|
1
|
Farrell B, Godwin J, Richards S and Warlow
C: UK-TIA Study Group: The United Kingdom transient ischaemic
attack (UK-TIA) aspirin trial: Final results. J Neurol Neurosurg
Psychiatry. 54:1044–1054. 1991.PubMed/NCBI View Article : Google Scholar
|
|
2
|
CAPRIE Steering Committee: A randomised,
blinded, trial of clopidogrel versus aspirin in patients at risk of
ischaemic events (CAPRIE). Lancet 348: 1329-1339, 1996.
|
|
3
|
Braunwald E, Antman EM, Beasley JW, Califf
RM, Cheitlin MD, Hochman JS, Jones RH, Kereiakes D, Kupersmith J,
Levin TN, Pepine CJ, Schaeffer JW, Smith EE III, Steward DE and
Theroux P: ACC/AHA 2002 guideline update for the management of
patients with unstable angina and non-ST-segment elevation
myocardial infarction: summary article: a report of the American
College of Cardiology/American Heart Association Task Force on
Practice Guidelines (Committee on the Management of Patients With
Uns Table Angina). Circulation. 106:1893–1900. 2002.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Ng FH, Wong SY, Chang CM, Chen WH, Kng C,
Lanas AI and Wong BC: High incidence of clopidogrel-associated
gastrointestinal bleeding in patients with previous peptic ulcer
disease. Aliment Pharmacol Ther. 18:443–449. 2003.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Lai KC, Lam SK, Chu KM, Wong BC, Hui WM,
Hu WH, Lau GK, Wong WM, Yuen MF, Chan AO, et al: Lansoprazole for
the prevention of recurrences of ulcer complications from long-term
low-dose aspirin use. N Engl J Med. 346:2033–2038. 2002.PubMed/NCBI View Article : Google Scholar
|
|
6
|
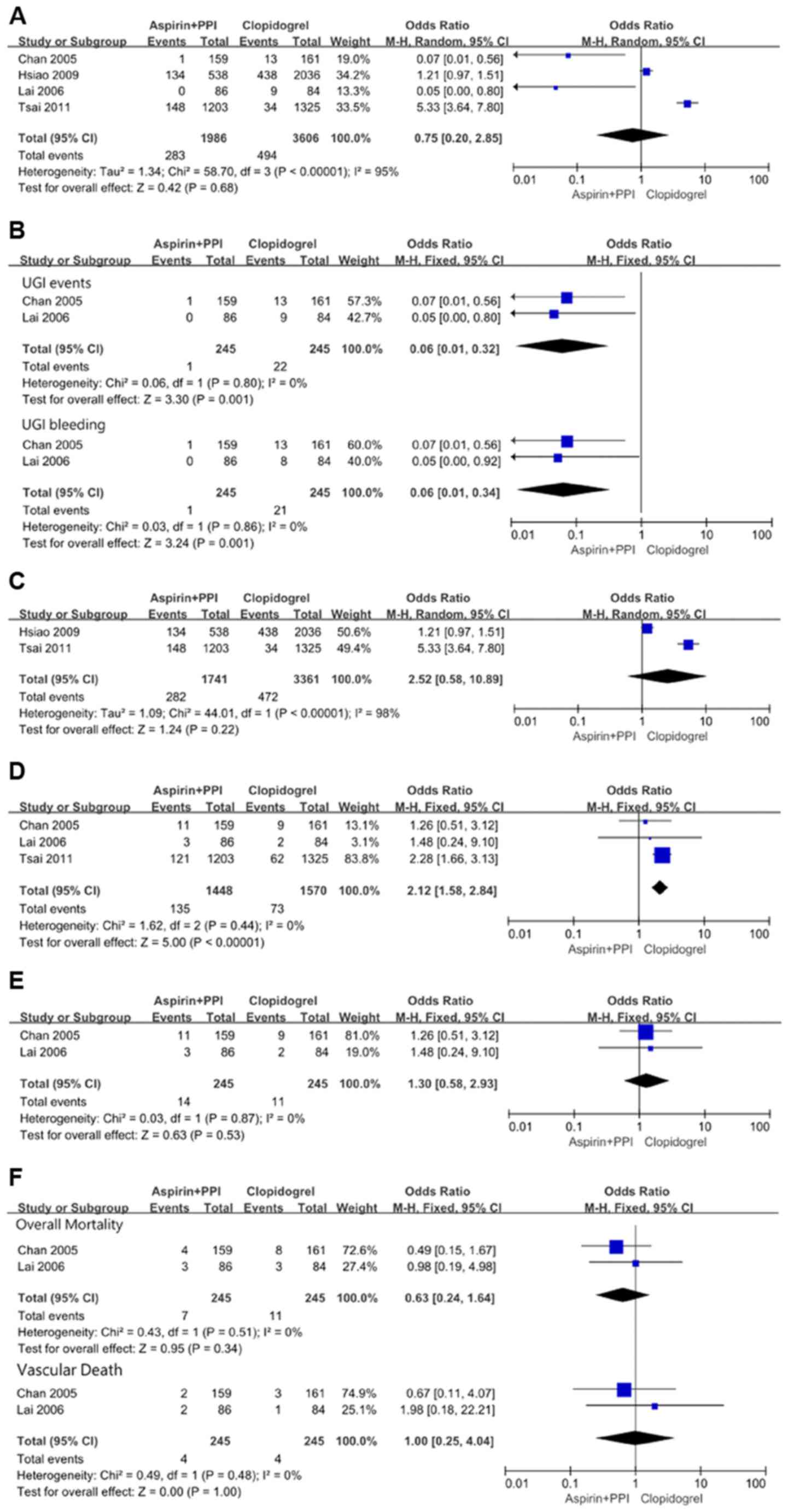
Chan FK, Ching JY, Hung LC, Wong VW, Leung
VK, Kung NN, Hui AJ, Wu JC, Leung WK, Lee VW, et al: Clopidogrel
versus aspirin and esomeprazole to prevent recurrent ulcer
bleeding. N Engl J Med. 352:238–244. 2005.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Lai KC, Chu KM, Hui WM, Wong BC, Hung WK,
Loo CK, Hu WH, Chan AO, Kwok KF, Fung TT, et al: Esomeprazole with
aspirin versus clopidogrel for prevention of recurrent
gastrointestinal ulcer complications. Clin Gastroenterol Hepatol.
4:860–865. 2006.PubMed/NCBI View Article : Google Scholar
|
|
8
|
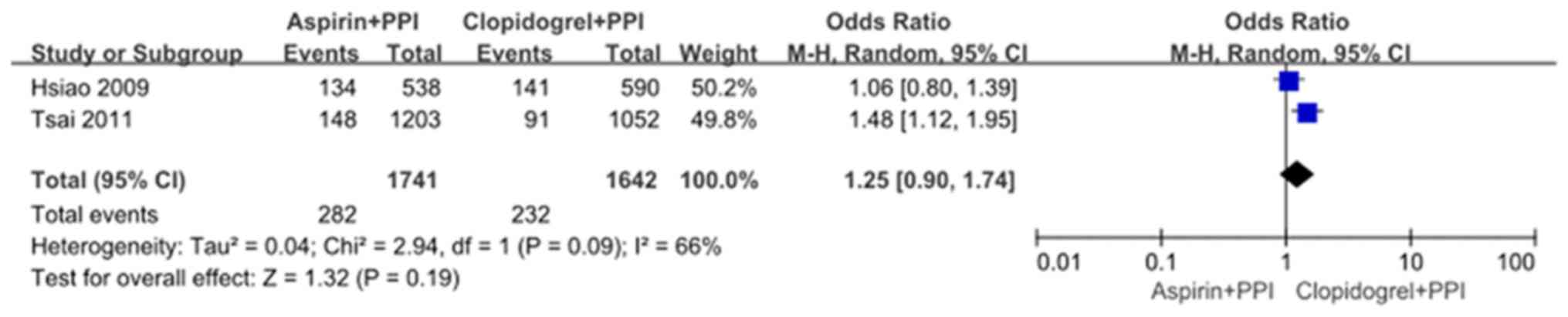
Tsai YW, Wen YW, Huang WF, Chen PF, Kuo KN
and Hsiao FY: Cardiovascular and gastrointestinal events of three
antiplatelet therapies: Clopidogrel, clopidogrel plus proton-pump
inhibitors, and aspirin plus proton-pump inhibitors in patients
with previous gastrointestinal bleeding. J Gastroenterol. 46:39–45.
2011.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Hsu PI, Lai KH and Liu CP: Esomeprazole
with clopidogrel reduces peptic ulcer recurrence, compared with
clopidogrel alone, in patients with atherosclerosis.
Gastroenterology. 140:791–798. 2011.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Hsiao FY, Tsai YW, Huang WF, Wen YW, Chen
PF, Chang PY and Kuo KN: A comparison of aspirin and clopidogrel
with or without proton pump inhibitors for the secondary prevention
of cardiovascular events in patients at high risk for
gastrointestinal bleeding. Clin Ther. 31:2038–2047. 2009.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Liberati A, Altman DG, Tetzlaff J, Mulrow
C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J
and Moher D: The PRISMA statement for reporting systematic reviews
and meta-analyses of studies that evaluate healthcare
interventions: Explanation and elaboration. BMJ. 339 (jul21
1)(b2700)2009.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Sterne JAC, Higgins JPT and Reeves BC: A
Cochrane Risk of Bias Assessment Tool: for Non-Randomized Studies
of Interventions (ACROBAT-NRSI). Version 1.0.0, September 24, 2014.
Retrieved from http://www.riskofbias.info.
Accessed: May 21, 2015.
|
|
13
|
Higgins JPT, Thompson SG, Deeks JJ and
Altman DG: Measuring inconsistency in meta-analyses. BMJ.
327:557–560. 2003.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Ma L, Elliott SN, Cirino G, Buret A,
Ignarro LJ and Wallace JL: Platelets modulate gastric ulcer
healing: Role of endostatin and vascular endothelial growth factor
release. Proc Natl Acad Sci USA. 98:6470–6475. 2001.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Ng FH, Wong BC, Wong SY, Chen WH and Chang
CM: Clopidogrel plus omeprazole compared with aspirin plus
omeprazole for aspirin-induced symptomatic peptic ulcers/erosions
with low to moderate bleeding/re-bleeding risk - a single-blind,
randomized controlled study. Aliment Pharmacol Ther. 19:359–365.
2004.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Hass WK, Easton JD, Adams HP Jr,
Pryse-Phillips W, Molony BA, Anderson S and Kamm B: Ticlopidine
Aspirin Stroke Study Group: A randomized trial comparing
ticlopidine hydrochloride with aspirin for the prevention of stroke
in high-risk patients. N Engl J Med. 321:501–507. 1989.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Savi P, Bernat A, Dumas A, Aït-Chek L and
Herbert JM: Effect of aspirin and clopidogrel on platelet-dependent
tissue factor expression in endothelial cells. Thromb Res.
73:117–124. 1994.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Kim KA, Park PW, Hong SJ and Park JY: The
effect of CYP2C19 polymorphism on the pharmacokinetics and
pharmacodynamics of clopidogrel: A possible mechanism for
clopidogrel resistance. Clin Pharmacol Ther. 84:236–242.
2008.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Sibbing D, Morath T, Stegherr J, Braun S,
Vogt W, Hadamitzky M, Schömig A, Kastrati A and von Beckerath N:
Impact of proton pump inhibitors on the antiplatelet effects of
clopidogrel. Thromb Haemost. 101:714–719. 2009.PubMed/NCBI
|
|
20
|
Gilard M, Arnaud B, Cornily JC, Le Gal G,
Lacut K, Le Calvez G, Mansourati J, Mottier D, Abgrall JF and
Boschat J: Influence of omeprazole on the antiplatelet action of
clopidogrel associated with aspirin: The randomized, double-blind
OCLA (Omeprazole CLopidogrel Aspirin) study. J Am Coll Cardiol.
51:256–260. 2008.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Juurlink DN, Gomes T, Ko DT, Szmitko PE,
Austin PC, Tu JV, Henry DA, Kopp A and Mamdani MM: A
population-based study of the drug interaction between proton pump
inhibitors and clopidogrel. CMAJ. 180:713–718. 2009.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Ho PM, Maddox TM, Wang L, Fihn SD, Jesse
RL, Peterson ED and Rumsfeld JS: Risk of adverse outcomes
associated with concomitant use of clopidogrel and proton pump
inhibitors following acute coronary syndrome. JAMA. 301:937–944.
2009.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Depta JP and Bhatt DL: Omeprazole and
clopidogrel: Should clinicians be worried? Cleve Clin J Med.
77:113–116. 2010.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Leontiadis GI, Sharma VK and Howden CW:
Systematic review and meta-analysis: Enhanced efficacy of
proton-pump inhibitor therapy for peptic ulcer bleeding in Asia - a
post hoc analysis from the Cochrane Collaboration. Aliment
Pharmacol Ther. 21:1055–1061. 2005.PubMed/NCBI View Article : Google Scholar
|