Introduction
The anterior cruciate ligament (ACL) is among the
important structures that maintain the stability of knee joints
(1,2). Partial ACL injury and complete ruptures
of the ACL are associated with high energy injuries and sports
trauma. ACL injury is commonly divided into three types: Mild,
moderate and severe injury, According to the severity of the
injury. In terms of the severity of injury, conservative treatment
or ligament reconstruction can be recommended. Whichever treatment
is selected, developing an animal model of ACL injury is one of the
effective methods of studying the developmental mechanism,
prevention, treatment and rehabilitation of ACL injury.
Severe injury or complete ruptures of the ACL have
more impact on the stability of knee joints, and ligament
reconstruction is often considered as a clinical treatment
(3–8). Injury to one-quarter of the ACL is
referred to as a mild injury. In cases of mild injury, if the other
ligaments and muscles around the knee joint still maintain the
stability of the joint, ligament reconstruction surgery is not
necessary, and non-surgical treatment is usually applied. In this
aspect, related research using animal models of partial ACL injury
are helpful and necessary to improve the efficiency of non-surgical
treatments and the recovery from ACL injury.
Many animal models of ACL injury have been reported,
some of which have been widely used in related research (9–11).
Generally speaking, there is still no suitable animal model that
exactly replicates the human knee and ACL injury. On the one hand,
it is not easy to develop an ACL injury model in small animals,
such as rats, despite the decreased modeling time, as the small
size of the knee joint increases the difficulty of surgery and
nursing, leading to an increased risk of infection or even
accidental death. On the other hand, for some models of large
animals such as rabbits and dogs, it is easier to perform surgery
due to the larger surgical visual field of the knee joint. However,
a longer duration of modeling and rehabilitation are needed, which
is costly in terms of experimental funding. In particular, previous
studies have been reported that the stifle joints of sheep and the
knees of pigs may be more similar to human knees than other animals
(such as rats, rabbits or dogs) based on the size and anatomy of
the knees (12,13). However, sheep or porcine models are
different from humans in terms of their standing physics. By
contrast, primates represent valuable models for human disease
research, since they are phylogenetically close to humans, sharing
more similarities in physiology, anatomy and genetics. From
previous observations made during feeding of cynomolgus monkeys, it
was noted that the monkeys had the ability to stand or walk on
their hind limbs alone, and that the length of time spent in such a
position was greater compared with the aforementioned animals,
thereby showing more similarity with the human body in terms of the
physics of standing or walking. These physiological characteristics
allow the knee joints of primates to better mimic the human model.
Moreover, the instability of the knee joint could be more obvious
in the state of standing on hind limbs alone than on four limbs and
may, therefore, be more similar to clinical manifestation of ACL
injury in humans. Therefore, the ACL injury model of cynomolgus
monkeys may be helpful in studying injury and reconstruction of the
ACL. However, to date, few studies using an ACL injury in primates
have been reported. On the basis of this, the current study mainly
focused on modeling ACL injury in cynomolgus monkeys.
Furthermore, the previous methods of developing
animal models of ACL injury have mainly involved open surgery, with
the risk of blood loss and trauma. With injury to the soft tissues
and anatomical structures around knee joint at the time of surgery,
rather than injury to the ACL alone, these models are different
from common spontaneous sports injury to the ACL in the human body.
Besides, these methods may have negative effects on certain
follow-up experiments involving structures around the knee joint.
Considering aforementioned points, it is necessary to seek a
modeling method to overcome these shortcomings. In this aspect,
arthroscopic technique could be a better solution. Based on these
considerations, we found that the size of the knee joint in monkeys
was large enough to operate arthroscopic technique as well, in
comparison with other animals.
In this study, we developed a useful alternative
model of ACL injury in cynomolgus monkeys via arthroscopic
techniques, which may provide a basis for research into ACL
injury.
Materials and methods
Ethical statement
All procedures were approved by the Ethical
Inspection Committee of Animal Experiments of Yunnan Yinmore
Biological Technology Co., Ltd. (Yunnan, China; no. 2016001).
Animal care was in accordance with the ‘Guide for the Care and Use
of Laboratory Animals’ (Office of Science and Health Reports
CPRR/NIH 1996).
Experimental animal and feeding
A total of 18 male cynomolgus monkeys (specific
pathogen free), were purpose-bred and purchased from Yunnan Yinmore
Biological Technology Co., Ltd., with accreditation of the animal
research facilities by the Association for Assessment and
Accreditation of Laboratory Animal Care (AAALAC).
All monkeys were housed at the Laboratory Animals
Breeding Center of Yunnan Yinmore Biological Technology Co., Ltd.
In detail, the monkeys were housed in during sleeping, feeding and
rest periods in several stable cages, each measuring 1.5 m (H) × 2
m (W) × 1.5 m (D). The housing conditions were a 12/12-h light/dark
cycle, with a temperature of 22–24°C and relative humidity of
45–65%. The monkeys were fed daily with formula feeds. Water was
available ad libitum via water bottles. Additionally, all
animals were moved out of the cages to another spacious activity
room, approximately measuring 4 m (H) × 12.5 m (W) × 8 m (D),
equipped with resting shelves, a small rockery, wooden branches and
a swing, for 6–8 h of free time per day. Additionally, videos and
music were occasionally played to relax the monkeys as well.
(Fig. 1A and B).
Animal modeling
The animals were randomly divided into three groups,
including a model group (n=6), a sham operation group (n=6), and a
blank control group (n=6). Based on previous experiments and
related statistical estimations, the sample size of 6 per group can
be statistically significant, especially for experiments on
primates, such as cynomolgus monkeys. In the model group and the
sham operation group, the unilateral side of injury was chosen at
random for each animal.
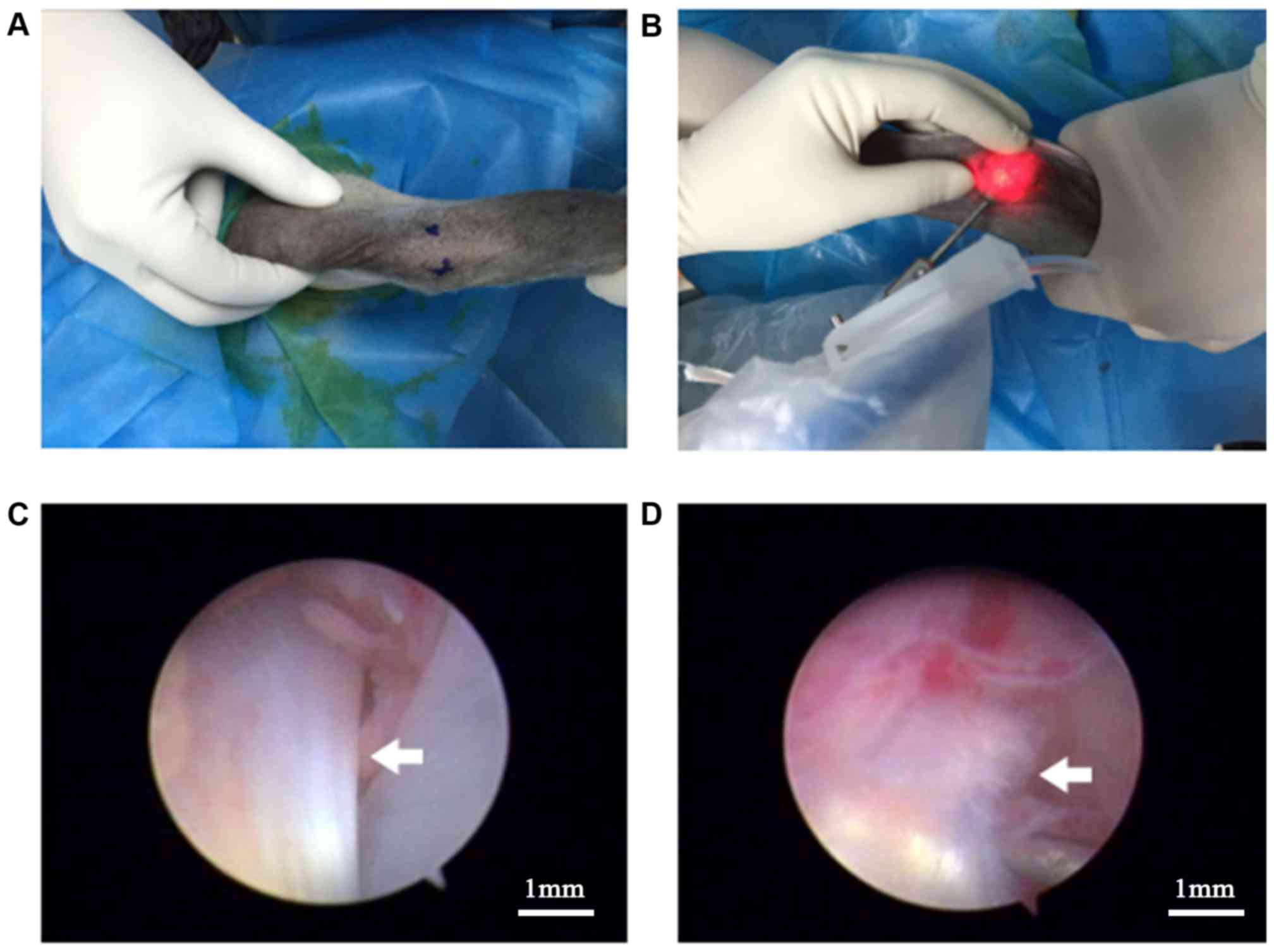
Cynomolgus monkeys in the model group were subjected
to unilateral knee surgery to induce ACL injury. The arthroscopic
instruments (Smith & Nephew Endoscopy, Andover, MA, USA;
72200616) were prepared before surgery and the equipment was
strictly sterilized by the operators. Then, the monkeys were
anesthetized using Zoletil 50 (Virbac, Carros, France; 5 mg/kg,
intramuscular) and were fixed in a supine position with the
surgical area shaved. Marking of the incision and the application
of an ipsilateral lower extremity proximal tourniquet was
performed. After all the preparatory steps, anterior medial and
anterior lateral approaches of the knee joint were built with
0.5-cm long incisions to explore the knee joint (Fig. 2A and B). Exploration indicated that
the articular cartilage, ACL, posterior cruciate ligament (PCL) and
meniscus were intact. Approximately, one-quarter of the ACL was
transversely cut (Fig. 2C and D)
under a clear arthroscopic field of vision. At the end of the
surgery, the incision was closed with 3-0 absorbable sutures (Alcon
Laboratories, Inc., Fort Worth, TX, USA). The operation finished.
The modeling operation was completed by the same group of doctors.
Soft padded bandages were placed and maintained on the operated
limbs for 2 weeks. For the first 3 postoperative days, levofloxacin
hydrochloride and sodium chloride injection (Heng Ao, Shanghai,
China; 8 mg/kg, one dose/12 h, intravenous) were used to prevent
infection. The animals were monitored daily and tramadol
hydrochloride for injections (QiMaiTe, Shijiazhuang, China; 2
mg/kg, one dose/day, intramuscular) were used to provide analgesia
as needed.
In the sham operation group, all preoperative
preparation and postoperative care was the same as the model group,
while only arthroscopic exploration was performed without any
interventions.
As a control, cynomolgus monkeys in the blank group
underwent normal feeding without any interventions.
Model identification
Magnetic resonance imaging (MRI)
The MRI (Multiva 1.5T; Philips Healthcare,
Amsterdam, The Netherlands) inspection of the knees of the monkeys
in the three groups was performed by the same radiologist, under
anesthesia, before surgery and at 2 weeks post-surgery.
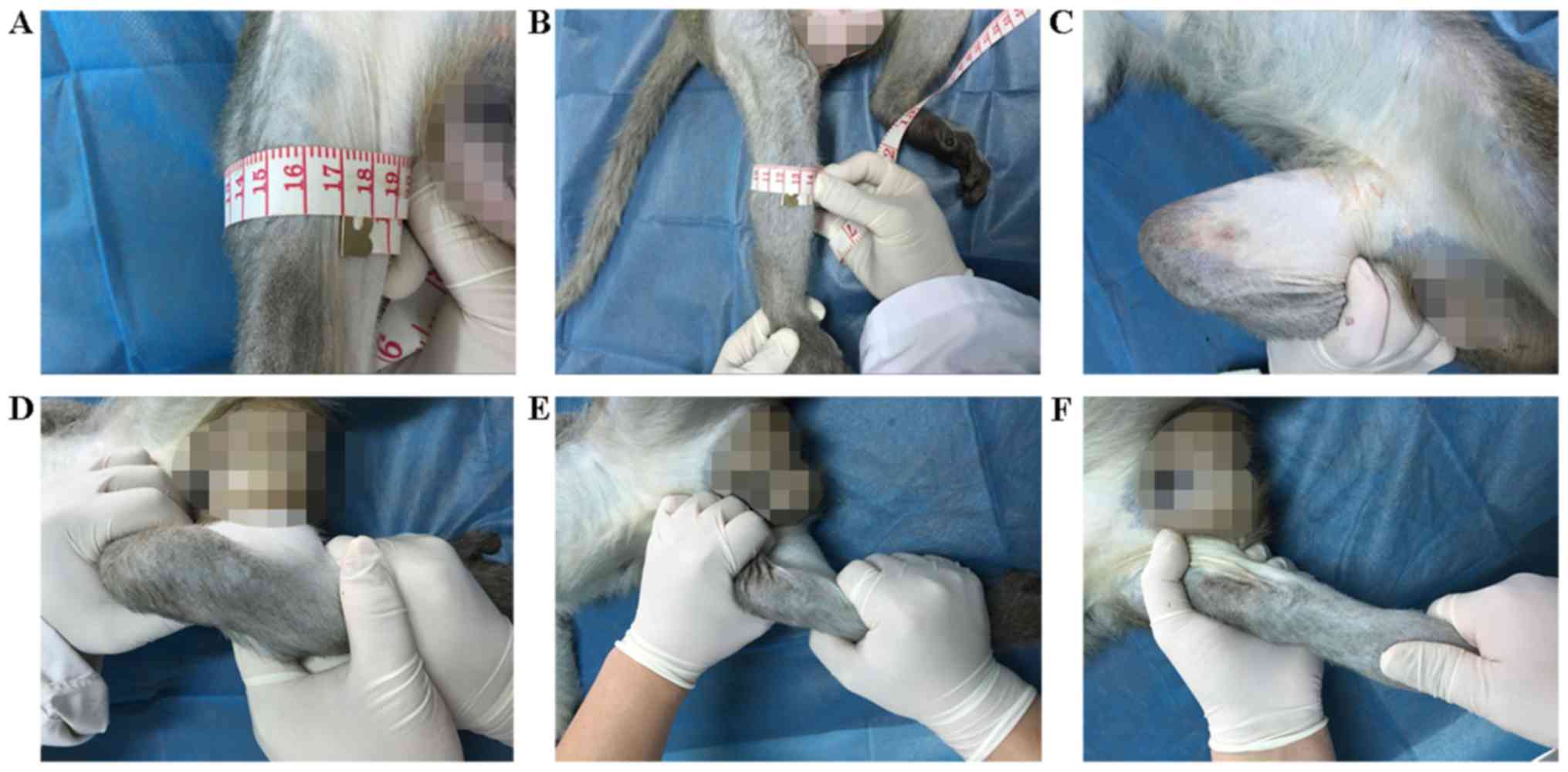
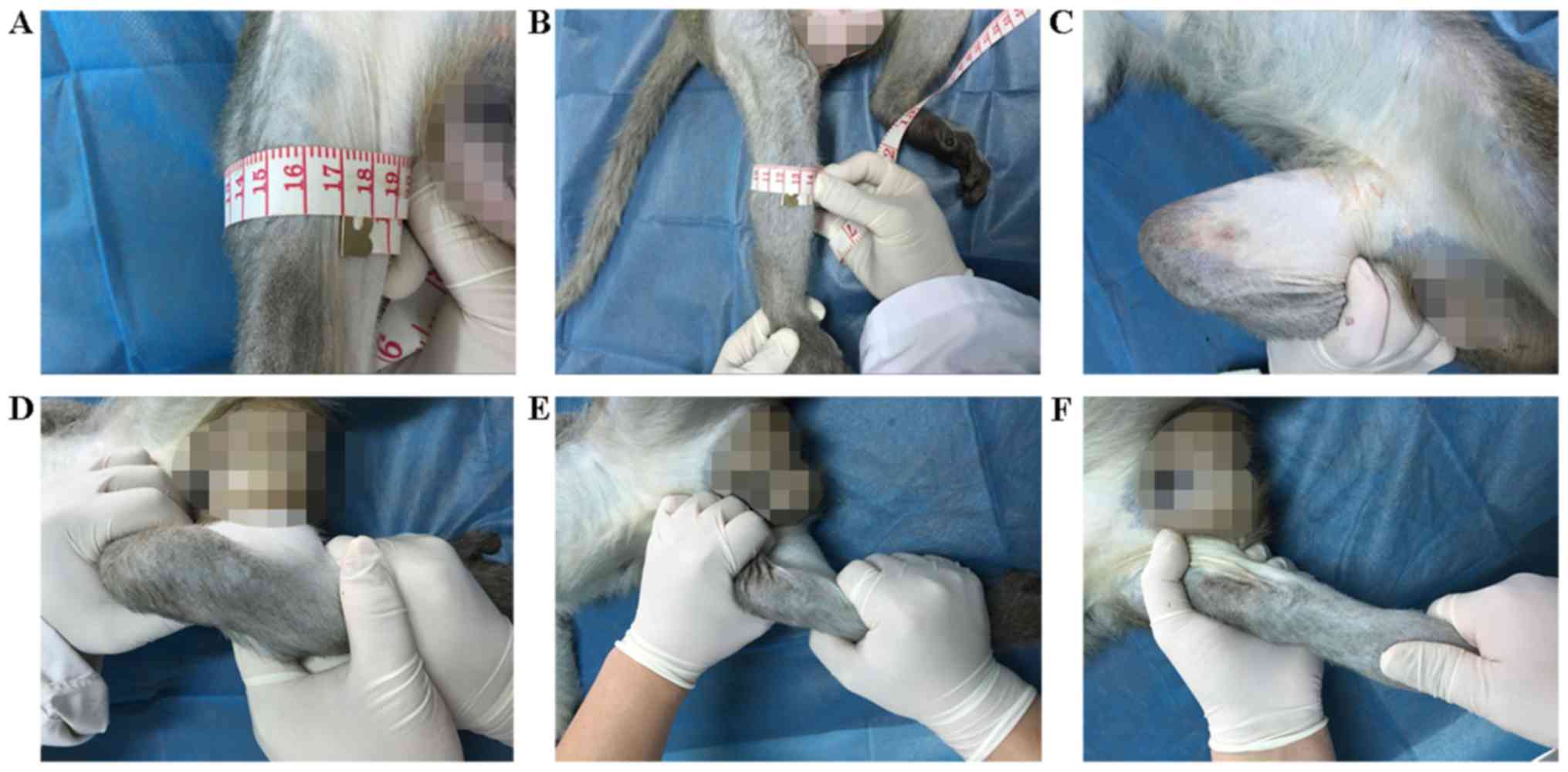
Observation of animal physiology
Before surgery, measurement of the circumference of
the thigh and calf, and of the maximum flexion degree of the knee,
as well as Anterior drawer, Lachman and Pivot-shift tests, were
performed on monkeys in the three groups under anesthesia, by the
same orthopedist specializing in surgery and recovery of the knees.
At 2 weeks post-surgery, when the incision had healed and tissue
edema had disappeared, these measurements were performed again in
the three groups.
Measurement of bilateral thigh and
calf circumference
Thigh circumference was measured at 5 cm above the
patella (Fig. 3A). Usually, the
thigh circumference of humans is measured at the suprapatellar
10–15 cm point. Because the thigh segment of the cynomolgus monkey
is shorter than that of humans, thigh circumference was tested at 5
cm above the patella on the monkeys. In addition, calf
circumference was measured at approximately the widest position of
the calf (Fig. 3B). The measurements
were helpful to compare the degree of muscular atrophy before and
after surgery.
 | Figure 3.Observation of animal physiology. (A)
Measurement of the circumference of the thigh. The thigh
circumference of humans is usually measured at the suprapatellar
10–15 cm point. As the thigh segment of the cynomolgus monkeys is
shorter than that of humans, thigh circumference was tested at 5 cm
above the patella on the monkeys. (B) Measurement of the
circumference of the calf. Calf circumference was measured at the
widest position on the calf. (C) Measurement of the maximum flexion
degree of the knee. In the state of anesthesia, the position of the
knee joint was flexed maximally in the supine position, and the
angle was measured. (D) Evaluation of the anterior drawer test.
Under anesthesia, monkeys were fixed in a supine position, with the
hips passively flexed to 45 degrees, the knee passively flexed to
90 degrees and the feet flat on the table. With the distal side of
the leg fixed, the proximal side of the leg was pulled forward by
the examiner using both hands, and the degree of movement of the
tibia was observed. (E) Evaluation of the Lachman test. The distal
side of the leg was held in one hand and the proximal side of the
calf was held with the other under anesthesia in a supine position,
so as to observe the movement by reverse force of both hands. (F)
Evaluation of the pivot-shift test. In a supine position, monkeys
were anesthetized before inspection with full extension of the knee
joint. One hand of the examiner was placed on the outside of the
knee, and the other held the foot to make the calf rotate. The knee
was gradually flexed from 0 degrees, and the tibial plateau began
to gradually move forward toward subluxation when the knee was
removed from the ‘lock’ position. When the knee was flexed to 20
degrees, instability appeared as a positive result. |
Maximum flexion degree of the
knee
Under anesthesia, the position of the knee joint was
flexed maximally in the supine position, and the angle (Fig. 3C) was measured. The measurement was
helpful to compare the motion of the knee joint before and after
surgery.
Anterior drawer test
Under anesthesia, monkeys were fixed in a supine
position, with the hips passively flexed to 45 degrees, the knee
passively flexed to 90 degrees and the feet flat on the table. With
the distal side of the leg fixed, the proximal side of the leg was
pulled forward by the examiner using both hands, and the degree of
movement of the tibia was scored as follows (Fig. 3D): (−), double tibial forward
movement was equal; (1+), the ipsilateral tibial migration was
greater than the healthy side and tibial forward movement was <5
mm; (2+), tibial forward movement was 5–10 mm; (3+), tibial forward
movement was >10 mm. In the clinic, (−) indicates that the
stability of the ipsilateral knee joint is normal. Meanwhile, other
scores indicate that the ipsilateral knee joint is unstable, and
higher scores indicate greater instability.
Lachman test
The distal side of the leg was held in one hand and
the proximal side of the calf was held in the other hand under
anesthesia in a supine position, so as to observe the movement by
reverse force of both hands (Fig.
3E). The scoring system was the same as for the anterior drawer
test.
Pivot-shift test
In a supine position, monkeys were anesthetized
before inspection with a fully-extended knee joint. One hand of the
examiner was placed on the outside of the knee, with the other
holding the foot to make the calf rotate. The knee was gradually
flexed from 0 degrees, and the tibial plateau began to gradually
move forward towards subluxation when the knee was moved from the
‘lock’ position. When the knee was flexed to 20 degrees,
instability appeared as a positive result (Fig. 3F). A positive result indicated
instability of the knee joint.
At the end of above evaluation, all cynomolgus
monkeys were fed continually as usual, in preparation for future
studies into ACL injury and other related research.
Statistical methods
All data were statistically analyzed using SPSS 17.0
(SPSS, Inc., Chicago, IL, USA) statistical software. All
measurement data are expressed as the mean ± standard deviation.
One way analysis of variance was used to compare differences among
the three groups in preoperative or postoperative indexes.
Comparisons were performed, by paired t-test and Levene's test,
between the preoperative and postoperative indexes of the same
group. The non-parametric Kruskal-Wallis H test and the
χ2 test were performed for comparison of ranked data
among the three groups. The level of statistical significance was
set at α=0.05.
Results
Animal status
At 2 weeks post-surgery, the incisions had healed
without any infection or delayed healing in the monkeys of the
model and sham operation groups. The operated limbs were able to be
exercised gradually. At the same time, the monkeys in the blank
control group remained healthy without any injury.
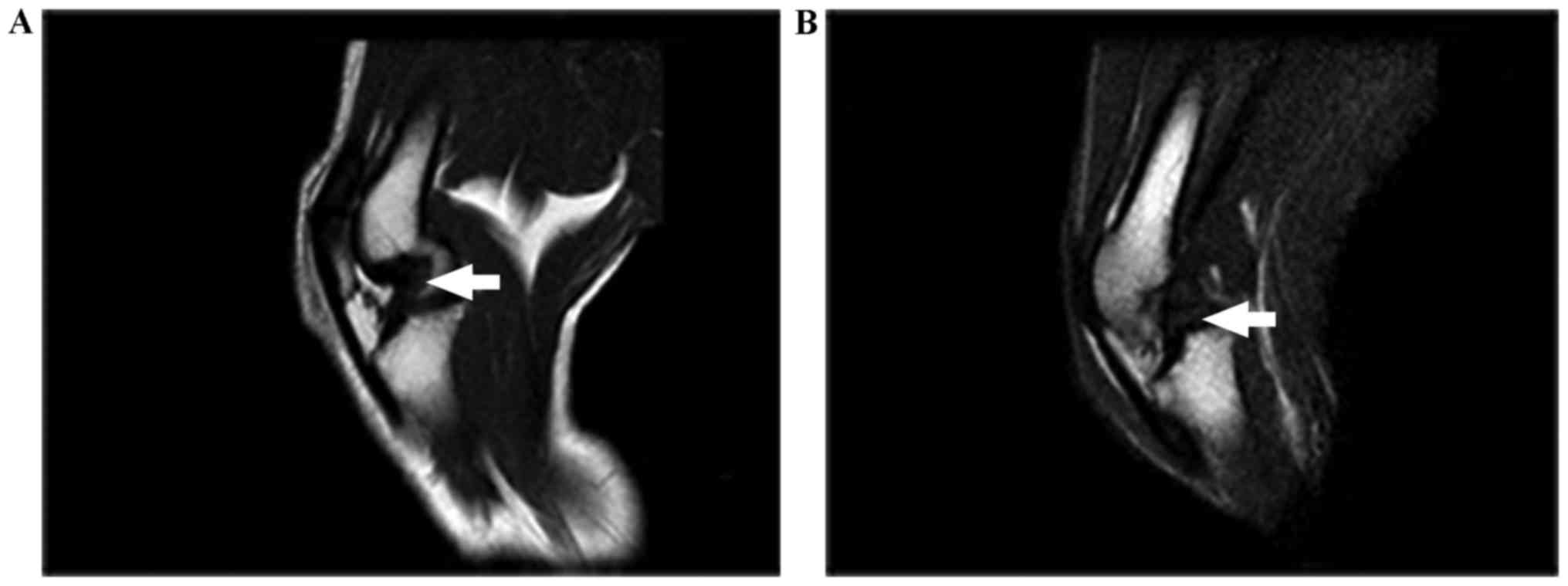
MRI
Before the operation, all animals were examined with
MRI and no abnormalities were found. The MRI inspection of the knee
joint in the model group showed that the ACL had some signs of
injury, while the articular cartilage, PCL and meniscus were intact
(Fig. 4A). In the sham operation
group and the blank control group, MRI analysis indicated that the
basic anatomical structures of the knee joint, including the
articular cartilage, ACL, PCL and meniscus, were intact (Fig. 4B).
Observation of animal physiology
Before the operation, no significant differences
were observed among the three groups regarding age, weight,
head-sacrum length, circumference of the thigh and calf, maximum
flexion degree of the knee, and anterior drawer test, Lachman test
and pivot-shift test results (Table
I).
 | Table I.Baseline characteristics of
cynomolgus monkeys prior to surgery. |
Table I.
Baseline characteristics of
cynomolgus monkeys prior to surgery.
| Parameter | Model group
(n=6) | Sham operation
group (n=6) | Blank control group
(n=6) |
|---|
| Age (years) |
4.62±0.12 |
4.62±0.10 |
4.62±0.13 |
| Weight (kg) |
6.55±0.21 |
6.52±0.18 |
6.49±0.47 |
| Head-sacrum length
(m) |
0.42±0.19 |
0.43±0.22 |
0.42±0.18 |
| Thigh circumference
(cm) |
16.85±0.31 |
16.82±0.16 |
16.87±0.32 |
| Calf circumference
(cm) |
12.03±0.34 |
12.00±0.26 |
12.03±0.41 |
| Maximum flexion
degree of knee (°) | 157.00±5.10 | 156.50±5.54 | 156.50±3.02 |
| Anterior
drawer | (−) (n=6) | (−) (n=6) | (−) (n=6) |
| Lachman | (−) (n=6) | (−) (n=6) | (−) (n=6) |
| Pivot-shift | (−) (n=6) | (−) (n=6) | (−) (n=6) |
There were no significant differences among the
three groups on examination of the circumference of the thigh and
calf, and the maximum flexion degree of the knee after surgery
(Table I). By contrast, in the
postoperative evaluations of the anterior drawer, Lachman and
pivot-shift tests, significant differences were noted among the
three groups, while no significant differences were found between
the sham operation and the blank control groups (Table II).
 | Table II.Comparison between the
characteristics prior to and following surgery in cynomolgus
monkeys. |
Table II.
Comparison between the
characteristics prior to and following surgery in cynomolgus
monkeys.
| Group | Time | Thigh circumference
(cm) | Calf circumference
(cm) | Maximum flexion
degree of knee (°) |
|---|
| Model group
(n=6) | Preoperation |
16.85±0.31 |
12.03±0.34 |
157.00±5.10 |
|
| Postoperation |
16.78±0.27 |
12.30±0.34 |
156.00±1.46 |
| Sham operation
group (n=6) | Preoperation |
16.82±0.16 |
12.00±0.26 |
156.50±5.54 |
|
| Postoperation |
16.82±0.16 |
11.92±0.87 |
156.17±2.20 |
| Blank control group
(n=6) | Preoperation |
16.87±0.32 |
12.03±0.41 |
156.50±3.02 |
|
| Postoperation |
16.88±0.24 |
11.90±0.49 |
156.00±1.29 |
No significant differences were observed between the
sham operation group and the blank control group regarding the
physical evaluations performed before and after surgery (Table II).
In the model group, the differences in the anterior
drawer test, Lachman test and pivot-shift test results were
significant between the preoperative and postoperative evaluations
(Table III). No significant
differences were identified between the preoperative and
postoperative evaluations of the circumference of the thigh and
calf, and the maximum flexion degree of the knee.
 | Table III.Comparison of physical examinations
prior to and following surgery in cynomolgus monkeys. |
Table III.
Comparison of physical examinations
prior to and following surgery in cynomolgus monkeys.
| Group | Time | Anterior drawer
test | Lachman test | Pivot-shift
test |
|---|
| Model group
(n=6) | Preoperation | (−) (n=6) | (−) (n=6) | (−) (n=6) |
|
| Postoperation | (2+) (n=5), (3+)
(n=1)a–c | (2+) (n=3), (3+)
(n=3)a–c | (+)
(n=6)a–c |
| Sham operation
group (n=6) | Preoperation | 0+(n=6) | 0+(n=6) | (−) (n=6) |
|
| Postoperation | 0+(n=6) | 0+(n=6) | (−) (n=6) |
| Blank control group
(n=6) | Preoperation | 0+(n=6) | 0+(n=6) | (−) (n=6) |
|
| Postoperation | 0+(n=6) | 0+(n=6) | (−) (n=6) |
Discussion
There is no definite classification for ACL
injuries, Ihara and Kawano (14)
classified MRI of the ACL in the sagittal plan into 4 types
according to the degree of injury: Type I, straight and continuous
band; type II, curved and continuous band; type III, displacement;
and type IV, disrupted or horizontally oriented or unclear.
American Academy of Orthopaedic Surgeons (AAOS) considered the
injured ligaments as ‘sprains’ and the ACL injuries are graded on a
severity scale: Grade 1 Sprains. The ligament is mildly damaged, it
has been slightly stretched, but is still able to help keep the
knee joint stable. Grade 2 Sprains. A Grade 2 Sprain stretches the
ligament to the point where it becomes loose, this is often
referred to as a partial tear of the ligament. Grade 3 Sprains.
This type of sprain is most commonly referred to as a complete tear
of the ligament, the ligament has been split into two pieces, and
the knee joint is unstable. It is known that the injured ACL has
the potential for primary healing, and several studies have
reported a spontaneous healing of the ACL after acute rupture
(15–17). Also, according to AAOS, nonsurgical
management of isolated ACL tears is likely to be successful or may
be indicated in patients with partial tears and no instability
symptoms. Whereas, there is a limitation for doctors to identify
the mild injury, and it would result in worse outcome if the
patients missed the proper treatments. Partial tears take up 10 to
35% of ACL lesions, which are more or less serious lesions with a
variable prognosis (18,19). The treatment of choice for partial
ACL tears remains ambiguous. Traditionally, there are two
treatments for partial tears: surgical treatments which require
sacrifice of the remnant ACL fiber for proper graft placement,
whereas nonsurgical treatments are suitable for patients who do not
participate in strenuous sports activities (20,21).
Besides, recently, selective ACL augmentation has been considered
as an alternative choice of treatment (22,23), as
it can preserve knee joint proprioception (24). Whereas the biological and
biomechanical advantages of the augmentation have not been fully
investigated (25). Several
comparative studies have compared augmentation with classical ACL
reconstruction and got unlike outcomes (26–28).
Thus, it is necessary to create models for studying the mild
injury. And one-quarter ACL injury is an ideal tear type that not
only represents for partial tear but also minimizes the injuries to
model animals.
In MRI analysis, the degree and range of injury of
the ACL may be displayed (29–31),
although the MRI signal of the ACL may be uneven, due to the
occurrence of natural degeneration of the ACL (32–34). As
a result, it is easy to misdiagnose ACL injury via MRI. Therefore,
MRI can only be used as an objective auxiliary examination of ACL
injury and must be confirmed with arthroscopy. In our study, the
model was evaluated after 2 weeks, mainly because tissues around
the knee joint that had been injured in the operation would have
recovered, and edema would have dissipated. Comparisons between the
functional evaluations of the knee joint were performed among the
three groups, as well as preoperative and postoperative evaluation
in the model group alone. Statistical differences were found in the
evaluations of the anterior drawer test, Lachman test and
pivot-shift test (35–37), while no significant differences in
the maximum flexion degree of the knee, and the circumference of
the thigh and calf, were observed. The results indicated that
one-quarter ACL injury may cause instability of the knee joint when
ligaments and muscles around the knee joint do not compensate to
maintain the stability of the joint (38–41),
which reflected the main characteristics of the model. At the same
time, it is notable that short-term instability of knee will not
lead to atrophy of the muscles of the hind limb and decreased
flexion of the knee. Moreover, in the sham operation and the blank
control groups, no statistical differences were observed regarding
the physiological tests performed before and after intervention,
excluding the effects of objective conditions on the development of
model, making the results more convincing.
The cynomolgus monkey ACL injury model has certain
advantages (42). Firstly, compared
with other experimental animals, cynomolgus monkeys are more
similar to human beings in the anatomical structure of the knee
joints, such as the femoral condyle, tibial plateau, patella,
patellar tendons, ACL, PCL, and medial and lateral meniscus.
Secondly, the instability of the knee joint after ACL injury in
monkeys is more similar to the common manifestation of ACL injury
in humans, as a result of similar standing physics. For instance,
the knee joints of the cynomolgus monkeys often bear vertical
weight through standing on the hind limbs during daily activities.
The length of time that the cynomolgus monkey spends standing
vertically or squatting is more similar to humans, compared with
other model animals, indicating similar biomechanical
characteristics. Thirdly, the size of the articular cavity is
acceptable for the arthroscopic lens (2.7 mm), allowing for
modeling by arthroscopy in this study.
In addition, this method of modeling is a
short-duration operation with minimal invasive surgical injury.
Animals were operated on under strict sterile procedures, and
surgery was performed by a qualified surgeon during the process of
modeling. The lack of any infection indicated that primates, such
as cynomolgus monkeys, may have a strong immune system, which is
conducive to an enhanced success rate of modeling. Simultaneously,
this reduces any interference of infection in the modeling process.
The whole modeling process was conducive to the rapid development
of a model with fast recovery and fewer adverse effects. Therefore,
this model of ACL injury is more similar to human ACL injury, which
may indicate its greater suitability, compared with other animals,
for basic research and clinical applications.
Arthroscopic techniques have been successfully
applied in many clinical disciplines (43,44). In
terms of joint surgery, arthroscopy has been widely used in the
shoulder, elbow, wrist, hip, knee, ankle and other joints (45–50),
especially in applications in the knee joint, and the technology
has progressed (51–57). As a result, arthroscopic techniques
were selected to develop the present model, due a series of
advantages. Firstly, compared with other modeling methods of open
surgery, the surgical trauma is limited and the surgical skin
incision is only 0.5 cm in length, leading to rapid postoperative
healing without other injuries or complications. This can
effectively ensure the simplicity of the model and reduce confounds
to the experimental results. Secondly, the small amount of
intraoperative bleeding reduces the risk of postoperative
complications, such as blood accumulation in the joint, infection,
inflammation and tissue adhesion after surgery. Thirdly,
arthroscopic techniques have the characteristic of enhanced
visibility in the joint cavity, reducing damage to surrounding
tissues and structures, so as to allow for quantification and
precision regarding damage to the ACL. Finally, under arthroscopy,
the tissue (joint fluid, ligaments, synovial membrane and
cartilage) in the joint cavity can be analyzed via dynamic
monitoring.
Despite the efficiency of the model obtained in this
study, certain limitations remained. Primarily, all of the
cynomolgus monkeys were male and there was, therefore, uncertainty
about the additional effects of gender on the results. In addition,
the model was evaluated at 2 weeks post-surgery, so there was a
lack of long term follow-up regarding the effects of the
arthroscopic surgery. The evaluation criteria of the animal model
could be more in-depth. In addition, the study did not include
pathological staining, immunohistochemistry or any other follow-up
observation of the ACL, and microscopic changes in the ACL due to
injury were not observed. All of these considerations remain to be
addressed in future studies.
In conclusion, the cynomolgus monkey model of ACL
injury, with the main feature of instability of the knee joint,
provides an important tool for basic research into ACL. Using the
arthroscopic technique, a method associated with little surgical
trauma and a short surgical and recovery duration, the aim of
quantitative and accurate ACL injury can be achieved. This model
may be helpful for basic research in this field.
Glossary
Abbreviations
Abbreviations:
|
ACL
|
anterior cruciate ligament
|
|
SPF
|
specific pathogen free
|
|
AAALAC
|
Association for Assessment and
Accreditation of Laboratory Animal Care International
|
|
PCL
|
posterior cruciate ligament
|
References
|
1
|
McHugh MP, Tyler TF, Nicholas SJ, Browne
MG and Gleim GW: Electromyographic analysis of quadriceps fatigue
after anterior cruciate ligament reconstruction. J Orthop Sports
Phys Ther. 31:25–32. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Rahnemai-Azar AA, Sabzevari S, Irarrázaval
S, Chao T and Fu FH: Anatomical individualized ACL reconstruction.
Arch Bone Jt Surg. 4:291–297. 2016.PubMed/NCBI
|
|
3
|
Fanlli GC, Orcutt DR and Edson CJ: The
multiple-ligament injured knee: Evaluation, treatment, and results.
Arthroscopy. 21:471–486. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Poehling GG, Curl WW, Lee CA, Ginn TA,
Rushing JT, Naughton MJ, Holden MB, Martin DF and Smith BP:
Analysis of outcomes of anterior cructate ligament repair with
5-year follw up: Allograft versus autograft. Arthroscopy.
21:774–785. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Almqvist KF, Willaert P, De Brabandere S,
Criel K and Verdonk R: A long-term study of anterior cruciate
ligament allograft reconstruction. Knee Surg Sports Traumatol
Arthrosc. 17:818–822. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Xie X, Liu X, Chen Z, Yu Y, Peng S and Li
Q: A meta-analysis of bone-patellar tendon-bone autograft versus
four-strand hamstring tendon autograft for anterior cruciate
ligament reconstruction. Knee. 22:100–110. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Calvo R, Figueroa D, Gili F, Vaisman A,
Mocoçain P, Espinosa M, Espinosa M, León A and Arellano S:
Transphyseal anterior cruciate ligament reconstruction in patients
with open physes: 10-year follow-up study. Am J Sports Med.
43:289–294. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sonnery-Cottet B, Thaunat M, Freychet B,
Pupim BH, Murphy CG and Claes S: Outcome of a combined anterior
cruciate ligament and anterolateral ligament reconstruction
technique with a minimum 2-year follow-up. Am J Sports Med.
43:1598–1605. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kiapour AM, Shalvoy MR, Murray MM and
Fleming BC: Validation of porcine knee as a sex-specific model to
study human anterior cruciate ligament disorders. Clin Orthop Relat
Res. 473:639–650. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Maerz T, Kurdziel MD, Davidson AA, Baker
KC, Anderson K and Matthew HW: Biomechanical characterization of a
model of noninvasive, traumatic anterior cruciate ligament injury
in the rat. Ann Biomed Eng. 43:2467–2476. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kiapour AM, Fleming BC, Proffen BL and
Murray MM: Sex influences the biomechanical outcomes of anterior
cruciate ligament reconstruction in a pre-clinical large animal
model. Am J Sports Med. 43:1623–1631. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Proffen BL, McElfresh M, Fleming BC and
Murray MM: A comparative anatomical study of the human knee and six
animal species. Knee. 19:493–499. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Madry H, Ochi M, Cucchiarini M, Pape D and
Seil R: Large animal models in experimental knee sports surgery:
Focus on clinical translation. J Exp Orthop. 2:92015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ihara H and Kawano T: Influence of age on
healing capacity of acute tears of the anterior cruciate ligament
based on magnetic resonance imaging assessment. J Comput Assist
Tomogr. 41:206–211. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Fujimoto E, Sumen Y, Ochi M and Ikuta Y:
Spontaneous healing of acute anterior cruciate ligament (ACL)
injuries-conservative treatment using an extension block soft brace
without anterior stabilization. Arch Orthop Trauma Surg.
122:212–216. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ihara H, Miwa M, Deya K and Torisu K: MRI
of anterior cruciate ligament healing. J Comput Assist Tomogr.
20:317–321. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kurosaka M, Yoshiya S, Mizuno T and Mizuno
K: Spontaneous healing of a tear of the anterior cruciate ligament:
A report of two cases. J Bone Joint Surg Am. 80:1200–1203. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Guenoun D, Le Corroller T, Amous Z, Pauly
V, Sbihi A and Champsaur P: The contribution of MRI to the
diagnosis of traumatic tears of the anterior cruciate ligament.
Diagn Interv Imaging. 93:331–341. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Donell ST, Marshall TJ, Darrah C and
Shepstone L: Cruciate ligament assessment in MRI scans: A pilot
study of a static drawer technique. Knee. 13:137–144. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Bak K, Scavenius M, Hansen S, Nørring K,
Jensen KH and Jørgensen U: Isolated partial rupture of the anterior
cruciate ligament: Long-term follow-up of 56 cases. Knee Surg
Sports Traumatol Arthrosc. 5:66–71. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Noyes FR, Mooar LA, Moorman CT III and
McGinniss GH: Partial tears of the anterior cruciate ligament:
Progression to complete ligament deficiency. J Bone Joint Surg Br.
71:825–833. 1989.PubMed/NCBI
|
|
22
|
Dienst M, Burks RT and Greis PE: Anatomy
and biomechanics of the anterior cruciate ligament. Orthop Clin
North Am. 33:605–620, v. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Duthon VB, Barea C, Abrassart S, Fasel JH,
Fritschy D and Ménétrey J: Anatomy of the anterior cruciate
ligament. Knee Surg Sports Traumatol Arthrosc. 14:204–213. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Buda R, Ferruzzi A, Vannini F, Zambelli L
and Di Caprio F: Augmentation technique with semitendinosus and
gracilis tendons in chronic partial lesions of the ACL: Clinical
and arthrometric analysis. Knee Surg Sports Traumatol Arthrosc.
14:1101–1107. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Mifune Y, Ota S, Takayama K, Hoshino Y,
Matsumoto T, Kuroda R, Kurosaka M, Fu FH and Huard J: Therapeutic
advantage in selective ligament augmentation for partial tears of
the anterior cruciate ligament: Results in an animal model. Am J
Sports Med. 41:365–373. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Serrano-Fernandez JM, Espejo-Baena A,
Martin-Castilla B, De La Torre-Solis F, Mariscal-Lara J and
Merino-Ruiz ML: Augmentation technique for partial ACL ruptures
using semitendinosus tendon in the over-the-top position. Knee Surg
Sports Traumatol Arthrosc. 18:1214–1218. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Demirağ B, Ermutlu C, Aydemir F and Durak
K: A comparison of clinical outcome of augmentation and standard
reconstruction techniques for partial anterior cruciate ligament
tears. Eklem Hastalik Cerrahisi. 23:140–144. 2012.PubMed/NCBI
|
|
28
|
Maestro A, Suárez-Suárez MA,
Rodríguez-López L and Villa-Vigil A: Stability evaluation after
isolated reconstruction of anteromedial or posterolateral bundle in
symptomatic partial tears of anterior cruciate ligament. Eur J
Orthop Surg Traumatol. 23:471–480. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Vahey TN, Broome DR, Kayes KJ and
Shelbourne KD: Acute and chronic tears of the anterior cruciate
ligament: Differential features at MR imaging. Radiology.
181:251–253. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Moore SL: Imaging the anterior cruciate
ligament. Orthop Clin North Am. 33:663–674. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Lee K, Siegel MJ, Lau DM, Hildebolt CF and
Matava MJ: Anterior cruciate ligament tears: MR imaging-based
diagnosis in a pediatric population. Radiology. 213:697–704. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Cushner FD, La Rosa DF, Vigorita VJ,
Scuderi GR, Scott WN and Insall JN: A quantitative histologic
comparison: ACL degeneration in the osteoarthritic knee. J
Arthroplasty. 18:687–692. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Zou YC, Chen LH, Ye YL, Yang GG, Mao Z,
Liu DD, Chen JQ, Chen JJ and Liu G: Attenuated synovial fluid
ghrelin levels are linked with cartilage damage, meniscus injury,
and clinical symptoms in patients with knee anterior cruciate
ligament deficiency. Discov Med. 22:325–335. 2016.PubMed/NCBI
|
|
34
|
Pedoia V, Su F, Amano K, Li Q, McCulloch
CE, Souza RB, Link TM, Ma BC and Li X: Analysis of the articular
cartilage T1ρ and T2 relaxation times changes after ACL
reconstruction in injured and contralateral knees and relationships
with bone shape. J Orthop Res. 35:707–717. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Kartus J, Movin T and Karlsson J:
Donor-site morbidity and anterior knee problems after anterior
cruciate ligament reconstruction using autografts. Arthroscopy.
17:971–980. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Adachi N, Ochi M, Uchio Y, Sakai Y,
Kuriwaka M and Fujihara A: Harvesting hamstring tendons for ACL
reconstruction influences postoperative hamstring muscle
performance. Arch Orthop Trauma Surg. 123:460–465. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Choi NH, Yang BS and Victoroff BN:
Clinical and radiological outcomes after hamstring anterior
cruciate ligament reconstructions: Comparison between fixed-loop
and adjustable-loop cortical suspension devices. Am J Sports Med.
45:826–831. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Boeth H, Duda GN, Heller MO, Ehrig RM,
Doyscher R, Jung T, Moewis P, Scheffler S and Taylor WR: Anterior
cruciate ligament-deficient patients with passive knee joint laxity
have a decreased range of anterior-posterior motion during active
movements. Am J Sports Med. 41:1051–1057. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Mather RC III, Koenig L, Kocher MS, Dall
TM, Gallo P, Scott DJ, Bach BR Jr and Spindler KP; MOON Knee Group,
: Societal and economic impact of anterior cruciate ligament tears.
J Bone Joint Surg Am. 95:1751–1759. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Bohn MB, Petersen AK, Nielsen DB, Sørensen
H and Lind M: Three-dimensional kinematic and kinetic analysis of
knee rotational stability in ACL-deficient patients during walking,
running and pivoting. J Exp Orthop. 3:272016. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Goetz J, Schiessl S, Baier C, Dullien S,
Mueller K, Grifka J and Koeck F: Postural stability after
patient-specific interpositional knee spacer or total knee
arthroplasty: A comparative study. Int Orthop. 41:67–73. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Fisher MB, Liang R, Jung HJ, Kim KE,
Zamarra G, Almarza AJ, McMahon PJ and Woo SL: Potential of healing
a transected anterior cruciate ligament with genetically modified
extracellular matrix bioscaffolds in a goat model. Knee Surg Sports
Traumatol Arthrosc. 20:1357–1365. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Aglietti P, Zaccherotti G, Menchetti PP
and De Biase P: A comparison of clinical and radiological
parameters with two arthroscopic techniques for anterior cruciate
ligament reconstruction. Knee Surg Sports Traumatol Arthrosc.
3:2–8. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Zelle S, Zantop T, Schanz S and Petersen
W: Arthroscopic techniques for the fixation of a three-dimensional
scaffold for autologous chondrocyte transplantation: Structural
properties in an in vitro model. Arthroscopy. 23:1073–1078. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Dørum IH, Heir S, Solheim E and Magnussen
LH: Implementation of conservative treatment prior to arthroscopic
subacromial decompression of the shoulder. Knee Surg Sports
Traumatol Arthrosc. 25:2060–2066. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Galle SE, Beck JD, Burchette RJ and
Harness NG: Outcomes of elbow arthroscopic osteocapsular
arthroplasty. J Hand Surg Am. 41:184–191. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Hao J, Xu Z and Zhao Z: Ulnar impaction
syndrome: Managed by wrist arthroscopy. Indian J Orthop.
50:172–176. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Kubo T, Utsunomiya H, Watanuki M, Hayashi
H, Sakai A and Uchida S: Hip arthroscopic osteochondral autologous
transplantation for treating osteochondritis dissecans of the
femoral head. Arthrosc Tech. 4:e675–e680. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Fosco M and Dagher E: Proposal of a
therapeutic protocol for selected patients with patellofemoral knee
osteoarthritis: Arthroscopic lateral retinacular release followed
by viscosupplementation. Musculoskelet Surg. 100:171–178. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Colcuc C, Fischer S, Colcuc S, Busse D,
Bliemel C, Neun O, Abt HP and Hoffmann R: Treatment strategies for
partial chronic instability of the distal syndesmosis: An
arthroscopic grading scale and operative staging concept. Arch
Orthop Trauma Surg. 136:157–163. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Kim SJ, Jo SB, Kim TW, Chang JH, Choi HS
and Oh KS: A modified arthroscopic anterior cruciate ligament
double-bundle reconstruction technique with autogenous quadriceps
tendon graft: Remnant-preserving technique. Arch Orthop Trauma
Surg. 129:403–407. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Ahn JH, Lee YS and Ha HC: Anterior
cruciate ligament reconstruction with preservation of remnant
bundle using hamstring autograft: Technical note. Arch Orthop
Trauma Surg. 129:1011–1015. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Lee BI, Min KD, Choi HS, Kwon SW, Chun DI,
Yun ES, Lee DW, Jin SY and Yoo JH: Immunohistochemical study of
mechanoreceptors in the tibial remnant of the ruptured anterior
cruciate ligament in human knees. Knee Surg Sports Traumatol
Arthrosc. 17:1095–1101. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Ochi M, Adachi N, Uchio Y, Deie M,
Kumahashi N, Ishikawa M and Sera S: A minimum 2-year follow-up
after selective anteromedial or posterolateral bundle anterior
cruciate ligament reconstruction. Arthroscopy. 25:117–122. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Lee JH, Bae DK, Song SJ, Cho SM and Yoon
KH: Comparison of clinical results and second-look arthroscopy
findings after arthroscopic anterior cruciate ligament
reconstruction using 3 different types of grafts. Arthroscopy.
26:41–49. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Morey VM, Nag HL, Chowdhury B, Pannu CD,
Meena S, Kumar K and Palaniswamy A: Arthroscopic anatomic double
bundle anterior cruciate ligament reconstruction: Our experience
with follow-up of 4 years. J Clin Orthop Trauma. 7:17–22. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Morey VM, Nag HL, Chowdhury B, Sankineani
SR and Naranje SM: A prospective comparative study of clinical and
functional outcomes between anatomic double bundle and single
bundle hamstring grafts for arthroscopic anterior cruciate ligament
reconstruction. Int J Surg. 21:162–167. 2015. View Article : Google Scholar : PubMed/NCBI
|