|
1
|
Marx RE: Platelet-rich plasma (PRP): What
is PRP and what is not PRP? Implants Dent. 10:225–228. 2001.
View Article : Google Scholar
|
|
2
|
Arnoczky SP, Delos D and Rodeo SA: What is
platelet-rich plasma? Oper Tech Sports Med. 19:142–148. 2011.
View Article : Google Scholar
|
|
3
|
Blair P and Flaumenhaft R: Platelet
alpha-granules: Basic biology and clinical correlates. Blood Rev.
23:177–189. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Leslie M: Cell biology. Beyond clotting:
The powers of platelets. Science. 328:562–564. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Knezevic NN, Candido KD, Desai R and Kaye
AD: Is platelet-rich plasma a future therapy in pain management?
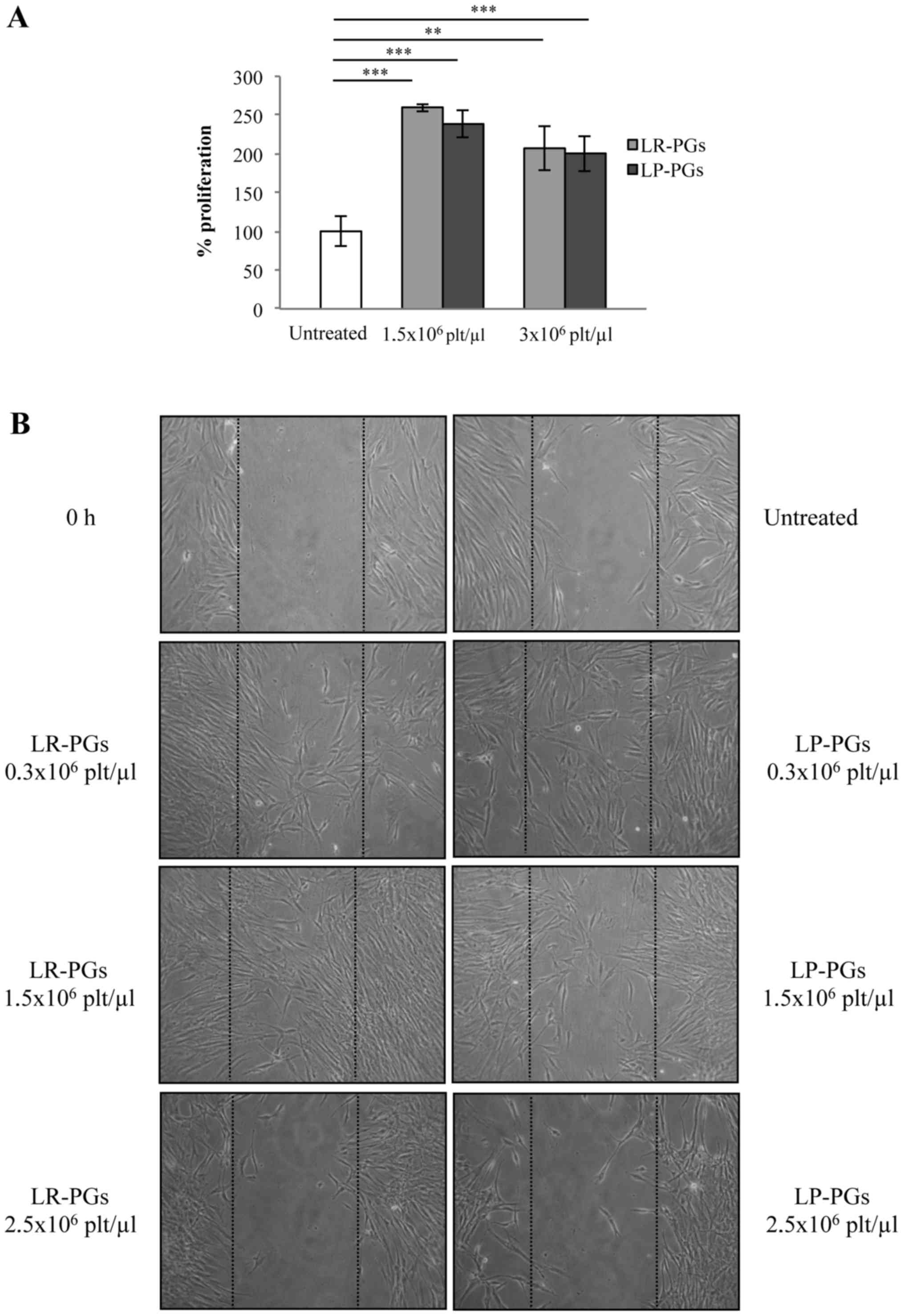
Med Clin North Am. 100:199–217. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Lacci KM and Dardik A: Platelet-rich
plasma: Support for its use in wound healing. Yale J Biol Med.
83:1–9. 2010.PubMed/NCBI
|
|
7
|
Mihaylova Z, Mitev V, Stanimirov P, Isaeva
A, Gateva N and Ishkitiev N: Use of platelet concentrates in oral
and maxillofacial surgery: An overview. Acta Odontol Scand.
75:1–11. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Fréchette JP, Martineau I and Gagnon G:
Platelet-rich plasmas: Growth factor content and roles in wound
healing. J Dent Res. 84:434–439. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
van der Meer PF, Seghatchian J and Marks
DC: Quality standards, safety and efficacy of blood-derived serum
eye drops: A review. Transfus Apher Sci. 54:164–167. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Hsu WK, Mishra A, Rodeo SR, Fu F, Terry
MA, Randelli P, Canale ST and Kelly FB: Platelet-rich plasma in
orthopaedic applications: Evidence-based recommendations for
treatment. J Am Acad Orthop Surg. 21:739–748. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lee KS: Platelet-rich plasma injection.
Semin Musculoskelet Radiol. 17:91–98. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Rughetti A, Giusti I, D'Ascenzo S, Leocata
P, Carta G, Pavan A, Dell'Orso L and Dolo V: Platelet gel-released
supernatant modulates the angiogenic capability of human
endothelial cells. Blood Transfus. 6:12–17. 2008.PubMed/NCBI
|
|
13
|
Giusti I, Rughetti A, D'Ascenzo S,
Millimaggi D, Pavan A, Dell'Orso L and Dolo V: Identification of an
optimal concentration of platelet gel for promoting angiogenesis in
human endothelial cells. Transfusion. 49:771–778. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Giusti I, Rughetti A, D'Ascenzo S, Di
Stefano G, Nanni MR, Millimaggi D, Dell'orso L and Dolo V: The
effects of platelet gel-released supernatant on human fibroblasts.
Wound Repair Regen. 21:300–308. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Cross JA, Cole BJ, Spatny KP, Sundman E,
Romeo AA, Nicholson GP, Wagner B and Fortier LA: Leukocyte-reduced
platelet-rich plasma normalizes matrix metabolism in torn human
rotator cuff tendons. Am J Sports Med. 43:2898–2906. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Dohan Ehrenfest DM, Bielecki T, Mishra A,
Borzini P, Inchingolo F, Sammartino G, Rasmusson L and Evert PA: In
search of a consensus terminology in the field of platelet
concentrates for surgical use: Platelet-rich plasma (PRP),
platelet-rich fibrin (PRF), fibrin gel polymerization and
leukocytes. Curr Pharm Biotechnol. 13:1131–1137. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Zhou Y, Zhang J, Wu H, Hogan MV and Wang
JH: The differential effects of leukocyte-containing and pure
platelet-rich plasma (PRP) on tendon stem/progenitor
cells-implications of PRP application for the clinical treatment of
tendon injuries. Stem Cell Res Ther. 6:1732015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Duif C, Vogel T, Topcuoglu F, Spyrou G,
von Schulze Pellengahr C and Lahner M: Does intraoperative
application of leukocyte-poor platelet-rich plasma during
arthroscopy for knee degeneration affect postoperative pain,
function and quality of life? A 12-month randomized controlled
double-blind trial. Arch Orthop Trauma Surg. 135:971–977. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Moojen DJ, Everts PA, Schure RM,
Overdevest EP, van Zundert A, Knape JT, Castelein RM, Creemers LB
and Dhert WJ: Antimicrobial activity of platelet-leukocyte gel
against Staphylococcus aureus. J Orthop Res. 26:404–410. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Mariani E, Canella V, Berlingeri A, Bielli
A, Cattini L, Landini MP, Kon E, Marcacci M, Di Matteo B and
Filardo G: Leukocyte presence does not increase microbicidal
activity of Platelet-rich Plasma in vitro. BMC Microbiol.
15:1492015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Dohan Ehrenfest DM, Bielecki T, Jimbo R,
Barbé G, Del Corso M, Inchingolo F and Sammartino G: Do the fibrin
architecture and leukocyte content influence the growth factor
release of platelet concentrates? An evidence-based answer
comparing a pure platelet-rich plasma (P-PRP) gel and a leukocyte-
and platelet-rich fibrin (L-PRF). Curr Pharm Biotechnol.
13:1145–1152. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Dragoo JL, Braun HJ, Durham JL, Ridley BA,
Odegaard JI, Luong R and Arnoczky SP: Comparison of the acute
inflammatory response of two commercial platelet-rich plasma
systems in healthy rabbit tendons. Am J Sports Med. 40:1274–1281.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Hasty KA, Pourmotabbed TF, Goldberg GI,
Thompson JP, Spinella DG, Stevens RM and Mainardi CL: Human
neutrophil collagenase: A distinct gene product with homology to
other matrix metalloproteinases. J Biol Chem. 265:11421–11424.
1990.PubMed/NCBI
|
|
24
|
McCarrel TM, Minas T and Fortier LA:
Optimization of leukocyte concentration in platelet rich plasma for
the treatment of tendinopathy. J Bone Joint Surg Am.
94:e143(18)2012. View Article : Google Scholar
|
|
25
|
Yin WJ, Xu HT, Sheng JG, An ZQ, Guo SC,
Xie XT and Zhang CQ: Advantages of pure platelet-rich plasma
compared with leukocyte- and platelet-rich plasma in treating
rabbit knee osteoarthritis. Med Sci Monit. 22:1280–1290. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Filardo G, Kon E, Pereira Ruiz MT, Vaccaro
F, Guitaldi R, Di Martino A, Cenacchi A, Fornasari PM and Marcacci
M: Platelet-rich plasma intra-articular injections for cartilage
degeneration and osteoarthritis: Single-vs. double-spinning
approach. Knee Surg Sports Traumatol Arthrosc. 20:2082–2091. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Riboh JC, Saltzman BM, Yanke AB, Fortier L
and Cole BJ: Effect of leukocyte concentration on the efficacy of
platelet rich plasma in the treatment of knee osteoarthritis. Am J
Sports Med. 44:792–800. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Diegelmann RF and Evans MC: Wound healing:
An overview of acute, fibrotic and delayed healing. Front Biosci.
9:283–289. 2004. View
Article : Google Scholar : PubMed/NCBI
|
|
29
|
Tzeng DY, Deuel TF, Huang JS and Baehner
RL: Platelet-derived growth factor promotes human peripheral
monocyte activation. Blood. 66:179–183. 1985.PubMed/NCBI
|
|
30
|
Elstad MR, McIntyre TM, Prescott SM and
Zimmerman GA: The interaction of leukocytes with platelets in blood
coagulation. Curr Opin Hematol. 2:47–54. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Grazul-Bilska AT, Johnson ML, Bilski JJ,
Redmer DA, Reynolds LP, Abdullah A and Abdullah KM: Wound healing:
The role of growth factors. Drugs Today (Barc). 39:787–800. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Giusti I, D'Ascenzo S, Mancò A, Di Stefano
G, Di Francesco M, Rughetti A, Dal Mas A, Properzi G, Calvisi V and
Dolo V: Platelet concentration in platelet-rich plasma affects
tenocyte behavior in vitro. Biomed Res Int. 2014:6308702014.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Granelli-Piperno A, Vassalli JD and Reich
E: Secretion of plasminogen activator by human polymorphonuclear
leukocytes. Modulation by glucocorticoids and other effectors. J
Exp Med. 146:1693–1706. 1977. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Salamonsen LA and Lathbury LJ: Endometrial
leukocytes and menstruation. Hum Reprod Update. 6:16–27. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Xue M, Thompson PJ, Clifton-Bligh R,
Fulcher G, Gallery ED and Jackson C: Leukocyte matrix
metalloproteinase-9 is elevated and contributes to lymphocyte
activation in type I diabetes. Int J Biochem Cell Biol.
37:2406–2416. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Hoeben A, Landuyt B, Highley MS, Wildiers
H, Van Oosterom AT and DeBruijn EA: Vascular endothelial growth
factor and angiogenesis. Pharmacol Rev. 56:549–580. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Soto-Pantoja DR, Shih HB, Maxhimer JB,
Cook KL, Ghosh A, Isenberg JS and Roberts DD: Thrombospondin-1 and
CD47 signaling regulate healing of thermal injury in mice. Matrix
Biol. 37:25–34. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Blanco-Mezquita JT, Hutcheon AE and Zieske
JD: Role of thrombospondin-1 in repair of penetrating corneal
wounds. Invest Ophthalmol Vis Sci. 54:6262–6268. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Laato M, Heino J, Gerdin B, Kähäri VM and
Niinikoski J: Interferon-gamma-induced inhibition of wound healing
in vivo and in vitro. Ann Chir Gynaecol. 90 Suppl 205:S19–S23.
2001.
|
|
40
|
Martínez CE, Smith PC and Palma Alvarado
VA: The influence of platelet-derived products on angiogenesis and
tissue repair: A concise update. Front Physiol. 6:2902015.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Penn JW, Grobbelaar AO and Rolfe KJ: The
role of the TGF-β family in wound healing, burns and scarring: A
review. Int J Burns Trauma. 2:18–28. 2012.PubMed/NCBI
|
|
42
|
Rozman P and Bolta Z: Use of platelet
growth factors in treating wounds and soft-tissue injuries. Acta
Dermatovenerol Alp Pannonica Adriat. 16:156–165. 2007.PubMed/NCBI
|