Introduction
Esophageal benign stenosis can be induced by a
variety of reasons, such as esophageal anastomotic stenosis,
gastroesophageal reflux, corrosive stenosis and radioactive injury
(1). Recently, more and more studies
have indicated that surgeries can also lead to benign esophageal
stenosis, including endoscopic mucosal resection (EMR) and
endoscopic submucosal dissection (ESD) (2). Under various physical and chemical
effects, activation of fibroblast proliferation enhances collagen
deposition and scar formation, thus eventually leading to
esophageal contracture. Clinical treatments of benign esophageal
stenosis are varied, including surgery, expansion, stents and drugs
(3). Most esophageal stenosis can
achieve long-term relief by endoscopic distension 3 times. However,
there are still some unrelieved cases that require repeated
treatments, which is called refractory esophageal stricture or
relapse esophageal stenosis (4). It
is worth mentioning that esophageal stricture is a common
complication of esophageal ESD. Particularly, esophageal stricture
with >3/4 peeled lesion is more prone to postoperative stenosis.
Some stenosis needs to be repeatedly expanded, which is known as
the intractable narrow (5).
Currently, there are some methods that can prevent
esophageal stenosis, including endoscopic balloon dilation,
glucocorticoid, tissue engineering, amniotic membrane
transplantation, gastric mucosa transplantation, polyglycolic acid
tablets transplantation, and local injection of botulinum toxin.
Prevention of esophageal stenosis with glucocorticoids has been
demonstrated in several studies (2,5–11). In the present study, we explored the
efficacy and safety of endoscopic balloon dilatation combined with
glucocorticoid therapy on the treatment of esophageal
stricture.
Patients and methods
Patients
A total of 183 patients aged from 35 to 76 years
with a mean age of 58.6 years were enrolled in our study, including
97 males and 86 females. Patients with benign esophageal stenosis
received digestive medicine in the hospital from March 2012 to
March 2015. This study was approved by the Ethics Committee of the
Third Affiliated Hospital of Soochow University (Changzhou, China).
Signed written informed consents were obtained from all
participants before the study. Inclusion criteria were applied in
patients with significant dysphagia, esophageal or anastomotic
stricture diagnosed by endoscopy or X-ray and benign esophageal
stricture confirmed by endoscopic esophageal mucosal biopsy.
Patients with esophageal pressure and esophageal benign tumor were
excluded by ultrasound endoscope. Exclusion criteria were applied
in patients with achalasia cardia and severe cardiopulmonary
insufficiency. Pregnancies and breastfeeding women were also
excluded.
Methods
All enrolled patients were divided into endoscopic
balloon dilatation combined with triamcinolone acetonide group
(treatment group) and simple balloon dilatation group (control
group). There were 82 cases aged 43–74 years with a mean age of
55.9 years in the treatment group, and 101 cases aged from 35 to 76
years with an average age of 60.2 years in the control group.
Treatment group was further divided into the <16- and >16-mm
subgroup based on the expansion degree. Among them, 39 cases were
expanded <16 mm and 43 cases were >16 mm.
In treatment group, the gastroscopy was placed to
the site of esophageal stricture. Briefly, guide wire was crossed
into the stenosis and retained in the human gastric cavity guided
with endoscopy. With X-ray imaging, the balloon catheter was placed
alongside the guide wire. The diluted contrast medium was then
injected into the balloon until the balloon struts disappeared at
the stenosis site. When the central portion of the balloon reached
the narrow central region, triamcinolone acetonide with 1 ml/10 mg
per point was injected at four points around the esophageal
dilatation or stenosis through biopsy tracts. Simple esophageal
balloon dilatation was performed to patients in control group.
Observation
Esophageal stenosis diameter and stenosis at 15
days, 1, 2 and 4 months after operation were recorded by upper
gastrointestinal angiography. During the 12-month follow-up,
postoperative complications and prognosis were observed.
Statistical analysis
Statistical Product and Service Solutions (SPSS)
22.0 software (IBM Corp., Armonk, NY, USA) was used for statistical
analysis. The data are presented as mean ± SD. The independent
t-test was used for the difference analysis of the two groups.
Enumeration data were presented by numbers and percentages and
analyzed by the Chi-square or rank sum test. P<0.05 was
considered statistically significant (P<0.05, P<0.01,
P<0.001).
Results
Patient characteristics
Patients were divided into endoscopic balloon
dilatation combined with triamcinolone acetonide group (treatment
group) and simple balloon dilatation group (control group). There
were 82 cases in the treatment group with 44 males and 38 females
aged from 43 to 74 years (55.9±7.3 years) and 101 cases in the
control group with 53 males and 48 females aged from 60 to 64 years
(60.2±6.8 years). No significant differences were observed in sex,
age, location and causes of stenosis between the treatment and
control group (Table I). Treatment
group was further divided into the <16- and >16-mm subgroups
according to the expansion degree. There were 39 cases in the
<16-mm subgroup with 20 males and 19 females and 43 cases in the
>16-mm subgroup with 24 males and 19 females (Table II).
 | Table I.Basic patient characteristics of the
control group. |
Table I.
Basic patient characteristics of the
control group.
| Characteristics | Triamcinolone group
(n=82) | Hormone-free group
(n=101) | P-value |
|---|
| Sex |
|
| 0.873 |
| Male | 44 | 53 |
|
|
Female | 38 | 48 |
|
| Age (years) | 55.9±7.3 | 60.2±6.8 | 0.368 |
| Narrow parts |
|
|
|
| Cervical
oesophagus | 14 | 12 | 0.317 |
| Upper
thoracic esophagus | 18 | 26 | 0.551 |
| Middle
thoracic esophagus | 27 | 36 | 0.700 |
| Lower
thoracic esophagus | 23 | 27 | 0.843 |
| Narrow etiology |
|
|
|
|
Esophageal cancer early after
ESD | 26 | 36 | 0.575 |
|
Esophageal cancer anastomotic
stenosis after radical surgery | 38 | 52 | 0.489 |
|
Others | 18 | 13 | 0.103 |
 | Table II.Basic information of the treatment
group. |
Table II.
Basic information of the treatment
group.
| Information | Expansion <16 mm
(n=39) | Expansion >16 mm
(n=43) | P-value |
|---|
| Sex |
|
| 0.681 |
| Male | 20 | 24 |
|
|
Female | 19 | 19 |
|
| Age (years) | 53.6±6.4 | 51.2±5.6 | 0.425 |
| Narrow parts |
|
|
|
| Cervical
oesophagus | 6 | 8 | 0.699 |
| Upper
thoracic esophagus | 9 | 9 | 0.815 |
| Middle
thoracic esophagus | 14 | 13 | 0.586 |
| Lower
thoracic esophagus | 10 | 13 | 0.644 |
| Narrow etiology |
|
|
|
|
Esophageal cancer early after
ESD | 12 | 14 | 0.862 |
|
Esophageal cancer anastomotic
stenosis after radical surgery | 18 | 20 | 0.974 |
|
Others | 9 | 9 | 0.815 |
Improvement of postoperative
esophageal stricture
In this study, patients with esophageal stricture
were diagnosed by esophageal angiography. The improvement of
esophageal stenosis in the treatment group was significantly better
than that of the control group at 2 and 4 months after treatment,
respectively (P=0.002, 0.013). However, there was no significant
difference in esophageal stenosis between the two groups at 15 days
and 1 month after operation, respectively (P=0.107, 0.128, Fig. 1).
Recurrence time of postoperative
esophageal stricture
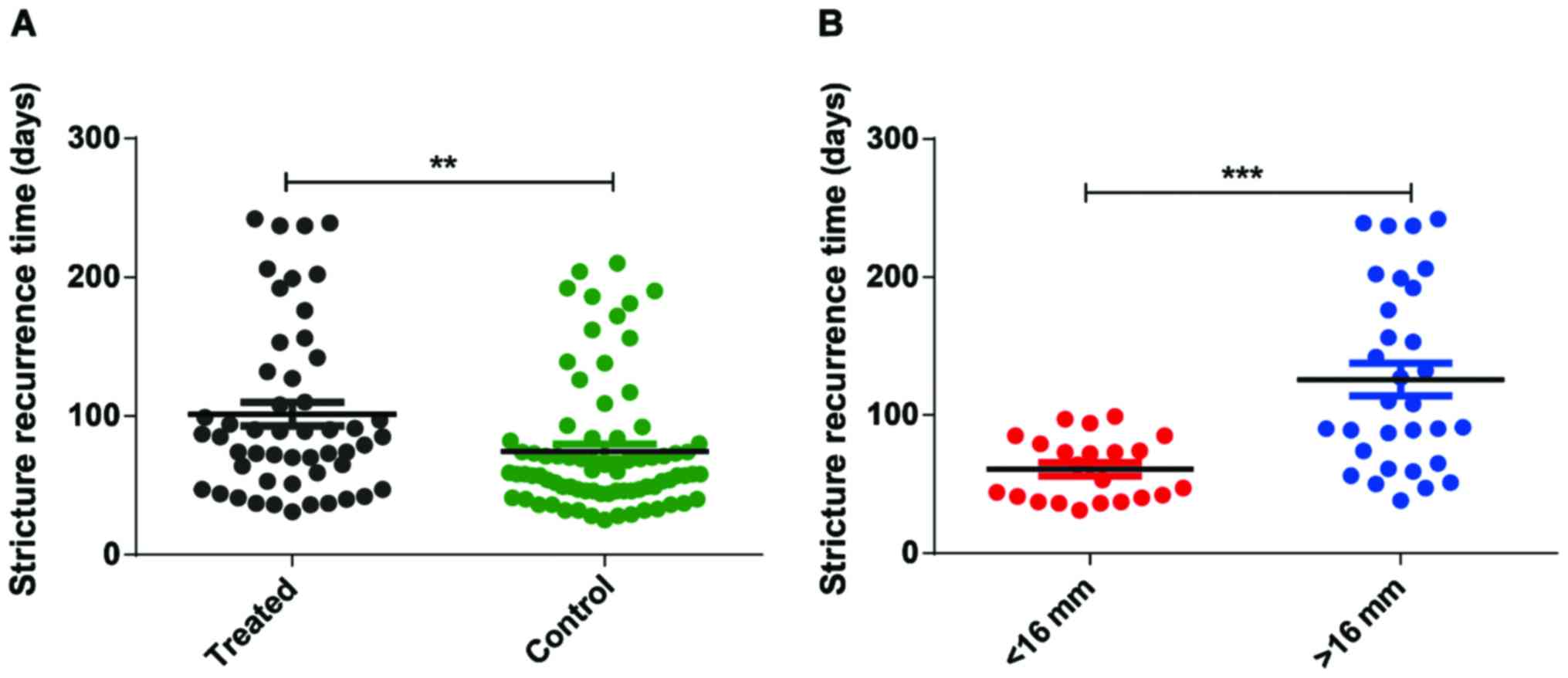
The recurrence rate of esophageal stricture in the
treatment and control group was 62.2% (51/82) and 77.2% (78/101)
within the 1-year follow-up, respectively (P=0.027). The recurrence
time of stenosis in the treatment group (101.4±8.6 days) was
markedly longer than that of the control group (75.4±5.2 days,
P=0.006). Furthermore, the recurrent time of the >16-mm subgroup
was also significantly longer than that of the <16-mm subgroup
(P<0.001, Fig. 2).
Adverse events and complications
There were 3 and 4 cases of postoperative bleeding
in the treatment and control group, respectively (P=0.916). Local
spraying of norepinephrine was administered to those patients for
hemostasis. Five patients in the treatment group experienced
postoperative fever but recovered after given physical cooling. No
patient had mediastinal emphysema, peri-esophageal abscess or
esophageal perforation during follow-up.
Discussion
The impact of esophageal stricture has been
increasingly expanding with the clinical application of esophageal
cancer surgery, radiotherapy and ESD and other new technologies.
Esophageal stenosis dilatation includes the probe dilation and the
balloon dilatation. Probe dilation was first developed dating back
to the 16th century, represented by Savary-Gilliard. Balloon
dilatation, performed in our study, was first proposed by Scolapio
(12). Hagel et al (13) retrospectively analyzed 368 cases of
esophageal stenosis from January 2002 to December 2011. A total of
8 cases experienced perforation, of which 1 patient in the probe
expansion group died. The total perforated rate was 0.54% (8/1479),
and the perforation rate of benign esophageal stenosis was 0.3%
(3/912). The results showed that despite lower perforation rate,
the balloon dilatation was much safer than that of the probe
dilation, which might be explained by the stronger destructive
effect of the probe. Glucocorticoids can not only inhibit the
exudation of inflammatory cells, granulation tissue proliferation
and submucosal tissue fibrosis, but also attenuate the activation
and migration of inflammatory cells and fibroblasts, reduce the
collagen synthesis and collagen degradation, and finally inhibit
the esophageal stenosis after the expansion of scar formation
(14). In this study, local
injection of triamcinolone acetonide was introduced to reduce the
scar formation after esophageal balloon dilatation.
It has been reported that steroid combined with
endoscopic distension is applied in esophageal benign stenosis
(15,16). The application of endoscopic dilation
and submucosal injection of triamcinolone acetonide in the
treatment of benign esophageal stenosis also achieved better
curative effect. However, some studies have found that the effect
of the combination treatment may be related to the stenosis
extent.
Our data showed that all patients had significant
improvement in swallowing and dilated symptoms at the end of
treatment. The combination treatment group showed a better relief
compared to that of the control group at 15 days and 1 month after
operation, but the difference was not statistically significant.
However, the degree of esophageal stenosis in the treatment group
at 2 and 4 months after treatment was significantly better than
that of the control group, the difference was statistically
significant. The recurrence time of treatment group was
significantly longer than that of control group, indicating that
hormone treatment combined with balloon dilatation had a better
effect than that of simple esophageal dilation treatment. Long-term
prognosis achieved the same result. The incidence of short-term
restenosis after endoscopic dilatation was higher in the control
group than that of the treatment group, suggesting that endoscopic
balloon dilation and submucosal triamcinolone acetonide injection
could prolong the short-term restenosis of esophagus and reduce the
incidence rate of recent restenosis.
In addition, the injection of triamcinolone
acetonide after endoscopic dilation could effectively reduce tissue
damage, inflammatory exudation and inflammatory cell aggregation,
inhibit fibroblast activity, and finally reduce or alleviate the
forming of scars. The specific mechanisms, however, need to be
further clarified. Clinical evidence also revealed that the
expansion extent is positively correlated with recurrence time of
esophageal stricture (17–19), which was consistent with our
findings. In our study, the recurrence time of esophageal stricture
in the <16-mm subgroup was significantly shorter than that in
the expanded >16-mm subgroup.
In this study, no patient had mediastinal emphysema,
esophageal abscess, esophageal perforation and other complications,
indicating that the degree of balloon expansion may not be
associated with the risk of esophageal perforation, which was
consistent with other researches (17,20).
In conclusion, our study showed that endoscopic
balloon dilatation combined with local injection of triamcinolone
acetonide in the treatment of benign esophageal stenosis is
superior to the simple balloon dilatation, which significantly
prolongs esophageal restenosis and reduces the duration of
esophageal dilatation. In addition, the effect of the combination
therapy is better when the degree of balloon dilatation is >16
mm.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
LQ and JC designed the study and performed the
experiments, WH, JY and YG collected the data, LQ and YG analyzed
the data, LQ and JC prepared the manuscript. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
the Third Affiliated Hospital of Soochow University (Changzhou,
China). Patients or their guardians provided written informed
consents for publication.
Patient consent for publication
Not applicable
Competing interests
The authors declare they have no competing
interests.
References
|
1
|
Altintas E, Kacar S, Tunc B, Sezgin O,
Parlak E, Altiparmak E, Saritas U and Sahin B: Intralesional
steroid injection in benign esophageal strictures resistant to
bougie dilation. J Gastroenterol Hepatol. 19:1388–1391. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wang GM, Liu DF, Xu YP, Meng T and Zhu F:
PET/CT imaging in diagnosing lymph node metastasis of esophageal
carcinoma and its comparison with pathological findings. Eur Rev
Med Pharmacol Sci. 20:1495–1500. 2016.PubMed/NCBI
|
|
3
|
Hirdes MM, Vleggaar FP and Siersema PD:
Stent placement for esophageal strictures: An update. Expert Rev
Med Devices. 8:733–755. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kochman ML, McClave SA and Boyce HW: The
refractory and the recurrent esophageal stricture: A definition.
Gastrointest Endosc. 62:474–475. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Miwata T, Oka S, Tanaka S, Kagemoto K,
Sanomura Y, Urabe Y, Hiyama T and Chayama K: Risk factors for
esophageal stenosis after entire circumferential endoscopic
submucosal dissection for superficial esophageal squamous cell
carcinoma. Surg Endosc. 30:4049–4056. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Mori H, Rafiq K, Kobara H, Fujihara S,
Nishiyama N, Oryuu M, Suzuki Y and Masaki T: Steroid permeation
into the artificial ulcer by combined steroid gel application and
balloon dilatation: Prevention of esophageal stricture. J
Gastroenterol Hepatol. 28:999–1003. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Isomoto H, Yamaguchi N, Nakayama T,
Hayashi T, Nishiyama H, Ohnita K, Takeshima F, Shikuwa S, Kohno S
and Nakao K: Management of esophageal stricture after complete
circular endoscopic submucosal dissection for superficial
esophageal squamous cell carcinoma. BMC Gastroenterol. 11:462011.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hanaoka N, Ishihara R, Takeuchi Y, Uedo N,
Higashino K, Ohta T, Kanzaki H, Hanafusa M, Nagai K, Matsui F, et
al: Intralesional steroid injection to prevent stricture after
endoscopic submucosal dissection for esophageal cancer: A
controlled prospective study. Endoscopy. 44:1007–1011. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Sato H, Inoue H, Kobayashi Y, Maselli R,
Santi EG, Hayee B, Igarashi K, Yoshida A, Ikeda H, Onimaru M, et
al: Control of severe strictures after circumferential endoscopic
submucosal dissection for esophageal carcinoma: Oral steroid
therapy with balloon dilation or balloon dilation alone.
Gastrointest Endosc. 78:250–257. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kataoka M, Anzai S, Shirasaki T, Ikemiyagi
H, Fujii T, Mabuchi K, Suzuki S, Yoshida M, Kawai T and Kitajima M:
Efficacy of short period, low dose oral prednisolone for the
prevention of stricture after circumferential endoscopic submucosal
dissection (ESD) for esophageal cancer. Endosc Int Open.
3:E113–E117. 2015.PubMed/NCBI
|
|
11
|
Yamaguchi N, Isomoto H, Nakayama T,
Hayashi T, Nishiyama H, Ohnita K, Takeshima F, Shikuwa S, Kohno S
and Nakao K: Usefulness of oral prednisolone in the treatment of
esophageal stricture after endoscopic submucosal dissection for
superficial esophageal squamous cell carcinoma. Gastrointest
Endosc. 73:1115–1121. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Scolapio JS, Pasha TM, Gostout CJ, Mahoney
DW, Zinsmeister AR, Ott BJ and Lindor KD: A randomized prospective
study comparing rigid to balloon dilators for benign esophageal
strictures and rings. Gastrointest Endosc. 50:13–17. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Hagel AF, Naegel A, Dauth W, Matzel K,
Kessler HP, Farnbacher MJ, Hohenberger WM, Neurath MF and Raithel
M: Perforation during esophageal dilatation: A 10-year experience.
J Gastrointestin Liver Dis. 22:385–389. 2013.PubMed/NCBI
|
|
14
|
Kochhar R and Makharia GK: Usefulness of
intralesional triamcinolone in treatment of benign esophageal
strictures. Gastrointest Endosc. 56:829–834. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hamad M: Article conflates academic
standards at UMST with student radicalisation. BMJ. 351:h40322015.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ramage JI Jr, Rumalla A, Baron TH, Pochron
NL, Zinsmeister AR, Murray JA, Norton ID, Diehl N and Romero Y: A
prospective, randomized, double-blind, placebo-controlled trial of
endoscopic steroid injection therapy for recalcitrant esophageal
peptic strictures. Am J Gastroenterol. 100:2419–2425. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Park JY, Song HY, Kim JH, Park JH, Na HK,
Kim YH and Park SI: Benign anastomotic strictures after
esophagectomy: Long-term effectiveness of balloon dilation and
factors affecting recurrence in 155 patients. AJR Am J Roentgenol.
198:1208–1213. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kim CG, Choi IJ, Lee JY, Cho SJ, Lee JH,
Ryu KW, Park SR, Bae JM and Kim YW: Effective diameter of balloon
dilation for benign esophagojejunal anastomotic stricture after
total gastrectomy. Surg Endosc. 23:1775–1780. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Huang Q, Zhong J, Yang T, Li J, Luo K,
Zheng Y, Yang H and Fu J: Impacts of anastomotic complications on
the health-related quality of life after esophagectomy. J Surg
Oncol. 111:365–370. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Fan Y, Song HY, Kim JH, Park JH,
Ponnuswamy I, Jung HY and Kim YH: Fluoroscopically guided balloon
dilation of benign esophageal strictures: Incidence of esophageal
rupture and its management in 589 patients. AJR Am J Roentgenol.
197:1481–1486. 2011. View Article : Google Scholar : PubMed/NCBI
|