Introduction
Blockade of the brachial plexus through an
interscalene approach has a relatively high success rate in
shoulder surgery (1–3). Ultrasound imaging of the brachial
plexus between the anterior and middle scalene muscles is feasible
(4), and it has been documented that
use of ultrasound improves the success rate and reduces the
prevalence of complications (5).
Furthermore, the site of injection may affect the spread of local
anesthetic (LA) (6), and a number of
studies comparing different approaches for nerve blocks have
documented that multiple injections of LA around the nerve result
in a higher prevalence of success and a shorter time of onset
compared with LA deposition at a single location (7–9).
Furthermore, the present authors have previously observed that
triple injection (TI) is necessary if LA is deposited inside the
paraneural sheath, and that the paraneurium ‘entraps’ LA molecules,
thereby ensuring circumferential spread around the interscalene
brachial plexus nerve (7).
Therefore, ultrasound-guided TI may increase the efficacy and
quality of interscalene brachial plexus blocks (IBPBs).
In the present study, a prospective, randomized,
observer-blinded trial was conducted to compare the efficacy and
safety of single injection (SI) and TI methods of IBPB for
arthroscopic shoulder surgery. The primary aims were to compare the
onset time of sensory and motor blocks and their distribution in
the radial, median, ulnar and axillary nerves, as well as the
duration of IBPBs. The secondary aims were to compare the
performance times, procedure-related pain, success rate and
prevalence of complications for the two methods.
Subjects and methods
Study subjects
A total of 111 patients undergoing arthroscopic
shoulder surgery between September and December 2015 at Subei
People's Hospital of Jiangsu Province (Yangzhou, China) were
included in the present study. The study protocol was approved by
the Ethics Review Board of the Clinical Medical College of Yangzhou
University (Yangzhou, China). All patients gave written informed
consent to participate in the study. The current trial is
registered in the Chinese Clinical Trial Registry
(ChiCTR-ICR-15007037).
The present study included patients presenting with
an American Society of Anesthesiologists (ASA) physical status of I
or II, aged ≥18 years and scheduled for elective arthroscopic
shoulder surgery. Patients with severe chronic obstructive
pulmonary disease, previous radiotherapy to the neck, coagulopathy
or a body mass index (BMI) >35 kg/m2 were excluded
from the present study. Patient characteristics are listed in
Table I. Patients were randomly
assigned to the SI (n=56) or TI (n=55) group.
 | Table I.Patient characteristics of the study
groups. |
Table I.
Patient characteristics of the study
groups.
| Variable | SI (n=56) | TI (n=55) | P-value |
|---|
| Age, years | 55.42±14.20 | 53.28±15.07 | 0.443 |
| Male/female | 29/27 | 26/29 | 0.706 |
| BMI,
kg/m2 | 26.71±6.89 | 27.13±7.02 | 0.751 |
| ASA physical status
(I/II) | 30/26 | 31/24 | 0.849 |
Interscalene blockade
Patients adopted a supine position with the head
turned 45° to the non-operative side. An electrocardiograph was
performed, and pulse oximetry and blood pressure monitoring was
conducted as part of routine procedure.
Standard monitoring (pulse oximeter,
electrocardiogram, noninvasive blood pressure) was performed during
the study and oxygen (2 l/min) was supplied via a nasal cannula,
and patients were intravenously administered with midazolam
(0.01–0.03 mg/kg, Jiangsu Nhwa Pharmaceutical Co., Ltd., Jiangsu,
China). A portable ultrasound machine (M-turbo; Fujifilm SonoSite,
Inc., Bothell, WA, USA) with a 6–13-MHz linear probe was used. A 50
mm, 22 G stimulating needle (Stimuplex; B. Braun Medical,
Bethlehem, PA, USA) was used to administer blocks. Blocks were
performed by three anaesthesiologists with substantial experience
of this method.
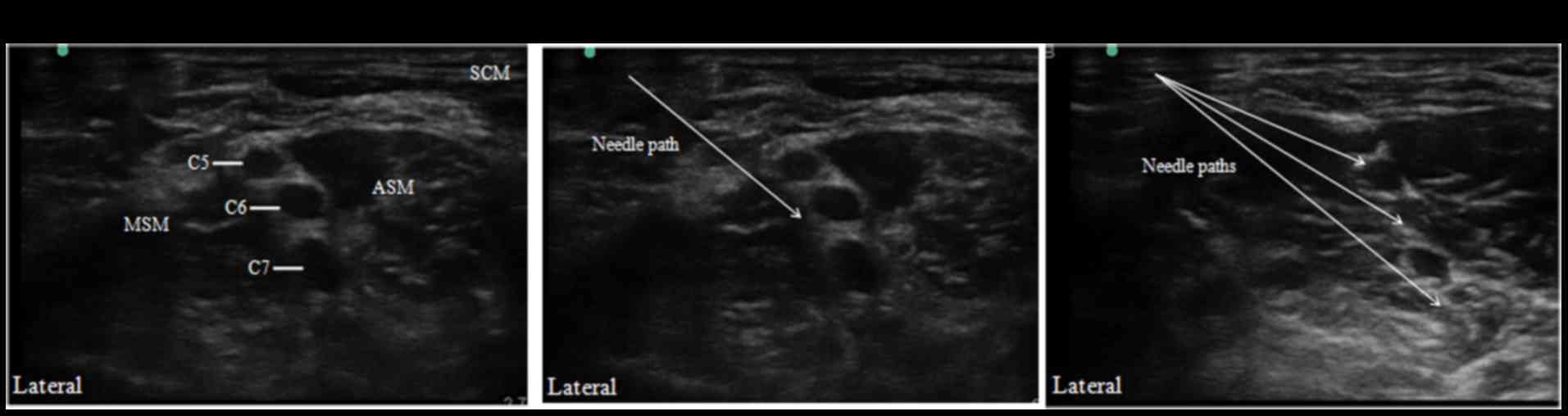
Using an aseptic technique, the interscalene area
was imaged to obtain a clear view of the brachial plexus (Fig. 1A). Roots of C5, C6, and C7 were
identified according to the description by Spence et al
(10). Following injection of the
skin with 1–2 ml of 1% lidocaine (Jiangsu Nhwa Pharmaceutical Co.,
Ltd.), the needle was introduced from a lateral-to-medial
direction. For the SI group, the needle-tip was positioned in the
middle section of the interscalene brachial plexus (Fig. 1B), and 15 ml of the LA 1% ropivacaine
(Yichang Humanwell Pharmaceutical Company, Ltd., Yichang, China)
was incrementally injected. In the TI group, 1% ropivacaine was
injected in three aliquots of 5 ml. Aliquots were deposited in the
upper-, middle, and lower-third of the interscalene brachial plexus
(Fig. 1C).
Assessment of blockade
Evaluation of nerve blockades was performed by a
separate anesthesiologist to those who administered the blocks. The
primary outcome was the onset of sensory and motor blocks of the
four nerves (radial, median, ulnar and axillary) assessed at 5 min
intervals for 30 min post-injection.
Sensory blockade was defined as a loss in pinprick
sensation in the territories of the radial, median, ulnar and
axillary nerves, with an identical stimulus delivered to the
opposite side, as a control. Sensory blockade was scored according
to a four-point scale (identical sharpness = 3; reduced sharpness =
2; sensation present but not sharp = 1; sensation absent = 0).
Motor blockade was evaluated according to a modified
scale of that used by Kapral et al (Table II) (11). The scale was based on thumb abduction
(radial nerve), thumb opposition (median nerve), forearm
supination/pronation (radial and median nerves), thumb adduction
(ulnar nerve), and abduction of the upper arm (axillary nerve).
 | Table II.Rating scale for muscle force. |
Table II.
Rating scale for muscle force.
| Rating | Description |
|---|
| 6 | Normal muscle
force |
| 5 | Slightly reduced
muscle force |
| 4 | Greatly reduced
muscle force |
| 3 | Slightly impaired
mobility |
| 2 | Greatly impaired
mobility |
| 1 | Near complete
paralysis |
| 0 | Complete
paralysis |
Blockade duration was determined 24 h following
nerve blockade by a research assistant blinded to the study
protocol. Patients were instructed to record on a pre-printed card
the time at which they were first able to flex their elbow, and
this was defined as the endpoint of the block. Patients were
instructed to attempt to flex their arm every 30 min following
discharge from the operating room. Arm flexion at the elbow was
chosen as the least ambiguous test to evaluate motor function
during follow-up. Similarly, the first occurrence of pain as
perceived by the patient (‘When did you first start feeling the
pain?’) was used as a proxy for the return of sensory function.
Blockade performance time was defined as the time
between the first ultrasound scan and removal of the needle at the
end of the block. A successful blockade was determined as one with
a good primary outcome (as defined above). An adequate surgical
blockade was defined as one able to tolerate a simulated surgical
stimulus (forceps pinching the prospective surgical area) at 30 min
post-injection. Unexpected vascular punctures, symptomatic
hemidiaphragmatic paresis, Horner syndrome, pneumothorax or
neurological deficits were recorded. Pain intensity related to the
procedure was assessed at the end of blockade using an 11-point
verbal numerical rating scale (NRS) from 0 (no pain) to 10 (worst
imaginable pain) by an observer blinded to the study protocol.
Statistical analysis
SPSS v. 15 (SPSS, Inc., Chicago, IL, USA) was used
to perform all statistical analyses. A pilot study was conducted on
20 patients to estimate the prevalence of a satisfactory sensory
block. A satisfactory block was found to be 75% at 30 min
post-injection using an SI (data not shown). It was hypothesized
that multiple injections may increase this proportion to 90%. A
calculated sample size of 111 patients per group was required for a
statistical power of 0.90 and type-I error of 0.05. Categorical
variables, including the proportion of patients with successful
sensory and motor blocks at 5, 10, 15, 20, 25 and 30 min, were
expressed as percentages. Continuous variables, including age and
BMI, were expressed as the mean + standard deviation. The
χ2 test was used to evaluate categorical variables
between the two groups, and the Student's t-test was used to
compare continuous variables. Successful sensory and motor blocks
at different times were compared using a Friedman's
repeated-measures analysis of variance on ranks for within-group
comparisons, and a Kruskal-Wallis one-way analysis of variance on
ranks for intergroup comparisons. The P-value was calibrated using
the Benjamini and Hochberg method. Kaplan-Meier life-table analysis
was used to analyze the duration of sensory and motor blocks.
P<0.05 was considered to indicate a statistically significant
difference.
Results
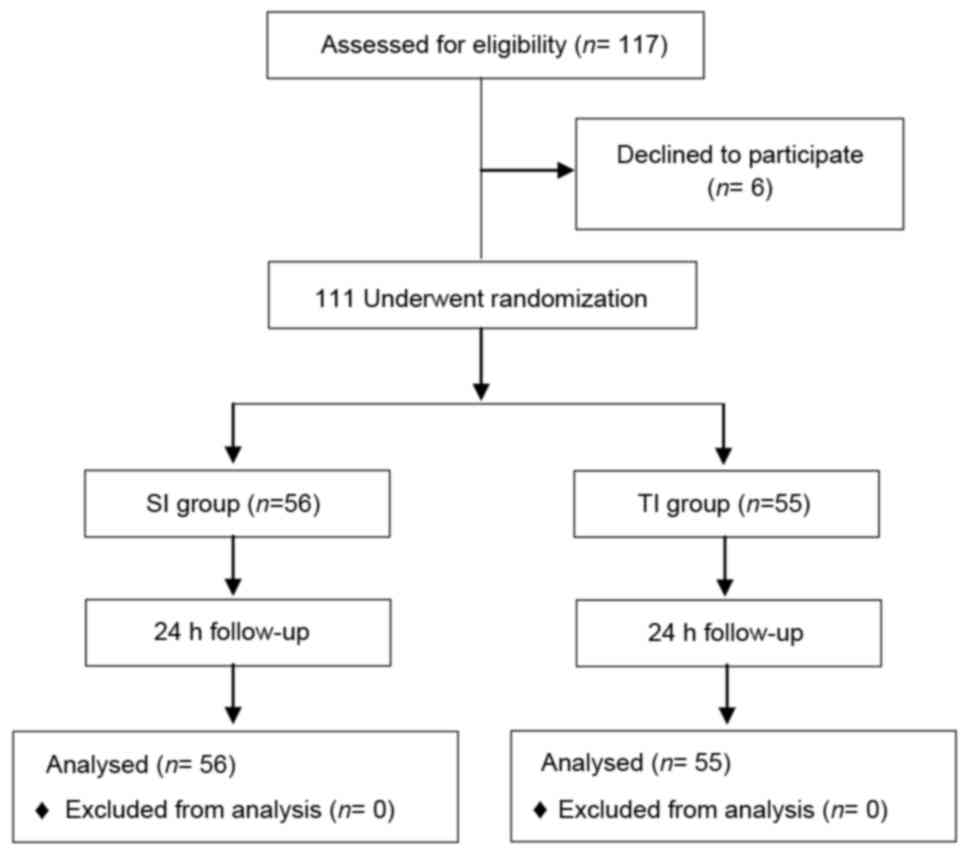
A total of 117 patients were enrolled, and 111
patients completed the study (Fig.
2). Age, sex, BMI or ASA physical status did not differ
significantly between the SI and TI groups (Table I).
Success of individual sensory and
motor blocks
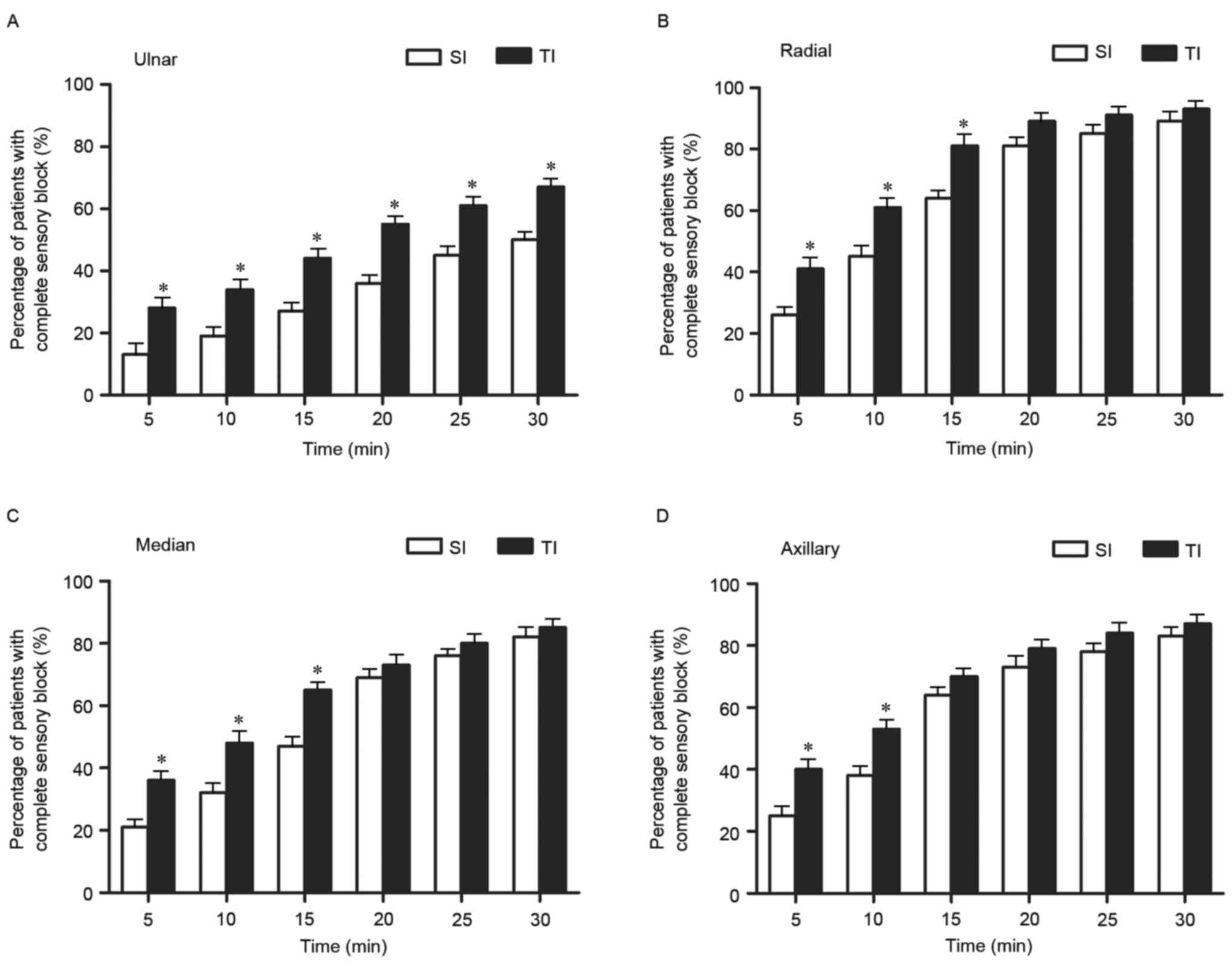
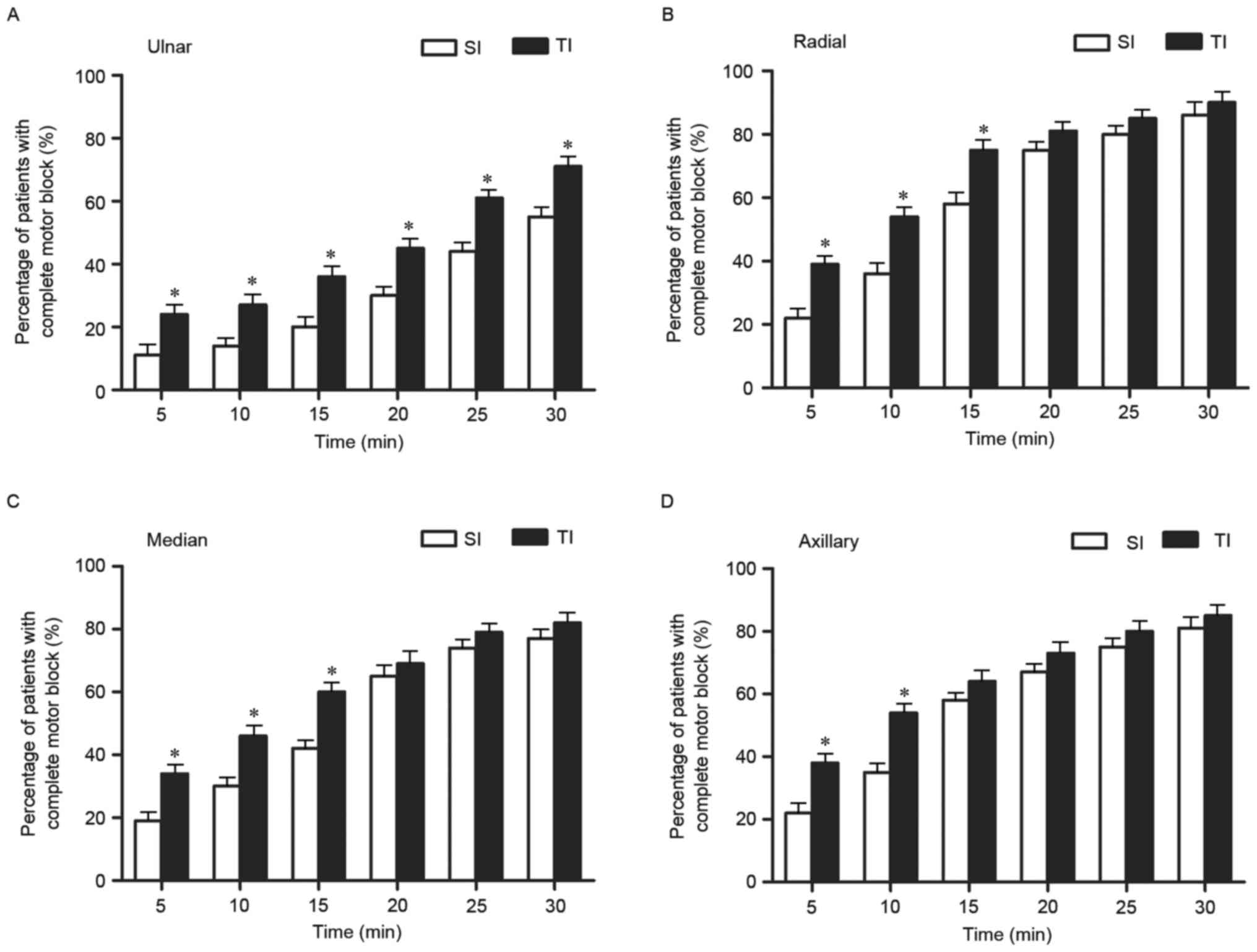
The success rates for sensory and motor blocks in
the ulnar, radial, median and axillary nerves differed between the
SI and TI groups (Figs. 3 and
4). The success rates for sensory
and motor blocks of the ulnar nerve from 5–30 min post-injection
were significantly higher in the TI group compared with the SI
group (P<0.05; Figs. 3A and
4A). The prevalence of complete
sensory and motor blocks of the radial and median nerves was
significantly higher in the TI group at 5, 10 and 15 min
(P<0.05; Figs. 3B and C, and
4B and C); however, they did not
differ significantly at 20, 25 or 30 min post-injection. The
prevalence of complete sensory and motor blocks of the axillary
nerve was significantly greater in the TI group at 5 and 10 min
post-injection (P<0.05), while no significant difference was
observed between the SI and TI groups at 15, 20, 25 or 30 min
post-injection (Figs. 3D and
4D).
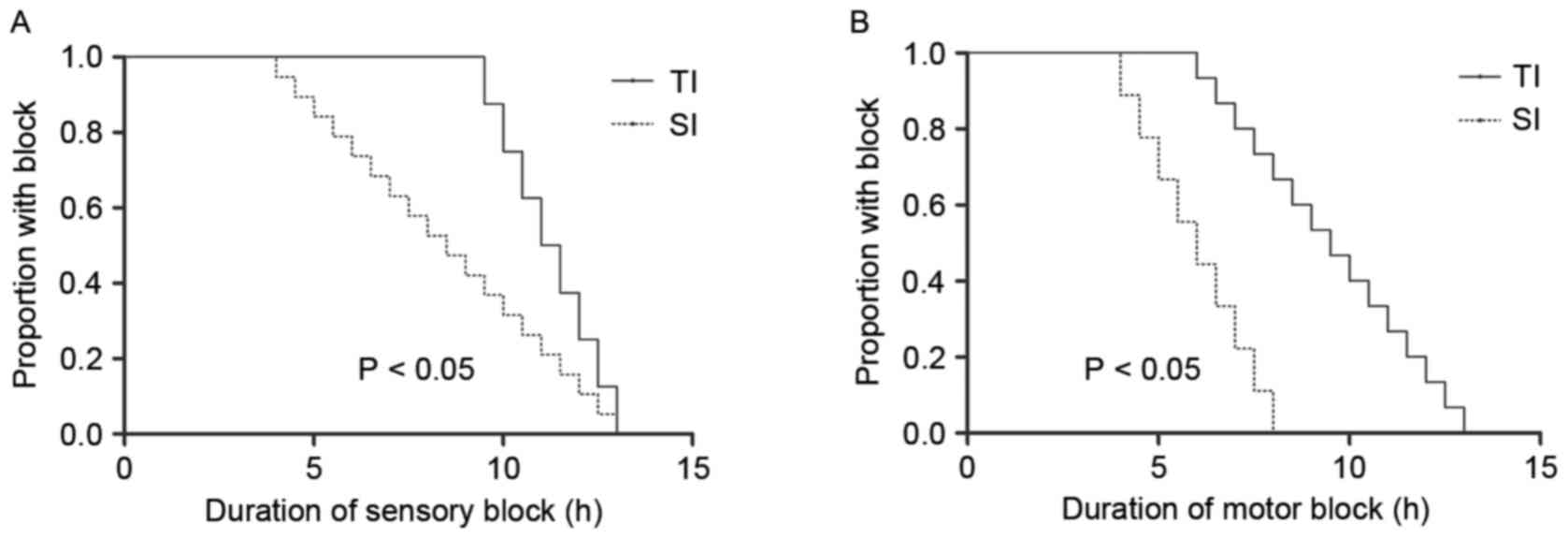
TI enhanced the duration of
blockade
Sensation or strength did not differ significantly
between the two groups at baseline testing. However, the duration
of sensory and motor blocks differed significantly between the
groups (P<0.05; Fig. 5). Patients
in the TI group described a greater sensory block to pain,
beginning at 30 min following the interscalene blockade, which
persisted throughout the 17 h assessment period (Fig. 5A). Similarly, motor blockade in the
TI group had a longer duration compared with the SI group (Fig. 5B).
Other secondary outcomes
The blockade performance time was significantly
longer in the TI group compared with the SI group (P<0.001;
Table III). SI and TI methods
resulted in a similar rate of success at 30 min. There were no
significant differences in the prevalence of unexpected vascular
punctures or Horner syndrome, and symptomatic hemidiaphragmatic
paresis, pneumothorax or neurological deficits were not observed.
No significant differences were observed in the NRS results for
pain during the procedure (Table
III).
 | Table III.Block characteristics and outcome of
the two study groups. |
Table III.
Block characteristics and outcome of
the two study groups.
| Characteristic | SI (n=56) | TI (n=55) | P-value |
|---|
| Performance time,
min | 4.15±2.21 | 7.22±2.46 | <0.001 |
| Success | 49 (88%) | 50 (91%) |
0.761 |
| Vascular
puncture | 1 | 2 |
|
| Horner syndrome | 2 | 2 |
|
| Symptomatic
hemidiaphragmatic paresis | 0 | 0 |
|
| Pneumothorax | 0 | 0 |
|
| Neurological
deficits | 0 | 0 |
|
| NRS values for
procedural pain | 2.5 (0–7) | 3 (0–8) |
0.082 |
Discussion
In the present study, the SI and TI methods of
ultrasound-guided SI and TI interscalene blocks were compared. The
TI method exhibited a faster onset post-injection compared to the
SI method, and patients in the TI group experienced longer sensory
and motor blocks compared with the SI group. However, there was no
significant difference in the success rate of surgical anesthesia
at 30 min post-injection.
There have been conflicting reports regarding the
quality of nerve blockade with TI compared with SI. A recent
systematic review of randomized controlled trials comparing
ultrasound-guided TI and SI for supraclavicular brachial plexus
blockade suggested that TI may provide a modest improvement in the
onset and quality of blockade (7).
In the present study, no significant differences were observed in
the success rate of the two methods. However, to the best of our
knowledge, this is the first study to focus on the onset of sensory
and motor blocks of four nerves, as well as the duration of
blockade as a primary outcome.
The TI group surpassed the SI group in achieving
sensory and motor blocks at 5 min intervals for the first 10 min. A
paraneural sheath surrounds the brachial plexus as a thin membrane
(10,12), and it is possible that the paraneural
sheath precludes the need for direct circumferential injection. As
the space between nerve roots is limited, the area becomes
saturated with LA, and multiple injections force incoming LA
molecules to find alternate paths of less resistance. In time, this
phenomenon results in the indirect spread of LA around the roots of
C5, C6, and C7 (7). This mechanism
may explain why, initially, the TI method provided a shorter time
of onset and more successful blocks in the first 10 min. In the
present study, sensory and motor blocks of the ulnar nerve were
significantly more effective with TI compared with SI at all time
points. The first injection of the TI was deep and potentially
close to the lower trunk. Accordingly, the subsequent difference in
the success of the ulnar nerve blockade may have eliminated the
need for further injections, as the initial deep injection
typically targets the lower region of the brachial plexus that
gives origin to the ulnar nerve (13,14).
Another notable observation in the present study was
that the duration of blockade was prolonged in the TI group
compared with the SI group. This may have been due to reduced
systemic uptake of LA in the TI group, due to more LA being
contained within the brachial plexus sheath, thus increasing the
reservoir volume of LA solution (10). Franco et al (12) described the interior of the sheath
surrounding the neuronal tissue as a combination of loose
connective tissue and fat, with few veins running along the sheath
interior. These observations potentially explain the results of the
present study, as there may have been decreased systemic absorption
of LA in the TI group due to reduced vascularity on the interior of
the sheath.
In conclusion, and in accordance with previous work
(7,15,16), no
significant difference was observed in the success rates of the SI
and multiple injection methods. However, the TI method for IBPB
resulted in improved onset time and more complete sensory and motor
blocks at 10 min compared with the SI method. Furthermore, the TI
method deposited LA in the interscalene brachial plexus more
caudally than in the SI method, which may have resulted in greater
distal distribution of anesthesia and a higher blockade success in
the ulnar nerve. The TI method also achieved a longer blockade
duration than the SI method, and was more effective in producing
postoperative analgesia. The results of the present study also
suggest that the TI method may be more suitable for IBPB than the
SI method due to its faster onset time and persistent analgesic
effect.
Acknowledgements
The present study was supported by the National
Natural Science Foundation of China (grant no. 81500947), the
Jiangsu Provincial Commission of Health and Family Planning
Research Project (project no. H2017059) and the Jiangsu Province
Youth Medical Talent Project (grant no. QNRC2016338).
References
|
1
|
Desmet M, Vanneste B, Reynvoet M, Van
Cauwelaert J, Verhelst L, Pottel H, Missant C and Van de Velde M: A
randomised controlled trial of intravenous dexamethasone combined
with interscalene brachial plexus blockade for shoulder surgery.
Anaesthesia. 70:1180–1185. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Fritsch G, Danninger T, Allerberger K,
Tsodikov A, Felder TK, Kapeller M, Gerner P and Brummett CM:
Dexmedetomidine added to ropivacaine extends the duration of
interscalene brachial plexus blocks for elective shoulder surgery
when compared with ropivacaine alone: A single-center, prospective,
triple-blind, randomized controlled trial. Reg Anesth Pain Med.
39:37–47. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Woo JH, Kim YJ, Kim DY and Cho S:
Dose-dependency of dexamethasone on the analgesic effect of
interscalene block for arthroscopic shoulder surgery using
ropivacaine 0.5%: A randomised controlled trial. Eur J
Anaesthesiol. 32:650–655. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Tsui BC and Lou L: Learning the
‘traceback’ approach for interscalene block. Anaesthesia. 69:83–85.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Danelli G, Bonarelli S, Tognu A, Tognú A,
Ghisi D, Fanelli A, Biondini S, Moschini E and Fanelli G:
Prospective randomized comparison of ultrasound-guided and
neurostimulation techniques for continuous interscalene brachial
plexus block in patients undergoing coracoacromial ligament repair.
Br J Anaesth. 108:1006–1010. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Bowens C Jr, Gupta RK, O'Byrne WT,
Schildcrout JS, Shi Y, Hawkins JJ, Michaels DR and Berry JM:
Selective local anesthetic placement using ultrasound guidance and
neurostimulation for infraclavicular brachial plexus block. Anesth
Analg. 110:1480–1485. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Arab SA, Alharbi MK, Nada EM, Alrefai DA
and Mowafi HA: Ultrasound-guided supraclavicular brachial plexus
block: Single versus triple injection technique for upper limb
arteriovenous access surgery. Anesth Analg. 118:1120–1125. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Tiyaprasertkul W, Bernucci F, González AP,
Leurcharusmee P, Yazer MS, Techasuk W, Arnuntasupakul V, de la
Garza DC, Finlayson RJ and Tran DQ: A Randomized comparison between
single- and triple-injection subparaneural popliteal sciatic nerve
block. Reg Anesth Pain Med. 40:315–320. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yamamoto H, Sakura S, Wada M and Shido A:
A prospective, randomized comparison between single- and
multiple-injection techniques for ultrasound-guided subgluteal
sciatic nerve block. Anesth Analg. 119:1442–1448. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Spence BC, Beach ML, Gallagher JD and
Sites BD: Ultrasound-guided interscalene blocks: Understanding
where to inject the local anaesthetic. Anaesthesia. 66:509–514.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kapral S, Krafft P, Eibenberger K,
Fitzgerald R, Gosch M and Weinstabl C: Ultrasound-guided
supraclavicular approach for regional anesthesia of the brachial
plexus. Anesth Analg. 78:507–513. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Franco CD, Rahman A, Voronov G, Kerns JM,
Beck RJ and Buckenmaier CC III: Gross anatomy of the brachial
plexus sheath in human cadavers. Reg Anesth Pain Med. 33:64–69.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Bloc S, Rontes O, Mercadal L and Delbos A:
Low approach to interscalene brachial plexus block: Safer under
ultrasound guidance. Anesth Analg. 113:1282–1283. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kim JH, Chen J, Bennett H, Lesser JB,
Resta-Flarer F, Barczewska-Hillel A, Byrnes P and Santos AC: A low
approach to interscalene brachial plexus block results in more
distal spread of sensory-motor coverage compared to the
conventional approach. Anesth Analg. 112:987–989. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Fredrickson MJ, Wolstencroft P, Kejriwal
R, Yoon A, Boland MR and Chinchanwala S: Single versus triple
injection ultrasound-guided infraclavicular block: Confirmation of
the effectiveness of the single injection technique. Anesth Analg.
111:1325–1327. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Tran DQ, Bertini P, Zaouter C, Muñoz L and
Finlayson RJ: A prospective, randomized comparison between single-
and double-injection ultrasound-guided infraclavicular brachial
plexus block. Reg Anesth Pain Med. 35:16–21. 2010. View Article : Google Scholar : PubMed/NCBI
|