Introduction
Osteoarthritis (OA) is the most common form of
arthritis and a major cause of reduced activity and disability,
with an increased incidence after 65 years of age, which is
characterized by progressive cartilage degradation (1–3). The
primary aims of treatments for OA are to reduce the pain and
disability experienced by patients, thus improving quality of life.
Various medications, including analgesics, non-steroidal
anti-inflammatories, platelet-rich plasma and steroids, are used in
combination with physical therapy and/or surgery to treat those
with OA (4). However, novel
treatments to prevent chondrocyte degeneration are required, as
current treatments only alleviate symptoms of OA and do not tackle
the underlying causes of the disease (5). In addition to analgesics, non-steroidal
anti-inflammatories, platelet-rich plasma and steroids,
intra-articular injections of hyaluronic acid (HA), a slow-acting
chondroprotective agent, are frequently administered to patients
with OA (5,6). HA has a more prolonged effect and
avoids several of the side effects associated with conventional OA
treatment, including gastrointestinal toxicity or increased risk of
the cardiovascular events (4,7,8).
HA is a long chain polysaccharide present in loose
connective tissue, skin, the eyes and synovial fluid (4,7,9). HA is concentrated at the surface of the
articular cartilage and the superficial layers of the synovial
membrane and forms a semi-permeable barrier between the synovial
fluid and cartilage. Marked decreases in HA concentration is
associated with the onset of OA (4,7). In
pathological conditions, the molecular weight (MW) of HA also
decreases, which increases the cartilage mechanical load, thus
inducing damage of the cartilage (1,9). The
administration of HA was previously determined to reduce
chondrocyte apoptosis rate in patients with OA (10). The role of HA in OA remains unclear;
however, it may promote cell proliferation and pericellular matrix
formation (4,7,11).
In the present study, the effect of different MWs of
HA on the proliferation of chondrocytes, as well as the expression
of collagen type II (COL2A1), hypoxia-inducible factor 1α (HIF-1α)
and chondroadherin (CHAD) in chondrocytes was investigated. To the
best of our knowledge, the current study is the first to determine
the effects of HA on the expression of HIF-1 and CHAD. Impairment
of anabolic and catabolic processes is common features of OA. In
healthy cartilage, the presence of COL2A1 is a marker of anabolism
(5). The COL2A1 gene encodes
an important cartilage-specific matrix protein and its expression
is regulated by transcription factors, including SOX9 and
transforming growth factor ß (12).
Furthermore, it has been demonstrated that an increase in
COL2A1 expression induces the production of extracellular
matrix (ECM) (12).
HIF-1 regulates the transcription of a wide range of
genes involved in glucose metabolism, angiogenesis and cell
survival (2,3). The HIF-1 heterodimeric transcription
complex is composed of HIF-1α and HIF-1β subunits. A hypoxic
environment, hormones and growth factors can induce the
translocation of HIF-1 to the nucleus, where it associates with its
corresponding subunit to form an active HIF-1 transcription factor
that may regulate the expression of its target genes (2,3). HIF-1α
regulates hypoxia-induced ECM synthesis in chondrocytes, as well as
cartilage regeneration (13–15).
CHAD is a class IV small leucine-rich
proteoglycan/protein that mediates the signaling between
chondrocytes and the ECM (16). CHAD
binds to the α2β1 integrin, cell surface proteoglycans and type II
collagen and serves a role in the regulation of chondrocyte
signaling and cartilage homeostasis (16).
The present study investigated the effect of
treatment with low, medium and high MW HA on COL2A1, HIF-1α and
CHAD expression in chondrocytes. Furthermore, the effect of HA on
chondrocyte viability and proliferation was assessed. The aim of
the current study was to determine whether the administration of
different MWs of HA may be an effective method of treating patients
with OA in a clinical setting.
Materials and methods
Patient selection
Cartilage tissue was obtained from 14 patients
diagnosed with OA from Istanbul Medipol University Hospital, Namik
Kemal University Hospital, Gaziosmanpasa Taksim Training and
Research Hospital, Abant Izzet Baysal University Hospital, Istanbul
Medipol University Hospital, Pamukkale University Hospital, Medical
Park Hospital, Denizli Private Hospital and Memorial Hospital.
Osteophytes were graded using the Kellgren-Lawrence radiological
grading scale (17). Patients were
excluded if they had defects in kidney function or an allergy to a
specific protein, including milk, egg or avian, or if they had
taken methotrexate, fludarabine, cyclophosphamide, high doses of
steroid and/or pressor substances, monoamine oxidase, coumarin
group anticoagulants, phenytoin, primidone, phenylbutazone or
tricyclic antidepressants in the preceding year. A total of 6
patients (3 female and 3 male; mean age, 64.92±3.68 years) were
included in the current study. These patients were also
unresponsive to medical and conservative treatments for
gonarthrosis. The present study was performed with the approval of
the Local Ethics Board of Pamukkale University (Denizli, Turkey).
Informed consent was obtained from patients attending the
Orthopedics and Traumatology Clinic of all the aforementioned
hospitals between August 2016 and June 2017, for use of their
cells. Researchers did not know which groups received drugs and
were blinded to which drugs were applied to the culture.
Study design and in vitro experimental
setup
Standard primary chondrocyte cultures were
established from surgically obtained osteochondral tissues taken
from all 6 patients. Chondrocyte cultures were monitored using an
inverted microscope. HAs of different MWs has been prepared using
the appropriate solutions and concentrations. In the well plates,
color-coded HAs were added and an extra plate from each treatment
was set aside for MTT analysis, acridin orange/propidium iodide
(AO/PI) staining and reverse transcription-quantitative polymerase
chain reaction (RT-qPCR).
Isolation of primary chondrocytes
Osteochondral tissues were obtained from the distal
femur and proximal tibia in patients with OA undergoing total knee
arthroplasty for gonarthrosis. Tissues were transferred to the
laboratory and cultured at 37°C in Dulbecco's modified Eagle's
medium supplemented with 1% penicillin-streptomycin, 15% fetal
bovine serum and 1% L-glutamine (all Gibco; Thermo Fisher
Scientific, Inc., Waltham, MA, USA). Osteochondral tissue samples
were irrigated with 0.9% isotonic sodium chloride solution in a
laminar flow cabinet to isolate samples from red blood cells.
Tissues were dissected into 0.4 cm3 pieces, washed in
Hank's balanced salt solution (Gibco; Thermo Fisher Scientific,
Inc.) and transferred to Falcon tubes. Collagenase type II (0.375
mg; Gibco; Thermo Fisher Scientific, Inc.) dissolved in complete
medium was added and incubated with tissues at 37°C overnight in 5%
CO2. Samples were then centrifuged at a speed of 130 × g
for 10 min in a coolant centrifuge at 4°C. Cells were subsequently
re-suspended in culture medium and transferred to T75 flasks prior
to incubation at 37°C with 5% CO2 to obtain primary cell
cultures. The cultures were incubated until they became a monolayer
confluent culture. Incubation duration differs between samples
depending on the age of the patient, viable cell count, transport
conditions and to doubling times of cells where they originated
from, as previously described (18).
Monolayer primary chondrocyte cultures were
trypsinized and viable cells were identified via staining with
trypan blue. Cell suspensions were seeded at a density of
1×104 cells/well in 96-well plates for MTT analysis,
3×104 cells/well in 24-well plates for AO/PI analysis
and 4×106 cell/dish in 100-mm petri dishes for RNA
isolation. Following 24 h incubation at 37°C, low, medium and high
MW HA was added to these cell cultures (0 h). Results from each
experiment were obtained at 0, 24 and 48 h following HA
treatment.
Preparation and application of HA
The stock solution concentrations of the HA
preparations used were: Low MW (800–1,200 kDa; Sinovial
One®; 50 mg/2.5 ml; IBSA Farmaceutici, Lodi, Italia),
medium MW (2,500 kDa; Viscoplus®; 75 mg/3 ml; BioMedical
B. Baumann GmbH, Rodgau, Germany) and high MW HA (10,000 kDa;
Durolane®; 60 mg/ml; Bioventus LCC, Durham, NC, USA). A
HA concentration of 1 µM was used in all experiments, as the
majority of pharmaceutical formulations are administered at this
concentration (19).
AO/PI staining
The AO/PI staining solution consisted of 10 g
disodium-EDTA, 4 mg PI, 50 ml FBS and 4 mg AO (dissolved in 2 ml
99% ethanol). The solution was mixed well and sterile distilled
water was added to form a final volume of 200 ml. After incubation
for 10 min at room temperature, cell cultures were monitored using
a fluorescent microscope.
The nucleic acid binding dyes AO and PI may be used
to accurately determine cell viability. AO is an intercalating dye
able to permeate living and dead cells; it stains all nucleated
cells and generates green fluorescence. PI can only enter dead
cells with poor membrane integrity; it stains all dead nucleated
cells to generate red fluorescence. Following staining with AO/PI,
live nucleated cells exhibit green fluorescence and all dead
nucleated cells exhibit red fluorescence (20).
Imaging with inverted and fluorescence
microscopy
An inverted light microscope (magnification, ×20;
CKX41; Olympus Corporation, Tokyo, Japan) was used to monitor cell
cultures and a fluorescent microscope (magnification, ×20; DM2500;
Leica Microsystems, Inc., Buffalo Grove, IL, USA) was used for
analysis of AO/PI staining. Microphotographs of the cell
organizations were obtained prior to and during HA treatment and
images were evaluated using the CytoVision capture station imaging
program V.7.2 (Leica Microsystems, Inc.).
MTT analysis
Cell viability was assessed using a commercial MTT
kit (Vybrant® MTT cell proliferation assay kit; Thermo
Fisher Scientific, Inc.) following the manufacturer's protocol. MTT
was prepared by adding 1 ml sterile PBS to a vial containing 5 mg
MTT to obtain a 12 mM MTT stock solution. To analyze cell
viability, 10% MTT solution prepared with complete medium was
applied to monolayer cultures. Cultures were then incubated in a
dark environment at 37°C for 4 h. At the end of the incubation
period, dimethyl sulfoxide was added to dissolve the purple
formazan and incubated at 37°C for an additional 10 min. Absorbance
was then measured at a wavelength of 540 nm. MTT analysis was
performed prior to the addition of HA (0 h; control) as well as 24
and 48 h following HA addition (18,20–25).
Absorbance was measured using a microplate reader (Mindray MR-96A;
Shenzhen Mindray Bio-Medical Electronics Co., Ltd., Shenzhen,
China).
Gene-specific RT-qPCR analysis
Total RNA was extracted from cultured primary human
chondrocytes using the PureLink RNA mini kit (cat. no. 12183018A;
Ambion; Thermo Fisher Scientific, Inc.) and 2-mercaptoethanol (cat.
no. 31350010; Thermo Fisher Scientific, Inc.). The quantity of RNA
obtained from each sample was measured using a UV spectrophotometer
(UV-VIS Spectrophotometer 2600; Shimadzu Corporation, Kyoto,
Japan). To obtain cDNA, 50 ng RNA was reverse transcribed using a
high-capacity cDNA reverse transcription kit (cat. no. 4368814;
Thermo Fisher Scientific, Inc.) and a thermal cycler (ProFlex;
Thermo Fisher Scientific, Inc.). For RT, 10 µl 10X reverse
transcription buffer, 4 µl 25X dNTP, 10 µl 10X random primers, 5 µl
50 U/µl reverse transcriptase, 51 µl nuclease free water and 20 µl
RNA were mixed well and held at 25°C for 10 min, and then
maintained at 37°C for 2 h. All genes were amplified using
TaqMan® Gene Expression assays for CHAD (assay ID.
Hs00154382_m1; cat. no. 4448892), HIF-1α (assay ID. Hs00153153_m1;
cat. no. 4453320), COL2A1 (assay ID. Hs00264051_m1; cat. no.
4453320) and internal control gene [housekeeping genes-actin beta
(ACTB; assay ID. Hs99999903_m1; cat. no. 4453320)]. qPCR was
performed on an Applied Biosystems 7300/7500 real-time PCR system
(Thermo Fisher Scientific, Inc.) and the reaction mixture consisted
of 1 µl TaqMan gene expression assay, 10 µl TaqMan gene expression
master mix (cat. no. 4369016), 4 µl cDNA template and UltraPure
DNase/RNase-free distilled water (cat. no. 10977035) for each gene
in MicroAmp fast optical 96-well reaction plates (cat. no.
4346906). The thermocycling conditions were as follows: 2 min at
50°C, 10 min at 95°C, 15 sec at 95°C and 1 min at 60°C, for 40
cycles. As a result of the RT-qPCR experiment, the RQ values of
each sample were obtained using the 7500 Fast-SDS program V.2.3
(Thermo Fisher Scientific, Inc.). An endogenous control (ACTB) was
utilized to normalize the target gene expression. For comparative
results, a reference (calibrator) sample (Group 1, 0 h) was used
and relative quantity (RQ) values were calculated using the
2−ΔΔCq method (21).
Statistical analysis
Statistical analysis was performed using the Minitab
program (version 16; Minitab, Inc., State College, PA, USA). All
data are expressed as the mean ± standard deviation. The results
were evaluated using repeated measures one-way analysis of variance
to assess whether there were significant differences across
experimental groups, followed by Tukey's honest significant
difference test for post hoc analysis. P<0.05 was considered to
indicate a statistically significant difference. All experiments
were repeated at least three times. To avoid measurement errors,
the same types of analysis were performed by the same
researchers.
Results
Morphological evaluation of
chondrocyte cultures
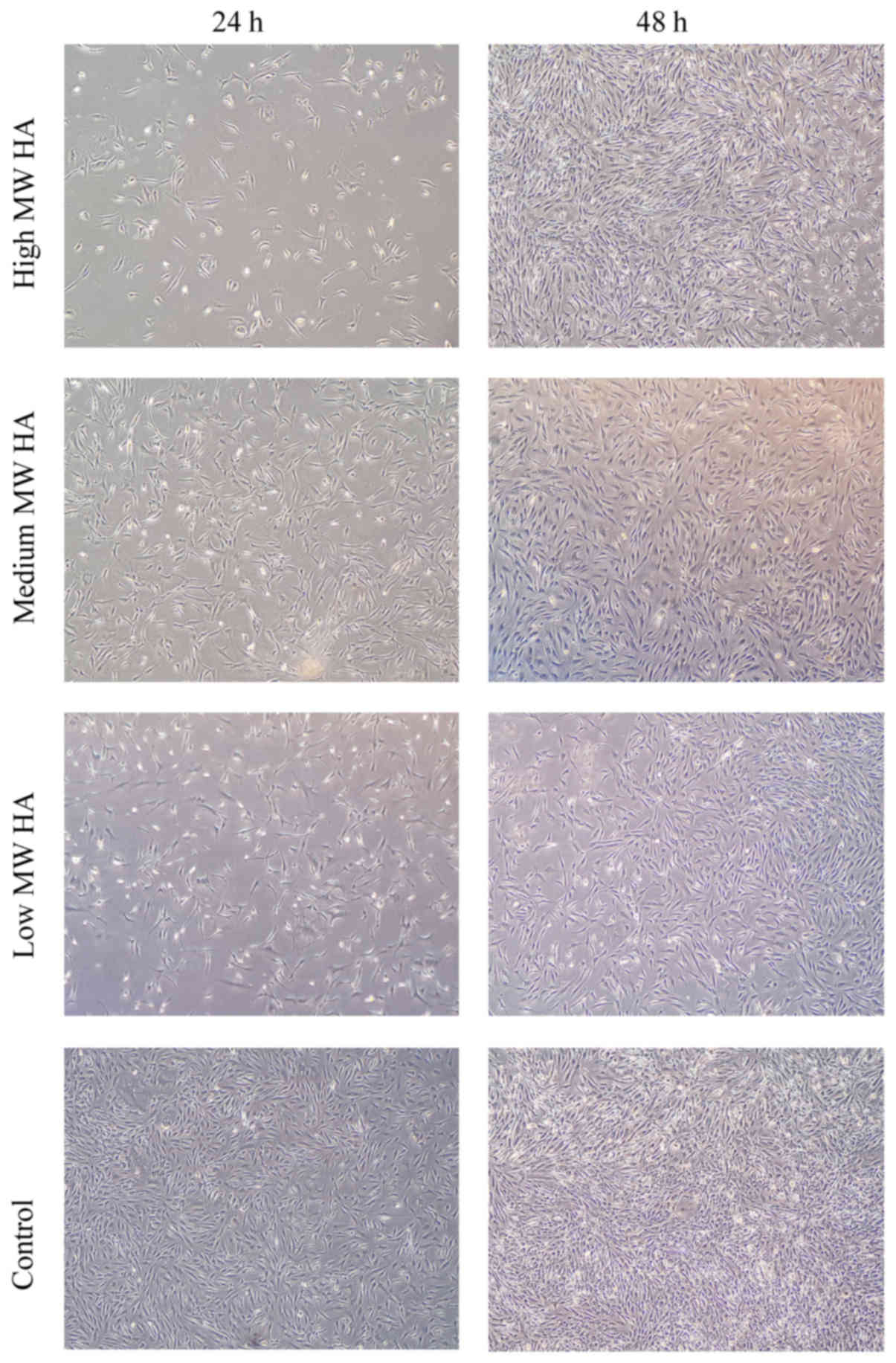
Chondrocyte morphology was evaluated 24 and 48 h
following treatment with low, medium and high MW HA. Cell
proliferation in the control group at 24 h was greater than in all
HA-treated experimental groups. Although the number of cells
appeared fewer in number than HA-treated groups in morphological
observations, MTT analysis demonstrated that the viable cell ratio
remained almost the same at 24 h in all groups. However, it was
observed that chondrocyte proliferation increased in all
experimental groups at 48 h following HA treatment, particularly in
the high-MW HA treatment group that underwent morphological
evaluation (Fig. 1). Despite
cultures in HA-treated groups having a weaker confluency following
24 h, to demonstrate that HA or its components do not suppress
chondrocyte proliferation and to confirm MTT data cell viability in
the same cultures were also assessed using AO/PI staining.
Micrographs obtained following AO/PI staining are presented in
Fig. 2. Cells retained their
specific morphology, maintained viability and continued to
proliferate in all experimental groups according to microscopic
examinations, indicating that HA does not have a repressive effect
(Fig. 2).
Statistical analysis of chondrocyte
proliferation
Cell viability was determined by MTT analysis,
confirmed by AO/PI staining and evaluated statistically. The
results revealed that the increase in cell proliferation was
significantly associated with the duration of application
(P<0.05; Fig. 3). However, there
were no significant differences between the cell viability in the
groups treated with HA that had different MWs (Table I).
 | Table I.Statistical analysis of hyaluronic
acid application with one-way analysis of variance and Tukey's post
hoc test. |
Table I.
Statistical analysis of hyaluronic
acid application with one-way analysis of variance and Tukey's post
hoc test.
|
| Mean OD ± SD |
|
|---|
|
|
|
|
|---|
| Hyaluronic acid
treatment | 0 h | 24 h | 48 h | P-value |
|---|
| Low MW | 0.322±0.03 | 0.328±0.05 | 0.310±0.01 | 0.310 |
| Medium MW | 0.322±0.03 | 0.332±0.04 | 0.334±0.01 | 0.311 |
| High MW | 0.322±0.03 | 0.320±0.06 | 0.332±0.03 | 0.298 |
| Control | 0.322±0.03 | 0.317±0.06 | 0.249±0.01 | 0.296 |
Analysis of CHAD, COL2A1 and HIF-1α
gene expression
The expression of CHAD, COL2A1 and
HIF-1α were assessed 24 and 48 h following treatment with HA
at different MWs. RQ) values were calculated for each experimental
group using the 7500 Fast-SDS program. β-actin was used as
endogenous control and the control group at 0 h was designated to
be the reference sample. The expression of the gene of interest was
determined as 100% and the RQ value was 1 in the reference sample
and RQ values of other samples were calculated as fold changes with
comparison to this reference (21).
No further statistical analysis was performed on the obtained RQ
values.
Fig. 4 summarizes the
RQ values determined for each experimental group. In the medium MW
HA treated group, COL2A1 gene expression increased 1.73-fold and
CHAD gene expression increased 1.35-fold at 48 h compared with the
control group. Furthermore, at 24 h, the COL2A1 gene RQ value was
1.05. In the high MW HA treated group, the RQ value determined for
the COL2A1 gene was 1.06 at 24 h and RQ value determined for the
HIF-1α gene was 1.07 at 48 h (Fig.
4).
Discussion
The primary goal of treatments for cartilage damage
is to completely restore hyaline cartilage. Surgery and other
treatments are being developed for this purpose. Although there are
a number of promising methods and some encouraging clinical
results, no treatments have achieved complete restoration (1,4).
Viscosupplementation with HA is an example of a promising treatment
method. HA injections reduce pain and recover joint function by
functioning as a lubricant and shock absorber (4,6).
Although not fully understood, HA injections have been demonstrated
to inhibit inflammation, decrease cartilage degradation and induce
ECM synthesis (1,6). Surgeons cannot yet achieve biological
repair following cartilage damage; however, treatment with HA is
preferred as it inhibits the pathophysiological pathway leading to
arthrosis and reduces the pain and movement limitation experienced
by patients (1).
HA concentrations are decreased in the affected
joints of patients with OA. It has been suggested that HA treatment
is more beneficial than viscous fluid replacement therapy, as it
stimulates tissue organization and modulates inflammation and
macrophages (8,19). Consequently, various commercial HA
preparations with different MWs are clinically used (9,23–25).
Certain studies have indicated that high MW HA is more effective
than low MW HA in treating OA; however, other studies suggest that
there is no substantial evidence to support this (1,24–27). In
the present study, chondrocyte cultures were morphologically
evaluated and cell viability and proliferation were determined. The
results revealed that the positive effect of HA treatment on cell
proliferation was independent of the MW of HA.
Animal tissue or commercial cell lines were not used
in the current study; instead, cartilage tissues were obtained from
patients with knee prosthesis during the course of routine clinical
practice. Following knee prosthesis, undamaged chondral tissues of
the resectioned articular surface were used to prepare primary
chondrocyte cultures. Human primary articular chondrocyte cultures
model complete tissue as they contain all cell types and ECM
components of their original tissue (28–31);
therefore the results of the present study may enhance
understanding of how cartilage degeneration occurs. However, as the
effects of HA in the present study were only evaluated in
vitro, the results cannot be generalized to predict the effects
of HA in vivo.
In the present study, the effect of HA with
different MWs on the levels of COL2A1, HIF-1α and CHAD expression
was investigated. The COL2A1 gene encodes an important
cartilage-specific extracellular matrix protein that is synthesized
from proliferative chondrocytes and is essential for chondrogenesis
(12,32). In the developing cartilage of the
growing bone, chondrocytes alter their morphology to become
hypertrophic and do not express COL2A1. In adult articular
cartilage, hypertrophic differentiation processes do not occur and
COL2A1 is expressed (32). However,
in OA degenerative articular cartilage, phenotypic conversion to
hypertrophic chondrocytes has been reported (32). Furthermore, anabolic and catabolic
processes are broadly affected in OA (12) and in cartilage, COL2A1 expression is
a marker of anabolic processes (5).
A previous study revealed that COL2A1 expression increases when
chondrocytes are cultured with HA and growth factors (12). It has also been reported that COL2A1
expression increases in human OA-derived chondrocytes following
treatment with high MW HA (5). The
results of the present study demonstrated that COL2A1 gene
expression increased in chondrocytes following treatment with
medium and high MW HA. COL2A1 expression was 5.58-fold higher in
the medium MW HA treated group (RQ=1.05) compared with the control
group (RQ=0.18) at 24 h. Furthermore, COL2A1 expression was
1.8-fold higher in the medium MW HA treated group (RQ=1.73)
compared with the control group (RQ=0.96) at 48 h. A 5.88-fold
increase in COL2A1 expression was only observed (RQ=1.06) in the
high MW HA treated group at 24 h. However, COL2A1 expression was
the same as the control following 48 h. It was also demonstrated
that increased duration of medium MW HA treatment increased the
expression of the COL2A1 gene, which is associated with chondrocyte
proliferation and ECM formation.
Chondrogenesis is regulated by numerous mechanisms,
including growth factors, cytokines and oxygen supply (15). During the initial stages of
chondrogenesis, the developing cartilaginous template is
avascularized and forms hypoxic niches (13,15).
HIF-1α is a basic helix-loop-helix transcription factor expressed
in hypoxic conditions (13,14). HIF-1 is a heterodimer of α and β
subunits. The expression of the α subunit is induced by hypoxia,
whereas the β subunit is constitutively expressed in the nucleus.
In hypoxic conditions, the activity of the HIF-targeting prolyl
hydroxylase enzymes (PHD)1, PHD2 and PHD3 is inactivated; as a
result, HIF-1α, is not hydroxylated and accumulates in the
cytoplasm. Following this, HIF-1 translocates into the nucleus and
dimerizes with HIF-1β to form the HIF-1 complex. This complex
subsequently binds to hypoxia responsive elements within the
promoter region of target genes, including Sox9, vascular
endothelial growth factor A, glycolytic enzymes and glucose
transporters, and induces their transcription, stimulating
chondrocyte differentiation and hypoxic condition adaptation
(13,15). HIF-1 therefore positively regulates
cartilage development and regeneration (13,14).
Several studies have suggested that HIF-1α serves a role in
regulating hypoxia-induced ECM synthesis in chondrocytes (13–15). In
the present study, it was observed that HIF-1α expression (RQ=1.07)
was 1.53-fold higher than the control group (RQ=0.70) at 48 h in
the high MW HA group only.
CHAD is a non-canonical class IV small leucine-rich
proteoglycan/protein. This 38 kDa protein mediates signaling
between chondrocytes and the ECM via α2β1 integrin, cell surface
proteoglycans and type II collagen binding (16). It has been demonstrated that the
expression of CHAD is upregulated in chondrocyte cultures (33). CHAD predominantly regulates the
formation of the collagen fibrillar network during early skeletal
development. Therefore, it has been hypothesized that CHAD
downregulation serves a critical role in the initiation and
progression of OA (16). In the
present study, a 1.49-fold increase in CHAD expression (RQ=1.36)
following 48 h was observed in the medium MW group alone.
The present study was performed in in vitro
primary cultures that directly reflected the entire structure of
the original tissue, increasing the value of the obtained data.
However, these primary cultures were established using samples
taken from only 6 patients; therefore, further studies are required
to definitively establish the effect of different MWs of HA on the
expression of different genes in OA. OA is a multifactorial
disease; therefore gene expression in different patients may vary
due to individual differences, independent from disease (34). In the present study, gene expression
increased as the duration of treatment increased in the medium and
high MW groups. Furthermore, the increased duration of treatment
increased chondrocyte viability and proliferation. Taken together,
these results indicate that administration of medium and high MW HA
may be successful at treating patients with OA.
In conclusion, the present study evaluated the
effects of low, medium and high MW HA on the expression of COL2A1,
CHAD and HIF-1α in a robust in vitro culture of
human-derived chondrocytes. Similar to previous studies, an
increase in COL2A1, CHAD and HIF-1α expression and proliferation
was observed, particularly in cultures treated with medium and high
MW HA. Further studies are required to confirm these results in
vivo. Typically, it is difficult to imitate the full scope of
OA with all the involved cellular constituents in vitro.
Therefore, the majority of in vitro OA models are designed
to focus on the late stages of disease, or use cell lines. However,
this has significant limitations and it is critical to evaluate the
mechanisms that are affected during the early stages of OA and in
primary cell cultures. The present study demonstrated that HA
administration at different molecular weights to cell cultures,
over short periods (24 and 48 h) changed the expression of certain
genes. Further study into gene expression is required to define
treatment protocols and elucidate the pathogenesis of OA. However,
clinicians should consider the cellular effects of HA molecular
weight in the treatment of OA.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The analyzed data sets generated during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
DYS contributed to the study concept and design and
preparation of manuscript, as well as the acquisition of subjects
and data, analysis and interpretation of data, preparation of human
primer chondrocyte culture, and performance and evaluation of PCR
analyses. NK contributed to the study concept and design,
acquisition of subjects and data, and the writing of the discussion
section. IY contributed to the preparation of human primer
chondrocyte culture, inverted light microscopy, performance and
evaluation of ELISA analyses, as well as the preparation and
storage of culture drugs. IY and HO contributed to the statistical
evaluation of the findings and writing of the manuscript. YA
selected the patients who met the inclusion criteria and
contributed to the statistical evaluation of findings. YK, OG, KO,
SA and MM diagnosed and operated on patients, and contributed to
the removal of tissues from the cases and their transfer to the
laboratory. HO, NK, NA, DYS contributed to the preparation and
critical revision of the manuscript for important intellectual
content. NA also prepared the drugs and adapted the clinical doses
to cell cultures. All authors have read and approved the final
version of the manuscript.
Ethics approval and consent to
participate
This study was performed with the approval of the
Local Ethics Board of Pamukkale University (Denizli, Turkey) and
informed consent was obtained from all patients for use of their
cells.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
CHAD
|
chondroadherin
|
|
COL2A1
|
collagen type II α 1 chain
|
|
ECM
|
extracellular matrix
|
|
HA
|
hyaluronic acid
|
|
HIF-1α
|
hypoxia-inducible factor 1α
|
|
MW
|
molecular weight
|
|
OA
|
osteoarthritis
|
|
RQ
|
relative quantity
|
References
|
1
|
Aggarwal A and Sempowski IP: Hyaluronic
acid injections for knee osteoarthritis. Systematic review of the
literature. Can Fam Physician. 50:249–256. 2004.PubMed/NCBI
|
|
2
|
Zelzer E, Mamluk R, Ferrara N, Johnson RS,
Schipani E and Olsen BR: VEGFA is necessary for chondrocyte
survival during bone development. Development. 131:2161–2171. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Charlier E, Relic B, Deroyer C, Malaise O,
Neuville S, Collée J, Malaise MG and De Seny D: Insights on
molecular mechanisms of chondrocytes death in osteoarthritis. Int J
Mol Sci. 17:E21462016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Neustadt DH: Intra-articular injections
for osteoarthritis of the knee. Cleve Clin J Med. 73(897–898):
901–904, 906–911. 2006.
|
|
5
|
Bauer C, Niculescu-Morzsa E, Jeyakumar V,
Kern D, Späth SS and Nehrer S: Chondroprotective effect of
high-molecular-weight hyaluronic acid on osteoarthritic
chondrocytes in a co-cultivation inflammation model with M1
macrophages. J Inflamm (Lond). 13:312016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kelly MA, Moskowitz RW and Lieberman JR:
Hyaluronan therapy: Looking toward the future. Am J Orthop (Belle
Mead NJ). 33 2 Suppl:S23–S28. 2004.
|
|
7
|
McGrath AF, McGrath AM, Jessop MA, Gandham
S, Datta G, Dawson-Bowling S and Cannon SR: A comparison of
intra-articular hyaluronic acid competitors in the treatment of
mild to moderate knee osteoarthritis. J Arthritis. 2:12013.
View Article : Google Scholar
|
|
8
|
Kelly MA, Kurzweil PR and Moskowitz RW:
Intra-articular hyaluronans in knee osteoarthritis: Rationale and
practical considerations. Am J Orthop (Belle Mead NJ). 33 2
Suppl:S15–S22. 2004.
|
|
9
|
Ghosh P and Guidolin D: Potential
mechanism of action of intra-articular hyaluronan therapy in
osteoarthritis: Are the effects molecular weight dependent? Semin
Arthritis Rheum. 32:10–37. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Barreto RB, Sadigursky D, de Rezende MU
and Hernandez AJ: Effect of hyaluronic acid on chondrocyte
apoptosis. Acta Ortop Bras. 23:90–93. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Patti AM, Gabriele A, Vulcano A, Ramieri
MT and Della Rocca C: Effect of hyaluronic acid on human
chondrocyte cell lines from articular cartilage. Tissue Cell.
33:294–300. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Klangjorhor J, Phitak T, Pruksakorn D,
Pothacharoen P and Kongtawelert P: Comparison of growth factor
adsorbed scaffold and conventional scaffold with growth factor
supplemented media for primary human articular chondrocyte 3D
culture. BMC Biotechnol. 14:1082014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Niebler S, Angele P, Kujat R and
Bosserhoff AK: Hypoxia-inducible factor 1 is an inductor of
transcription factor activating protein 2 epsilon expression during
chondrogenic differentiation. Biomed Res Int. 2015:3805902015.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kozhemyakina E, Lassar AB and Zelzer E: A
pathway to bone: signaling molecules and transcription factors
involved in chondrocyte development and maturation. Development.
142:817–831. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wang P, Zhang F, He Q, Wang J, Shiu HT,
Shu Y, Tsang WP, Liang S, Zhao K and Wan C: Flavonoid compound
icariin activates hypoxia inducible factor-1α in chondrocytes and
promotes articular cartilage repair. PLoS One. 11:e01483722016.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Batista MA, Nia HT, Önnerfjord P, Cox KA,
Ortiz C, Grodzinsky AJ, Heinegård D and Han L: Nanomechanical
phenotype of chondroadherin-null murine articular cartilage. Matrix
Biol. 38:84–90. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kellgren JH and Lawrence JS: Radiological
assessment of rheumatoid arthritis. Ann Rheum Dis. 16:485–493.
1957. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Isyar M, Yilmaz I, Sirin Yasar D, Yalcin
S, Guler O and Mahirogullari M: A practical way to prepare primer
human chondrocyte culture. J Orthop. 13:162–167. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Rayahin JE, Buhrman JS, Zhang Y, Koh TJ
and Gemeinhart RA: High and low molecular weight hyaluronic acid
differentially influence macrophage activation. ACS Biomater Sci
Eng. 1:481–493. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Mascotti K, McCullough J and Burger SR:
HPC viability measurement: Trypan blue versus acridine orange and
propidium iodide. Transfusion. 40:693–696. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
VanGuilder HD, Vrana KE and Freeman WM:
Twenty-five years of quantitative PCR for gene expression analysis.
Biotechniques. 44:619–626. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Smith MM and Ghosh P: The synthesis of
hyaluronic acid by human synovial fibroblasts is influenced by the
nature of the hyaluronate in the extracellular environment.
Rheumatol Int. 7:113–122. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Aviad AD and Houpt JB: The molecular
weight of therapeutic hyaluronan (sodium hyaluronate): How
significant is it? J Rheumatol. 21:297–301. 1994.PubMed/NCBI
|
|
25
|
Arrich J, Piribauer F, Mad P, Schmid D,
Klaushofer K and Müllner M: Intra-articular hyaluronic acid for the
treatment of osteoarthritis of the knee: Systematic review and
meta-analysis. CMAJ. 172:1039–1043. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Zhao H, Liu H, Liang X, Li Y, Wang J and
Liu C: Hylan G-F 20 vs. low molecular weight hyaluronic acids for
knee osteoarthritis: A meta-analysis. Bio Drugs. 30:387–396.
2016.
|
|
27
|
Lo GH, LaValley M, McAlindon T and Felson
DT: Intra-articular hyaluronic acid in treatment of knee
osteoarthritis: A meta-analysis. JAMA. 290:3115–3121. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Gokce A, Yilmaz I, Bircan R, Tonbul M,
Gokay NS and Gokce C: Synergistic effect of TGF-β1 and BMP-7 on
chondrogenesis and extracellular matrix synthesis: An in vitro
study. Open Orthop J. 6:406–413. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Gökçe A, Yılmaz I, Gökay NS, Can L and
Gökçe C: Does insulin, transferrin and selenous acid preparation
effect chondrocyte proliferation? Acta Orthop Traumatol Turc.
48:313–319. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Isyar M, Bilir B, Yilmaz I, Cakmak S,
Sirin DY, Guzelant AY and Mahirogullari M: Are biological agents
toxic to human chondrocytes and osteocytes? J Orthop Surg Res.
10:1182015. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Gumustas SA, Yilmaz İ, Isyar M, Sirin DY,
Batmaz AG, Ugras AA, Oznam K, Ciftci Z and Mahirogullari M:
Assessing the negative impact of phenyl alkanoic acid derivative, a
frequently prescribed drug for the suppression of pain and
inflammation, on the differentiation and proliferation of
chondrocytes. J Orthop Surg Res. 11:702016. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Ushijima T, Okazaki K, Tsushima H and
Iwamoto Y: CCAAT/enhancer-binding protein β regulates the
repression of type II collagen expression during the
differentiation from proliferative to hypertrophic chondrocytes. J
Biol Chem. 289:2852–2863. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Ezura Y, Sekiya I, Koga H, Muneta T and
Noda M: Methylation status of CpG islands in the promoter regions
of signature genes during chondrogenesis of human synovium-derived
mesenchymal stem cells. Arthritis Rheum. 60:1416–1426. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Pombo-Suarez M, Calaza M, Gomez-Reino JJ
and Gonzalez A: Reference genes for normalization of gene
expression studies in human osteoarthritic articular cartilage. BMC
Mol Biol. 9:172008. View Article : Google Scholar : PubMed/NCBI
|