Introduction
Hypertension is believed to be a major reason of
people deaths caused by cardiovascular diseases, which is largely
responsible for chronic kidney injury and end-stage renal disease
(1). Multiple therapeutic choices
may slow down the development and progression of hypertensive
nephropathy, a large number of hypertensive patients are still
ultimately suffering to end-stage renal disease (2). The deoxycorticosterone acetate or
high-salt diet-induced hypertension is associated with
amplification of renal injury in Goto Kakizaki (GK) rats (3). Renal impairment is a frequent problem
in cardiovascular diseases including hypertension (4). The destructive renal function
contributes to tubular interstitial fibrosis, vascular sclerosis
and glomerular sclerosis (5).
Activation of renin-angiotensin-aldosterone system, inflammation,
oxidative stress, endoplasmic reticulum stress, apoptosis and
mitochondrial dysfunction are vital contributors in hypertensive
nephropathy (6–9). The renal inflammation, tubular
interstitial fibrosis, proteinuria and glomerular sclerosis are
valuable markers for evaluation of renal dysfunction in chronic
kidney disease (10). Application of
angiotensin-converting enzyme inhibitor can reverse
hypertension-induced proteinuria and renal damage (11). It is well accepted that
antihypertensive therapy can retard the decrease in renal function
(12).
Hypertension is recognized as an independent risk
factor for chronic renal failure, and renal injury in response to
hypertension is reflected by glomerular and tubulointerstitial
damages, which is an important determinant for end-stage
nephropathy and renal dysfunction (13). Complementary therapies are
recommended as promising strategies for prevention and treatment of
hypertension and renal damages (14–16).
Vaccarin is isolated from Vaccaria segetalis seeds (17), which protects endothelial cells
against oxidative stress or high glucose-induced injury (18,19).
Bacterial cellulose and bacterial cellulose-vaccarin membranes
accelerate wound healing in mice (19). We recently established that
intraperitoneal injection of vaccarin ameliorate renovascular
hypertension and cardiovascular remodeling in rats (20). However, it is so far unclear whether
or not vaccarin can prevent the renal injury secondary to
hypertension and, if yes, what were the possible mechanisms.
Therefore, we assessed the effects of chronic infusion with
vaccarin on renal structure in renovascular hypertensive rats and
further attempted to clarify the underlying mechanisms.
Materials and methods
Animals
Male Sprague-Dawley rats weighing 160–180 g were
purchased from Vital River Laboratories Co., Ltd. (Beijing, China).
All experiments were conformed to the Guide for the Care and Use of
Laboratory Animal published by the US National Institutes of Health
(NIH publication, 8th edition, 2011). All procedures were complied
with the Experimental Animal Care and Use Committee of Jiangnan
University. All animals were caged in a temperature-controlled and
humidity-controlled room and they were free accessed to standard
chow and tap water. All rats were sacrificed under overdose of
anesthesia (pentobarbital sodium, peritoneal injection) to minimize
discomfort and pain.
Renovascular hypertensive models
The renovascular hypertensive models (two-kidney
one-clip, 2K1C) were produced as we previously described (21,22). In
short, the rats were anaesthetized by peritoneal injection of
pentobarbital sodium (60 mg/kg) ip. A retroperitoneal flank
incision was made to expose the right renal artery, and a U-shaped
silver clip of 0.2-mm internal diameter was used to partly occlude
the right renal artery under sterile techniques. The sham operated
rats (Sham) rats underwent similar surgery without clipping. Two
weeks after operation, the 2K1C rats received intraperitoneal
injection of saline, low dose of vaccarin (10 mg/kg; Shanghai
Shifeng Technology Co., Ltd., Shanghai, China), high dose of
vaccarin (30 mg/kg), captopril (30 mg/kg; Beijing Inoke Co., Ltd.,
Beijing, China) for 14 days, respectively. The sham operated rats
were treated with intraperitoneal injection of saline at the same
time. The concentration of vaccarin used in the present study was
determined according to our preliminary studies and other previous
reports (20,23–25).
Blood pressure and heart rate
measurement
The systolic blood pressure (SBP), diastolic blood
pressure (DBP), mean arterial pressure (MAP) and heart rate (HR)
measured using a a noninvasive computerized tail-cuff IITC blood
pressure system (MRBP-2; IITC Life Science Inc., Woodland Hills,
CA, USA) according to the manufacturer's instructions. The rats
were warmed for 30 min at 28°C in a bag before each measurement to
obtain steady pulse level. The SBP, DBP, MAP, and HR were averaged
by 10 measurements (26).
Angiotensin (Ang) II levels
The Ang II levels in the right kidney were
determined by using an enzyme-linked immunosorbent assay (ELISA)
kits (Boster Biological Technology Co., Ltd., Wuhan, China)
according to the manufacturer's descriptions. The reacted
microtiterplate was ended with stop solution, and the optical
density was read at 450 nm with a microtiter plate reader
(STNERGY/H4; BioTek Instruments, Inc., Winooski, VT, USA).
Angiotensin-converting enzyme (ACE)
activity assay
The activity of ACE was determined using
commercially available kits (Beijing Equation Biological Science
and Technology Co., Ltd., Beijing, China) according to the
manufacturer's instructions as previously described (27,28). The
activity of ACE in the right kidney was expressed in U/mg
protein.
Histopathology and
immunohistochemistry
The rats were sacrificed with overdose of
pentobarbital sodium, the right kidney were collected,
paraffin-embedded kidney sections (5 µm) were stained with Masson's
trichrome staining as previous report (29). Immunohistochemistry with angiotensin
type 1 (AT1) antibody (Abcam, Cambridge, MA, USA) were performed on
the right kidney. The relative AT1 positive cells were quantified
with the aid of ImageJ software.
TUNEL assay and ROS detection
The apoptosis of right kidney was assessed by
terminal deoxynucleotidyl transferase dUTP nick end labeling
(TUNEL) assay. In short, the sectioned kidney was stained using
fluorescein-conjugated TUNEL, and the cell nuclei were stained with
Hoechst staining. The TUNEL-positive cells were observed a
fluorescence microscope (80i; Nikon Corporation, Tokyo, Japan). The
apoptotic rate was quantified by counting TUNEL positive cells from
6 random fields and was expressed as a percentage of total cells.
The kidney sections were 2′,7′-dichlorofluorescein diacetate
(DCFH-DA, 10 µM) as previous report (30,31). The
fluorescence signals were captured with a multi-detection
microplate reader, and quantified with the Image-Pro Plus 6.0 by
using the same parameters. The measured fluorescence values were
normalized to the fluorescence in control groups.
Real-time quantitative PCR
analysis
Total RNA was obtained using TRIzol reagent. Equal
RNA levels were reversed transcribed into cDNA using HiScriptQ RT
SuperMix for qPCR (Vazyme Biotech Co., Ltd., Nanjing, China). The
real-time quantitative PCR was conducted using ChamQ™
SYBR® qPCR Master Mix (Vazyme Biotech Co., Ltd.). The
relative quantification of gene expression was calculated by using
the 2−ΔΔCt method (32).
The sequences of required primers were listed in the Table I.
 | Table I.Primers for real-time quantitative
PCR analysis in rats. |
Table I.
Primers for real-time quantitative
PCR analysis in rats.
| Gene | Primer | Sequence | Accession no. |
|---|
| Collagen I | Forward |
5′-GAGCCTAACCATCTGGCATCT-3′ | NM-053304.1 |
|
| Reverse |
5′-AGAACGAGGTAGTCTTTCAGCAAC-3′ |
|
| Collagen III | Forward |
5′-AGATGCTGGTGCTGAGAAG-3′ | NM-032085.1 |
|
| Reverse |
5′-TGGAAAGAAGTCTGAGGAAGG-3′ |
|
| Fibronectin | Forward |
5′-GTGAAGAACGAGGAGGATGTG-3′ | XM-006245159.1 |
|
| Reverse |
5′-GTGATGGCGGATGATGTAGC-3′ |
|
| GAPDH | Forward |
5′-GGAAAGCTGTGGCGTGAT-3′ | NM-017008.4 |
|
| Reverse |
5′-AAGGTGGAAGAATGGGAGTT-3′ |
|
Western blot analysis
The protein in right kidney was extracted in RIPA
lysis, and was electrophoresed, blotted, and then incubated with
indicated primary antibodies at 4°C overnight. The blots were then
incubated with appropriate secondary horseradish peroxidase
(HRP)-conjugated antibodies, the immunoreactive proteins were
visualized by enhanced chemiluminescence (Merck KGaA, Darmstadt,
Germany).
Reagents
Vaccarin (Fig. 1) was
purchased from Shanghai Shifeng Technology Co., Ltd. Cell Meter™
terminal deoxynucleotidyl transferase-mediated dUTP nick end
labeling (TUNEL) apoptosis assay kit was obtained from AAT
Bioquest, Inc. (Sunnyvale, CA, USA). DCFH-DA
(2′,7′-dichlorofluorescin diacetate) were obtained from
Sigma-Aldrich (Merck KGaA). The required sequences of paired
primers were synthesized by Sangon Biotech Co., Ltd. (Shanghai,
China). The primary antibodies against caspase-3, Bcl-2 associated
X (Bax), B cell lymphoma (Bcl)-2, AT1, NADPH oxidase (NOX)2, NOX4
and 3NT were purchased from Abcam. Antibodies against tumor
necrosis factor-α (TNF-α), interleukin 1β (IL-1β), and IL-6 and
HRP-labeled secondary antibodies were purchased from SANYING
Biotechnology Co., Ltd. (Wuhan, China). Antibodies against GAPDH,
and the horseradish peroxidase conjugated secondary antibody were
purchased from Vazyme Biotech Co., Ltd. Immunohistochemistry kit
and diaminobenzidine (DAB) were obtained from Boster Biological
Technology Co., Ltd.
Statistical analysis
All results were defined as mean ± SD. Comparisons
within two groups were made by Student's t-test. Statistical
analysis was performed by ANOVA/Dunnet t-test for multiple group
comparisons. The criterion for statistical significance was set at
P<0.05.
Results
General data
There was no significant difference in body weight
(BW) between the five groups at the end of the 4th week after 2K1C
or sham operation. The right kidney weight (RKW) was substantially
decreased, but the left kidney weight (LKW) was obviously increased
in 2K1C rats compared with those in Sham-operated rats, which were
reversed by high dose of vaccarin (HDV) and captopril. The lowed
RKW/BW ratio and enhanced LKW/BW ratio in 2K1C rats were restored
by both high dose of vaccarin and Captopril (Table II).
 | Table II.Body weight, kidney weight at the end
of the fourth week. |
Table II.
Body weight, kidney weight at the end
of the fourth week.
| Variables | Sham | 2K1C-Veh | 2K1C-LDV | 2K1C-HDV | 2K1C-Captopril |
|---|
| BW, g | 331.6±26.1 | 338.6±27.2 | 331.0±23.3 | 333.7±18.7 | 337.1±25.6 |
| RKW, mg | 840.0±40.7 |
280.9±53.6a | 359.0±99.9 |
489.0±177.3b |
812.4±91.2b |
| LKW, mg | 848.3±59.1 |
1497.6±330.0a | 1166.4±142.0 |
991.0±81.4b |
900.0±102.8b |
| RKW/BW | 2.5±0.2 |
0.8±0.2a | 1.1±0.4 |
1.5±0.5b |
2.4±0.2b |
| LKW/BW | 2.6±0.2 |
4.4±0.8a | 3.5±0.5 |
3.0±0.2b |
2.7±0.3b |
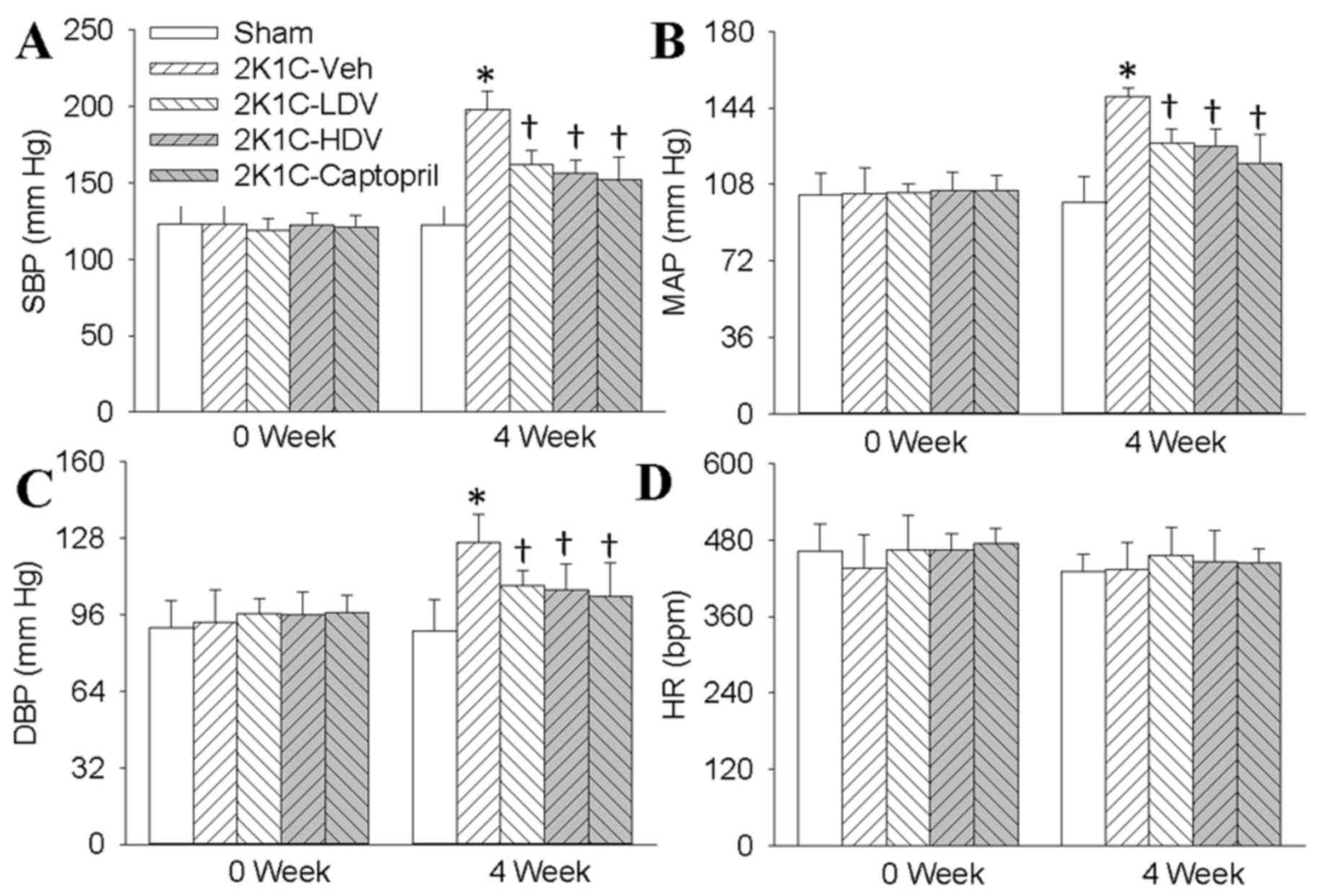
Effects of vaccarin on blood pressure
and heart rate in 2K1C rats
The SBP (Fig. 2A),
MAP (Fig. 2B), DBP (Fig. 2C) registered on tail artery in
conscious state of 2K1C rats were significantly higher than those
in Sham rats four weeks after surgery. It is interesting that
vaccarin at both low dose and high dose effectively reduced SBP
(Fig. 2A), MAP (Fig. 2B), DBP (Fig. 2C) in 2K1C rats, but the high dose of
vaccarin caused a similar effect as captopril. There was no
significant difference in HR (Fig.
2D) among groups at the end of four weeks.
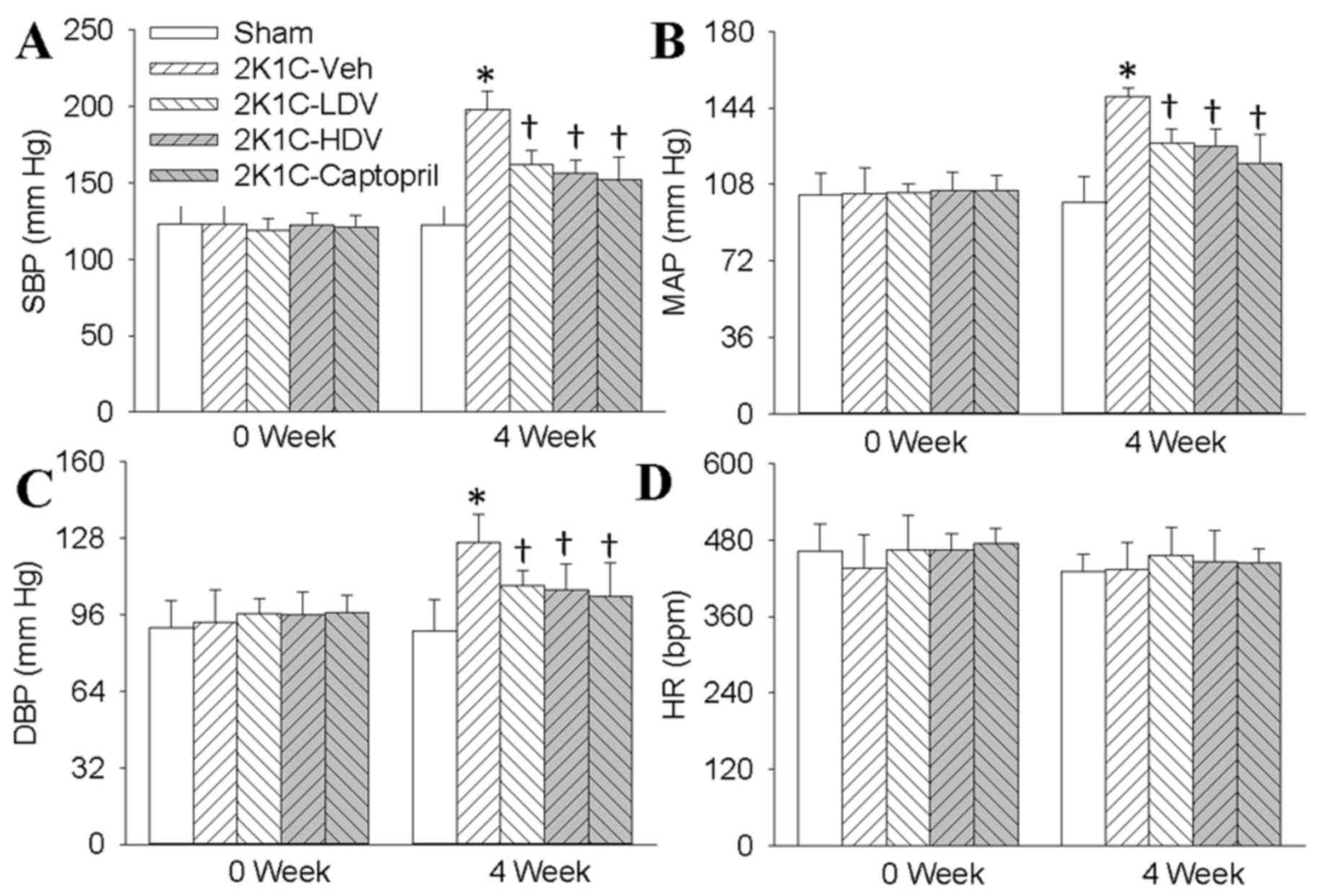 | Figure 2.Effects of Vaccarin on the BP and HR
in sham-operated or 2K1C rats. The 2K1C rats were subjected to
intraperitoneal injection low dose of Vaccarin (LDV, 10 mg/kg/day),
high dose of Vaccarin (HDV, 30 mg/Kg/day) or captopril (30
mg/Kg/day) for 14 days after 2 weeks' operation. The (A) SBP, (B)
MAP, (C) DBP and (D) HR were measured with a noninvasive
computerized tail-cuff system in conscious rats. Values are
expressed as means ± SD. (n=7 rats/group). *P<0.05 vs. Sham;
†P<0.05 vs. 2K1C-Veh (vehicle). BP, blood pressure; HR, heart
rate; 2K1C, two-kidney, one clip; DBP, diastolic blood pressure;
SBP, systolic blood pressure; MAP, mean arterial pressure. |
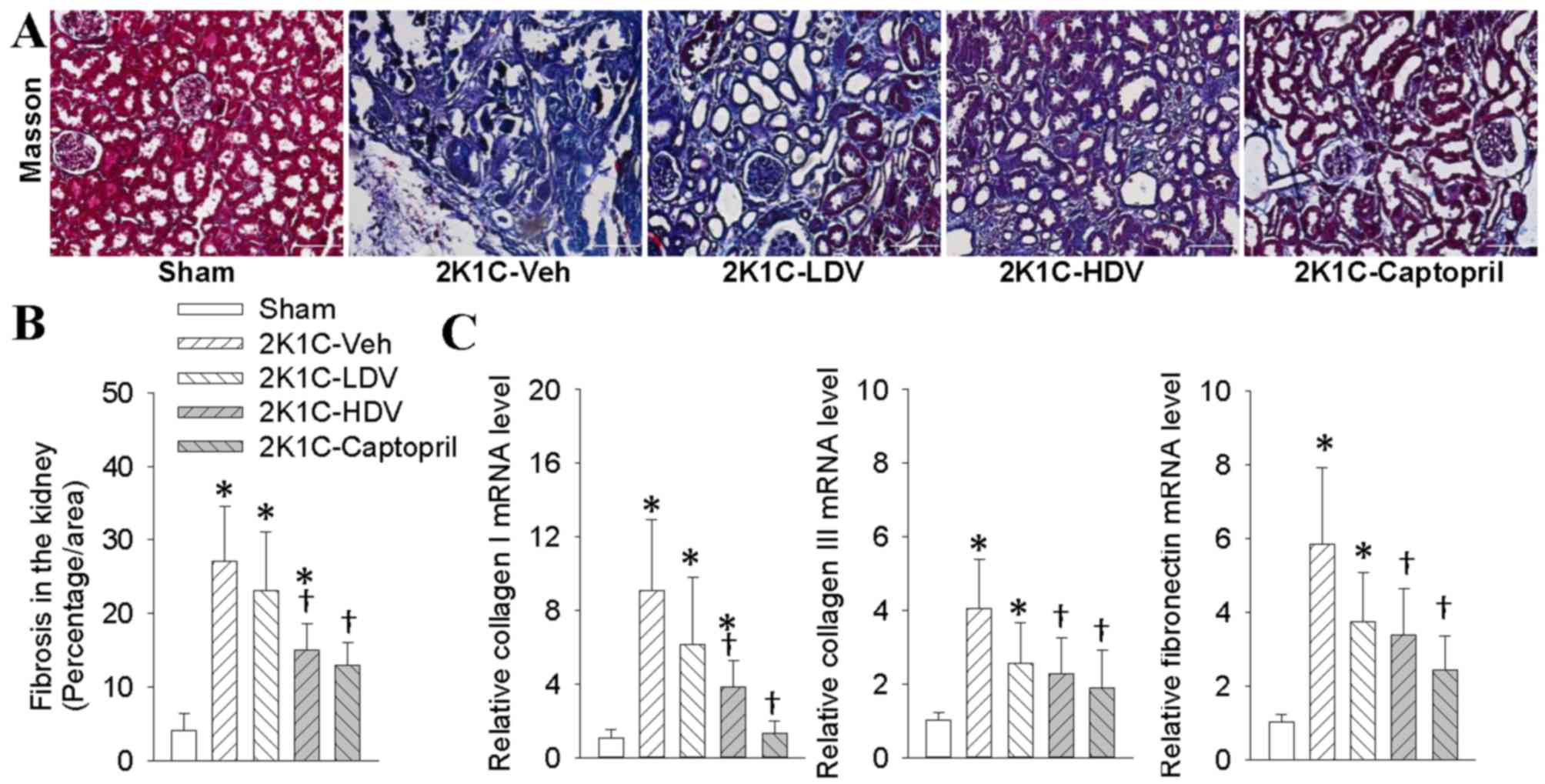
Effects of vaccarin on renal fibrosis
in 2K1C rats
Masson's staining showed that the renal fibrosis was
significantly elevated in 2K1C rats compared with Sham rats, which
was consistent with previous findings (33–35).
Intraperitoneally administrated with high dose of vaccarin or
captopril abrogated the fibrosis in the right kidney in 2K1C rats
(Fig. 3A and B), which were further
confirmed by the down-regulated markers of fibrosis (collagen-I,
collagen-III and fibronectin, Fig.
3C) in the right kidney of 2K1C rats.
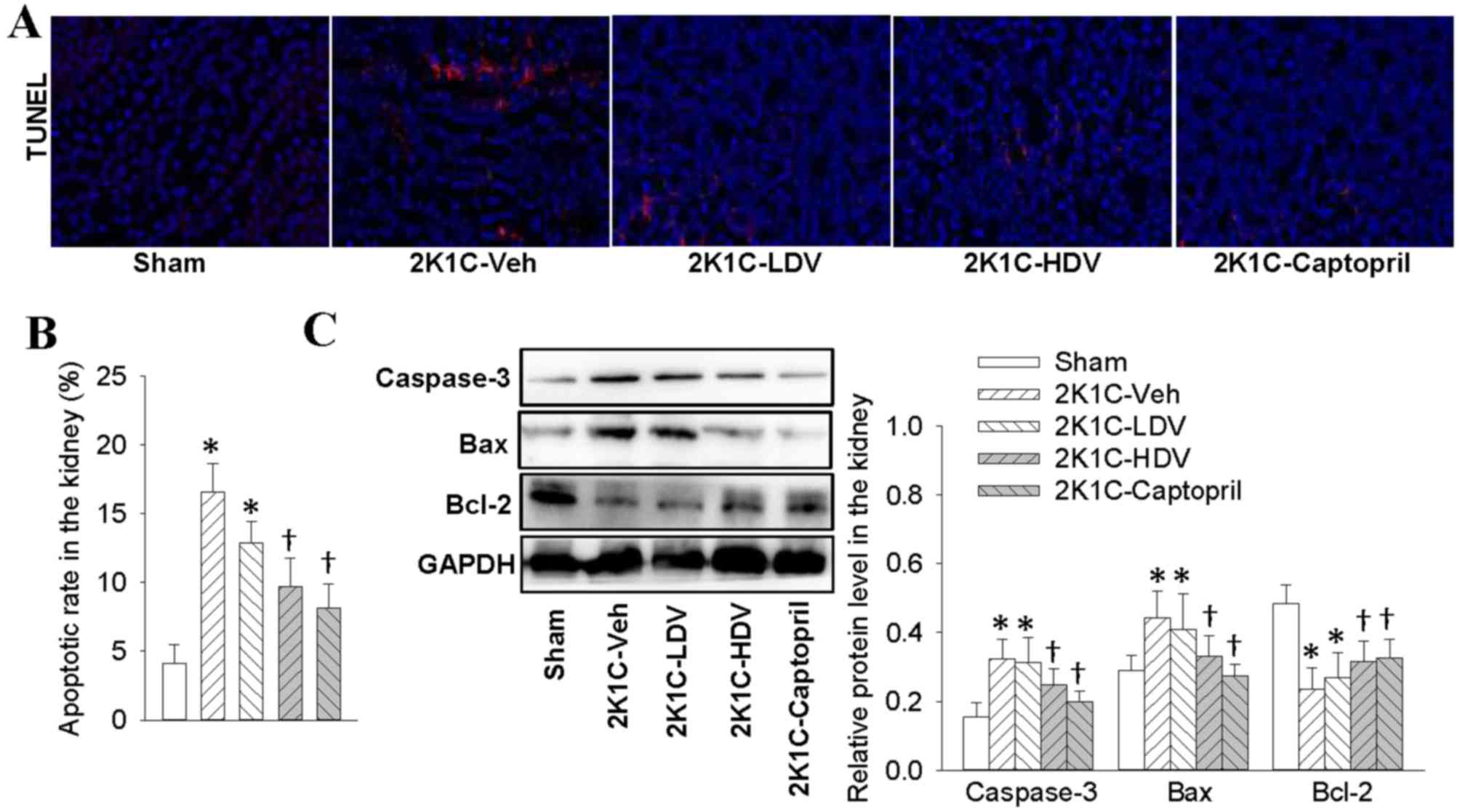
Effects of vaccarin on renal cell
apoptosis in 2K1C rats
The 2K1C rats had a greater cell apoptotic rate in
the right kidney compared with normotensive rats. Compared with
rats in the 2K1C group, both high dose of vaccarin and captopril
suppressed renal cell apoptosis of right kidney, as revealed by
TUNEL staining (Fig. 4A and B). The
expressions of pro-apoptotic proteins including caspase-3 and Bax
were upregulated, whereas anti-apoptosis protein Bcl-2 was
decreased in 2K1C rats, which were treated by high dose of vaccarin
and captopril (Fig. 4C).
Effects of vaccarin on oxidative
stress in 2K1C rats
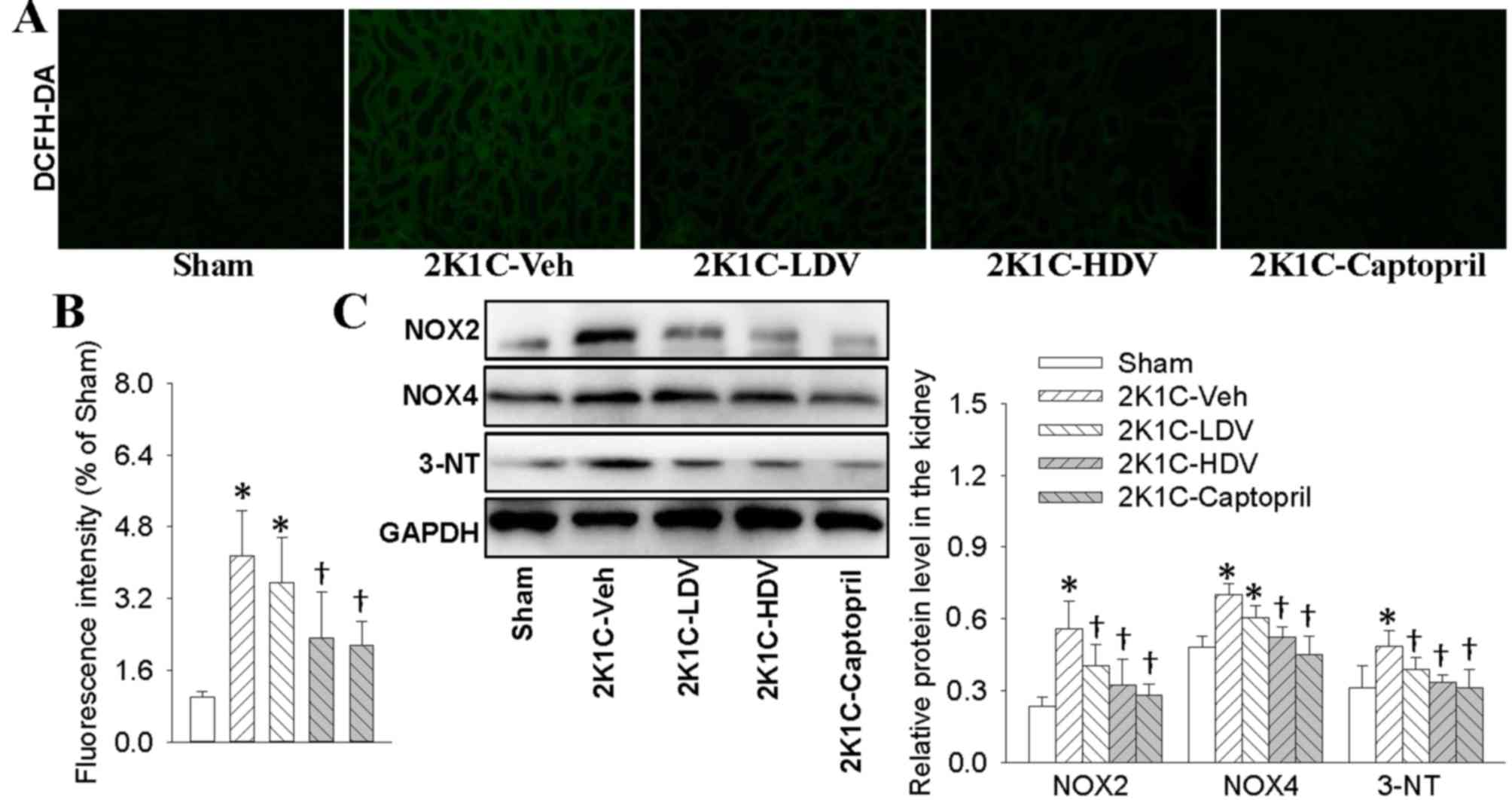
Immunofluorescence revealed that 2K1C rats exhibited
higher superoxide in the right kidney, as determined by fluorescent
labeled DCFH-DA in comparison with Sham rats (Fig. 5A and B). When compared with Sham
rats, 2K1C rats had more NOX2, NOX4, and 3NT protein levels in the
right kidney, as measured by western blot analysis (Fig. 5C). Interestingly, chronic application
of high dose of vaccarin and captopril prevented the increase in
oxidative stress related markers in right kidney of 2K1C rats
(Fig. 5).
Effects of vaccarin on inflammatory
cytokines in 2K1C rats
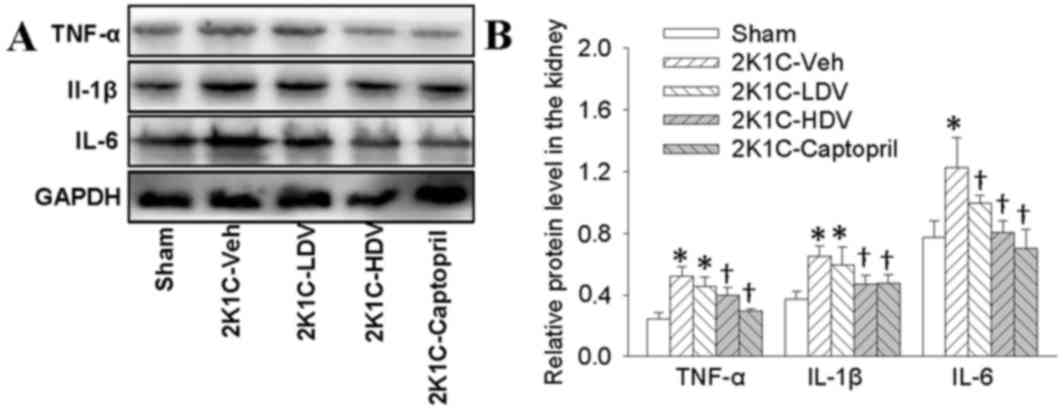
We observed that the protein expressions of TNF-α,
IL-1β and IL-6 were higher in the right kidney of 2K1C rats than
those in Sham rats, both high dose of vaccarin and captopril
treatment resulted in significant decreases in TNF-α, IL-1β and
IL-6 protein levels in 2K1C rats (Fig.
6).
Effects of vaccarin on Ang II and AT1
receptors in 2K1C rats
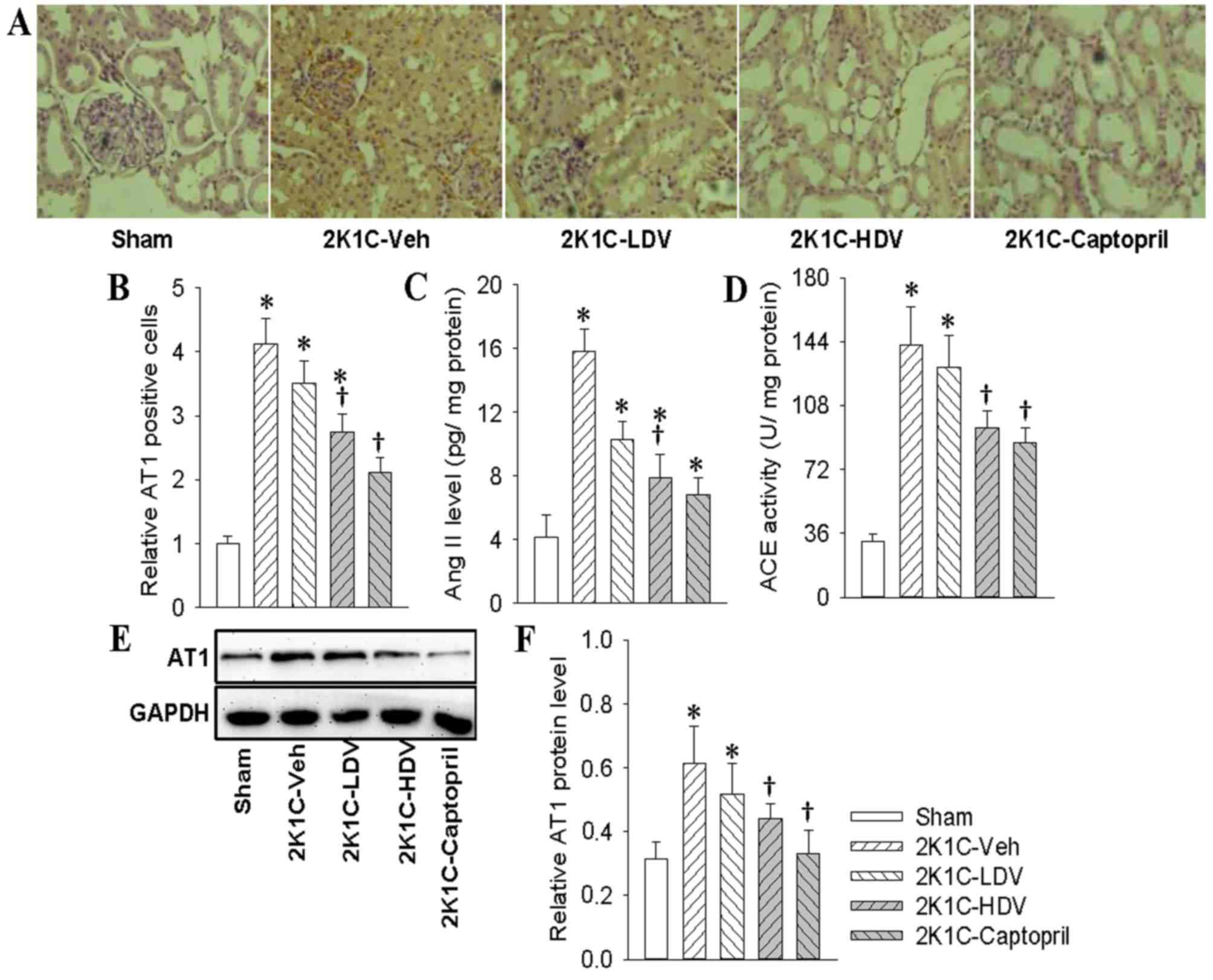
Immunohistochemical results revealed that AT1
receptor positive cells were up-regulated in right kidney of 2K1C
rats in comparison with Sham rats, chronic intraperitoneal infusion
of high dose of vaccarin and captopril prevented the AT1 receptor
positive cells in renovascular hypertensive rats (Fig. 7A and B). Ang II levels in the right
kidney was augmented in 2K1C rats, which was prevented by high dose
of vaccarin and captopril (Fig. 7C).
Our results also showed that the ACE activity in the right kidney
was higher in 2K1C rats than that in Sham rats. Similarly, vaccarin
treatment attenuated the changes in the ACE activity (Fig. 7D). Western blot further demonstrated
that high dose of vaccarin and captopril treatment attenuated the
upregulated AT1 protein expressions in 2K1C rats (Fig. 7E and F).
Discussion
Chronic kidney disease is a prevalent medical
condition with increased morbidity worldwide (36). Hypertension is an important
pathogenic factor that participates in the deterioration of renal
function, and many patents with hypertension eventually develop
chronic kidney disease (37).
Hypertension is one of the most common comorbidities in patients
with chronic kidney disease, more than 85% of patients with stage
3–5 chronic kidney disease are complicated with hypertension
(38). Vaccarin is believed to play
a protective role in endothelial dysfunction. However, the
therapeutic effects of vaccarin on hypertensive kidney damage have
not been researched. In this study, we demonstrated for the first
time that vaccarin not only normalized blood pressure, but also
attenuates renal fibrosis, renal cell apoptosis, oxidative stress,
inflammatory response, Ang II and AT1 receptors expressions in 2K1C
renovascular hypertensive rats. These results suggested that
vaccarin exerted antioxidant, antifibrotic, antiapoptotic and
anti-inflammatory effects in hypertensive renal injury associated
with downregulation of Ang II/AT1 system in 2K1C rats.
Renal fibrosis is one of the characteristics in
end-stage renal failure, which may result from hypertension and
diabetic nephropathy (39).
Progressive destructive function of kidney is associated with
tubular interstitial fibrosis in hypertension. It is reported that
gene deletion of growth arrest-specific protein 6 lowed renal
inflammation and renal fibrosis (40). The renal apoptosis is enhanced in the
right kidney in 2K1C rats (41,42).
Administration of angiotensin- (1–7) improves
glomerular tuft volume and decreases tubular apoptosis in Akita
mice (43). In this study, our data
showed that vaccarin caused reductions in collagen synthesis in
right kidney of 2K1C rats. Furthermore, the increased renal cell
apoptosis rate evidenced by TUNEL staining, augmented pro-apoptotic
proteins including caspase-3, Bax, and downregulated anti-apoptosis
protein Bcl-2 in 2K1C rats were treated by vaccarin treatment.
These results suggested that vaccarin may be beneficial to kidney
via targeted inhibition of renal fibrosis and apoptosis.
Oxidative stress plays a key role in renal
dysfunction and hypertension (44–46).
Excessive ROS production response to oxidative stress may affect
all types of intrinsic kidney cells (47). Oxidative stress leads to podocyte
apoptosis and subsequent segmental glomerulosclerosis, resulting in
kidney damage in hypertension (48).
In addition, oxidative stress also induces the myofibroblasts
accumulation in the kidney and remodeling of the extracellular
matrix of the tubulointerstitium (48). NOXs are major sources of ROS
production within the kidney (49).
It has been established that the increased levels of medullary NOX2
and tissue ROS in Dahl salt-sensitive (SS) hypertensive rats are
alleviated by chronic medullary interstitial infusions of NOX
inhibitor apocynin (50). NOX4 is
also abundantly expressed in the kidney, and knock out of NOX4
blocked oxidative stress, protein matrix production, and kidney
injury in the kidney of SS rat (51). 3-NT is taken as a marker for
peroxynitrite-evoked oxidative stress (52). In the present study, we showed that
the ROS, NOX2, NOX4 and 3NT expressions were significantly
increased in the 2K1C rats compared to those in the Sham rats,
However, these effects were decreased following vaccarin treatment.
These results indicated that vaccarin exhibited an obvious
improvement in oxidative stress injury in 2K1C rats.
Inflammation is a major player in
hypertension-associated of kidney disease. Oxidative stress and
inflammation in kidney may synergistically contribute to the
pathogenesis of renal injury (53).
The glomerular microinflammation is occurred in persistent systemic
hypertension state (54). Treatment
with statin abated the renal inflammation and podocyte damage in
DOCA-salt hypertension rats (55).
Pharmacological inhibition of galectin-3 reduces inflammatory
cytokines, and extracellular matrix proteinases, and renal fibrosis
in TGR (mREN)27 (REN2) hypertensive rats (4). The levels of TNF-α are upregulated in
the kidney of Ang II-dependent hypertensive models and associated
kidney disease (56).
Anti-inflammatory therapy may be promising therapeutic strategy for
hypertensive kidney damage. Our results showed that vaccarin
treatment decreased the expressions of inflammatory mediators
including TNF-α, IL-1β and IL-6 in the right kidney of 2K1C rats.
These data hinted that vaccarin may act anti-inflammatory effects
to protect kidney from injury in 2K1C renovascular hypertensive
rats.
The renin-angiotensin system (RAS) has a critical
role in mammalian homeostasis (57).
The RAS family consists of angiotensinogen, renin,
angiotensin-converting enzyme, Ang II and AT1 receptors, and other
main components, among which, Ang II and AT1 receptors displayed
powerful effects on kidney damage by a variety of mechanisms in
chronic kidney disease (58).
Mounting evidence demonstrates that local intrarenal RAS activation
may directly dictate kidney damage (59). Ang II binds to AT1 receptors to
stimulate generation of reactive oxygen species, and renal
inflammation, which are synergistically for the initiation and
progression of renal damage in hypertension (60). It has been established that Ang II
infusion leads to hypertension and renal fibrosis in mice or rats
(61). The abnormal formation of Ang
II triggers systemic hypertension and renal damages associated with
activation of fibrogenic, pro-inflammatory and apoptotic pathways
(6). AT1 receptor antagonist
Losartan is used to treat hypertension and targeted renal damage.
Our study showed that the elevated SBP, MAP, DBP, Ang II and AT1
receptor levels were increased in 2K1C rats in comparison with Sham
rats, which were partially abolished by vaccarin in 2K1C rats.
These results implied that vaccarin may counteract Ang II/AT1
system in the kidney to impede renal fibrosis, apoptosis, ROS
generation and inflammatory response, thus protecting against
hypertension-related renal damages.
Taken together, our results provided for the first
time that vaccarin protected the 2K1C rats from renal oxidative
stress, renal inflammatory response, renal injury and hypertension.
Vaccarin may be employed as a complementary and alternative
pharmacological agent that ameliorates hypertension and renal
function detriment in subjects who were predisposed to
hypertension. Nevertheless, as a natural product, high dose of
vaccarin at least showed the similar protective effects on
hypertension and cardiovascular remodeling as captopril from animal
research. In addition, such ACE inhibitors including captopril have
clinical side effects including cough, angioneurotic edema, and
deleterious effects during pregnancy (62,63). In
terms of vaccarin, there are still many unsolved problems, such as
whether vaccarin can be employed as a prescription for hypertension
in hypertensive patients, whether combination of vaccarin with
classical antihypertensive drugs exerted better effect and less
adverse reactions on hypertension. Further studies are needed
regarding the more detailed role of vaccarin in hypertension and
cardiovascular remodeling.
Acknowledgements
This work was supported by Fundamental Research
Funds for the Central Universities (JUSRP11745), Public Health
Research Center at Jiangnan University (grant no. JUPH201504),
Jiangsu Natural Science Foundation of China (grant no. BK20170179)
and Project funded by China Postdoctoral Science Foundation
(2017M611688).
References
|
1
|
Wang Z, do Carmo JM, Aberdein N, Zhou X,
Williams JM, da Silva AA and Hall JE: Synergistic interaction of
hypertension and diabetes in promoting kidney injury and the role
of endoplasmic reticulum stress. Hypertension. 69:879–891. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Retnakaran R, Cull CA, Thorne KI, Adler AI
and Holman RR; UKPDS Study Group, : Risk factors for renal
dysfunction in type 2 diabetes: U.K. Diabetes. 55:1832–1839. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Janssen U, Riley SG, Vassiliadou A, Floege
J and Phillips AO: Hypertension superimposed on type II diabetes in
Goto Kakizaki rats induces progressive nephropathy. Kidney Int.
63:2162–2170. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Frenay AR, Yu L, van der Velde AR,
Vreeswijk-Baudoin I, López-Andrés N, van Goor H, Silljé HH, Ruifrok
WP and de Boer RA: Pharmacological inhibition of galectin-3
protects against hypertensive nephropathy. Am J Physiol Renal
Physiol. 308:F500–F509. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Becker GJ and Hewitson TD: The role of
tubulointerstitial injury in chronic renal failure. Curr Opin
Nephrol Hypertens. 9:133–138. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Padda RS, Shi Y, Lo CS, Zhang SL and Chan
JS: Angiotensin-(1–7): A novel peptide to treat hypertension and
nephropathy in diabetes? J Diabetes Metab. 6:2015.PubMed/NCBI
|
|
7
|
Miloradović Z, Ivanov M, Jovović D,
Karanović D, Vajić UJ, Marković-Lipkovski J, Mihailović-Stanojević
N and Milanović JG: Angiotensin 2 type 1 receptor blockade
different affects postishemic kidney injury in normotensive and
hypertensive rats. J Physiol Biochem. 72:813–820. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Gai Z, Gui T, Hiller C and Kullak-Ublick
GA: Farnesoid X receptor protects against kidney injury in
uninephrectomized obese mice. J Biol Chem. 291:2397–2411. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Linkermann A, Chen G, Dong G, Kunzendorf
U, Krautwald S and Dong Z: Regulated cell death in AKI. J Am Soc
Nephrol. 25:2689–2701. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Granger JP: An emerging role for
inflammatory cytokines in hypertension. Am J Physiol Heart Circ
Physiol. 290:H923–H924. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Brouwers FP, de Boer RA, van der Harst P,
Struck J, de Jong PE, de Zeeuw D, Gans RO, Gansevoort RT, Hillege
HL, van Gilst WH and Bakker SJ: Influence of age on the prognostic
value of mid-regional pro-adrenomedullin in the general population.
Heart. 98:1348–1353. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Peterson JC, Adler S, Burkart JM, Greene
T, Hebert LA, Hunsicker LG, King AJ, Klahr S, Massry SG and Seifter
JL: Blood pressure control, proteinuria, and the progression of
renal disease. The Modification of Diet in Renal Disease Study. Ann
Intern Med. 123:754–762. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Crews DC, Plantinga LC, Miller ER III,
Saran R, Hedgeman E, Saydah SH, Williams DE and Powe NR; Centers
for Disease Control and Prevention Chronic Kidney Disease
Surveillance Team, : Prevalence of chronic kidney disease in
persons with undiagnosed or prehypertension in the United States.
Hypertension. 55:1102–1109. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Veeramani C, Al-Numair KS, Chandramohan G,
Alsaif MA and Pugalendi KV: Antihyperlipidemic effect of Melothria
maderaspatana leaf extracts on DOCA-salt induced hypertensive rats.
Asian Pac J Trop Med. 5:434–439. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Yu D, Shi M, Bao J, Yu X, Li Y and Liu W:
Genipin ameliorates hypertension-induced renal damage via the
angiotensin II-TLR/MyD88/MAPK pathway. Fitoterapia. 112:244–253.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Liu XP, Pang YJ, Zhu WW, Zhao TT, Zheng M,
Wang YB, Sun ZJ and Sun SJ: Benazepril, an angiotensin-converting
enzyme inhibitor, alleviates renal injury in spontaneously
hypertensive rats by inhibiting advanced glycation
end-product-mediated pathways. Clin Exp Pharmacol Physiol.
36:287–296. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Balsevich JJ, Ramirez-Erosa I, Hickie RA,
Dunlop DM, Bishop GG and Deibert LK: Antiproliferative activity of
Saponaria vaccaria constituents and related compounds. Fitoterapia.
83:170–181. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Xie F, Cai W, Liu Y, Li Y, Du B, Feng L
and Qiu L: Vaccarin attenuates the human EA.hy926 endothelial cell
oxidative stress injury through inhibition of Notch signaling. Int
J Mol Med. 35:135–142. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Qiu Y, Qiu L, Cui J and Wei Q: Bacterial
cellulose and bacterial cellulose-vaccarin membranes for wound
healing. Mater Sci Eng C Mater Biol Appl. 59:303–309. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Zhu X, Zhou Z, Zhang Q, Cai W, Zhou Y, Sun
H and Qiu L: Vaccarin administration ameliorates hypertension and
cardiovascular remodeling in renovascular hypertensive rats. J Cell
Biochem. Jul 6–2017.(Epub ahead of print).
|
|
21
|
Zhang LL, Ding L, Zhang F, Gao R, Chen Q,
Li YH, Kang YM and Zhu GQ: Salusin-β in rostral ventrolateral
medulla increases sympathetic outflow and blood pressure via
superoxide anions in hypertensive rats. J Hypertens. 32:1059–1067.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Zhou YB, Sun HJ, Chen D, Liu TY, Han Y,
Wang JJ, Tang CS, Kang YM and Zhu GQ: Intermedin in paraventricular
nucleus attenuates sympathetic activity and blood pressure via
nitric oxide in hypertensive rats. Hypertension. 63:330–337. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Zhang NB, Huang ZG, Cui WD and Ding BP:
Effects of puerarin on expression of cardiac Smad3 and Smad7 mRNA
in spontaneously hypertensive rat. J Ethnopharmacol. 138:737–740.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ghazi-Khansari M, Mohammadi-Karakani A,
Sotoudeh M, Mokhtary P, Pour-Esmaeil E and Maghsoud S: Antifibrotic
effect of captopril and enalapril on paraquat-induced lung fibrosis
in rats. J Appl Toxicol. 27:342–349. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Wu JB, Zhou Y, Liang CL, Zhang XJ, Lai JM,
Ye SF, Ouyang H, Lin J and Zhou JY: Cyclovirobuxinum D alleviates
cardiac hypertrophy in hyperthyroid rats by preventing apoptosis of
cardiac cells and inhibiting the p38 mitogen-activated protein
kinase signaling pathway. Chin J Integr Med. Mar 17–2016.(Epub
ahead of print).
|
|
26
|
Chen WW, Sun HJ, Zhang F, Zhou YB, Xiong
XQ, Wang JJ and Zhu GQ: Salusin-β in paraventricular nucleus
increases blood pressure and sympathetic outflow via vasopressin in
hypertensive rats. Cardiovasc Res. 98:344–351. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Wang C, Liu X, Tang Y, Peng H, Ye Z, Zhang
J, Tang H and Lou T: Medium from mesangial cells incubated with
aggregated IgA1 from IgA nephropathy patients reduces podocyte
adhesion through activation of the renin angiotensin system. Swiss
Med Wkly. 141:w133042011.PubMed/NCBI
|
|
28
|
Takai S, Jin D, Chen H, Li W, Yamamoto H,
Yamanishi K, Miyazaki M, Higashino H, Yamanishi H and Okamura H:
Chymase inhibition improves vascular dysfunction and survival in
stroke-prone spontaneously hypertensive rats. J Hypertens.
32:1637–1649. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Sun HJ, Liu TY, Zhang F, Xiong XQ, Wang
JJ, Chen Q, Li YH, Kang YM, Zhou YB, Han Y, et al: Salusin-β
contributes to vascular remodeling associated with hypertension via
promoting vascular smooth muscle cell proliferation and vascular
fibrosis. Biochim Biophys Acta. 1852:1709–1718. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Sun HJ, Zhao MX, Ren XS, Liu TY, Chen Q,
Li YH, Kang YM, Wang JJ and Zhu GQ: Salusin-β promotes vascular
smooth muscle cell migration and intimal hyperplasia after vascular
injury via ROS/NFκB/MMP-9 pathway. Antioxid Redox Signal.
24:1045–1057. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Kim MJ, Ryu JC, Kwon Y, Lee S, Bae YS,
Yoon JH and Ryu JH: Dual oxidase 2 in lung epithelia is essential
for hyperoxia-induced acute lung injury in mice. Antioxid Redox
Signal. 21:1803–1818. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Sun HJ, Chen D, Han Y, Zhou YB, Wang JJ,
Chen Q, Li YH, Gao XY, Kang YM and Zhu GQ: Relaxin in
paraventricular nucleus contributes to sympathetic overdrive and
hypertension via PI3K-Akt pathway. Neuropharmacology. 103:247–256.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Cuevas CA, Tapia-Rojas C, Cespedes C,
Inestrosa NC and Vio CP: β-Catenin-dependent signaling pathway
contributes to renal fibrosis in hypertensive rats. Biomed Res Int.
2015:7260122015. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Wang Z, Zhu Q, Li PL, Dhaduk R, Zhang F,
Gehr TW and Li N: Silencing of hypoxia-inducible factor-1α gene
attenuates chronic ischemic renal injury in two-kidney, one-clip
rats. Am J Physiol Renal Physiol. 306:F1236–F1242. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Cavallari LH, Fashingbauer LA, Camp JR,
King ST and Geenen DL: Hypertension-induced renal fibrosis and
spironolactone response vary by rat strain and mineralocorticoid
receptor gene expression. J Renin Angiotensin Aldosterone Syst.
9:146–153. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Go AS, Chertow GM, Fan D, McCulloch CE and
Hsu CY: Chronic kidney disease and the risks of death,
cardiovascular events, and hospitalization. N Engl J Med.
351:1296–1305. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Whitman IR, Feldman HI and Deo R: CKD and
sudden cardiac death: Epidemiology, mechanisms, and therapeutic
approaches. J Am Soc Nephrol. 23:1929–1939. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Muntner P, Anderson A, Charleston J, Chen
Z, Ford V, Makos G, O'Connor A, Perumal K, Rahman M, Steigerwalt S,
et al: Hypertension awareness, treatment, and control in adults
with CKD: Results from the chronic renal insufficiency cohort
(CRIC) Study. Am J Kidney Dis. 55:441–451. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Piret SE, Olinger E, Reed AA, Nesbit MA,
Hough TA, Bentley L, Devuyst O, Cox RD and Thakker RV: Mouse model
for inherited renal fibrosis associated with endoplasmic reticulum
stress. Dis Model Mech. 10:773–786. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Park JK, Theuer S, Kirsch T, Lindschau C,
Klinge U, Heuser A, Plehm R, Todiras M, Carmeliet P, Haller H, et
al: Growth arrest specific protein 6 participates in DOCA-induced
target-organ damage. Hypertension. 54:359–364. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Campagnaro BP, Tonini CL, Doche LM,
Nogueira BV, Vasquez EC and Meyrelles SS: Renovascular hypertension
leads to DNA damage and apoptosis in bone marrow cells. DNA Cell
Biol. 32:458–466. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Li P, Huang PP, Yang Y, Liu C, Lu Y, Wang
F, Sun W and Kong XQ: Renal sympathetic denervation attenuates
hypertension and vascular remodeling in renovascular hypertensive
rats. J Appl Physiol (1985). 122:121–129. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Shi Y, Lo CS, Padda R, Abdo S, Chenier I,
Filep JG, Ingelfinger JR, Zhang SL and Chan JS: Angiotensin-(1–7)
prevents systemic hypertension, attenuates oxidative stress and
tubulointerstitial fibrosis, and normalizes renal
angiotensin-converting enzyme 2 and Mas receptor expression in
diabetic mice. Clin Sci (Lond). 128:649–663. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Cowley AW Jr: Renal medullary oxidative
stress, pressure-natriuresis, and hypertension. Hypertension.
52:777–786. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Araujo M and Wilcox CS: Oxidative stress
in hypertension: Role of the kidney. Antioxid Redox Signal.
20:74–101. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Manning RD Jr, Tian N and Meng S:
Oxidative stress and antioxidant treatment in hypertension and the
associated renal damage. Am J Nephrol. 25:311–317. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Daehn I, Casalena G, Zhang T, Shi S,
Fenninger F, Barasch N, Yu L, D'Agati V, Schlondorff D, Kriz W, et
al: Endothelial mitochondrial oxidative stress determines podocyte
depletion in segmental glomerulosclerosis. J Clin Invest.
124:1608–1621. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Eddy AA: Molecular basis of renal
fibrosis. Pediatr Nephrol. 15:290–301. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Lassegue B, San Martin A and Griendling
KK: Biochemistry, physiology, and pathophysiology of NADPH oxidases
in the cardiovascular system. Circ Res. 110:1364–1390. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Taylor NE, Glocka P, Liang M and Cowley AW
Jr: NADPH oxidase in the renal medulla causes oxidative stress and
contributes to salt-sensitive hypertension in Dahl S rats.
Hypertension. 47:692–698. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Cowley AW Jr, Yang C, Zheleznova NN,
Staruschenko A, Kurth T, Rein L, Kumar V, Sadovnikov K, Dayton A,
Hoffman M, et al: Evidence of the importance of Nox4 in production
of hypertension in Dahl salt-sensitive rats. Hypertension.
67:440–450. 2016.PubMed/NCBI
|
|
52
|
Wu N, Shen H, Liu H, Wang Y, Bai Y and Han
P: Acute blood glucose fluctuation enhances rat aorta endothelial
cell apoptosis, oxidative stress and pro-inflammatory cytokine
expression in vivo. Cardiovasc Diabetol. 15:1092016. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Ruiz S, Pergola PE, Zager RA and Vaziri
ND: Targeting the transcription factor Nrf2 to ameliorate oxidative
stress and inflammation in chronic kidney disease. Kidney Int.
83:1029–1041. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Meguid El Nahas A and Bello AK: Chronic
kidney disease: The global challenge. Lancet. 365:331–340. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Hartner A, Klanke B, Cordasic N, Amann K,
Schmieder RE, Veelken R and Hilgers KF: Statin treatment reduces
glomerular inflammation and podocyte damage in rat
deoxycorticosterone-acetate-salt hypertension. J Hypertens.
27:376–385. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Zhang J, Patel MB, Griffiths R, Mao A,
Song YS, Karlovich NS, Sparks MA, Jin H, Wu M, Lin EE and Crowley
SD: Tumor necrosis factor-α produced in the kidney contributes to
angiotensin II-dependent hypertension. Hypertension. 64:1275–1281.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Rincón J, Correia D, Arcaya JL, Finol E,
Fernández A, Pérez M, Yaguas K, Talavera E, Chávez M, Summer R and
Romero F: Role of Angiotensin II type 1 receptor on renal NAD(P)H
oxidase, oxidative stress and inflammation in nitric oxide
inhibition induced-hypertension. Life Sci. 124:81–90. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Zhou L, Mo H, Miao J, Zhou D, Tan RJ, Hou
FF and Liu Y: Klotho ameliorates kidney injury and fibrosis and
normalizes blood pressure by targeting the renin-angiotensin
system. Am J Pathol. 185:3211–3223. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Crowley SD, Gurley SB, Herrera MJ, Ruiz P,
Griffiths R, Kumar AP, Kim HS, Smithies O, Le TH and Coffman TM:
Angiotensin II causes hypertension and cardiac hypertrophy through
its receptors in the kidney. Proc Natl Acad Sci USA. 103:pp.
17985–17990. 2006; View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Ruggenenti P, Cravedi P and Remuzzi G:
Mechanisms and treatment of CKD. J Am Soc Nephrol. 23:1917–1928.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Zhang JS, Zhang YL, Wang HX, Xia YL, Wang
L, Jiang YN, Li HH and Liu Y: Identification of genes related to
the early stage of Angiotensin II-induced acute renal injury by
microarray and integrated gene network analysis. Cell Physiol
Biochem. 34:1137–1151. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Kuriyama S: The relation between green tea
consumption and cardiovascular disease as evidenced by
epidemiological studies. J Nutr. 138:1548S–1553S. 2008.PubMed/NCBI
|
|
63
|
Israili ZH and Hall WD: Cough and
angioneurotic edema associated with angiotensin-converting enzyme
inhibitor therapy. A review of the literature and pathophysiology.
Ann Intern Med. 117:234–242. 1992. View Article : Google Scholar : PubMed/NCBI
|