|
1
|
Madelung CF, Falk MK and Sørensen TL: The
association between neovascular age-related macular degeneration
and regulatory T cells in peripheral blood. Clin Ophthalmol.
9:1147–1154. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Attridge K and Walker LS: Homeostasis and
function of regulatory T cells (Tregs) in vivo: Lessons from
TCR-transgenic Tregs. Immunol Rev. 259:23–39. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Käser T, Mair KH, Hammer SE, Gerner W and
Saalmüller A: Natural and inducible Tregs in swine: Helios
expression and functional properties. Dev Comp Immunol. 49:323–331.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zhang H, Kong H, Zeng X, Guo L, Sun X and
He S: Subsets of regulatory T cells and their roles in allergy. J
Transl Med. 12:1252014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lu Y, Wang X, Gu J, Lu H, Zhang F, Li X,
Qian X, Wang X and Lu L: iTreg induced from CD39(+) naive T cells
demonstrate enhanced proliferate and suppressive ability. Int
Immunopharmacol. 28:925–930. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Biswas M, Sarkar D, Kumar SR, Nayak S and
Rogers GL: Synergy between rapamycin and FLT3 ligand enhances
plasmacytoid dendritic cell-dependent induction of CD4+CD25+FoxP3+
Treg. Blood. 125:2937–2947. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Shigematsu Y, Hanagiri T, Shiota H, Kuroda
K, Baba T, Ichiki Y, Yasuda M, Uramoto H, Takenoyama M, Yasumoto K
and Tanaka F: Immunosuppressive effect of regulatory T lymphocytes
in lung cancer, with special reference to their effects on the
induction of autologous tumor-specific cytotoxic T lymphocytes.
Oncol Lett. 4:625–630. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Demir N, Ilhan F, Demir T and Godekmerdan
A: sCTLA-4, CD4+CD25+Foxp3+ regulatory T cells in Behçet's disease
patients. Clin Exp Rheumatol. 30(3): Suppl 72:S116–S117.
2012.PubMed/NCBI
|
|
9
|
Daniel V, Sadeghi M, Wang H and Opelz G:
CD4 (+)CD25 (+)Foxp3(+)IFNγ(+) Treg are immunosuppressive in vitro
and increase with intensity of the alloresponse in pretransplant
MLC. Transpl Immunol. 27:114–121. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Tselios K, Sarantopoulos A, Gkougkourelas
I and Boura P: The influence of therapy on CD4+CD25 (high)FOXP3+
regulatory T cells in systemic lupus erythematosus patients: A
prospective study. Scand J Rheumatol. 44:29–35. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zeng H and Chi H: The interplay between
regulatory T cells and metabolism in immune regulation.
Oncoimmunology. 2:e265862013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sun YL, Lin GG, Zhang K and Wang LN:
Application and effects of mouse Foxp3 antibody and
fixation/permeabilization buffer on the detection of CD4+
regulatory T cells in various mammal species. Genet Mol Res.
12:6535–6545. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kim MH, Koo JS and S L: FOXP3 expression
is related to high Ki-67 index and poor prognosis in lymph
node-positive breast cancer patients. Oncology. 85:128–136. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Vent-Schmidt J, Han JM, MacDonald KG and
Levings MK: The role of FOXP3 in regulating immune responses. Int
Rev Immunol. 33:110–128. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Jiang N, Li M and Zeng X: Correlation of
Th17 cells and CD4+CD25+ regulatory T cells
with clinical parameters in patients with systemic sclerosis. Chin
Med J (Engl). 127:3557–3561. 2014.PubMed/NCBI
|
|
16
|
Schoenbrunn A, Frentsch M, Kohler S, Keye
J, Dooms H, Moewes B, Dong J, Loddenkemper C, Sieper J, Wu P, et
al: A converse 4-1BB and CD40 ligand expression pattern delineates
activated regulatory T cells (Treg) and conventional T cells
enabling direct isolation of alloantigen-reactive natural Foxp3+
Treg. J Immunol. 189:5985–5994. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Chauhan SK, Saban DR, Dohlman TH and Dana
R: CCL-21 conditioned regulatory T cells induce allotolerance
through enhanced homing to lymphoid tissue. J Immunol. 192:817–823.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Tognela A, Spring KJ, Becker T, Caixeiro
NJ, Bray VJ, Yip PY, Chua W, Lim SH and de Souza P: Predictive and
prognostic value of circulating tumor cell detection in lung
cancer: A clinician's perspective. Crit Rev Oncol Hematol.
93:90–102. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Greystoke A, Ayub M, Rothwell DG, Morris
D, Burt D, Hodgkinson CL, Morrow CJ, Smith N, Aung K, Valle J, et
al: Development of a circulating miRNA assay to monitor tumor
burden: From mouse to man. Mol Oncol. 10:282–291. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Yu Y, Chen Z, Dong J, Wei P, Hu R, Zhou C,
Sun N, Luo M, Yang W, Yao R, et al: Folate receptor-positive
circulating tumor cells as a novel diagnostic biomarker in
non-small cell lung cancer. Transl Oncol. 6:697–702. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Li G, Liu D, Cooper TK, Kimchi ET, Qi X,
Avella DM, Li N, Yang QX, Kester M, Rountree CB, et al: Successful
chemoimmunotherapy against hepatocellular cancer in a novel murine
model. J Hepatol. 66:75–85. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Zhou Y, Wang B, Wu J, Zhang C, Zhou Y,
Yang X, Zhou J, Guo W and Fan J: Association of preoperative EpCAM
Circulating Tumor Cells and peripheral Treg cell levels with early
recurrence of hepatocellular carcinoma following radical hepatic
resection. BMC Cancer. 16:5062016. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Duan MC, Zhong XN, Liu GN and Wei JR: The
Treg/Th17 paradigm in lung cancer. J Immunol Res. 2014:7303802014.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Li S, Li Y, Qu X, Liu X and Liang J:
Detection and significance of TregFoxP3(+) and Th17 cells in
peripheral blood of non-small cell lung cancer patients. Arch Med
Sci. 10:232–239. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Sun L, Wu J and Yi S: Foxp3 is critical
for human natural CD4+CD25+ regulatory T cells to suppress
alloimmune response. Transpl Immunol. 26:71–80. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Sela U, Olds P, Park A, Schlesinger SJ and
Steinman RM: Dendritic cells induce antigen-specific regulatory T
cells that prevent graft versus host disease and persist in mice. J
Exp Med. 208:2489–2496. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Hasegawa H, Lei J, Matsumoto T, Onishi S,
Suemori K and Yasukawa M: Lysophosphatidylcholine enhances the
suppressive function of human naturally occurring regulatory T
cells through TGF-β production. Biochem Biophys Res Commun.
415:526–531. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
de Almeida AS, Fiske CT, Sterling TR and
Kalams SA: Increased frequency of regulatory T cells and T
lymphocyte activation in persons with previously treated
extrapulmonary tuberculosis. Clin Vaccine Immunol. 19:45–52. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Guo Y, Wu CZ, Liao Y and Zhang QY: The
expression and significance of CD4+CD25+CD127low/-regulatory T
cells and Foxp3 in patients with portal hypertension and
hypersplenism. Hepatogastroenterology. 60:581–584. 2013.PubMed/NCBI
|
|
30
|
Kumar S, Naqvi RA, Ali R, Rani R, Khanna N
and Rao DN: CD4+CD25+ T regs with acetylated FoxP3 are associated
with immune suppression in human leprosy. Mol Immunol. 56:513–520.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Hamza E, Akdis CA, Wagner B, Steinbach F
and Marti E: In vitro induction of functional allergen-specific
CD4+ CD25high Treg cells in horses affected with insect bite
hypersensitivity. Clin Exp Allergy Aug. 43:889–901. 2013.
View Article : Google Scholar
|
|
32
|
Avalos-Martínez CE, Rodríguez-Alba JC,
Berrón-Ruiz L, Romero-Ramírez H, Santos-Argumedo L, Jiménez-Zamudio
LA, Domínguez-López ML, Vega-López A and García-Latorre E:
Measurement of suppressor activity of T
CD4+CD25+ T reg cells using bromodeoxyuridine
incorporation assay. Immunol Invest. 42:369–381. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Turner MS, Kane LP and Morel PA: Dominant
role of antigen dose in CD4+Foxp3+ regulatory T cell induction and
expansion. J Immunol. 183:4895–4903. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Chen JH, Huang PH, Lee CC and Chen PY: A
bovine whey protein extract can induce the generation of regulatory
T cells and shows potential to alleviate asthma symptoms in a
murine asthma model. Br J Nutr. 109:1813–1820. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Baecher-Allan CM, Costantino CM,
Cvetanovich GL, Ashley CW, Beriou G, Dominguez-Villar M and Hafler
DA: CD2 costimulation reveals defective activity by human
CD4+CD25(hi) regulatory cells in patients with multiple sclerosis.
J Immunol. 186:3317–3326. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Hamza E, Gerber V, Steinbach F and Marti
E: Equine CD4(+) CD25(high) T cells exhibit regulatory activity by
close contact and cytokine-dependent mechanisms in vitro.
Immunology. 134:292–304. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
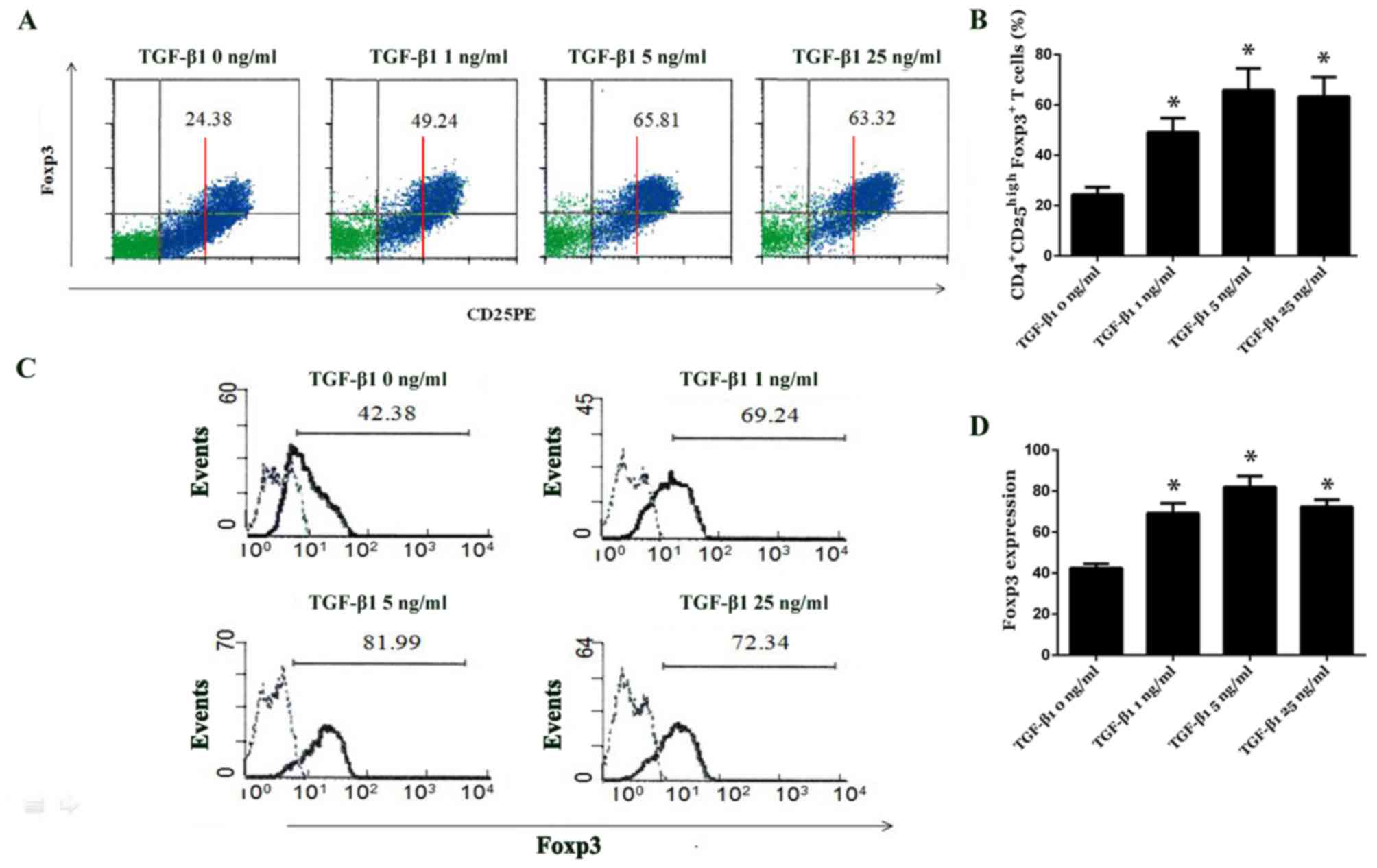
Fu S, Zhang N, Yopp AC, Chen D, Mao M,
Chen D, Zhang H, Ding Y and Bromberg JS: TGF-beta induces Foxp3 +
T-regulatory cells from CD4 + CD25-precursors. Am J Transplant.
4:1614–1627. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Ethan S, Dat T, Todd D and John A: The
critical contribution of TGF-β to the induction of foxp3 expression
and treg function. Eur J Immunol. 38:915–917. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Goubran HA, Kotb RR, Stakiw J, Emara ME
and Burnouf T: Regulation of tumor growth and metastasis: The role
of tumor microenvironment. Cancer Growth Metastasis. 7:9–18. 2014.
View Article : Google Scholar : PubMed/NCBI
|