|
1
|
Kinikoglu B, Damour O and Hasirci V:
Tissue engineering of oral mucosa: A shared concept with skin. J
Artif Organs. 18:8–19. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
MacNeil S: Progress and opportunities for
tissue-engineered skin. Nature. 445:874–880. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ueda M, Tohnai I and Nakai H: Tissue
engineering research in oral implant surgery. Artif Organs.
25:164–171. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Liu J, Bian Z, Kuijpers-Jagtman AM and Von
den Hoff JW: Skin and oral mucosa equivalents: Construction and
performance. Orthod Craniofac Res. 13:11–20. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mohd Nor NH, Berahim Z, Ahmad A and Kannan
TP: Properties of cell sources in tissue-engineered
three-dimensional oral mucosa model: A review. Curr Stem Cell Res
Ther. 12:52–60. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Berthiaume F, Maguire TJ and Yarmush ML:
Tissue engineering and regenerative medicine: History, progress,
and challenges. Annu Rev Chem Biomol Eng. 2:403–430. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Girod DA, Sykes K, Jorgensen J, Tawfik O
and Tsue T: Acellular dermis compared to skin grafts in oral cavity
reconstruction. Laryngoscope. 119:2141–2149. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Livesey SA, Herndon DN, Hollyoak MA,
Atkinson YH and Nag A: Transplanted acellular allograft dermal
matrix. Potential as a template for the reconstruction of viable
dermis. Transplantation. 60:1–9. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Rhee PH, Friedman CD, Ridge JA and Kusiak
J: The use of processed allograft dermal matrix for intraoral
resurfacing: An alternative to split-thickness skin grafts. Arch
Otolaryngol Head Neck Surg. 124:1201–1204. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
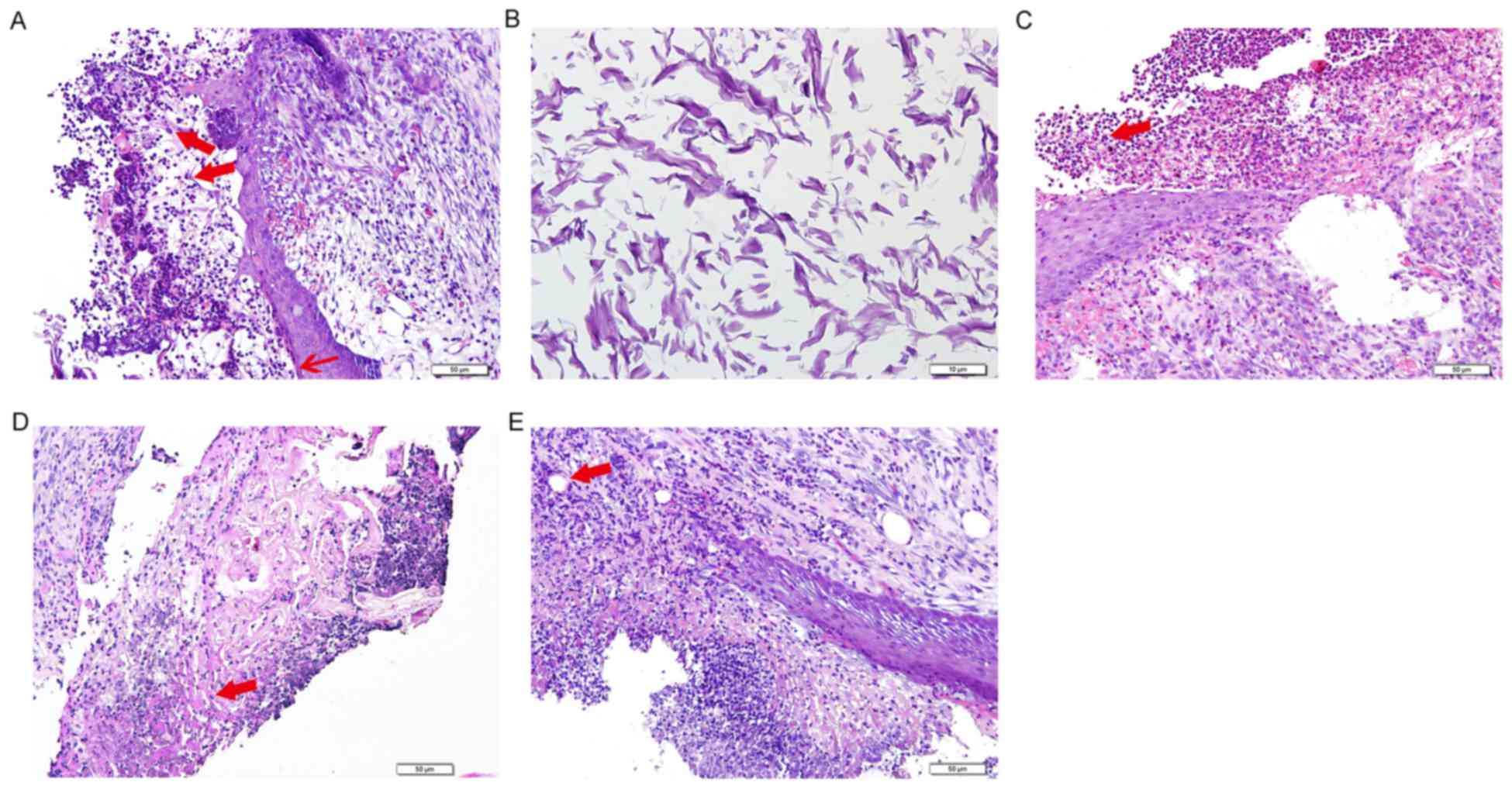
Fischer AH, Jacobson KA, Rose J and Zeller
R: Hematoxylin and eosin staining of tissue and cell sections. CSH
Protoc. 2008:pdb.prot49862008.PubMed/NCBI
|
|
11
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wainwright DJ: Use of an acellular
allograft dermal matrix (AlloDerm) in the management of
full-thickness burns. Burns. 21:243–248. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wong AK, Schonmeyr B, Singh P, Carlson DL,
Li S and Mehrara BJ: Histologic analysis of angiogenesis and
lymphangiogenesis in acellular human dermis. Plast Reconstr Surg.
121:1144–1152. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Buinewicz B and Rosen B: Acellular
cadaveric dermis (AlloDerm): A new alternative for abdominal hernia
repair. Ann Plast Surg. 52:188–194. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Becker S, Saint-Cyr M, Wong C, Dauwe P,
Nagarkar P, Thornton JF and Peng Y: AlloDerm versus DermaMatrix in
immediate expander-based breast reconstruction: A preliminary
comparison of complication profiles and material compliance. Plast
Reconstr Surg. 123:1–6; discussion 107–108. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Adetayo OA, Salcedo SE, Bahjri K and Gupta
SC: A meta-analysis of outcomes using acellular dermal matrix in
breast and abdominal wall reconstructions: Event rates and risk
factors predictive of complications. Ann Plast Surg. 77:e31–e38.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Luczyszyn SM, Papalexiou V, Novaes AB Jr,
Grisi MF, Souza SL and Taba M Jr: Acellular dermal matrix and
hydroxyapatite in prevention of ridge deformities after tooth
extraction. Implant Dent. 14:176–184. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Fernandes PG, Novaes AB Jr, de Queiroz AC,
de Souza SL, Taba M Jr, Palioto DB and Grisi MF: Ridge preservation
with acellular dermal matrix and anorganic bone matrix cell-binding
peptide P-15 after tooth extraction in humans. J Periodontol.
82:72–79. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Izumi K, Feinberg SE, Iida A and Yoshizawa
M: Intraoral grafting of an ex vivo produced oral mucosa
equivalent: A preliminary report. Int J Oral Maxillofac Surg.
32:188–197. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Xiong X, Zhao Y, Zhang W, Xie W and He S:
In vitro engineering of a palatal mucosa equivalent with acellular
porcine dermal matrix. J Biomed Mater Res A. 86:544–551. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Ophof R, Maltha JC, Von den Hoff JW and
Kuijpers-Jagtman AM: Histologic evaluation of skin-derived and
collagen-based substrates implanted in palatal wounds. Wound Repair
Regen. 12:528–538. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Wainwright D, Madden M, Luterman A, Hunt
J, Monafo W, Heimbach D, Kagan R, Sittig K, Dimick A and Herndon D:
Clinical evaluation of an acellular allograft dermal matrix in
full-thickness burns. J Burn Care Rehabil. 17:124–136. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Kridel RW, Foda H and Lunde KC: Septal
perforation repair with acellular human dermal allograft. Arch
Otolaryngol Head Neck Surg. 124:73–78. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Luczyszyn SM, Grisi MF, Novaes AB Jr,
Palioto DB, Souza SL and Taba M Jr: Histologic analysis of the
acellular dermal matrix graft incorporation process: A pilot study
in dogs. Int J Periodontics Restorative Dent. 27:341–347.
2007.PubMed/NCBI
|
|
25
|
Yannas IV, Lee E, Orgill DP, Skrabut EM
and Murphy GF: Synthesis and characterization of a model
extracellular matrix that induces partial regeneration of adult
mammalian skin. Proc Natl Acad Sci USA. 86:pp. 933–937. 1989;
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Uğurlu K, Hüthüt I, Ozçelik D, Ozer K,
Sakiz D, Yildiz K and Baş L: Epithelialization process of free
fascial flaps used in reconstruction of oral cavity mucosa defects
in dogs. Plast Reconstr Surg. 113:915–926. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Wei PC, Laurell L, Lingen MW and Geivelis
M: Acellular dermal matrix allografts to achieve increased attached
gingiva. Part 2. A histological comparative study. J Periodontol.
73:257–265. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Chaplin JM, Costantino PD, Wolpoe ME,
Bederson JB, Griffey ES and Zhang WX: Use of an acellular dermal
allograft for dural replacement: An experimental study.
Neurosurgery. 45:320–327. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Takami Y, Matsuda T, Yoshitake M,
Hanumadass M and Walter RJ: Dispase/detergent treated dermal matrix
as a dermal substitute. Burns. 22:182–190. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Szpaderska AM, Walsh CG, Steinberg MJ and
DiPietro LA: Distinct patterns of angiogenesis in oral and skin
wounds. J Dent Res. 84:309–314. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Nakanishi Y, Izumi K, Yoshizawa M, Saito
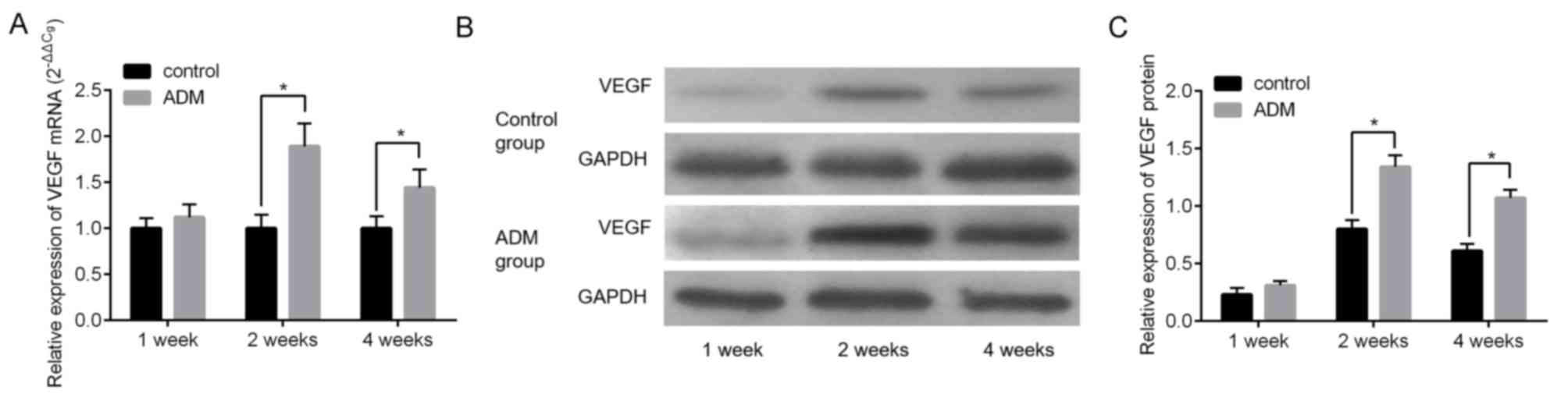
C, Kawano Y and Maeda T: The expression and production of vascular
endothelial growth factor in oral mucosa equivalents. Int J Oral
Maxillofac Surg. 36:928–933. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Lenoir MC, Bernard BA, Pautrat G, Darmon M
and Shroot B: Outer root sheath cells of human hair follicle are
able to regenerate a fully differentiated epidermis in vitro. Dev
Biol. 130:610–620. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
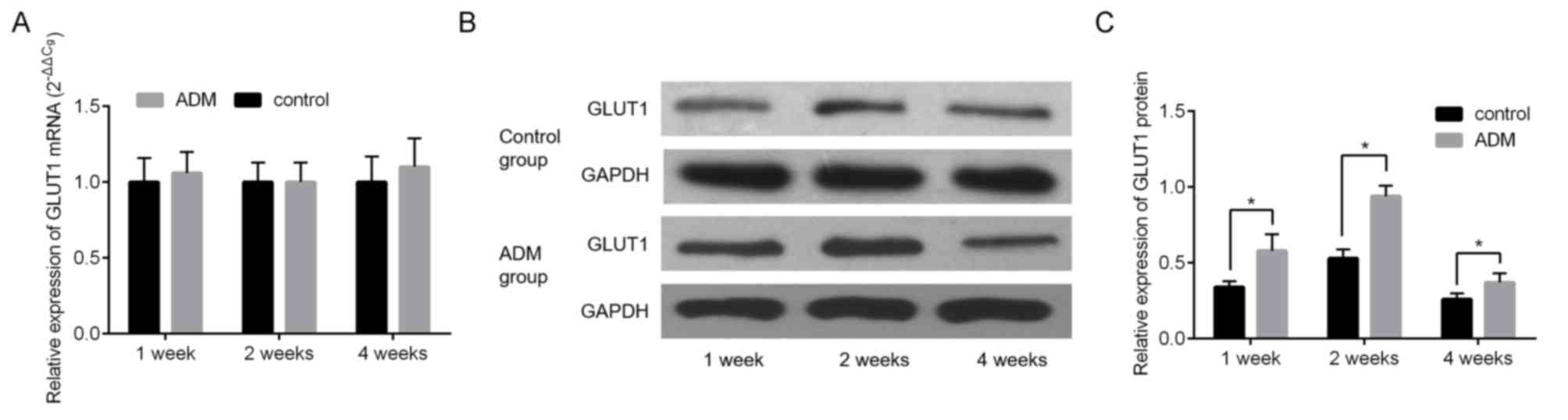
Takahashi H, Kaminski AE and Zieske JD:
Glucose transporter 1 expression is enhanced during corneal
epithelial wound repair. Exp Eye Res. 63:649–659. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Kuroki S, Yokoo S, Terashi H, Hasegawa M
and Komori T: Epithelialization in oral mucous wound healing in
terms of energy metabolism. Kobe J Med Sci. 55:E5–E15.
2009.PubMed/NCBI
|
|
35
|
Liemburg-Apers DC, Wagenaars JA, Smeitink
JA, Willems PH and Koopman WJ: Acute stimulation of glucose influx
upon mitoenergetic dysfunction requires LKB1, AMPK, Sirt2 and
mTOR-RAPTOR. J Cell Sci. 129:4411–4423. 2016. View Article : Google Scholar : PubMed/NCBI
|