Introduction
Oral mucosal lesions, facial trauma and management
of tumors of the oral cavity often cause oral mucosal defects.
Repair of the oral mucosa requires tissue engineering or
transplantation as large defects cannot be directly sutured
(1). Split-thickness skin grafts are
considered the ‘gold standard’ for the treatment of skin wounds
(2). However, the small size of
donor oral tissue, limited graft survival due to the full thickness
nature of mucosal grafts and contracture/scarring at the donor site
have all limited the use of mucosal grafts for the treatment of
oral wounds (3). In addition, due to
the differences between skin and oral mucosa, the transplanted skin
grafts are poorly assimilated even years after transplantation
(4). Different approaches to the
reconstruction of oral mucosa have been employed in attempts to
find a solution to this issue. These include oral epithelial cell
sheets, guided tissue replacement and vestibuloplasty (5). However, identifying an acceptable
source for transplantations or autologous grafts is challenging
(6).
Acellular dermal matrix (ADM), processed from
allogeneic human skin, has been proposed as an alternative approach
for the treatment of oral mucosal wounds (7). Following removal of the
keratin-containing epidermis, the dermal layer is processed to
remove all DNA without disrupting the collagen matrix. This
preparation allows for host cell infiltration, neovascularization
and epithelialization without rejection (8). Rhee et al (9) used commercially available ADM as a
substitute for autologous, split-thickness skin grafts for the
resurfacing of intraoral defects in 29 patients. The overall
success rate was 90%, with complete epithelialization within 4
weeks noted during clinical evaluation. The clinical application of
ADM has yielded promising results and high success rates. However,
the changes in histopathology and molecular biology that occur
during the epithelialization process following transplantation into
the oral cavity remain unclear. To the best of our knowledge, few
studies have investigated the functional properties of ADM in oral
mucosal repair in animal models. Thus, the present study was
designed to assess the repair of oral mucosal defects in rabbits
over time using ADM and to investigate the potential biological
mechanisms underlying its efficacy in order to further support and
inform the use of this strategy in clinical settings.
Materials and methods
Animals
In total, 30 healthy adult (25–28 weeks) male New
Zealand white rabbits weighing 4.0–4.5 kg were used in the present
study (Peking University Laboratory Animal Center, Beijing, China).
All rabbits were acclimated in the experimental animal laboratory
of Peking University Hospital of Stomatology for 1 week prior to
the experiment. Rabbits were maintained on a 14 h light/8 h dark
cycle at 23±2°C and 60–70% air humidity with free access to food
and water. Experimental procedures were performed in accordance
with the Guidelines for Animal Experimentation of Peking University
with the approval of the Animal Care and Use Committee at Peking
University School and Hospital of Stomatology.
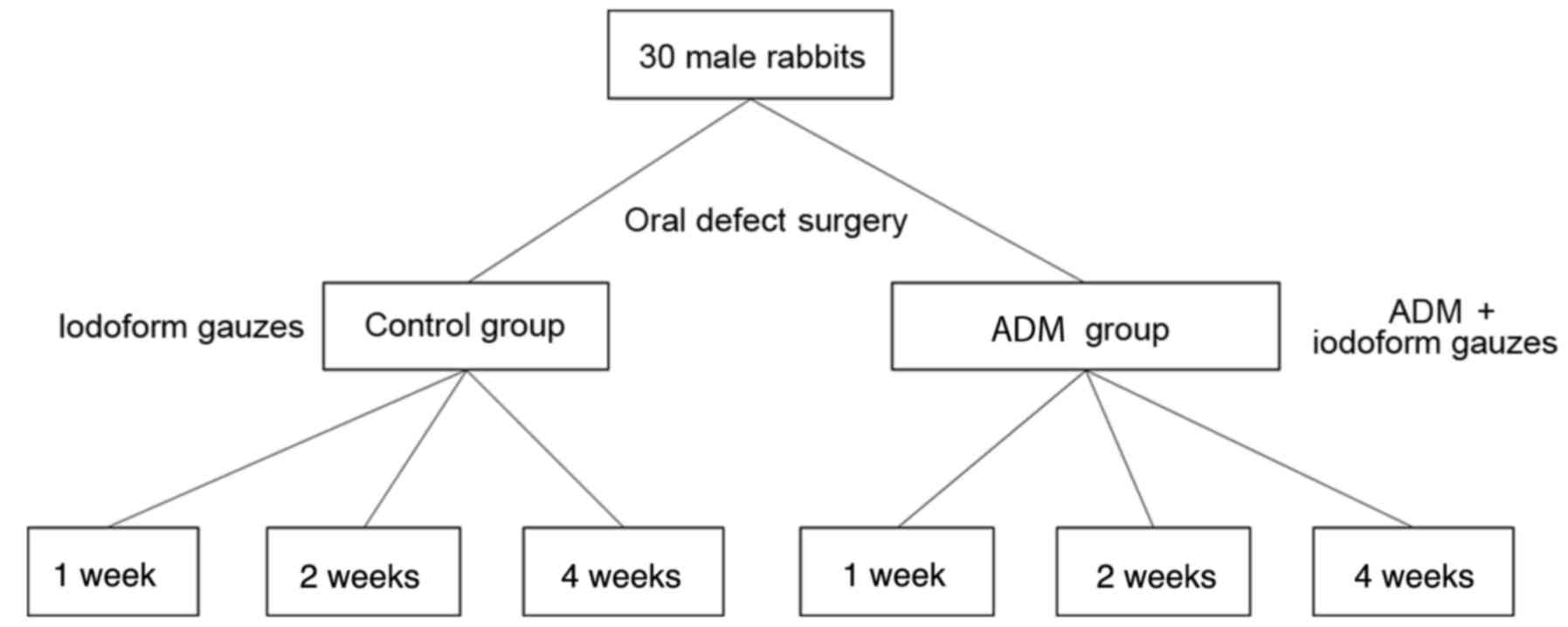
Study design
Animals were assigned to one of two groups. The
rabbits in the ADM group (n=15) underwent oral mucosal defect
surgery and were treated with an ADM covering and iodoform gauze.
The rabbits in the control group (n=15) were treated with only
iodoform gauze following oral mucosal defect surgery. At 1, 2, and
4 weeks after the surgery, 5 animals per group were sacrificed in
order to perform histological investigations. The study design is
presented in Fig. 1.
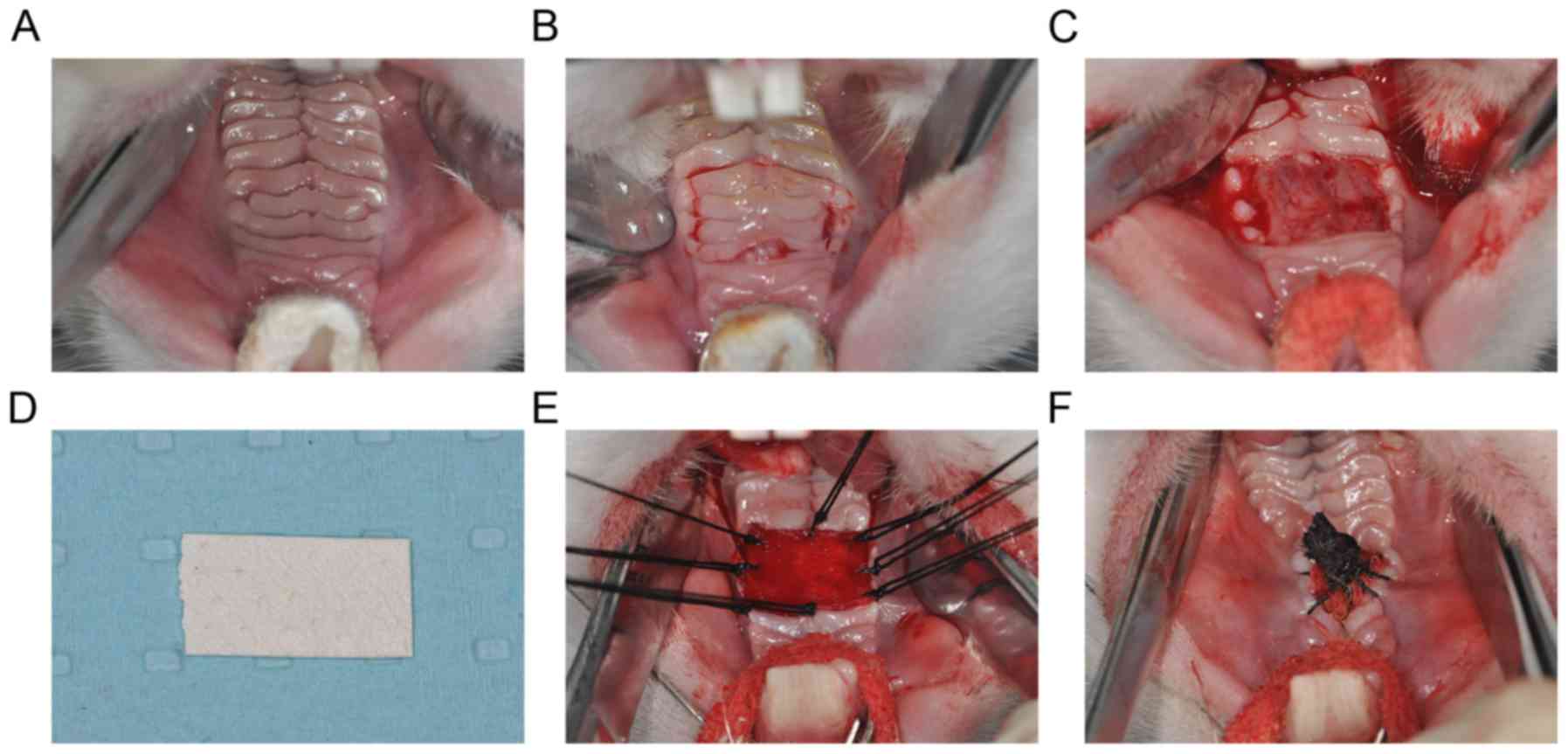
Surgical procedures
Rabbits were anesthetized with intravenous
pentobarbital sodium (30 mg/kg). Following disinfection with 1%
iodine tincture and local anesthesia with 1% lidocaine, the palate
was fully exposed (Fig. 2A). Palatal
mucosa was carefully separated from the underlying submucosa
backwards from the fourth palatal rugae and was then excised,
ensuring that the bilateral incision did not exceed the outer
boundary of the palatal mucosa. The deficient area was ~1×1
cm2 (Fig. 2B). Adequate
hemostasis was then ensured in the mucosa-deficient region
(Fig. 2C). Subsequently, for the ADM
group, ADM (1×1 cm; Beijing Jayyalife Biological Technology Co.,
Ltd., Beijing, China) was hydrated with two saline washes according
to the manufacturer's protocol (Fig.
2D) and was then cut to the same size as the wound surface. The
ADM was then embedded in the defect region and attached as a
covering tissue with a simple interrupted suture with 3-0 stitches
(Fig. 2E). Wounds were then covered
with iodoform gauze and wrapped together with ADM (Fig. 2F). In the control group, the wound
surface was covered with iodoform gauze only. Surgery was performed
under sterile conditions. Following surgery, all rabbits were
fasted and deprived of water for 12 h and then provided only soft
food for 1 week. Following removal of the iodoform gauze under
intravenous anesthesia with 30 mg/kg 3% pentobarbital sodium via
the ear vein, rabbits were returned to a diet of normal pellets and
water.
Histological procedures
All rabbits were sacrificed with an overdose of
pentobarbital sodium (>120 mg/kg) through the ear vein. The
front jaw was removed and the soft tissue of the palate, together
with the corresponding deep bone tissue were immediately collected
and fixed in 10% buffered formalin for 2 days at room temperature.
The periosteum of the palate was then bluntly separated and the
wound region was obtained, together with 2-3 cm of normal palatal
mucosa around the operative region. Following routine procedures,
tissues were embedded in paraffin and 10-µm sections were prepared
for histological evaluation. Hematoxylin and eosin (H&E)
staining was performed according to a previously published protocol
(10) to evaluate the morphology of
the palate mucosa under a light microscope.
Reverse transcription-quantitative
polymerase chain reaction (RT-qPCR)
Total RNA was extracted from tissue sections that
had been stored in liquid nitrogen using TRIzol reagent
(Invitrogen; Thermo Fisher Scientific, Inc., Waltham, MA, USA)
according to the manufacturer's protocol. cDNA was then synthesized
and quantified using the PrimeScript RT reagent kit (Takara
Biotechnology Co., Ltd., Dalian, China) on an ABI 7300 System
(Applied Biosystems; Thermo Fisher Scientific, Inc.). The reaction
was performed at 16°C for 30 min; 42°C for 30 min and 85°C for 5
min. qPCR was carried out using a Power SYBR Green PCR master mix
(Applied Biosystems; Thermo Fisher Scientific, Inc.). Primers
sequences were as follows: GLUT1, forward,
5′-CAGTTCGGCTATAACACTGGTG-3′ and reverse,
5′-GCCCCCGACAGAGAAGATG-3′; VEGF, forward,
5′-TGCCCACTGAGGAGTCCAAC-3′ and reverse, 5′-TGGTTCCCGAAACGCTGAG-3′
(Guangzhou RiboBio Co., Ltd., Guangzhou, China); and GAPDH,
forward, 5′-GCACCGTCAAGGCTGAGAAC-3′ and reverse,
5′-ATGGTGGTGAAGACGCCAGT-3′. PCR reactions were performed using the
following conditions: 94°C for 1 min followed by 40 cycles of 94°C
for 30 sec, 60°C for 60 sec and 72°C for 15 sec. Amplification of
the target genes was normalized to GAPDH. All reactions were
performed in triplicate. The 2−ΔΔCq method (11) was used to determine the relative
expression of VEGF and GLUT1.
Western blot analysis
Total protein was extracted from the epithelium of
the wound tissue using PRO-PREP (Intron Biotechnology, Inc.,
Seongnam, Korea), according to the manufacturer's protocol and the
BCA protein determination method was used. Equal amounts of protein
(30 µg per lane) were separated by 12% SDS-PAGE, transferred onto
PVDF membranes (EMD Millipore, Billerica, MA, USA) and blocked with
10% bovine serum albumin (Sigma-Aldrich; Merck KGaA, Darmstadt,
Germany) at room temperature for 2 h. Membranes were then incubated
with antibodies specific to GLUT1 (1:1,000; cat no. NB110-39113;
Novus Biologicals Canada ULC, Oakville, ON, Canada), vascular
endothelial growth factor (VEGF) (1:500; cat no. MAB293R; R&D
Systems, Inc., Minneapolis, MN, USA) and GAPDH (1:2,000; cat no.
GTX100118; GeneTex, Inc., Irvine, CA, USA) overnight at 4°C,
followed by incubation with anti-rabbit Immunoglobulin G
horseradish peroxidase-conjugated antibodies (1:5,000; cat no.
7071; Cell Signaling Technology, Inc., Danvers, MA, USA) for 2 h at
room temperature. Immunoreactive bands were detected using an ECL
detection system (cat no. 6883, Cell Signaling Technology, Inc.)
and analyzed with Quantity One 4.0 software (Bio-Rad Laboratories,
Inc., Hercules, CA, USA).
Statistical analysis
Data are expressed as mean ± standard deviation.
Group comparisons were calculated using SPSS 19.0 software (IBM
Corp., Armonk, NY, USA) and unpaired, two-tailed Student's t-tests.
P<0.05 was considered to indicate a statistically significant
difference.
Results
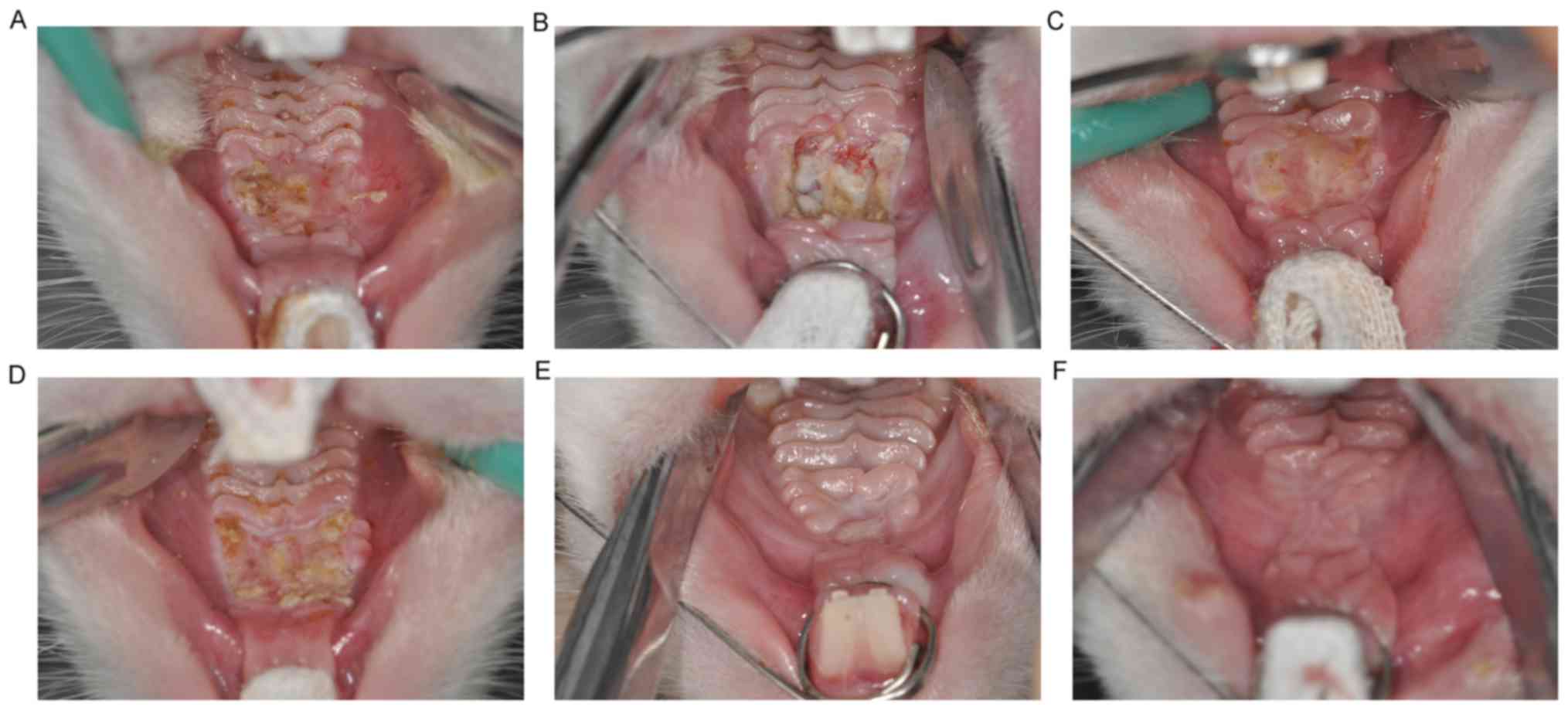
Clinical observation
No hematomas or inflammation were observed in
rabbits following surgery. At 1 week following surgery, superficial
ulcers and some necrotic tissue were observed in the operative site
of animals in the ADM group. The boundaries between the operative
region and normal mucosal were unclear, and granulation tissue
continuous with the connective tissue of the oral mucosa was
observed (Fig. 3A). By comparison,
rabbits in the control group displayed deeper ulcers and more
necrotic tissue, with new granulation tissue filling the surgical
wounds (Fig. 3B). At 2 weeks
following surgery, the ulcers were significantly reduced in the ADM
group and the mucosa had begun to form with a tenacious texture.
However, the palatal rugae remained unclear (Fig. 3C). By contrast, despite the
boundaries between the operative region and normal mucosal tissue
becoming less clearly defined, ulcers remained relatively large and
dispersed necrotic tissue remained present in the control group
(Fig. 3D). At 4 weeks following
surgery, all animals from the ADM and control groups had recovered
and palatal rugae were resurgent, with no ulcers or necrosis in the
operative area (Fig. 3E and F).
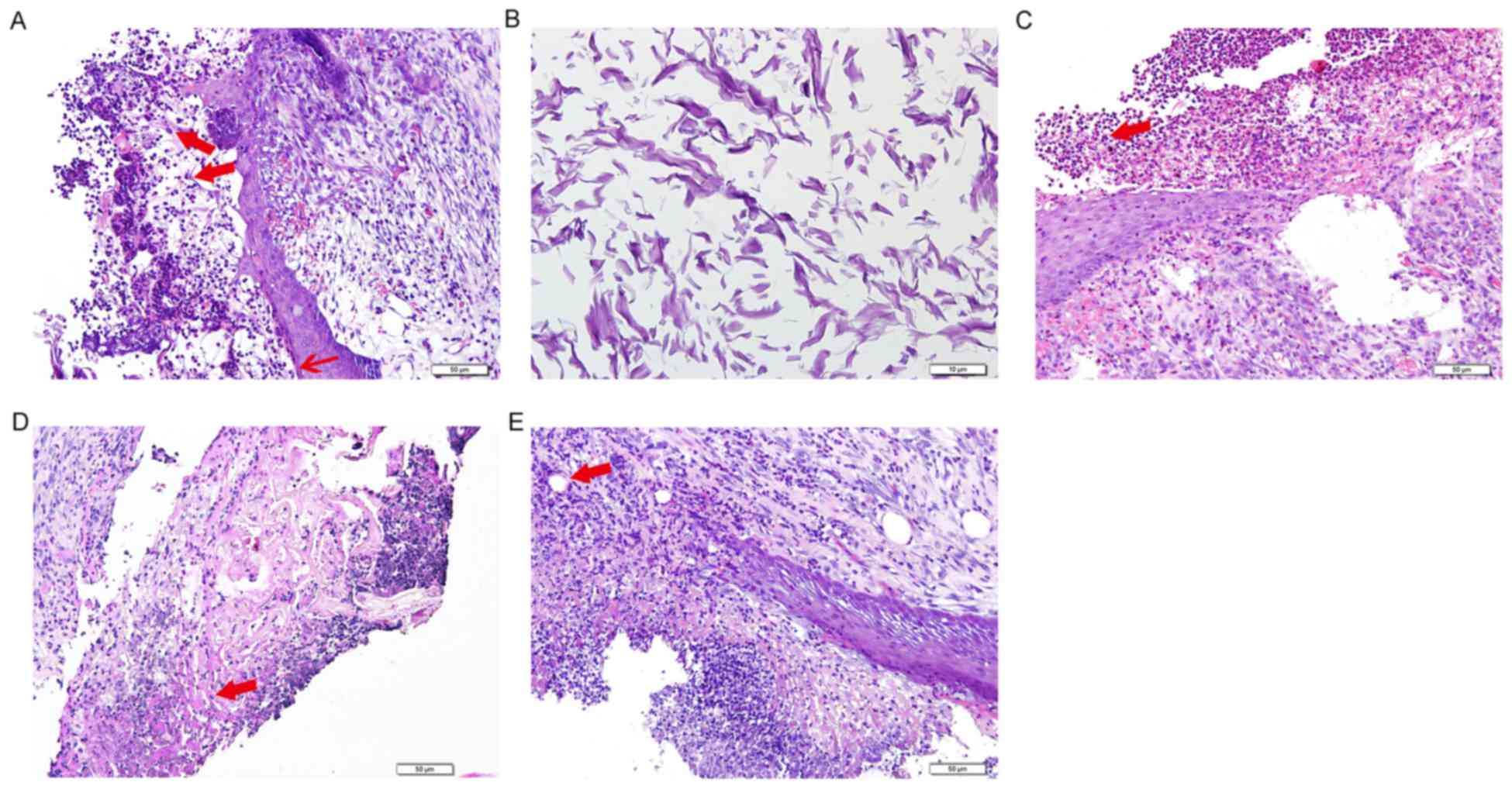
Histopathological analysis
At 1 week following surgery in the ADM group,
H&E staining indicated a moderate degree of cellulose-like
exudation on the surface of epithelial defects, suggesting that
epithelialization was incomplete. In addition, the ADM collagen was
filled with a large number of inflammatory and endothelial cells.
Collagen fibers were arranged in fascicular clusters in the lower
layer of the oral mucosa and the defect border had regularly
arranged, neonatal epithelial tissue growing into the inflammatory
site (Fig. 4A and B). Inflammatory
cells were predominantly lymphocytes and granulocytes, with a lower
proportion of macrophages. Early revascularization of the dermal
equivalent was noted. However, in the control group, a larger
amount of cellulose-like exudate was observed and the submucosa had
fewer collagen fibers, which were randomly oriented (Fig. 4C). There was also an increased number
of inflammatory cells compared with the ADM group.
Epithelialization of the sutured wound progressed in the ADM group
2 weeks following surgery (Fig. 4D).
However, keratinization was not complete and epithelial ridges were
not present. Fibroblasts with large nuclei remained present in the
submucosa, as well as a small number of inflammatory cells. Some
vascularization was observed at the ADM graft sites. Histopathology
of the wound area in the control group 2 weeks following surgery
was comparable to that seen in the ADM group 1 week following
surgery (Fig. 4E). Cellulose-like
exudate was present on the surface of the wound area and acute
inflammatory cells that had infiltrated the collagen fibers were
present in the submucosa. Minimal vascularization was noted at the
margin of the defects. At 4 weeks following surgery, the defects
were covered by well-organized, stratified squamous epithelium, and
appeared similar to the normal surrounding mucosa in the control
and ADM groups (data not shown).
Molecular biological
investigation
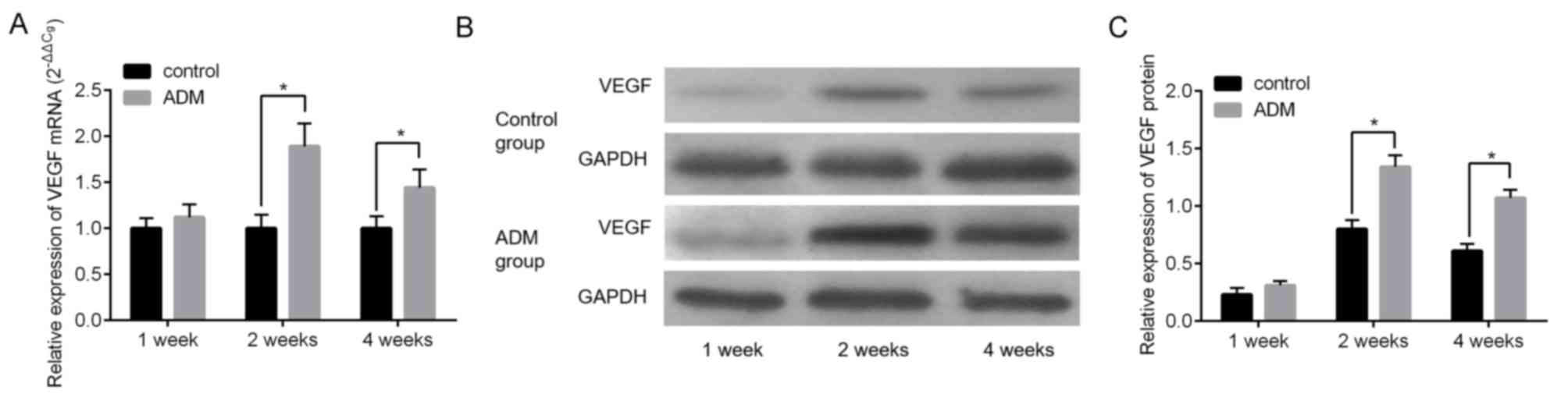
The molecular biological alterations occurring
during wound healing following the treatment with ADM were
investigated. The difference in the expression of vascular
endothelial growth factor (VEGF), which is a well-known angiogenic
factor that is important for vascular development and maintenance
during wound healing, between the control and ADM groups at 1 week
post-surgery was not significant at mRNA and protein levels
(Fig. 5A-C). However, the expression
of VEGF was significantly increased in the ADM group compared with
the control group at 2 and 4 weeks following surgery (Fig. 5A-C, P<0.05).
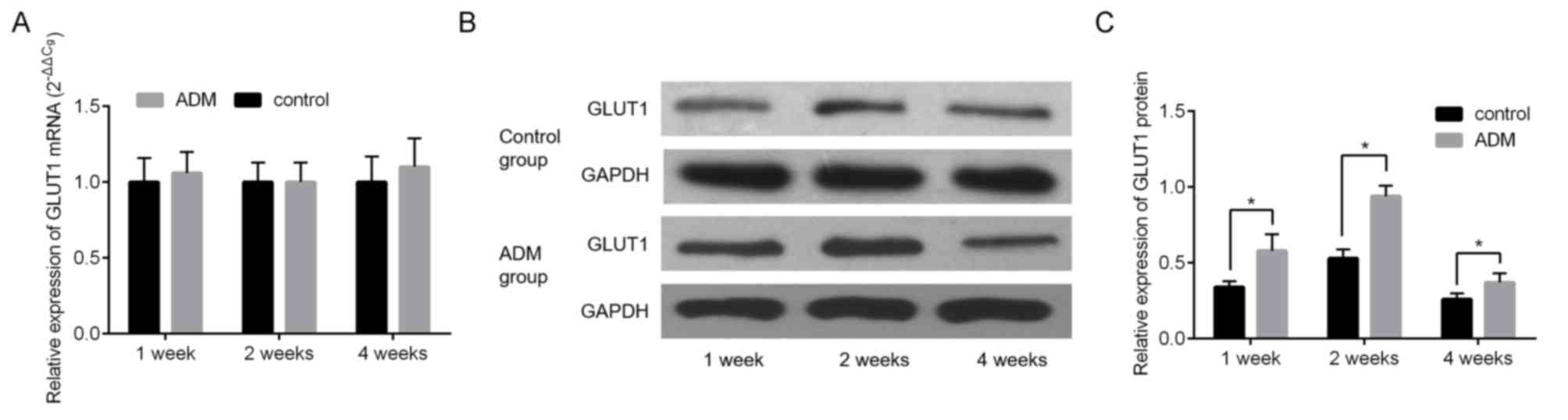
The expression of GLUT1 was measured using RT-qPCR
and western blotting. The difference in the expression of GLUT1
mRNA between the control and ADM groups was not significant at all
time points (Fig. 6A). However,
GLUT1 protein expression was significantly increased in the ADM
group compared with the control group at all time points (all
P<0.05, Fig. 6B and C).
Discussion
Wainwright (12) was
the first to illustrate the use of an ADM processed from allogeneic
human skin for the treatment of a full-thickness burn injury and
since then a variety of reconstructive procedures utilizing ADM
have emerged. These include supporting lymphangiogenesis (13), abdominal wall reconstructions
(14) and postmastectomy
reconstruction (15,16). In the reconstruction of ridge
deformities following tooth extraction in humans, ADM was novelly
employed as a membrane associated with resorbable hydroxyapatite
for bone regeneration, resulting in the preservation of ridge
thickness and an increase in the width of keratinized tissue
(17). When associated with an
organic bovine bone matrix and P-15, a synthetic compound
containing 15 amino acids of collagen type I, ADM exhibited the
effective preservation of the alveolar ridge following the
extraction of anterior maxillary teeth (18).
Regarding the use of ADM in oral cavity
reconstruction, Izumi et al (19) developed a human oral mucosa
equivalent that was produced ex vivo in a serum-free culture
system without a feeder layer. It comprised a stratified layer of
autogeneous human oral keratinocytes seeded on top of ADM and was
demonstrated to promote wound healing more favorably than AlloDerm
alone for human intraoral grafting procedures. In addition, Girod
et al (7) compared the
efficacy of ADM and split thickness skin grafts in oral cavity
reconstruction and concluded that the use of ADM had several
advantages over split thickness skin grafts. These included a lack
of donor site morbidity, a natural-appearing mucosal surface and
lower surgical fees. However, to the best of our knowledge, few
studies have been performed in animals to observe the dynamic
progress of tissue growth or investigate alterations in molecular
biology during reconstruction of intraoral defects over time.
In the present study, observation of the gross
appearance between the ADM and control groups indicated that ADM
improved the healing rate of oral mucosal wounds and shortened the
recovery time while inducing only a low inflammatory response
compared with the tissue reaction in an untreated wound. These
results are consistent with a previous clinical study (19). Notably, the histological analysis
executed by Xiong et al (20)
on a palatal mucosa equivalent consisting of cultured oral
keratinocytes and porcine ADM indicated that keratinocytes
infiltrated the empty spaces of the porcine ADM and formed an
anchor-like structure, resembling the rete ridges of the native
palate mucosa. Thus, it was hypothesized in the current study that
ADM serves as a cellular scaffold in oral mucosal defect recovery
and guides tissue regeneration. However, the pathological
regression of ADM used in surgery, including absorption,
degradation or incorporation as an autologous structure into the
palate, remains unclear. In a previous study conducted by Ophof
et al (21), it was also
unclear whether ADM was rapidly degraded or sequestrated. A low
level of phagocytic cells was observed in the ADM group compared
with the control group, indicating minimal rejection, which may be
due to the histocompatibility of ADM (22). Therefore, the likelihood of
absorption and degradation of the ADM was decreased. No clear
differences were identified between the two groups in gross
appearance and pathological features at 4 weeks following surgery,
suggesting that ADM had no notable short-term side effects on
recovery.
It has previously been demonstrated that ADM may be
used as an interpositional connective tissue graft for the repair
of mucosal defects (23). Therefore,
in the current study, histology was used to investigate the dynamic
tissue response of the palatal mucosa. More specifically, the
infiltration of inflammatory cells, epithelialization,
revascularization and collagen orientation were assessed. Luczyszyn
et al (24) and Izumi et
al (19) demonstrated similar
results by examining the repair of mucosal defects treated with
ADM. In the current study, prominent epithelialization and
transformation were observed in the ADM group when assessed at week
2 following surgery. In addition, a decreased inflammatory reaction
was observed compared with the control group, which was marked by a
small number of inflammatory cells and well-organized tissue in the
ADM group. Inflammation is always accompanied by remodeling of the
extracellular matrices in this mucosa equivalent, which is
essential for the formation of granulation tissue (25). Foldable tissues possess a high
capacity for epithelialization in order to preserve local anatomy
as well as chewing, phonation and deglutition (26). It has been previously demonstrated
that the collagen fibers in a healing wound run in the direction of
the contraction forces (27). In the
current study, the collagen fibers in the tissue of the control
group were more randomly oriented compared with those in the ADM
group and the wounds treated with ADM exhibited fewer fibroblasts
compared with untreated wounds. Revascularization during the
recovery progress is necessary for wound healing (28). In the current study, rapid
revascularization was observed in ADM-treated defects within 1 week
and a wide range of vascularization was present by 2 weeks
following surgery. These results are consistent with results
presented by Takami et al (29). The mechanisms underlying the faster
revascularization observed with ADM grafts compared with untreated
wounds was further explored in the current study. It has previous
been demonstrated that VEGF is highly expressed by epidermal
keratinocytes and is overexpressed during wound healing (30). In the current study, the expression
of VEGF during oral mucosal repair with or without ADM treatment
was evaluated. We indicated that there was a higher expression of
VEGF in the ADM-treated group compared with the control at 2 and 4
weeks following surgery, suggesting that VEGF secreted by an ADM
graft may assist vascularization following grafting, which is
critical to subsequent graft survival (31). These results provide an explanation
for the rapid revascularization present in the ADM-treated group in
the present study.
During wound healing, proliferative cell activity is
another key component required for the promotion of
epithelialization. High GLUT1 expression has previously been
reported in the wound margin, with re-epithelialization
demonstrated to occur in GLUT1 positive sites (32). This suggests that GLUT1 expression is
an indicator of proliferative cell activity during wound healing.
It was thus hypothesized that GLUT1 levels are enhanced following
wounding, which serves a critical role in the healing of oral
wounds. In the current study, it was observed that GLUT1 protein
was highly expressed in ADM grafts compared with untreated wounds.
However, the use of ADM had no effect on the expression of GLUT1
mRNA. GLUT1 is a membrane protein and member of the glucose
transporter family, which acts as a carrier for glucose uptake into
cells (33). Kuroki et al
(34) identified that GLUT1
expression was present throughout all epithelial cell layers in the
oral mucosa and was decreased in parallel with the differentiation
gradient. Activation of GLUT1 requires an increased level of
glucose (35). The cellular scaffold
role of ADM may reduce the consumption of energy so that the
cellular level of glucose increases. Under these circumstances,
GLUT1 protein levels would subsequently be increased. Therefore,
the current study provides cytobiological evidence to indicate that
ADM promotes epithelialization and revascularization during wound
healing without rejection.
However, the current study had the following
limitations: It was performed on individual animals and individual
heterogeneity was not considered; the only histological analyses
performed used H&E staining, while the use of more specific
stains may have contributed additional information. Furthermore,
immunohistochemical analyses to explore the distribution of VEGF
and GLUT1 should be performed in future studies.
In conclusion, in comparison with untreated wounds,
it appears that palatal wounds treated with ADM stimulate a mild
inflammatory response, exhibit rapid epithelialization and
revascularization and are accompanied by an increase in VEGF and
GLUT1, all leading to the promotion of tissue growth in defect
sites. The effects on molecular biology and the histological
process of repair for defects of the oral mucosa that have been
treated with ADM were elucidated. The results provide evidence
supporting the clinical use of ADM, which may lead to improvements
in intraoral mucosal repair in humans in the future.
Glossary
Abbreviations
Abbreviations:
|
ADM
|
acellular dermal matrix
|
|
VEGF
|
vascular endothelial growth factor
|
|
GLUT1
|
glucose transporter 1
|
References
|
1
|
Kinikoglu B, Damour O and Hasirci V:
Tissue engineering of oral mucosa: A shared concept with skin. J
Artif Organs. 18:8–19. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
MacNeil S: Progress and opportunities for
tissue-engineered skin. Nature. 445:874–880. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ueda M, Tohnai I and Nakai H: Tissue
engineering research in oral implant surgery. Artif Organs.
25:164–171. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Liu J, Bian Z, Kuijpers-Jagtman AM and Von
den Hoff JW: Skin and oral mucosa equivalents: Construction and
performance. Orthod Craniofac Res. 13:11–20. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mohd Nor NH, Berahim Z, Ahmad A and Kannan
TP: Properties of cell sources in tissue-engineered
three-dimensional oral mucosa model: A review. Curr Stem Cell Res
Ther. 12:52–60. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Berthiaume F, Maguire TJ and Yarmush ML:
Tissue engineering and regenerative medicine: History, progress,
and challenges. Annu Rev Chem Biomol Eng. 2:403–430. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Girod DA, Sykes K, Jorgensen J, Tawfik O
and Tsue T: Acellular dermis compared to skin grafts in oral cavity
reconstruction. Laryngoscope. 119:2141–2149. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Livesey SA, Herndon DN, Hollyoak MA,
Atkinson YH and Nag A: Transplanted acellular allograft dermal
matrix. Potential as a template for the reconstruction of viable
dermis. Transplantation. 60:1–9. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Rhee PH, Friedman CD, Ridge JA and Kusiak
J: The use of processed allograft dermal matrix for intraoral
resurfacing: An alternative to split-thickness skin grafts. Arch
Otolaryngol Head Neck Surg. 124:1201–1204. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Fischer AH, Jacobson KA, Rose J and Zeller
R: Hematoxylin and eosin staining of tissue and cell sections. CSH
Protoc. 2008:pdb.prot49862008.PubMed/NCBI
|
|
11
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wainwright DJ: Use of an acellular
allograft dermal matrix (AlloDerm) in the management of
full-thickness burns. Burns. 21:243–248. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wong AK, Schonmeyr B, Singh P, Carlson DL,
Li S and Mehrara BJ: Histologic analysis of angiogenesis and
lymphangiogenesis in acellular human dermis. Plast Reconstr Surg.
121:1144–1152. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Buinewicz B and Rosen B: Acellular
cadaveric dermis (AlloDerm): A new alternative for abdominal hernia
repair. Ann Plast Surg. 52:188–194. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Becker S, Saint-Cyr M, Wong C, Dauwe P,
Nagarkar P, Thornton JF and Peng Y: AlloDerm versus DermaMatrix in
immediate expander-based breast reconstruction: A preliminary
comparison of complication profiles and material compliance. Plast
Reconstr Surg. 123:1–6; discussion 107–108. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Adetayo OA, Salcedo SE, Bahjri K and Gupta
SC: A meta-analysis of outcomes using acellular dermal matrix in
breast and abdominal wall reconstructions: Event rates and risk
factors predictive of complications. Ann Plast Surg. 77:e31–e38.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Luczyszyn SM, Papalexiou V, Novaes AB Jr,
Grisi MF, Souza SL and Taba M Jr: Acellular dermal matrix and
hydroxyapatite in prevention of ridge deformities after tooth
extraction. Implant Dent. 14:176–184. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Fernandes PG, Novaes AB Jr, de Queiroz AC,
de Souza SL, Taba M Jr, Palioto DB and Grisi MF: Ridge preservation
with acellular dermal matrix and anorganic bone matrix cell-binding
peptide P-15 after tooth extraction in humans. J Periodontol.
82:72–79. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Izumi K, Feinberg SE, Iida A and Yoshizawa
M: Intraoral grafting of an ex vivo produced oral mucosa
equivalent: A preliminary report. Int J Oral Maxillofac Surg.
32:188–197. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Xiong X, Zhao Y, Zhang W, Xie W and He S:
In vitro engineering of a palatal mucosa equivalent with acellular
porcine dermal matrix. J Biomed Mater Res A. 86:544–551. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Ophof R, Maltha JC, Von den Hoff JW and
Kuijpers-Jagtman AM: Histologic evaluation of skin-derived and
collagen-based substrates implanted in palatal wounds. Wound Repair
Regen. 12:528–538. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Wainwright D, Madden M, Luterman A, Hunt
J, Monafo W, Heimbach D, Kagan R, Sittig K, Dimick A and Herndon D:
Clinical evaluation of an acellular allograft dermal matrix in
full-thickness burns. J Burn Care Rehabil. 17:124–136. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Kridel RW, Foda H and Lunde KC: Septal
perforation repair with acellular human dermal allograft. Arch
Otolaryngol Head Neck Surg. 124:73–78. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Luczyszyn SM, Grisi MF, Novaes AB Jr,
Palioto DB, Souza SL and Taba M Jr: Histologic analysis of the
acellular dermal matrix graft incorporation process: A pilot study
in dogs. Int J Periodontics Restorative Dent. 27:341–347.
2007.PubMed/NCBI
|
|
25
|
Yannas IV, Lee E, Orgill DP, Skrabut EM
and Murphy GF: Synthesis and characterization of a model
extracellular matrix that induces partial regeneration of adult
mammalian skin. Proc Natl Acad Sci USA. 86:pp. 933–937. 1989;
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Uğurlu K, Hüthüt I, Ozçelik D, Ozer K,
Sakiz D, Yildiz K and Baş L: Epithelialization process of free
fascial flaps used in reconstruction of oral cavity mucosa defects
in dogs. Plast Reconstr Surg. 113:915–926. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Wei PC, Laurell L, Lingen MW and Geivelis
M: Acellular dermal matrix allografts to achieve increased attached
gingiva. Part 2. A histological comparative study. J Periodontol.
73:257–265. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Chaplin JM, Costantino PD, Wolpoe ME,
Bederson JB, Griffey ES and Zhang WX: Use of an acellular dermal
allograft for dural replacement: An experimental study.
Neurosurgery. 45:320–327. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Takami Y, Matsuda T, Yoshitake M,
Hanumadass M and Walter RJ: Dispase/detergent treated dermal matrix
as a dermal substitute. Burns. 22:182–190. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Szpaderska AM, Walsh CG, Steinberg MJ and
DiPietro LA: Distinct patterns of angiogenesis in oral and skin
wounds. J Dent Res. 84:309–314. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Nakanishi Y, Izumi K, Yoshizawa M, Saito
C, Kawano Y and Maeda T: The expression and production of vascular
endothelial growth factor in oral mucosa equivalents. Int J Oral
Maxillofac Surg. 36:928–933. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Lenoir MC, Bernard BA, Pautrat G, Darmon M
and Shroot B: Outer root sheath cells of human hair follicle are
able to regenerate a fully differentiated epidermis in vitro. Dev
Biol. 130:610–620. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Takahashi H, Kaminski AE and Zieske JD:
Glucose transporter 1 expression is enhanced during corneal
epithelial wound repair. Exp Eye Res. 63:649–659. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Kuroki S, Yokoo S, Terashi H, Hasegawa M
and Komori T: Epithelialization in oral mucous wound healing in
terms of energy metabolism. Kobe J Med Sci. 55:E5–E15.
2009.PubMed/NCBI
|
|
35
|
Liemburg-Apers DC, Wagenaars JA, Smeitink
JA, Willems PH and Koopman WJ: Acute stimulation of glucose influx
upon mitoenergetic dysfunction requires LKB1, AMPK, Sirt2 and
mTOR-RAPTOR. J Cell Sci. 129:4411–4423. 2016. View Article : Google Scholar : PubMed/NCBI
|