Introduction
Inguinal hernias in children is mainly caused by
non-closed or incompletely closed congenital peritoneal
encapsulation (1). It is a common
disease frequently seen in children, which is considered a
congenital disease. The high ligation of the hernias is the
standard procedure for inguinal hernias in children with a high
success and low incidence rate of complications (2). In previous years, with the development
of the minimally invasive herniorrhaphy, the treatment method has
been gradually changed from the traditional open into the minimally
invasive laparoscopic herniorrhaphy. The meta-analysis of Yang
et al (3) reported that the
laparoscopic herniorrhaphy was more effective in the treatment of
bilateral inguinal hernias with a lower incidence rate of
contralateral hernias than conventional open herniorrhaphy. At the
approach level, the laparoscopic herniorrhaphy has two approaches,
that is; the intraperitoneal approach (4,5); and the
extraperitoneal approach (6). The
extracorporeal approach refers to the operation that the suture is
completed, the knot is tied and the inner ring is closed (by both
single- and double-site laparoscopies) in vitro, which is
the most widely used technology at present. In order to compare the
difference between the two laparoscopic herniorrhaphies in the
treatment of inguinal hernias in children, we selected 1,010
patients with inguinal hernias who were admitted to Beijing
Chao-Yang Hospital of Capital Medical University from March 2011 to
December 2014 and treated with the single-site laparoscopic
herniorrhaphy (SSLH) and double-site laparoscopic herniorrhaphy
(DSLH) for children with inguinal hernias.
Patients and methods
A total of 1,010 children with inguinal hernias who
were diagnosed and treated by the western district of Beijing
Chao-Yang Hospital of Capital Medical University were selected. A
total of 502 children were treated with the traditional DSLH from
March 2011 to June 2013 and 508 children were treated with the SSLH
using needle instruments from July 2013 to the end of 2014.
Symptoms and the results of ultrasound and other auxiliary tests of
all the children were consistent with the diagnostic criteria of
inguinal hernias (7). In the
single-site group using needle instruments, there were 440 males
and 68 females aged 1–11 years with the mean age of 4.32±1.62
years. Among them, there were 371 children with hernias on the
right side and 137 children on the left side. In the traditional
double-site group: There were 452 males and 50 females aged 1–11
aged years with the mean age of 4.46±1.34 years. Among them, there
were 356 children with hernias on the right side and 146 children
on the left side. All the children were diagnosed with unilateral
inguinal hernias and received the herniorrhaphy for the first time.
Parents signed the informed consent. All the children were followed
up for 2 years. The study was approved by the Ethics Committee of
Beijing Chao-Yang Hospital of Capital Medical University and
informed consents were signed by the patients and/or guardians.
Operation methods
The SSLH using needle instruments
Children received general anesthesia through the
laryngeal mask airway and were placed in the trendelenburg position
where the feet were higher than the head. A 5 mm incision was cut
in the umbilical ring or the lower edge of the skin folds to
establish pneumoperitoneum, and the air pressure was maintained at
8–10 mmHg (1 mmHg = 0.133 kPa). A 5 mm laparoscope was inserted at
30° through puncturing the detection of bilateral inner ring. A 1.5
mm incision was cut on the middle or relative upper point of the
linea alba on the hypogastrium. A 1.5 mm incision was cut on the
projection spot on the top surface of the inner ring, and the
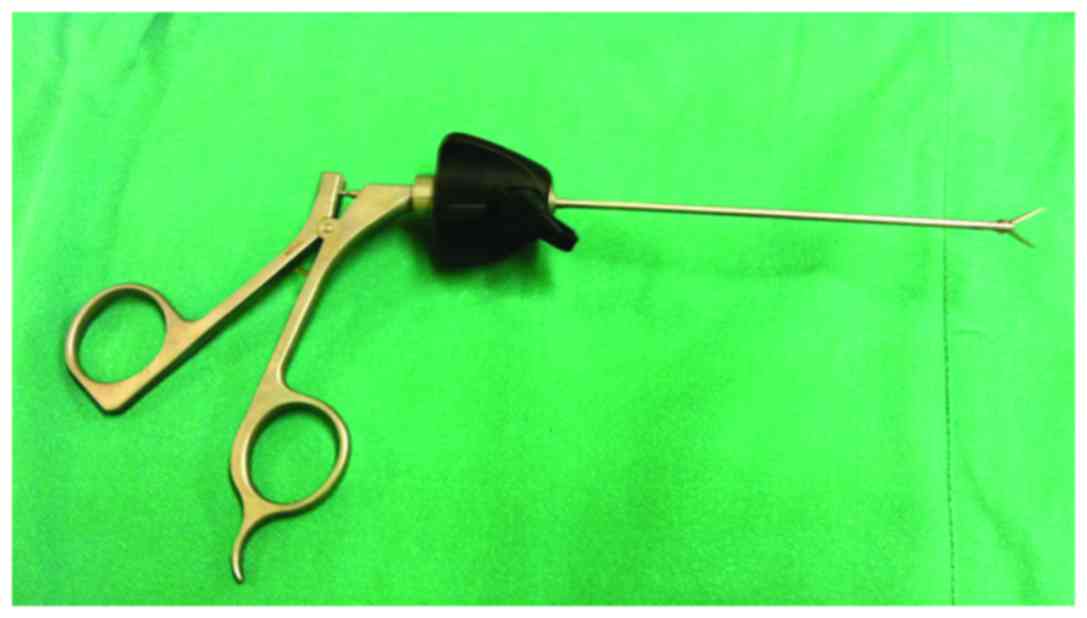
home-made needle instrument was inserted (Fig. 1). We punctured with no. 4 polyester
thread crochet to the peritoneum. Under the laparoscopic
monitoring, the needle instrument and crochet proceeded from 11
o'clock position of the inner ring to avoid the lower abdominal
artery and along the inner ring from top to bottom under the
peritoneum. After they came across seminiferous ducts and spermatic
vessels, they punctured the peritoneum into the abdominal cavity.
The needle instrument was used to pull the two threads, which were
then left in the abdominal cavity, and the crochet was taken out.
Afterwards, we inserted the crochet from the original skin
incision. The crochet proceeded from the 12 o'clock position of the
inner ring along the inner ring under the outer half cycle of
peritoneum. After it reached the inner half cycle, we threaded the
crochet with the abdominal suture and then took it out from the
body. Then we squeezed the scrotum, and after the pneumatosis
occurred at the groin area, we tightened the suture and knotted it
in the skin. After that, we completed the high ligation of the
hernias sac. Meanwhile, we detected the contralateral situation. If
the contralateral hernias existed, we would conduct a herniorrhaphy
at the same time. After the contralateral area was detected to be
without error, we pulled out the puncture needle and removed the
pneumoperitoneum to end the herniorrhaphy. Umbilical puncture holes
were routinely sutured with a stitch, and the bio-adhesive bound
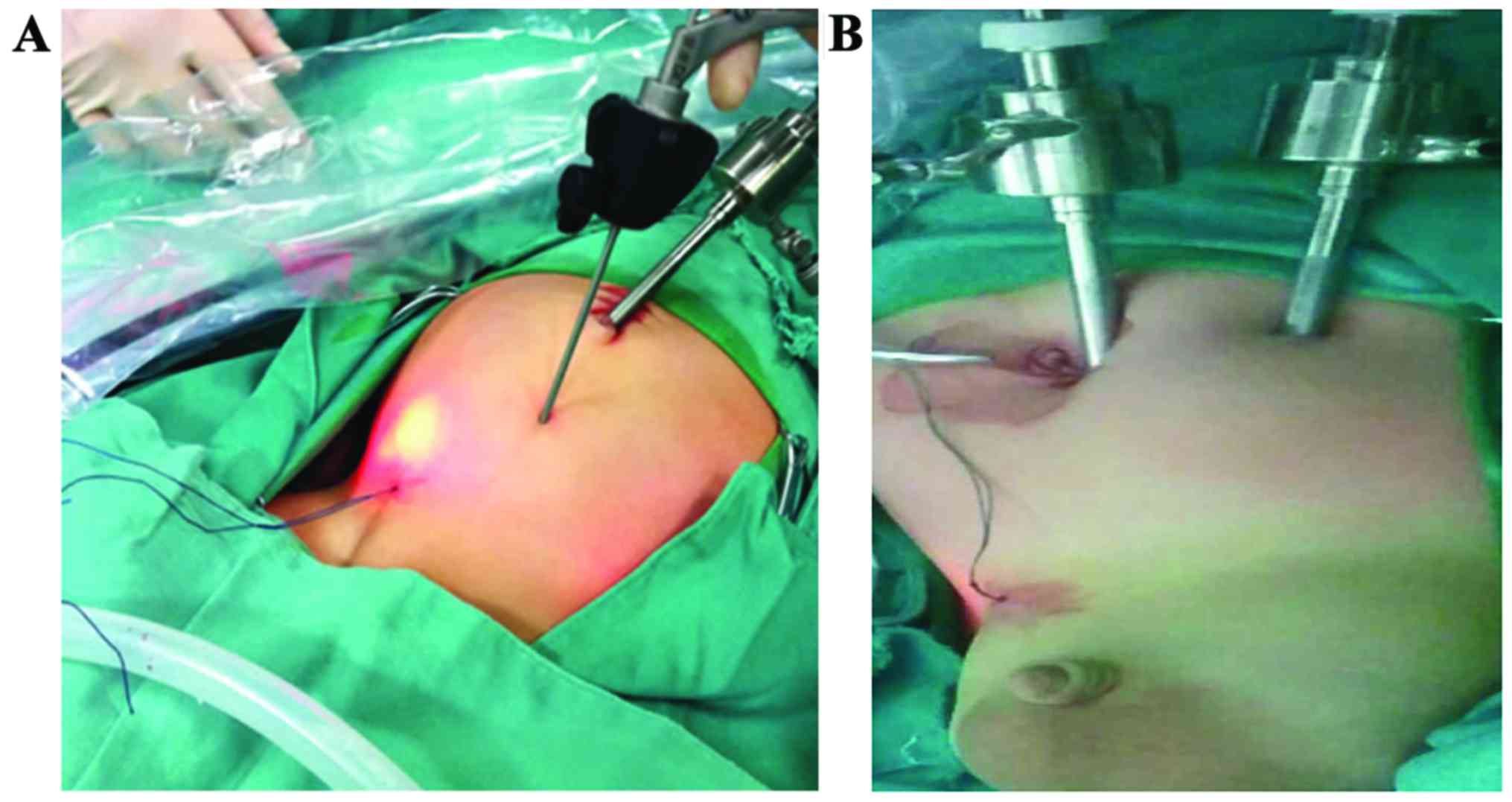
the skin incision (Fig. 2).
The DSLH
Routine disinfection and draping were conducted. A
0.5 cm incision on the umbilical region was taken. After the
establishment of pneumoperitoneum, the incision was inserted into
the 5 mm trocar and then into the laparoscope lens. Then another
0.5 cm incision on the contralateral rectus abdominis was made,
where a 5 mm trocar was inserted. A pair of operation forceps was
inserted to probe the abdominal cavity and bilateral inner ring.
Other operations were the same as those in the SSLH, and the
herniorrhaphy was concluded.
Statistical analysis
SPSS 17.0 (SPSS, Inc., Chicago, IL, USA) was used to
analyze the data. The measurement data were expressed as mean ± SD.
The independent two-sample t-test was conducted. The enumeration
data were detected by Chi-square test. P<0.05 was considered to
indicate a statistically significant diference.
Results
As shown in Table I,
among 1,010 children with inguinal hernias, there were 892 males
and 118 females, in which there were 727 children with inguinal
hernias at the right side and 283 children with inguinal hernias at
the left side. A total of 508 children were treated with SSLH using
needle instruments while 502 children underwent DSLH. There were no
significant statistical differences (P=0.446, 0.09 and 0.454,
respectively) between the two groups in terms of sex, age, surgical
site and other clinical data after comparisons, but these data were
comparable. The operation time, intraoperative blood loss, time of
off-bed and discharge time of the single-site group were
significantly lower than those of the traditional double-site
group, so the differences were statistically significant
(P<0.001, <0.001 and <0.01, respectively). In terms of
postoperative complications, as children in both groups were
operated by skilled surgeons, there were no serious complications
(P=0.249). There was 1 child with incision dehiscence in the
single-site group and 2 children in the traditional double-site
group. All children were followed up for 2 years. There was no
recurrence in the single-site group, but 2 children had recurrence
in the traditional double-site group. A total of 113 children were
detected with contralateral occult hernia in the single-site group
and 96 children in the traditional double-site group. The
difference between the two groups has no statistical significance
after the comparison (P=0.221). Intraoperative operations under
operations of the laparoscope are shown in Fig. 3 and the postoperative comparison of
effects is shown in Fig. 4.
Abdominal scars were obvious in the double-site group.
 | Table I.Comparisons of the clinical data of
children with inguinal hernias in the SSLH group using needle
instruments and the traditional double-site group. |
Table I.
Comparisons of the clinical data of
children with inguinal hernias in the SSLH group using needle
instruments and the traditional double-site group.
| Parameters | SSLH group using
needle instruments (n=508) | Traditional DSLH
group (n=502) | P-value |
|---|
| Age | 4.32±1.62 | 4.46±1.34 |
0.446 |
| Sex |
|
|
|
| Male | 440 (86.6%) | 452 (90%) |
0.090 |
|
Female | 68
(13.4%) | 50 (10%) |
|
| Position |
|
|
|
| Right
side | 371 (73.0%) | 356
(70.9%) |
0.454 |
| Left
side | 137 (27.0%) | 146
(29.1%) |
|
| Operation time
(min) | 6.33±1.56 | 8.57±2.26 |
<0.001 |
| Intraoperative blood
loss (ml) | 0.58±0.15 | 1.12±0.33 |
<0.001 |
| Time of off-bed
(h) |
|
|
|
|
<4 | 483 (95.1%) | 55
(11.0%) |
<0.001 |
| 4–24 | 25 (4.9%) | 447 (89.0%) |
|
| Discharge time
(days) | 1.23±0.16 | 1.58±0.49 |
0.003 |
| Complications | 2
(0.38%) | 5
(1.0%) |
0.249 |
| Puncture
infection | 1 (0.19%) | 1
(0.20%) |
|
| Incision
dehiscence | 1 (0.19%) | 2
(0.40%) |
|
| Recurrence | 0 2 (0.40%) |
|
|
| Appearance of
contralateral occult hernia | 113 (22.2%) | 96 (19.1%) |
0.221 |
Discussion
Laparoscopic herniorrhaphy in the treatment of
children with inguinal hernias has been gradually replacing the
traditional open high ligation of the hernias sac, which occupies
an indispensable position. At present, there is no uniform norm for
the inguinal hernias laparoscopic herniorrhaphy in China or other
countries, but as the open herniorrhaphy, has been developed on the
basis of the high ligation of the hernias sac combined with the
advantages of the laparoscopic technology. Present laparoscopic
herniorrhaphy methods and improved technologies exist in a wide
range, so how to safely and effectively complete a herniorrhaphy
with increasingly minimal traumas and no scars has become the new
focal point of study. Based on this concept, we made a miniature
needle instrument, which helps us operate the SSLH using the needle
instrument. In the present study, we compared the new operation
method SSLH using the needle instrument with the traditional DSLH
in the prognosis of children with inguinal hernias so as to
pinpoint the curative effect and safety of the SSLH using needle
instruments for children with inguinal hernias.
Results of our study showed that the operation time,
intraoperative blood loss, time of off-bed and discharge time of
the single-site group using needle instruments were significantly
lower than those of the traditional double-site group (8), and the differences were statistically
significant. As the needle instrument helped us quickly find the
hernia sac as well as the peritoneum and the suture clamped by the
needle holder, and reduced the time of placing a trocar and
stitching a puncture, the operation time in the single-site group
(6.33 min on average) was shorter than that in the double-site
group. In addition, children in the single-site group using needle
instruments could move after waking up from anesthesia, and were
discharged on the operation day without taking painkillers or
antibiotics, greatly reducing the hospital stays in children. The
umbilicus and linea alba approach of children: The needle
instrument was punctured in the linea alba of the umbilicus, there
appeared no muscle, nerve and vascular injury, and the bleeding was
significantly reduced. Besides, children felt no pain caused by
muscular traction and contraction, so it was easy for children to
recover, and the time of off-bed of children was significantly
shortened. As for complications, the SSLH using needle instruments
had generalities of the laparoscopic herniorrhaphy, so the
spermatic cord of the inner ring was not easy to be damaged under
the direct vision. This herniorrhaphy retained the integrity of the
inguinal canal, reduced the degree of nerve damage and effectively
avoided the hematoma of scrotum and the recurrent hernias caused by
neurocranial muscle paralysis. Due to children with low immunity
congenitally, puncture infection would occur in some children to a
certain degree and the incision dehiscence would occur in a very
small number of children if the disinfection of the intraoperative
umbilical incision was not strictly conducted and no antibiotics
were used after herniorrhaphy. Another advantage of laparoscopic
herniorrhaphy is that the contralateral occult hernia can be found
and treated at once during the herniorrhaphy. About 20% children in
the two groups were found to have contralateral occult hernia, and
this herniorrhaphy avoided the pain caused by the re-herniorrhaphy.
From the aesthetic aspects of herniorrhaphy, there was only a 5 mm
observation hole left in the umbilical region in the single-site
group using needle instruments, and there was basically no scar but
the skin color was deep on the linea alba pinhole, which achieves
the cosmetic results with no scar based on SSLH. Therefore, this
herniorrhaphy is better than the traditional DSLH.
The technological difficulty of SSLH is that there
is only the observation hole without the operation hole, but in
order to overcome this technical bottleneck, a number of scholars
attempted to improve new surgeries. Kimura et al (9) used port-closure techniques following
laparoscopic herniorrhaphies; Zhou et al (10) selected umbilical approach
herniorrhaphy, in which the umbilical cord incision was enlarged,
and the laparoscope and the operating forceps were inserted at the
same time; Shen et al (11)
jointly applied ureteroscopic mirror body and the operation hole to
conduct the herniorrhaphy, and moved the operation hole to the
umbilical region close to the observation hole so as to avoid the
appearance of scars. All these herniorrhaphies are not SSLH in the
true sense. Moreover, the inserting site of laparoscope is close to
that of the instrument, which results in the affection,
interference and collision between each other as well as the
existence of chopsticks effect. Difficulties also exist in this
difficult operation, high technical threshold and the need for
special equipment and expanded incision, which may also cause the
corresponding complications, so it is not easy to be promoted. The
single-site laparoscope can only puncture a 5 mm trocar hole on the
umbilical ring and only a pinhole in the linea alba on the
hypogastrium, so inserting a needle holder can help the operation
forceps to pull the peritoneum and suture, making the herniorrhaphy
operation simple and the learning curve short. This is more
consistent with the concept of minimally invasive herniorrhaphy and
easier to be popularized.
This study applied the improved SSLH using needle
instruments for children with inguinal hernias for the first time.
The curative efficacy of SSLH using needle instruments was better
than that of the traditional DSLH, and it produced no scars. The
SSLH is characterized by shorter operation time, fewer traumas,
less pain, faster recovery period, more consistent with the concept
of minimally invasive herniorrhaphy and easier to learn. Therefore,
we recommend that this new herniorrhaphy should be clinically
popularized and applied. However, longer-term curative efficacy
also requires support from multi-center and large-sample data and
longer-term follow-up.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Potts WJ, Riker WL and Lewis JE: The
treatment of inguinal hernia in infants and children. Ann Surg.
132:566–576. 1950. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Dallas T: Treatment of congenital infuinal
hernia. Ann Surg. 135:879–884. 1952. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Yang C, Zhang H, Pu J, Mei H, Zheng L and
Tong Q: Laparoscopic vs open herniorrhaphy in the management of
pediatric inguinal hernias: A systemic review and meta-analysis. J
Pediatr Surg. 46:1824–1834. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Montupet P and Esposito C: Laparoscopic
treatment of congenital inguinal hernias in children. J Pediatr
Surg. 34:420–423. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Zallen G and Glick PL: Laparoscopic
inversion and ligation inguinal hernia repair in girls. J
Laparoendosc Adv Surg Tech A. 17:143–145. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Tatekawa Y: Laparoscopic extracorporeal
ligation of hernia defects using an epidural needle and
preperitoneal hydrodissection. J Endourol. 26:474–477. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gilbert AI: An anatomic and functional
classification for the diagnosis and treatment of inguinal hernias.
Am J Surg. 157:331–333. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Liu SJ, Wang F, Zhu YL, Yang S, Shen YM,
Wang MG and Chen J: Analysis of minimally invasive SSLH using
needel instruments in the treatment of children with inguinal
hernias. Chin Dep Herniorrhaph Abdom Wall Hernias. 8:17–20.
2014.
|
|
9
|
Kimura T, Yamauchi K, Ihara Y, Sawai T,
Kosumi T and Yonekura T: Single-site laparoscopic herniorrhaphy
using needle instruments for inguinal hernias in children: A novel
technique. Surg Today. 42:100–103. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zhou X, Song D, Miao Q and Shan W:
Transumbilical endoscopic herniorrhaphy for completely enclosing
inguinal hernias in children. J Pediatr Surg. 46:2417–2420. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Shen W, Ji H, Lu G, Chen Z, Li L, Zhang H
and Pan J: A modified single-port technique for the minimally
invasive treatment of pediatric inguinal hernias with high ligation
of the vaginal process: The initial experience. Eur J Pediatr.
169:1207–1212. 2010. View Article : Google Scholar : PubMed/NCBI
|