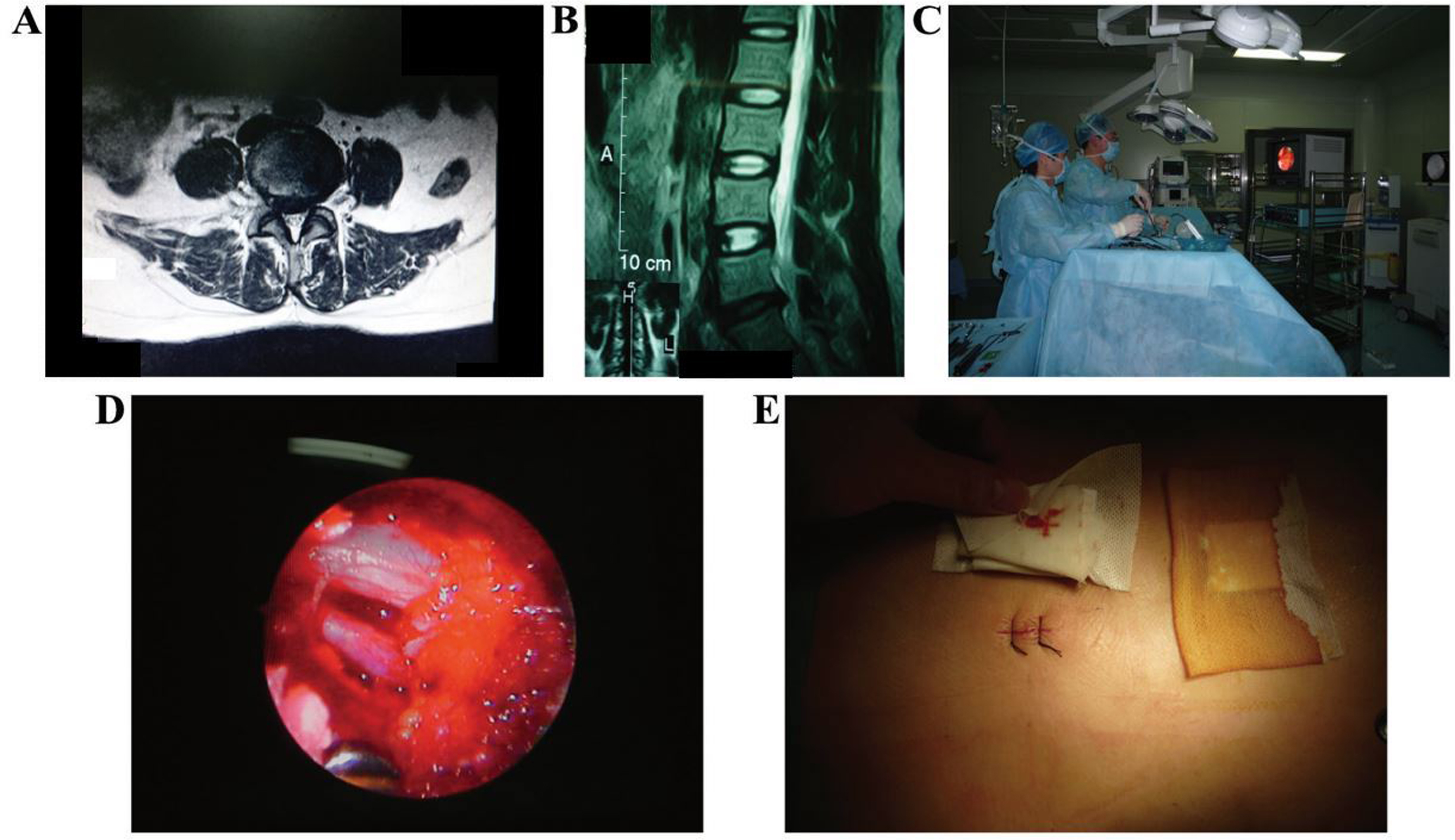
Patients in the MED group adopted a prone position,
lying on the spinal operation racks with abdomen hanging in the
air. We located the working routeway using X-ray machine (Philips
Research Laboratories, Eindhoven, Netherlands) for perspective. The
Kirschner wire (Nanjing Jiancheng Co., Nanjing, China) was inserted
into the right intervertebral space. We incised 1.8 cm by taking
the wire as center and fixed the working routeway through expanding
the insert by bushing by degrees. We cleared the soft tissue and
ligamentum flavum in sight and exposed the dural sac and nerve
root. We stripped the adhesion and pulled the nerve root towards
the outside through a nerve hook. We also exposed the protruding
intervertebral disc, used bipolar coagulation for hemostasis and
intervertebral disc scalpel for excision. We took the
intervertebral disc tissue of lesion out through nucleus pulposus
forceps holder and irrigated the working routeway with a sterile
saline solution of 0.9% and sutured the skin (Fig. 1).
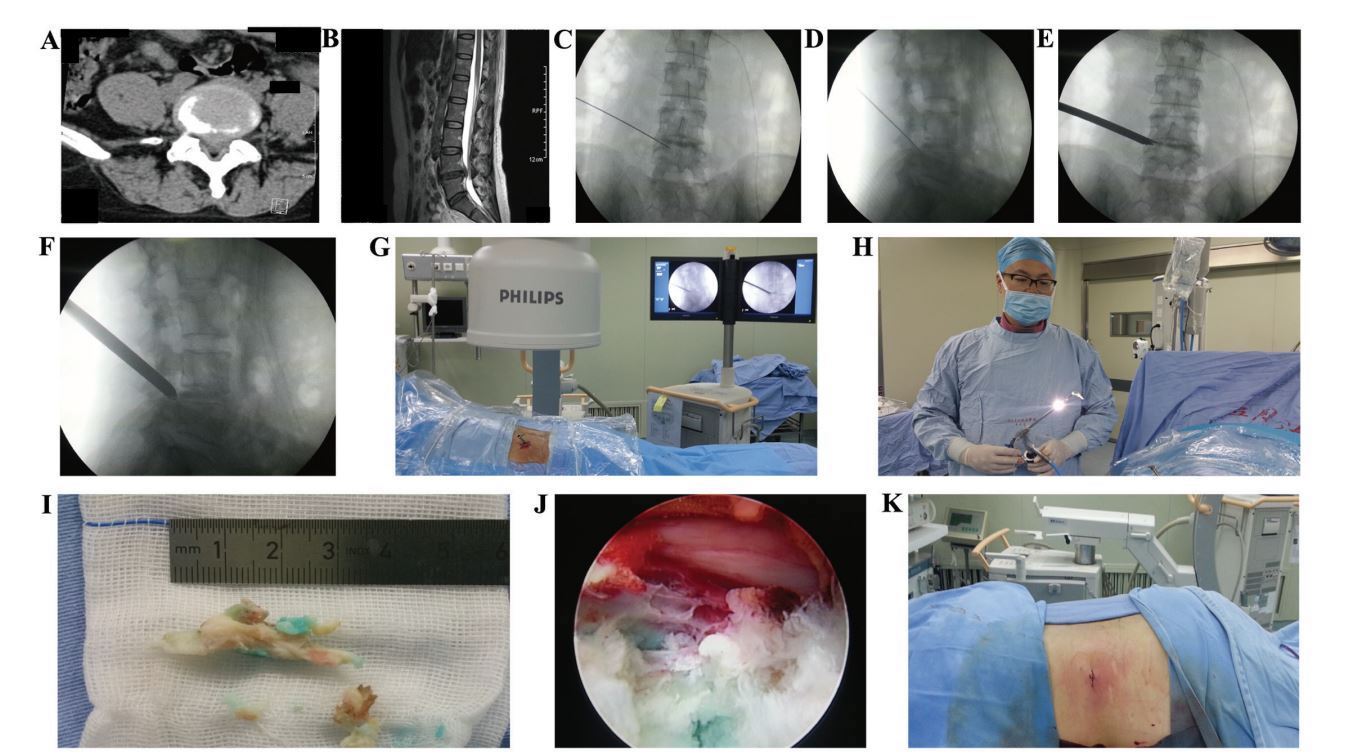
The operation process for the PELD group was as
follows: i) Locate the puncture point, demarcate the horizontal
line (which passes through the superior border of intervertebral
disc and the midcourt line of lumbar vertebra spinous process) and
side position line (which passes through superior border of
intervertebral disc along the dip direction of intervertebral
space); use the intersection of the two lines as the puncture
point. ii) Discography, under the post-anterior perspective of the
X-ray, use no. 18 puncture needle to puncture to the ideal position
through puncture point; penetrate into the protruding
intervertebral disc through no. 18 needle, put no. 22 aortography
needle into the center of intervertebral disc and inject the
contrast agent (with omnipaque to methylene blue of 3:1). iii)
Working routeway, make an incision of 0.7 cm taking no. 22 needle
as the centre and fix the working route way through inserting
expanding bushing by grades. iv) Excision, put the PTED in through
the working route; continue irrigation with 2,500 ml NaCl solution
of 0.9% with gentamicin (0.16 million U) and epinephrine (1 mg)
inside to keep the view clear. Find the nucleus pulposus of aizen
degeneration; make excision and bring it out and search and expose
the nerve fully. Use bipolar RF for the coagulation and hemostasis
of annulus fibrosus. iv) Irrigate the working routeway time again
with a 0.9% NaCl solution. The skin was sutured without drainage
tube (Fig. 2).
Observational index and evaluation
methods
We compared the operation time, cadaverine quantity
of bleeding during operation, average length of incision and the
time of rest after operation. We adopted VSA to evaluate the ache
levels, 0 (without ache) to 10 (unbearable sharp ache), for
evaluation. The dysfunction of patients was scored according to
oswestry dysfunction index (ODI) with the range from 0 (without
dysfunction) to 5 (with the most obvious dysfunction) and from
three points (10 items) of ache (ache level, influence on sleep),
single-ability (carry items, sitting, standing, walking) and
personal comprehensive ability (daily activities ability, social
activity, sexual life and outing excursion). We obtained the ODI
with 100 being divided by the score; thus, dysfunction is more
serious as the index is bigger. The average follow-up visit period
after operation was 18 months. The operation results can be divided
into four degrees of excellent, good, medium and poor according to
the improved MacNab standard. The conditions of complication during
perioperative period were recorded.
Statistical analysis
Statistical analysis software SPSS 19.0 (IBM,
Armonk, NY, USA) was used for data processing and all the
measurement data are shown as the mean ± standard deviation (SD).
We chose t-test for comparison among groups and compared the normal
distribution data of different points in time within group and
analyzed the variance of data through repeated measure. We adopted
the χ2 test (for rectification) for enumeration data.
The rank sum test was also used. P<0.05 was considered to
indicate a statistically significant difference.
Results
Comparison of the time of operation,
cadaverine quantity of bleeding during operation, average length of
incision and rest after operation
The operation time of the two groups is not
statistically significant. Furthermore, the average length of
incision and the length of stay were shortened for the PELD group
compared to the MED group. The difference was statistically
significant (P<0.05) as shown in Table II.
 | Table II.The comparison of the time of
operation, cadaverine quantity of bleeding during operation,
average length of incision and the time in bed after operation. |
Table II.
The comparison of the time of
operation, cadaverine quantity of bleeding during operation,
average length of incision and the time in bed after operation.
| Groups | The time of operation
(min) | Cadaverine quantity
of bleeding during operation (ml) | Average length of
incision (cm) | The time in bed after
operation (days) |
|---|
| PELD | 78.7±13.4 | 50.6±18.3 | 0.8±0.2 | 1.3±0.5 |
| MED | 76.6±15.5 | 100.7±46.5 | 1.7±0.6 | 4.6±0.7 |
| t-test | 0.676 | 5.325 | 5.854 | 5.621 |
| P-value | 0.324 | 0.024 | 0.020 | 0.022 |
Comparison of visual analogue scale
(VAS) scores
As shown in Table
III, the VAS scores of the two groups reduced as the time was
extended and there is no statistical significance of difference
between the two groups (P>0.05).
 | Table III.Comparison of VAS scores. |
Table III.
Comparison of VAS scores.
| Groups | Before operation | One month after
operation | Six months after
operation | Twelve months after
operation | F-value | P-value |
|---|
| PELD | 4.5±1.1 | 2.6±0.7 | 1.3±0.4 | 0.2±0.1 | 8.627 | <0.001 |
| MED | 4.6±1.2 | 2.5±0.8 | 1.5±0.5 | 0.2±0.1 | 8.457 | <0.001 |
| t-test | 0.386 | 0.453 | 0.541 | 0.006 |
|
|
| P-value | 0.645 | 0.582 | 0.461 | 0.948 |
|
|
Comparison of ODI scores
As shown in Table
IV, the ODI scores of both groups are decreased as the time was
extended; there is no statistical significance of difference
between the two groups (P>0.05).
 | Table IV.Comparison of ODI scores. |
Table IV.
Comparison of ODI scores.
| Groups | Before operation | One month after
operation | Six months after
operation | Twelve months after
operation | F-value | P-value |
|---|
| PELD | 30.8±7.4 | 11.6±3.8 | 5.5±1.4 | 1.3±0.4 | 16.235 | <0.001 |
| MED | 31.6±7.5 | 13.7±4.3 | 5.7±1.6 | 1.2±0.3 | 14.857 | <0.001 |
| t-test | 0.218 | 0.767 | 0.412 | 0.257 |
|
|
| P-value | 0.825 | 0.325 | 0.635 | 0.764 |
|
|
Comparison between treatment effects
and complications
It is not necessary to compare the difference
between treatment effects and complications of two groups
statistically (P>0.05). Both groups have severe wound infection,
intervertebral disc relapsing dislocation, nerve or blood vessel
damage and vertebral instability (Table
V).
 | Table V.Comparison between treatments effects
(example, %). |
Table V.
Comparison between treatments effects
(example, %).
| Groups | Cases | Excellent | Good |
| Qualified | Poor | Rate (excellent and
good) |
|---|
| PELD | 30 | 13 (43.3) | 15 (50.0) |
| 1 (3.3) | 1 (3.3) | 28 (93.3) |
| MED | 30 | 14 (46.7) | 13 (43.3) |
| 2 (6.7) | 1 (3.3) | 27 (90.0) |
| Z/χ2
test |
|
|
| 0.381 |
|
| <0.001 |
| P-value |
|
|
| 0.826 |
|
| 1.000 |
Discussion
Prolapse of lumbar intervertebral disc occurs when
the intervertebral disc has retrogression and is under external
force. In this case, the intervertebral disc tissue fiber is
damaged and has water loss, cauda equine and nerve root suffers
mechanical compression coming from nucleus pulposus which causes
extreme lumbago and radiating pain in lower limbs. Under serious
circumstances, it may lead to gatism, neurological deficit, foot
drop or even paralysis (7).
Microscopic endoscopic treatment is carried out in
place of display system, surgical channel and surgical instruments.
With the combination of micro-endoscopic technique and traditional
open surgery, the surgical field of micro-endoscopy will be
effectively amplified, and coupled with good lighting system
providing the doctor with a clearer field of vision. Therefore, it
minimizes damage to surrounding tissues by fine operation (8). However, due to the two-dimensional
image and under non-direct vision circumstances, it leads to larger
difficulties in operation and high-level requirements on the
surgeon. Local hospitals with limited medical resources may face
many difficulties for this operation (9). In addition, nerve root may be pulled in
surgery in order to expose protuberances which easily produces
nerve root damage and adhesion. It is the same with traditional
surgery, and is minimally invasive (10).
PELD can puncture and undergo accurate positioning,
after disc herniation foramen ipsilateral punctures directly to the
salient points from outside to inside, braking through the
posterior-lateral, far lateral and interlaminar approaching
limitations; in this way, you can reach any section segment
(11). Cannula inserted through to
expand the foramen intervertebral for grinding zygopophysis. It is
clearly viewed under the endoscope, and surgery can be done in a
direct vision manner. There is no structural damage on the ligament
and the neural plate does not need to be removed; thus, it is
conducive to the stability of the lumbar spine (12), and use of bipolar radiofrequency
coagulation of the annulus collagen fibers destruction and nerve
endings to reduce pain (13).
The present study shows that there were no
significant differences in the operation time between these two
groups. The PELD group has less blood loss than the MED group; it
has shorter average length of incision and shorter hospital stay
time than the MED group. In PELD and MED groups, the ODI and VAS
are significantly improved compared to those before surgery. The
rate (excellent and good) of PELD and MED groups is 93.0 and 90.0%,
respectively. There are no differences in perioperative
complication rates between the two groups. In conclusion, PELD and
MED are two types of minimally invasive surgical treatments of
lumbar disc herniation, whose short-term efficacy is satisfactory.
With the choice of surgical indications under strict circumstances,
PELD makes a small incision, which leads to less bleeding, fewer
traumas and faster postoperative recovery and other advantages, and
is a safe and effective surgical method.
References
|
1
|
Pandit P, Talbott JF, Pedoia V, Dillon W
and Majumdar ST: T1ρ and T2-based characterization of regional
variations in intervertebral discs to detect early degenerative
changes. J Orthop Res. 34:1373–1381. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Shin JS, Lee J, Kim MR, Jung J, Shin BC,
Lee MS and Ha IH: The short-term effect of integrated complementary
and alternative medicine treatment in inpatients diagnosed with
lumbar intervertebral disc herniation: A prospective observational
study. J Altern Complement Med. 22:533–543. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Riesenburger RI and David CA: Lumbar
microdiscectomy and microendoscopic discectomy. Minim Invasive Ther
Allied Technol. 15:267–270. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Huang CJ, Tang HW, Liang DB, Lou YM and
Guan W: Treatment of the recurrent lumbar disc herniation: A
comparison between endoscopic surgery and open surgery. Zhongguo Gu
Shang. 26:810–814. 2013.(In Chinese). PubMed/NCBI
|
|
5
|
Gadjradj PS and Harhangi BS: Percutaneous
transforaminal endoscopic discectomy for lumbar disk herniation.
Clin Spine Surg. 29:368–371. 2016.PubMed/NCBI
|
|
6
|
Gadjradj PS, van Tulder MW, Dirven CM,
Peul WC and Harhangi BS: Clinical outcomes after percutaneous
transforaminal endoscopic discectomy for lumbar disc herniation: A
prospective case series. Neurosurg Focus. 40:E32016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Orita S, Inage K, Sainoh T, Fujimoto K,
Sato J, Shiga Y, Kanamoto H, Abe K, Yamauchi K, Aoki Y, et al:
Lower lumbar segmental arteries can intersect over the
intervertebral disc in the oblique lateral interbody fusion
approach with a risk for arterial injury: Radiological analysis of
lumbar segmental arteries by using magnetic resonance imaging.
Spine (Phila Pa 1976). 42:135–142. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Zhao LJ, Jiang WY, Ma WH, Xu RM and Sun
SH: Micro-endoscopic discectomy for the treatment of lumbar disc
herniation in senile patients over seventy years old. Zhongguo Gu
Shang. 24:811–815. 2011.(In Chinese). PubMed/NCBI
|
|
9
|
Ye CP and Zhu JJ: Treatment of senile
lumbar nerve root canal stenosis with micro-endoscope discectomy.
Zhongguo Gu Shang. 26:805–809. 2013.(In Chinese). PubMed/NCBI
|
|
10
|
Sinkemani A, Hong X, Gao ZX, Zhuang SY,
Jiang ZL, Zhang SD, Bao JP, Zhu L, Zhang P, Xie XH, et al: Outcomes
of microendoscopic discectomy and percutaneous transforaminal
endoscopic discectomy for the treatment of lumbar disc herniation:
A comparative retrospective study. Asian Spine J. 9:833–840. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Fan G, Guan X, Sun Q, Hu A, Zhu Y, Gu G,
Zhang H and He S: Puncture reduction in percutaneous transforaminal
endoscopic discectomy with HE's lumbar LOcation (HELLO) system: A
cadaver study. PLoS One. 10:e01449392015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Fan G, Guan X, Zhang H, Wu X, Gu X, Gu G,
Fan Y and He S: Significant improvement of puncture accuracy and
fluoroscopy reduction in percutaneous transforaminal endoscopic
discectomy with novel lumbar location system: Preliminary report of
prospective Hello study. Medicine (Baltimore). 94:e21892015.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Hu DX, Zheng Q, Zhu B, Ying XZ and Wang
YF: Percutaneous intervertebral foramina endoscopic lumbar
discectomy decompression for elder patients with lumbar spinal
stenosis syndrome. Zhongguo Gu Shang. 27:194–198. 2014.(In
Chinese). PubMed/NCBI
|