Article
GLP‑1 receptor agonist on cardiovascular complications of diabetes mellitus
- Authors:
-
View Affiliations / Copyright
Affiliations:
Department of Cardiovascular Medicine (II), Tengzhou Central People's Hospital, Tengzhou, Shandong 277500, P.R. China, Department of Internal Medicine, Tengzhou Central People's Hospital, Tengzhou, Shandong 277500, P.R. China
-
Pages:
2259-2265
|
Published online on:
January 20, 2020
https://doi.org/10.3892/etm.2020.8439
- Expand metrics +
Metrics:
Total
Views: 0
(Spandidos Publications: | PMC Statistics:
)
Metrics:
Total PDF Downloads: 0
(Spandidos Publications: | PMC Statistics:
)
This article is mentioned in:
Abstract
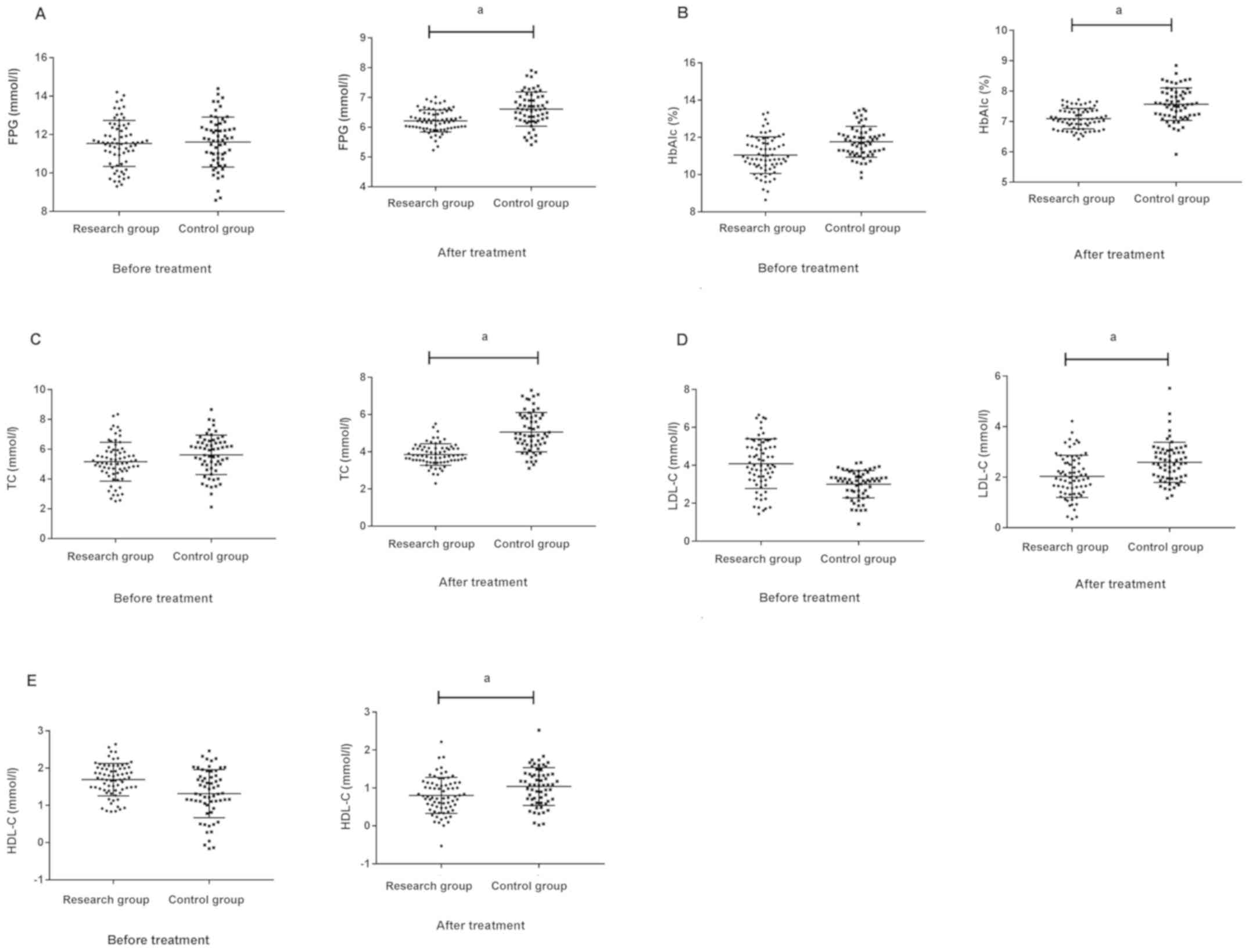
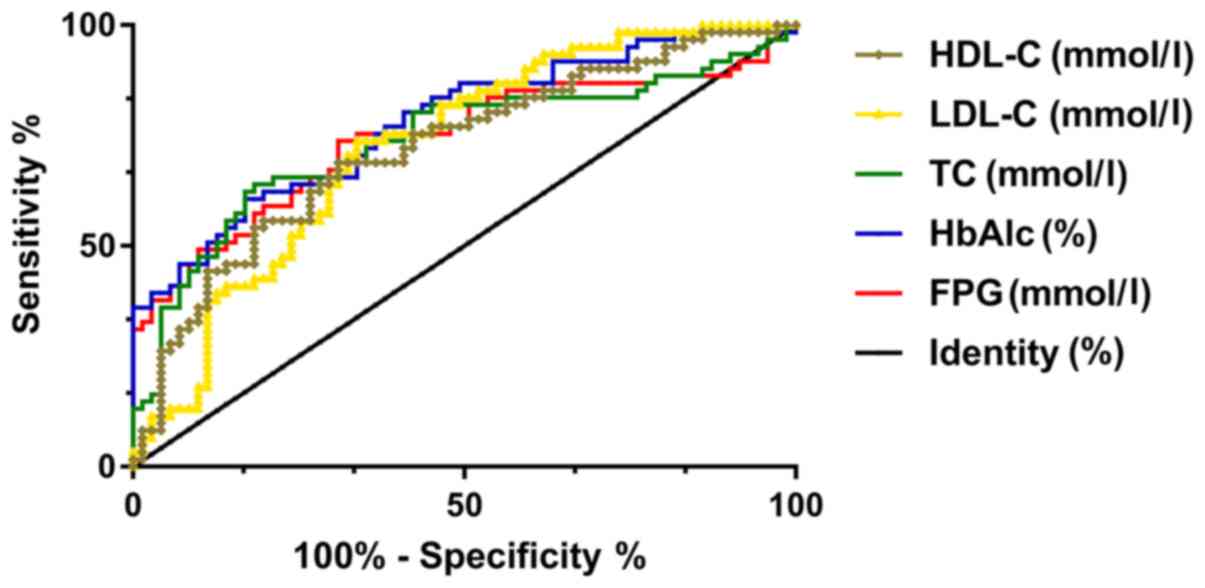
Effects of glucagon‑like peptide‑1 (GLP‑1) receptor agonist on cardiovascular complications of diabetes mellitus (DM) were investigated. In total, 132 DM patients treated in Tengzhou Central People's Hospital from April 2013 to September 2016 were included. Of these, 71 cases treated with basic drugs plus GLP‑1 were the research group, and 61 cases treated with glipizide controlled release tablets the control group. The improvement of clinical efficacy of patients in the two groups after treatment was observed. The concentrations of FPG, HbAlc, TC, LDL‑C, and HDL‑C in serum of patients in the two groups before and after treatment were compared, and the incidence rate of cardiovascular disease complications of diabetes was recorded. Expression of FPG, HbAlc, TC, LDL‑C, and HDL‑C of patients in the two groups were further detected. ROC curve was drawn to analyze its predictive value. In terms of markedly effective treatment rate and overall effective rate, the research group was significantly better than the control group (P<0.05). After treatment, the concentrations of FPG, HbAlc, TC, LDL‑C, and HDL‑C in serum of patients in the research group were significantly lower than those in the control group (P<0.05). The incidence rate of cardiovascular diseases and residual vascular risks in the research group were significantly higher than those in the control group (P<0.05). After treatment, the AUC of FPG, HbAlc, TC, LDL‑C, and HDL‑C in serum for predicting cardiovascular complications in DM patients were, respectively, 0.742, 0.780, 0.737, 0.726, and 0.721. In conclusion, GLP‑1 receptor agonist can improve the clinical efficacy of patients. Through ROC curve, FPG, HbAlc, TC, LDL‑C and HDL‑C can be used as predictors of cardiovascular complications in DM patients, which has high clinical value.
View References
|
1
|
American Diabetes Association: Standards
of medical care in diabetes - 2016 abridged for primary care
providers. Clin Diabetes. 34:3–21. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
American Diabetes Association: Diagnosis
and classification of diabetes mellitus. Diabetes Care. 33 (Suppl
1):S62–S69. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
American Diabetes Association: (2)
Classification and diagnosis of diabetes. Diabetes Care. 38
(Suppl):S8–S16. 2015. View Article : Google Scholar
|
|
4
|
Zinman B, Wanner C, Lachin JM, Fitchett D,
Bluhmki E, Hantel S, Mattheus M, Devins T, Johansen OE, Woerle HJ,
et al EMPA-REG OUTCOME Investigators, : Empagliflozin,
cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J
Med. 373:2117–2128. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Go AS, Mozaffarian D, Roger VL, Benjamin
EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, et al
American Heart Association Statistics Committee and Stroke
Statistics Subcommittee, : Executive summary: heart disease and
stroke statistics - 2013 update: a report from the American Heart
Association. Circulation. 127:143–152. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Low Wang CC, Hess CN, Hiatt WR and
Goldfine AB: Clinical update: Cardiovascular disease in diabetes
mellitus: Atherosclerotic cardiovascular disease and heart failure
in type 2 diabetes mellitus - mechanisms, management, and clinical
considerations. Circulation. 133:2459–2502. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Nauck MA, Kleine N, Orskov C, Holst JJ,
Willms B and Creutzfeldt W: Normalization of fasting hyperglycaemia
by exogenous glucagon-like peptide 1 (7–36 amide) in type 2
(non-insulin-dependent) diabetic patients. Diabetologia.
36:741–744. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Drucker DJ and Nauck MA: The incretin
system: Glucagon-like peptide-1 receptor agonists and dipeptidyl
peptidase-4 inhibitors in type 2 diabetes. Lancet. 368:1696–1705.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Basu S, Yoffe P, Hills N and Lustig RH:
The relationship of sugar to population-level diabetes prevalence:
an econometric analysis of repeated cross-sectional data. PLoS One.
8:e578732013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ha KH and Kim DJ: Trends in the Diabetes
Epidemic in Korea. Endocrinol Metab (Seoul). 30:142–146. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Monami M, Adalsteinsson JE, Desideri CM,
Ragghianti B, Dicembrini I and Mannucci E: Fasting and
post-prandial glucose and diabetic complication. A meta-analysis.
Nutr Metab Cardiovasc Dis. 23:591–598. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Fowler MJ: Microvascular and macrovascular
complications of diabetes. Clin Diabetes. 26:77–82. 2008.
View Article : Google Scholar
|
|
13
|
Malik VS, Popkin BM, Bray GA, Després JP
and Hu FB: Sugar-sweetened beverages, obesity, type 2 diabetes
mellitus, and cardiovascular disease risk. Circulation.
121:1356–1364. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zhang Y, Hu G, Yuan Z and Chen L:
Glycosylated hemoglobin in relationship to cardiovascular outcomes
and death in patients with type 2 diabetes: A systematic review and
meta-analysis. PLoS One. 7:e425512012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Gaster B and Hirsch IB: The effects of
improved glycemic control on complications in type 2 diabetes. Arch
Intern Med. 158:134–140. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
UK Prospective Diabetes Study (UKPDS)
Group, : Intensive blood-glucose control with sulphonylureas or
insulin compared with conventional treatment and risk of
complications in patients with type 2 diabetes (UKPDS 33). Lancet.
352:837–853. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Shichiri M, Kishikawa H, Ohkubo Y and Wake
N: Long-term results of the Kumamoto Study on optimal diabetes
control in type 2 diabetic patients. Diabetes Care. 23 (Suppl
2):B21–B29. 2000.PubMed/NCBI
|
|
18
|
Nadkarni P, Chepurny OG and Holz GG:
Regulation of glucose homeostasis by GLP-1. Prog Mol Biol Transl
Sci. 121:23–65. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Seino S, Shibasaki T and Minami K:
Dynamics of insulin secretion and the clinical implications for
obesity and diabetes. J Clin Invest. 121:2118–2125. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Gaisano HY, Macdonald PE and Vranic M:
Glucagon secretion and signaling in the development of diabetes.
Front Physiol. 3:3492012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Than NN and Newsome PN: A concise review
of non-alcoholic fatty liver disease. Atherosclerosis. 239:192–202.
2015. View Article : Google Scholar : PubMed/NCBI
|