Introduction
Osteopetrosis (OP) is a rare congenital bone
disorder (1) that is characterized
by systemic osteosclerosis due to a deficiency of or functional
defect in osteoclasts (2,3). As a result, fractures, anemia and nerve
compression, which may lead to deafness and/or blindness (4,5).
However, little is known on the complications and operative
difficulties associated with total hip arthroplasty (THA) in OP
patients. The present study presents a case of osteoarthritis of
the left hip joint in a patient with OP who was treated
successfully with THA at the Affiliated Hospital of Jiangsu
University (Zhenjiang, China). Additionally, a review of the
literature was performed to summarize our current knowledge of
clinical and imaging manifestations, pathogenesis, clinical
classification and treatment of OP, aiming to improve the diagnosis
and treatment of this disease.
Case report
In September 2015, A 52-year-old female patient with
OP presented to the Affiliated Hospital of Jiangsu University
(Zhenjiang, China) with a history of left hip pain and a limp, with
progressive activity limitation over the past 20 years. The patient
reported no previous history of fracture and had declined any
treatment during those two decades. There was no family history of
OP. X-ray examination of skull, chest, spine and pelvis performed 8
years ago in another hospital revealed manifestations of OP,
including systemic osteosclerosis and hyperplasia, obliteration of
the medullary cavity and the left hip space, and necrosis of the
femoral head. Although the left hip pain gradually subsided after a
conservative therapy such as reducing activity and taking pain
killers, there was no significant improvement in the disability.
One week before admission, the left hip pain worsened
significantly, and the patient was only able to walk for a maximum
of 50 m, beyond which the pain became unbearable.
At the time of admission, the patient's condition
was carefully evaluated based on physical examination, laboratory
tests and imaging studies. The physical examination revealed
tenderness and pain on percussion in the left hip. A test for the
range of hip motion showed 90° forward flexion, 0° backward
extension, 10° adduction and 10° abduction. In addition, the lower
extremities appeared to be of unequal length, and the left leg was
shown to be 2 cm shorter than the right. On neurological
examination, the patient had full motor strength in her lower
extremities with no obvious abnormality in skin sensation. The
findings of other examinations, including head and chest condition,
tapping pain in the liver and kidney areas, hearing and visual
acuity, peripheral blood supply, spinal activity and curvature and
tenderness in the spine area, were normal. The laboratory results
were notable for a platelet count of 1.69x1011 cells/l
(normal levels: 1.0-3.0x1011 cells/l), a reduced white
blood cell count of 3x109 cells/l (normal levels:
3.5-9.5x109 cells/l), a reduced red blood cell count of
3.78x1012 cells/l (normal levels:
3.8-5.1x1012 cells/l), a serum calcium concentration of
1.21 mmol/l (normal levels: 1.13-1.35 mmol/l) and a serum alkaline
phosphatase concentration of 91.5 U/l (normal levels: 50-135
U/l).
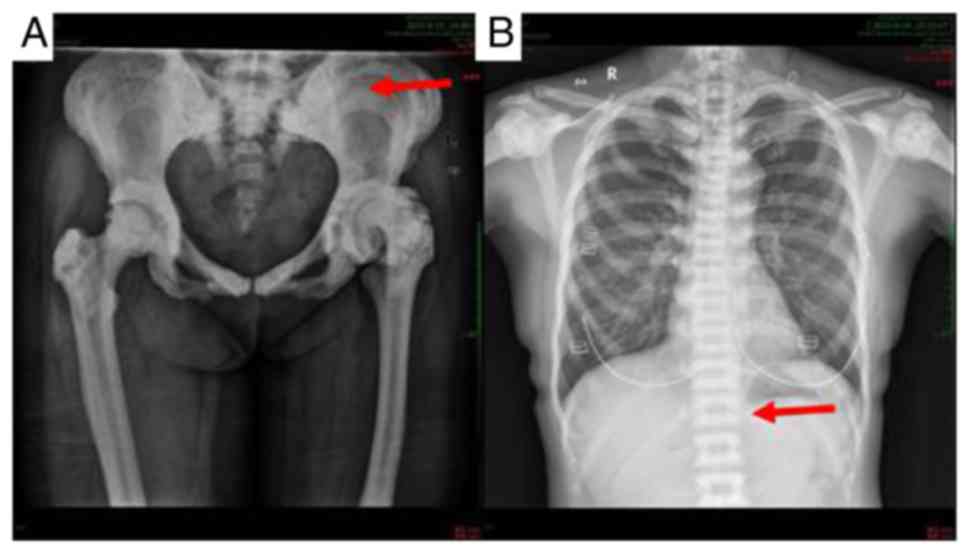
A radiological examination was performed. X-ray
imaging of the bilateral femora and pelvis revealed markedly
increased bone density with reduced left hip joint space, enlarged
left femoral head, marked left acetabular proliferation and
proximal migration of the left femoral head. In addition, the left
iliac bone and left femoral shaft were smaller compared with those
on the opposite side (Fig. 1A). An
X-ray of the spine and upper limbs revealed thickened and compact
superior and inferior endplates with loose and transparent
vertebral midbodies, thickened cortex of the bilateral upper humeri
and narrowed medullary cavity (Fig.
1B). Thus, the patient was diagnosed with OP complicated with
osteoarthritis of the left hip joint.
Given the history of OP and presumed poor bone
quality, THA was performed under epidural anesthesia via a
posterolateral approach. However, the surgery did not go smoothly,
as the femoral head was found to be deformed and articular
cartilage was destroyed by acetabular osteophyte proliferation
(Fig. 2). It was also difficult to
realign their position due to the bone stiffness and fragility.
Considering these factors, a biological total hip prosthesis was
selected. However, a fracture of the proximal femur occurred during
intramedullary reaming and the operation was terminated. During
surgery, the patient lost 300 ml of blood and was treated with
suspended red blood cells (300 ml) and plasma (225 ml). At the end
of the surgery, a drainage tube was inserted into the joint cavity
from the proximal 10-cm incision after confirming that bleeding had
ceased. On the first postoperative day, ~300 ml blood was observed
in the drainage tube.
The patient developed certain unexpected symptoms
postoperatively, including decreased muscle strength of the left
lower extremity, reduced skin sensation below the knee joint and
limited dorsal extension of the foot. At that time, it was
considered that the symptoms may due to sciatic nerve traction, and
the patient was treated with mecobalamin for neuronutrition, fluid
replacement, mannitol for detumescence, acupuncture and
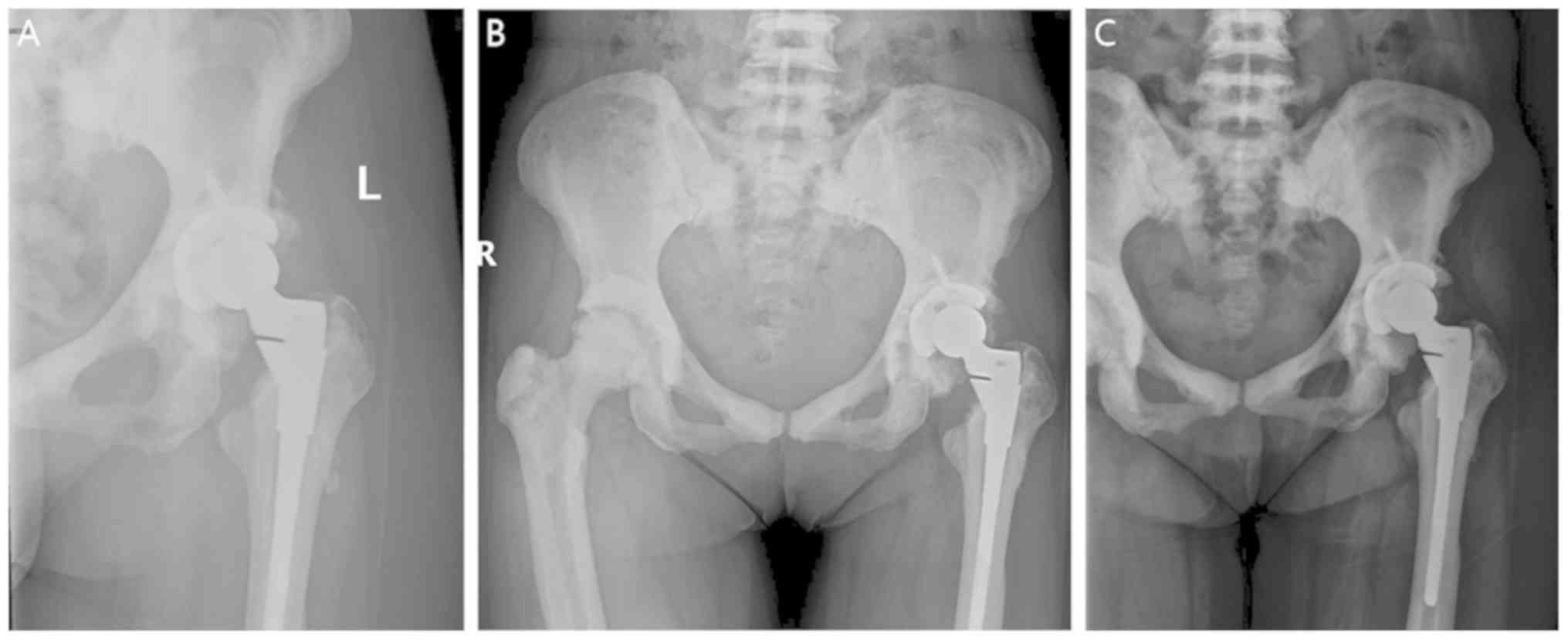
moxibustion. The symptoms were relieved after treatment. X-ray
imaging 2 weeks after surgery revealed satisfactory positioning of
the components, and the left femur was 2 cm longer compared with
the preoperative length. In addition, a radiolucent line was
observed (Fig. 3). Postoperative
pathology revealed that histological changes in the left hip were
consistent with chronic synovitis (Fig.
4). According to previous reports, the pathological changes of
OP may be summarized as follows (6,7):
Cortical hyperplasia and thickening; dense cancellous bone;
abnormal trabecular bone structure; decrease of intraosseous blood
vessels, fat and medullary substance; markedly sclerotic cortical
bone; and cancellous bone with unclear demarcation.
At 18 days after the surgery, the symptoms of
sciatic nerve injury in the left lower extremity of the patient had
significantly improved. The patient was able to perform walking
exercises using sticks without experiencing any pain in the left
hip joint, except for some numbness. On follow-up examinations at 6
months, 1 year and 2 years after surgery, the patient remained
asymptomatic and pain-free. Repeat X-ray imaging at these time
points revealed complete recovery from the fracture of the upper
left femur (Fig. 5A-C).
Discussion
Bone tissue is dynamically active, and under
physiological states, bone homeostasis is maintained by a balanced
formation of bone by osteoblasts, and bone resorption by
osteoclasts. OP, also referred to as ‘marble bone disease’,
generalized brittle osteosclerosis, ‘chalk bone’ or congenital
osteosclerosis, is a hereditary osteogenesis disease (6,8).
Previous studies suggested that osteosclerotic changes with
increased bone mass were observed due to a deficiency of or
functional defect in osteoclasts (4). The characteristic findings include bone
hyperplasia, disappearance of bone trabeculae, reduction or absence
of the medullary spaces, bony fragility and a high risk of fracture
(4). Bone resorption and remodeling
can be impaired as a result of the lack of osteoclasts. The bone
tissues become dense, where the bone appears as chalk-like or
marble-like. As a result, the weight-bearing ability is impaired
and fracture susceptibility increases. According to Stattin et
al (5), individuals with OP were
30 times more likely to suffer from recurrent fractures. When the
marrow cavity and skull are involved, hematopoietic disorders and
reflux of blood and cerebrospinal fluid may occur. Subsequent
manifestations may include bone marrow anemia, leukocytopenia,
thrombocytopenia, decreased haptoglobin, hydrocephalus, cerebellar
tonsil hernia and cranial nerve compression (9,10).
Generally, OP may be divided into two types:
Autosomal recessive OP (AROP) and autosomal dominant OP (ADOP).
AROP can be further be subdivided into 3 types according to the
time of onset and the progression rate of the disease. Type 1 is
malignant OP, which presents soon after birth and is characterized
by rapid progression, high mortality and low survival rates
(1). Type 2 is intermediate
autosomal recessive OP, and it is usually diagnosed within the
first decade of life due to incidental fractures. Patients with
this type are usually short, with a history of repeated fractures,
and it may be accompanied by osteomyelitis of the jaw (11). The characteristics of type 3,
carbonic anhydrase deficiency syndrome, include osteosclerosis with
near-medium, far-medium or complex renal tubular acidosis. The
majority of patients with ADOP, which is also known as benign
osteoporosis, are adults with a late onset, a stable condition,
relatively few symptoms and a good prognosis. Of patients with
ADOP, 50% are asymptomatic and 25% may suffer from backache. In
ADOP, compression of cranial nerves, coxa varus, lateral femoral
arch and other deformities; low incidence of anemia and
hepatosplenomegaly may also be found (12). The patient in the present case was 52
years old with mild symptoms and was admitted to the hospital due
to aggravated pain in the left hip. The patient's prognosis was
good following THA. Taking all the findings into consideration, the
diagnosis was benign OP.
The following classical radiographical
characteristics of OP are the minimum requirement to make the
diagnosis (13-15):
i) Parallel bands of dense bone giving the appearance of
‘bone-within-bone’ or ‘endobones’, which is often prominent in the
pelvis, long bones, phalanges and vertebrae; ii) vertebrae appear
as ‘sandwich vertebrae’ or ‘rugger-jersey’, where the superior and
inferior endplates exhibit high density, while the vertebral
midbodies appear to be normal; iii) diffuse sclerosis, affecting
the skull, spine, pelvis and appendicular bones; iv) skull changes,
including calvarial and basilar thickening, as well as poor sinus
development; v) bone modeling defects at the metaphyses of long
bones, such as the funnel-like appearance of the ‘Erlenmeyer flask’
deformity and characteristic lucent bands; and vi) ring-like
changes of the iliac wing. The X-ray manifestations of the disease
in the patient in the present case were consistent with these
characteristic findings.
OP is a genetic disease for which there is no
specific effective medical treatment (16). However, for patients affected by the
lethal autosomal recessive form of the disease, hematopoietic stem
cell transplantation (HSCT) is curative (17,18).
Successful HSCT leads to engraftment of macrophage-derived
osteoclasts of donor origin, resulting in remodeling of bone
structure and establishment of normal hematopoiesis (17). Early HSCT is considered to be
associated with favorable prognosis, which can relieve progressive
optic canal stenosis and control the deterioration of visual
function (19). However, this
remains controversial. According to a study by Overholt et
al (20), early HSCT in patients
without clinical or global neurological signs does not prevent the
onset or progression of neurological deterioration. Recently, HSCT
for AROP with a reduced-intensity conditioning regimen was proven
to be safe and effective, providing us with the ability to
performed HSCT on young patients with significant comorbidities
soon after diagnosis, with a lower risk of severe side effects
(21).
However, given that the transplant procedure itself
has a high risk of failure due to complications that may be
life-threatening, HSCT is not considered as an option for ADOP,
which rarely reduces life expectancy (22). Considering the high incidence of
fractures in patients with ADOP, surgical treatment is usually
required; however, this is complicated by the difficulty of working
with the extremely hard bones (23).
Plate osteosynthesis, intramedullary nailing and total joint
arthroplasty are all suitable options. Hasan et al (24) provided a summary of the difficulties
in treating OP fractures, including broken/bent drill bits,
infection, hard bone, bone overheating, periprosthetic fracture,
slow healing of fracture and narrow medullary canal, and concluded
that plate osteosynthesis may be preferred.
In addition to those specific treatments, for the
majority of patients with OP, supportive treatment is the most
important (25), including
painkillers and antibiotics for osteomyelitis (7). According to a study by Dunphy et
al (18), antibiotic therapy
combined with complete debridement of necrotic tissue, bacterial
culture and sensitivity testing, followed by suturing of soft
tissue, is the main therapeutic approach to patients with OP that
is complicated with osteomyelitis of the mandible. A sequence of
treatments, progressing from drainage, antibiotic therapy,
sequestrectomy, tooth extraction, saucerization, decortication, to
bone resection and oxygen therapy, has been proven to be valuable
in the management of osteomyelitis (26). For patients with benign OP,
non-operative treatment options include hip spica plaster cast,
traction, splint and avoidance of weight bearing (24). A low-calcium diet can create a
calcium-absorptive state and calcitriol can stimulate bone
resorption, which may delay the process of bone sclerosis (27).
The patient in the present case was diagnosed with
ADOP. The presence of anemia suggested the involvement of the bone
marrow cavity. As the case was complicated with osteoarthritis and
the patient had limited mobility, THA was selected as a suitable
treatment. Difficulty was experienced in reaming the femoral
medullary cavity due to the rigid, brittle bone and narrowed
medullary cavity in OP. Thus, it is strongly recommended that
surgeons performing this type of surgery prepare small reaming
tools and small prostheses prior to surgery. The patient developed
symptoms of sciatic nerve injury after the operation. The potential
reasons for this were as follows: i) Limb lengthening and sciatic
nerve traction; ii) compression by the retractors during prolonged
surgery; or iii) irrigation with iodine. In order to avoid
complications such as fracture and excessive stretching of the
sciatic nerve, gentle handling by surgeons is recommended. As
regards postoperative checks, routine blood tests, blood
biochemistry and pelvic X-ray should be reviewed regularly, and the
patient should be closely observed. Postoperative functional
exercises for patients with OP ought to be carried out as
usual.
In conclusion, our patient was diagnosed with ADOP
and hip osteoarthritis according to the clinical symptoms and
imaging examinations. THA in this case may not be completely
curative, but it was deemed as a useful method for reducing hip
pain and improving the quality of the patient's life. As the
previous literature on patients with OP complicated with hip
osteoarthritis who required THA is limited, the treatment approach
in the present case may represent a feasible option for such
patients. There were certain limitations to the present study: Only
one case was included, the follow-up was only 2 years, and genetic
examinations and information on the bone growth of the prosthesis
were lacking. Additional case reports with successful treatment are
required in the future to help reach a consensus on the optimal
treatment for such patients.
Acknowledgements
Not applicable.
Funding
This study was supported by the National Fund
Cultivation Program of Tong Ren Hospital Affiliated to Shanghai
Jiao Tong University School of Medicine(Shanghai, China, TRYJ(JC)03
) and Maternal and Child Health Care Project in Jiangsu Province
(F201656).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
XG collected and analyzed the data, participated in
the discussion, conducted the literature search, and wrote the
initial draft of the manuscript. QC performed the surgery, analyzed
and discussed the data, finalized the manuscript. XZ conceptualized
and oversaw the project, discussed and analyzed the data,
critically revised and finalized the manuscript. GZ participated in
the surgery and data discussion. All authors approved the final
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written consent was obtained from the patient for
the publication of this case report and all accompanying
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Palagano E, Menale C, Sobacchi C and Villa
A: Genetics of Osteopetrosis. Curr Osteoporos Rep. 16:13–25.
2018.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Moreno Garcia MS and Del Río-Martínez PS:
Osteopetrosis type II: Albers-Schonberg disease. Joint Bone Spine.
83(231)2016.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Pang Q, Chi Y, Zhao Z, Xing X, Li M, Wang
O, Jiang Y, Liao R, Sun Y, Dong J and Xia W: Novel mutations of
CLCN7 cause autosomal dominant Osteopetrosis type II (ADO-II) and
intermediate autosomal recessive Osteopetrosis (IARO) in Chinese
patients. Osteoporos Int. 27:1047–1055. 2016.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Machado Cde V, da Rocha MC and Telles PD:
Infantile Osteopetrosis associated with osteomyelitis. BMJ Case
Rep. 2015(pii: bcr2014208085)2015.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Stattin EL, Henning P, Klar J, McDermott
E, Stecksen-Blicks C, Sandström PE, Kellgren TG, Rydén P, Hallmans
G, Lönnerholm T, et al: SNX10 gene mutation leading to
Osteopetrosis with dysfunctional osteoclasts. Sci Rep.
7(3012)2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Nour M: Infantile malignant Osteopetrosis.
J Pediatrics. 163:1230–1230.e1. 2013. View Article : Google Scholar
|
|
7
|
Saigal A, Gopal M, Mohanty N and Misra SR:
Recurrent osteomyelitis of the mandible in Osteopetrosis: A common
complication of an uncommon disease. BMJ Case Rep. 2015(pii:
bcr2014208974)2015.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Alsahlawi A, Ekhzaimy A, Alshowair D and
Ajlan A: Decompressive cranioplasty in a patient with
osteopetrosis. World Neurosurg. 108:991.e1–991.e5. 2017.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Stella I, Vinchon M, Guerreschi P, De
Berranger E and Bouacha I: Case update on cranial Osteopetrosis:
Which is the role of the neurosurgeon? Childs Nerv Syst.
33:2181–2186. 2017.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Akutsu N, Koyama J, Kawamura A, Nagashima
T, Taniguchi M and Kohmura E: Endoscopic third ventriculostomy for
hydrocephalus in Osteopetrosis: A case report and review of the
literature. Childs Nerv Syst. 34:991–994. 2018.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Mosayebi Z, Mirfazaelian H, Khademi B,
Bagheri N and Daneshbod Y: Osteopetrosis in siblings. Intern Emerg
Med. 11:615–616. 2016.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Butscheidt S, Rolvien T, Kornak U, Schmidt
FN, Schinke T, Amling M and Oheim R: Clinical significance of DXA
and HR-pQCT in autosomal dominant Osteopetrosis (ADO II). Calcif
Tissue Int. 102:41–52. 2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Wu CC, Econs MJ, DiMeglio LA, Insogna KL,
Levine MA, Orchard PJ, Miller WP, Petryk A, Rush ET, Shoback DM, et
al: Diagnosis and management of Osteopetrosis: Consensus guidelines
from the Osteopetrosis working group. J Clin Endocrinol Metab.
102:3111–3123. 2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Stark Z: Osteopetrosis. Orphanet J Rare
Dis. 4(5)2009.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Hashemi Taheri AP, Radmard AR, Kooraki S,
Behfar M, Pak N, Hamidieh AA and Ghavamzadeh A: Radiologic
resolution of malignant infantile Osteopetrosis skeletal changes
following hematopoietic stem cell transplantation. Pediatric Blood
Cancer. 62:1645–1649. 2015.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Erkus S, Turgut A, Kose O and Kalenderer
Ö: Management of early-onset hip osteoarthritis in an adolescent
patient with OP tarda: A case report. J Pediatr Orthop B.
28:487–490. 2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Stepensky P, Grisariu S, Avni B, Zaidman
I, Shadur B, Elpeleg O, Sirin M, Hoenig M, Schuetz C, Furlan I, et
al: Stem cell transplantation for Osteopetrosis in patients beyond
the age of 5 years. Blood Adv. 3:862–868. 2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Dunphy L, Warfield A and Williams R:
Osteomyelitis of the mandible secondary to malignant infantile
Osteopetrosis in an adult. BMJ Case Rep. 12(pii:
e224452)2019.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Cao W, Wei W, Yu G, Wu Q and Qin M:
Comparison of optic canal diameter in children with malignant
infantile Osteopetrosis and normal children and the effects of
hematopoietic stem cell transplantation on the optic canal
diameter. J Pediatr Ophthalmol Strabismus. 56:35–42.
2019.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Overholt KM, Rose MJ, Joshi S, Herman GE,
Bajwa R, Abu-Arja R, Rangarajan HG and Horwitz EM: Hematopoietic
cell transplantation for a child with OSTM1 Osteopetrosis. Blood
Adv. 1:279–281. 2017. View Article : Google Scholar
|
|
21
|
Shadur B, Zaidman I, NaserEddin A, Lokshin
E, Hussein F, Oron HC, Avni B, Grisariu S and Stepensky P:
Successful hematopoietic stem cell transplantation for
Osteopetrosis using reduced intensity conditioning. Pediatr Blood
Cancer. 65(e27010)2018.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Maurizi A, Capulli M, Patel R, Curle A,
Rucci N and Teti A: RNA interference therapy for autosomal dominant
Osteopetrosis type 2 towards the preclinical development. Bone.
110:343–354. 2018.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Yamane K and Kai N: Anterior cervical
arthrodesis for chronic hangman's fracture in a patient with
Osteopetrosis: A case report. Arch Orthop Trauma Surg. 138:783–789.
2018.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Hasan O, Pathan AZ, Naqi H, Aqueel T,
Hashmi P and Lakdawala RH: Inheritance patterns, challenges, and
outcomes of fracture management in Osteopetrosis patients. CASE
series and review of pertinent literature. Ann Med Surg (Lond).
36:191–198. 2018.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Teti A and Econs MJ: Osteopetroses,
emphasizing potential approaches to treatment. Bone. 102:50–59.
2017.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Carvalho PHA, Moura LB, Real Gabrielli MF,
Cabrini Gabrielli MA and Antonio Pereira Filho V: Maxillary
osteomyelitis associated with Osteopetrosis: Systematic review. J
Craniomaxillofac Surg. 46:1905–1910. 2018.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Wang J, Liang Y, Zhang Q, Jiao J and Kan
W: Total joint arthroplasty in a patient with Osteopetrosis:
10-year follow-up. Orthopedics. 33:2010.doi:
10.3928/01477447-20100225-23. PubMed/NCBI View Article : Google Scholar
|