Introduction
Dry eye (DE) is a chronic inflammatory disease
caused by a lack of or excessive evaporation of tears, which causes
damage to the interpalpebral ocular surface and is associated with
symptoms of ocular discomfort (1).
DE affects ~14.5% of the world's population, with rising prevalence
(2). In the developed world, DE has
become one of the leading reasons for patients seeking
ophthalmological care (3).
Currently, cyclosporine and artificial tears have been the main
treatment approaches for chronic inflammatory DE (4,5).
However, to the best of our knowledge, the pathogenesis of DE has
not been fully elucidated.
Oxidative stress and increased levels of reactive
oxygen species (ROS) are known to serve important roles in the
development of DE (6). The close
relationship between lipid peroxidation-related membrane injury,
protein oxidation, ROS production and inflammation was confirmed in
patients and animal models of DE (7-9).
Previous studies have demonstrated that topically applied medicinal
plant extracts or tropical tree leaf extracts are effective for
stressed human corneal epithelial (HCE) cells and murine DE by
exhibiting anti-oxidative and anti-inflammatory properties
(10-12).
Furthermore, anti-oxidative glasses containing extracts of
medicinal plants were also indicated to be effective in improving
symptoms of DE, both reducing dryness and redness and increasing
tear break up time (TBUT) and Schirmer's test results (13).
Eurya japonica (EJ) is an ornamental plant
distributed in coastal areas, particularly in southern Korea,
southern China and south central Japan (14,15). The
leaves of Eurya emarginata have been used to treat ulcers or as a
diuretic in certain regions of Asia (14). Recent studies have suggested that EJ
has a variety of biological functions, including anti-cytotoxic,
anti-apoptotic, anti-angiogenic and anti-cancer effects (14,16-19).
Furthermore, chrysoeriol, eutigoside B and eutigoside C isolated
from EJ leaves were revealed to exert anti-oxidative and
anti-inflammatory effects (19-21).
However, to the best of our knowledge, no studies have investigated
the effectiveness of EJ in the treatment of inflammatory ocular
diseases.
Based on the aforementioned characteristics of EJ,
it was hypothesized that EJ extracts may exhibit an effect on
DE-associated inflammation and oxidative damage. Therefore, the
efficacy of topical EJ extracts in HCE cells and murine
experimental dry eye (EDE) was investigated.
Materials and methods
Preparation of EJ leaf extracts
EJ leaves were collected from the Jangseong province
of South Korea. Following collection, fresh leaves were washed with
distilled water and placed in a drying oven set to 40°C. After 10
days, when the water content of the leaves was <5% of their dry
weight, the leaves were grinded to a size of 0.5 mm using a
pin-type mill. The samples were extracted using a supercritical
CO2 extraction system (cat. no. 06RA06-104010-A0031;
ISA-SCFE system; Ilshin Autoclave Co., Ltd) at the Nano Bio
Research Center, Jangseong. Pure CO2 was applied to the
samples using a syringe pump. Each container was filled with leaves
weighing 100-125 g, and under a pressure of 200 bar, CO2
was used as the main extraction gas, C2H3OH
was used as the co-solvent and supercritical extraction was
performed (22,23). During the 2 h extraction process,
care was taken to control the temperature, pressure and
CO2 flow at 40°C, 200 bar and 60 ml/min, respectively,
and the co-solvent flow rate was 3 ml/min. EJ extract
concentrations with a density of 0.818 g/ml were collected by
supercritical fluid extraction at 40°C for 120 min and stored in a
clean vial at -20°C until subsequent use.
EJ extracts were diluted to concentrations of 0.001,
0.01 and 0.1% for both in vitro and in vivo
experiments. For in vitro experiments, EJ extracts were
diluted with phosphate-buffered saline (PBS; Biosesang). For animal
experiments, EJ extracts were diluted with balanced salt solution
(BSS; Alcon).
Cell culture and viability assay
HCE-2 [50.B1] cells (cat. no. CRL-11135; American
Type Culture Collection) at passage 28 were cultured at 37°C in a
humidified incubator containing 5% CO2. Cells were
maintained in EpiLife® (Gibco; Thermo Fisher Scientific,
Inc.) medium and supplemented with human corneal growth supplement
(1X; Gibco; Thermo Fisher Scientific, Inc.), 100 U/ml penicillin
and 100 µg/ml streptomycin (Gibco; Thermo Fisher Scientific,
Inc.).
Cell viability was measured using a water-soluble
tetrazolium salt (WST)-based EZ-Cytox assay kit (DoGen Bio Co.,
Ltd.) (24). HCE cells
(2x105 cells/well) were seeded in a 96-well plate and
incubated for 24 h at 37°C. Subsequently, the cells were
pre-treated with different concentrations of EJ extracts (0.001,
0.01 and 0.1% diluted in PBS) and PBS only for 1 h at 37°C. PBS
only-treated cells were used as a negative control. Cells were then
rinsed with PBS and cultured for an additional 24 h at 37°C. Plates
containing 10 µl WST (DoGen Bio Co., Ltd.) reagent solution in each
well were incubated at 37°C for an additional 3 h in a
CO2 incubator. The absorbance was measured at a
wavelength of 570 nm using an ELx808 absorbance microplate reader
(BioTek Instruments, Inc.). Cells treated with 200 µM hydrogen
peroxide (H2O2; Thermo Fisher Scientific,
Inc.) were used as a positive control to evaluate the effect of the
EJ extracts on cell viability following oxidative stress (25). To maximize the antioxidative effects
of EJ extracts, EJ extracts were diluted to several different
concentrations (0.001, 0.01 and 0.1%) with PBS. Cells were
pretreated with PBS only, 0.001, 0.01 or 0.1% EJ extracts for 1 h
at room temperature, followed by treatment with 200 µM
H2O2 at room temperature for 30 min. In
addition, cells untreated with EJ extract or
H2O2 were used as a negative control. EJ
extract-pre-treated and H2O2-treated cells
were used for subsequent in vitro assays. Each assay was
performed in triplicate.
Determination of intracellular ROS
levels
The levels of intracellular ROS were determined
using the CM-H2DCFDA kit (cat. no. C6827; Invitrogen; Thermo Fisher
Scientific, Inc.) according to the manufacturer's protocols, as
previously described (11). Briefly,
HCE cells were washed three times with PBS, cells were seeded in
PBS containing 10 µM chloromethyl-H2DCF-DA for 30 min at
37°C and washed another three times with PBS. Cellular fluorescence
was quantified using a fluorescent microscope (magnification, x40;
Eclipse TE300; Nikon Corporation) at an excitation setting of 515
nm and an emission setting of 550 nm. Dichlorodihydrofluorescein
diacetate (DCF-DA) fluorescence intensities were quantified using
ImageJ software (version 1.45; National Institutes of Health) and
expressed as percentages normalized to the negative control.
Mitochondrial membrane potential
assay
To determine whether EJ extracts alter the
mitochondrial function in cells under
H2O2-induced oxidative stress, a
5,5',6,6'-tetrachloro-1,1',3,3'-tetraethyl
benzimidazolylcarbocyanine iodide (JC-1) probe was used to assess
the loss of mitochondrial membrane potential (26). EJ extract-pre-treated and
H2O2-treated cells were cultured at 37°C on
6-well culture plates at a concentration of 1x105 cells
per well and incubated with 2 µM JC-1 (Invitrogen; Thermo Fisher
Scientific, Inc.) for 30 min at 37°C. Cells were washed with PBS
and incubated with 1 ml Accutase® solution (cat. no.
A1110501; Thermo Fisher Scientific, Inc) at 37°C for flow cytometry
analysis. The plates were carefully tapped to detach the cells
after 2 min of incubation. Suspended cells were then washed twice
with cold PBS and resuspended in cold PBS. Flow cytometer (BD
Accuri C6; BD Biosciences) and the flow cytometric analysis program
(BD Accuri C6 Software; version 202.8; BD Biosciences) were used to
quantify JC-1 fluorescence; a decrease in red fluorescence
(Fג585) accompanied by an increase in green
fluorescence (Fג510) indicated a decrease in
the mitochondrial membrane potential. Red fluorescence was
calculated relative to the percentage of the total fluorescence
(summation of red and green fluorescence).
Mouse model of dry eye and
experimental design
The research protocol was approved by the Chonnam
National University Medical School Research Institutional Animal
Care and Use Committee (approval no. CNU IACUC-H-2015-11).
Maintenance of animals and all in vivo experiments were
performed in accordance with the Association for Research in Vision
and Ophthalmology statement for the Use of Animals in Ophthalmic
and Vision Research.
Female C57BL/6 mice (age, 6-8 weeks; weight, 16.0±2
g; n=25) were obtained from Orient Bio Center and used following
experiments. The EDE mouse model was induced via subcutaneous
injection of 0.5 mg/0.2 ml scopolamine hydrobromide (Sigma-Aldrich;
Merck KGaA) four times per day (at 8 and 11 am and 2 and 5 pm) with
exposure to an air draft and 30% ambient humidity for seven days,
as previously described (27,28).
During the experiments, animal movement and food and water intake
were not restricted. The animals were housed at 22°C and 30%
humidity on a 12 h light/dark cycle.
The mice were randomly assigned to five groups based
on the topical treatment, which was administered for seven days, as
follows: i) EDE control mice that received no eye drops; ii) EDE
mice treated with BSS (Alcon); iii) EDE mice treated with 0.001% EJ
extract (Nano Bio Research Center); iv) EDE mice treated with 0.01%
EJ extract (Nano Bio Research Center) and v) EDE mice treated with
0.1% EJ extract (Nano Bio Research Center). EJ extracts were
diluted in BSS for each treatment group. A total of 2 µl eye drops
(BSS; 0.001; 0.01 or 0.1% EJ extract) were applied topically to
both eyes of the mice three times a day for seven days. Clinical
parameters, including tear volume, tear film break-up time and
corneal fluorescein staining scores (CFSS) (29) were measured on the seventh day of
treatment. Measurements were made 3 h following the last
scopolamine injection and eye drop application. After measurement
of the clinical parameters, the mice were anesthetized via
intraperitoneal injection of sodium pentobarbital (50 mg/kg).
Transcardial perfusion was then performed with phosphate buffer (pH
7.4) for euthanasia. A multiplex immunobead assay and measurement
of conjunctival ROS production using a CM-H2DCFDA kit were
performed following tissue harvesting. Each group consisted of five
mice. All experiments and analyses were repeated three times.
Measurement of cellular ROS
levels
Levels of intracellular ROS production were measured
using a CM-H2DCFDA kit according to the manufacturer's protocol, as
previously described (12). In
summary, the conjunctivas of the mice (5 eyes/group) were
surgically harvested, dipped in PBS, torn apart using scissors and
incubated at 37°C for 1 h in the presence of 0.5 mg/ml collagenase
type D (Roche Applied Science). Following incubation, the tissues
were disrupted by grinding using a syringe plunger and passed
through a cell strainer with a pore size of 100 mm. Cells were
centrifuged at 450 x g for 7 min at 4°C and washed with PBS and 10
µM DCF-DA (cat. no. D399; Molecular Probes; Thermo Fisher
Scientific, Inc.) and incubated for 30 min at 37°C. Cells were
analyzed using a FACSCalibur flow cytometer (BD Biosciences) at an
excitation wavelength of 480 nm and an emission wavelength of 530
nm. The results were expressed as the mean percentage increase of
DCF-DA fluorescence over the control tissue (conjunctival tissue
harvested from mice that were not exposed to desiccant stress or
topical treatment) with CellQuest software (version 5.2.1; BD
Biosciences).
Multiplex immunobead assay for
inflammatory cytokines and chemokines
A multiplex immunobead assay (cat. no.
LX200-XPON3.1; Luminex 200; Luminex Corporation) was used to
measure the concentrations of tumor necrosis factor (TNF)-α,
interleukin (IL)-1β, 10 kDa interferon gamma-induced protein 10
(IP-10) and monokine induced by interferon-γ (MIG) in the
conjunctivas, as previously described (30). Conjunctival tissues were collected
(five eyes per group) and pooled in a lysis buffer (TissueLyser;
Qiagen GmbH) containing protease inhibitor for 30 min. Cell
extracts were then centrifuged at 14,000 x g at 4°C for 15 min. The
supernatants were stored at -70°C until further analysis. After
centrifugation, each sample (10 µg/25 µl) was added to a well of a
96-well plate and incubated in the dark overnight at 4°C with 25 µl
of 1X beads conjugated to the following mouse
cytokine/chemokine-specific antibodies: Anti-mouse TNF-α (cat. no.
MCYTNFA-MAG; Milliplex®; Merck KGaA), anti-mouse IL-1β
(cat. no. MIL1B-MAG; Milliplex®; Merck KGaA), anti-mouse
IP-10 (cat. no. MIP10-MAG; Milliplex®; Merck KGaA),
anti-mouse MIG (cat. no. MMIG-MAG; Milliplex®; Merck
KGaA). Serial dilutions of each cytokine/chemokine (cat. no.
MTH17-8047; Milliplex®; Merck KGaA) were also added to
wells in the same plate to generate a standard curve. The next day,
the beads were washed with wash buffer (cat. no. L-WB;
Milliplex®; Merck KGaA) and mixed with 25 µl of 1X
biotinylated secondary cytokine/chemokine antibody mixture (cat.
no. MTH17-1047; Milliplex®; Merck KGaA) for 1 h at room
temperature, followed by washing with wash buffer and subsequent
incubation with 25 µl of streptavidin-phycoerythrin for 30 min
(both steps performed in the dark). After a final wash, the wells
were resuspended in 100 µl of assay buffer. The reactions were
detected following the addition of streptavidin-phycoerythrin
(Milliplex®; Merck KGaA) using the xPONENT software
analysis system (version 3.1; Luminex Corporation). The
concentrations of tissue cytokines and chemokines were calculated
from the standard curves of known concentrations of recombinant
mouse cytokines and chemokines.
Evaluation of tear film and ocular
surface parameters
The tear volume was measured using phenol
red-impregnated cotton threads (Zone-Quick Thread Tear Test; Oasis
Medical) as previously described (28). The thread was placed on the lower
conjunctival fornix at approximately one-third of the lower eyelid
distance from the lateral canthus for 20 sec. The length of the wet
red thread was measured in mm under a photomicroscope (light
microscope; magnification, x1; SMZ 1500; Nikon Corporation). A
standard curve was derived to convert distance into volume based on
the known uptake volume of basic stock solution (1,500 ml 0.9%
saline combined with 5 ml 5 M NaOH) over a 20 sec period.
TBUT and CFSS measurements were conducted as
previously described (31). Sodium
instilling was performed with 1 µl 1% sodium fluorescein into the
inferior conjunctival sac using a micropipette. After three blinks,
the TBUT was recorded in seconds using slit-lamp biomicroscopy
(magnification, x16; BQ-900; Haag-Streit) under cobalt blue light.
After a total of 90 seconds, punctate staining of the corneal
surface was evaluated by a researcher who was blinded to the
therapeutic conditions. For CFSS, each cornea was divided into four
quadrants that were individually scored. The intensity of corneal
fluorescein staining was calculated using a 4-point scale (0-4)
based on a previous study (29), as
follows: 0, absent; 1, slight punctate staining, <30 spots; 2,
punctate staining >30 spots, but non-diffuse; 3, diffuse
staining but no positive plaque; and 4, positive fluorescein
plaque. Total scores collected from the four quadrants,
respectively, were added to generate a final grade; the maximum
possible score was 16 points.
Statistical analysis
Data are presented as the mean ± standard deviation.
SPSS 18.0 (SPSS, Inc.) was used for analysis. The Kruskal-Wallis
test with Bonferroni post hoc analysis was used to compare cell
viability, cytokine and chemokine levels and DCF-DA value between
the groups. Normal distribution of the data was verified using the
Kolmogorov-Smirnov test. Statistical differences in tear volume,
TBUT and corneal fluorescein staining among the groups were
determined using one-way ANOVA followed by Dunnett's post hoc test.
Sphericity assumptions were evaluated with Mauchly's test, and in
the case of violation, the data were adjusted with an Epsilon
Greenhouse-Geisser statistic. P<0.05 was considered to indicate
a statistically significant difference.
Results
H2O2-induce
scytotoxicity in HCE cells
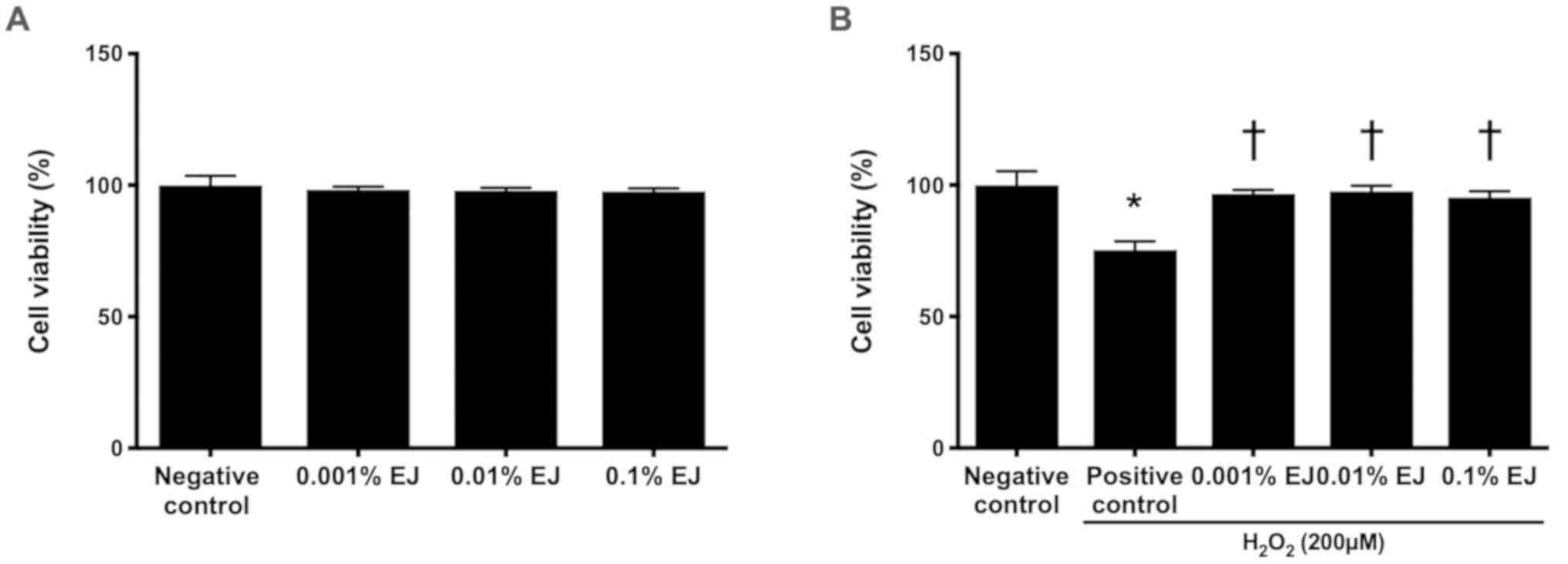
No statistically significant difference was
indicated on the viability of HCE cells between the 0.001, 0.01 and
0.1% EJ extract groups compared with the positive control (Fig. 1A). The positive control exhibited a
significant decrease in HCE cell viability compared with the
negative control (75.33±3.22%; P<0.01; Fig. 1B). The viability of HCE cells
pretreated with EJ extracts were 96.67±1.53% in the 0.001% EJ
group, 97.67±2.08% in the 0.01% EJ group and 95.33±2.31% in the
0.1% EJ group (all P<0.01 vs. the positive control; Fig 1B).
ROS levels in HCE cells
A significant increase in DCF-DA fluorescence was
observed in HCE cells following exposure to 200 µM
H2O2 (P<0.01 vs. negative control).
Pre-treatment with 0.01 and 0.1% EJ extracts significantly reduced
DCF-DA fluorescence intensity in a concentration-dependent manner
(0.001% EJ, P=0.9 vs. positive control; 0.01% EJ and 0.1% EJ,
P<0.05 vs. positive control or 0.001% EJ; Fig. 2).
Mitochondrial membrane potential in
HCE cells
In the mitochondrial membrane potential assay,
H2O2-treated HCE cells demonstrated a
significant decrease in red fluorescent signal compared with the
negative control (P<0.01). Compared with the
H2O2 positive control group, different
concentrations of EJ extracts significantly increased the red
fluorescence signal in a concentration-dependent manner (all
P<0.05 vs. the positive control; 0.1% EJ, P=0.03 vs. 0.001% EJ).
Compared with the negative control group, there was no significant
difference in the proportion of red fluorescence between the 0.01%
and 0.1% EJ groups (Fig. 3; Table I).
 | Table IPercentage of red fluorescence in the
negative control and hydrogen peroxide-treated cells with or
without EJ extract pretreatment. |
Table I
Percentage of red fluorescence in the
negative control and hydrogen peroxide-treated cells with or
without EJ extract pretreatment.
| Groups | Red fluorescence
(%) |
|---|
| Negative
control | 89.47±5.79 |
| Positive
control |
57.27±7.51a |
| 0.001% EJ |
72.67±2.67a,b |
| 0.01% EJ |
81.83±3.45b |
| 0.1% EJ |
87.83±2.93b,c |
ROS levels in conjunctival
tissues
In the DCF-DA assay, treatment with 0.01 and 0.1% EJ
extracts resulted in a significant decrease in ROS levels compared
with the EDE, BSS or 0.001% EJ group (all P<0.05). In addition,
the 0.1% EJ group showed a significantly lower DCF-DA staining
intensity compared with the 0.01% EJ group (P=0.02; Fig. 4).
Inflammatory cytokine and chemokine
levels in conjunctival tissues
The concentrations of TNF-α, IL-1β, IP-10 and MIG in
the 0.1% EJ group were significantly lower compared with the EDE,
BSS, 0.001% EJ and 0.01% EJ groups (all P<0.05). The 0.01% EJ
group also demonstrated significantly reduced TNF-α, IL-1β and
IP-10 levels compared with the EDE or BSS groups (all P<0.05)
and significantly reduced MIG levels compared with the EDE group
(P=0.02). No significant differences were observed in the
inflammatory cytokine and chemokine levels among the EDE, BSS and
0.001% EJ groups (Fig. 5).
 | Figure 5Levels of (A) TNF-α, (B) IL-1β, (C)
IP-10 and (D) MIG in the conjunctivas of EDE, BSS, and 0.001, 0.01
and 0.1% EJ extract groups. *P<0.05 vs. EDE;
†P<0.05 vs. BSS; ‡P<0.05 vs. 0.001% EJ
and §P<0.05 vs. 0.01% EJ. TNF-α, tumor necrosis
factor; IL-1β, interleukin-1β; IP-10, 10 kDa interferon
gamma-induced protein 10; MIG, monokine induced by interferon-γ;
EDE, experimental dry eye; BSS, balanced salt solution; EJ,
Eurya japonica. |
Clinical parameters in the tear film
and ocular surface
Following a period of seven days of desiccating
stress, the mean tear volumes were 0.020±0.007 µl (EDE group),
0.023±0.007 µl (BSS group), 0.025±0.006 µl (0.001% EJ group),
0.032±0.006 µl (0.01% EJ group) and 0.038±0.007 µl (0.1% EJ group).
The 0.01% EJ group indicated a significant increase in tear volume
compared with the EDE or BSS groups, and the 0.1% EJ group
indicated a significant increase in tear volume compared with the
EDE, BSS or 0.001% EJ groups (all P<0.05; Fig. 6A).
Following a period of seven days of desiccating
stress, the TBUT was demonstrated to be 1.50±0.26 sec in the EDE
group, 1.54±0.18 sec in the BSS group, 1.61±0.17 sec in the 0.001%
EJ group, 1.88±0.19 sec in the 0.01% EJ group and 1.96±0.26 sec in
the 0.1% EJ group. The 0.01% EJ and 0.1% EJ groups had
significantly increased TBUT compared with the EDE or BSS groups
(all P<0.05). In addition, the 0.1% EJ group exhibited a
significant increase in the TBUT compared with the 0.001% EJ group
(P<0.05 Fig. 6B).
Following a period of seven days of EDE induction in
mice, the CFSS scores were 14.80±1.03 (EDE group), 14.20±1.48 (BSS
group), 13.30±0.64 (0.001% EJ group), 8.20±1.40 (0.01% EJ group)
and 6.50±1.96 (0.1% EJ group). The 0.01% EJ and 0.1% EJ groups had
significantly decreased CFSS scores compared with the EDE, BSS or
0.001% EJ groups (all P<0.05 Fig.
6C and D).
Discussion
Oxidative stress is caused by an imbalance between
the anti-oxidant and the pro-oxidant system (6). When excess oxidative stress arises, the
balance is shifted in favor of the pro-oxidant system (32). ROS are natural by-products of normal
oxygen metabolism and participate in cell signaling and homeostasis
(33). A number of studies have
reported that oxidative stress serves an important role in a
variety of eye diseases, including uveitis, keratitis, age-related
cataracts and ocular inflammation (32,34-36).
Oxidative stress can damage the ocular surface via ROS production,
leading to visual impairment (37).
Chronic inflammation in DE is associated with
hyperosmolarity and tear film instability (38). In addition, oxidative stress is
closely associated with DE and is involved in the initiation and
progression of epithelial cell injury (39-41).
Previous studies have indicated that hyperosmolarity induces
oxidative stress, mitochondrial dysfunction and apoptosis in HCE
cells by stimulating ROS production and disrupting the balance of
oxygenases and anti-oxidant enzymes (42,43).
Oxidative stress may lead to inflammation and cell death in the
ocular surface epithelium of murine DE (10,13).
Currently, a number of different therapies, including
administration of cyclosporine and artificial tears, have been used
to treat DE (4,5). However, these agents have variable
therapeutic responses and are unable to achieve complete resolution
of inflammatory DE (11,31). Topical or local application of
anti-oxidative agents may be a novel treatment approach for DE
(10-12).
Among agents that have anti-inflammatory and anti-oxidant effects
for the treatment of DE, the efficacy of different concentrations
of EJ extracts was evaluated via topical application.
The leaves of EJ contain eutigoside B and C, which
exert anti-oxidative and anti-inflammatory effects through the
inhibition of pro-inflammatory cytokines (TNF-α and IL-6),
inducible nitric oxide synthase and cyclo-oxygenase-2(21). Chrysoeriol isolated from Eurya
ciliata protected osteoblasts from oxidative stress-induced
toxicity by inhibiting H2O2-induced nuclear
factor-κB ligand and IL-6 production (19).
In the present in vitro study, a variety of
concentrations of EJ extracts could maintain the viability of HCE
cells in the presence of H2O2. In addition,
the DCF-DA assay and mitochondrial membrane potential measurements
showed that the EJ extracts could reduce ROS production and protect
mitochondrial function. These findings demonstrated that EJ
extracts had anti-oxidative properties in HCE cells exposed to
oxidative stress. In the present in vivo study, the levels
of conjunctival intracellular ROS significantly decreased following
topical instillation of EJ extracts. In addition, topically applied
EJ extracts significantly decreased the expression of inflammatory
cytokines and chemokines TNF-α, IL-1β, IP-10 and MIG in the
conjunctiva. These results suggested that EJ extracts could have
anti-oxidative and anti-inflammatory properties in the ocular
surface following topical administration.
Previous studies have demonstrated that topical
administration of anti-oxidants could decrease inflammation on the
ocular surface of animal EDE (10-13).
It has also been demonstrated that topical application of
anti-inflammatory medicines exerted beneficial effects on tear film
stability and ocular surface integrity (44,45). In
the present study, the effects of topical EJ extracts on a variety
of clinical parameters, including the tear volume, TBUT and CFSS
scores were investigated using a mouse model of EDE. Despite
continuous exposure to desiccating stress and anticholinergic
treatment, 0.01% and 0.1% EJ extract-treated eyes showed an
increase in tear production, improvement in TBUT and reversal of
corneal epithelial damage as determined by the decrease in corneal
fluorescein uptake. The present study demonstrated that the
anti-oxidative and anti-inflammatory properties of EJ extracts
exibit a beneficial effect on the improvement of various tear film
and ocular surface parameters.
Collectively, EJ extracts protected the ocular
surface of epithelial cells against oxidative stress by inhibiting
ROS production. In addition, topical EJ extract application could
reduce the production of ROS and expression of inflammatory
molecules in the ocular surface, thereby improving the clinical
signs of murine DE. Therefore, topical EJ extract application could
ameliorate DE in terms of its oxidative, inflammatory and clinical
characteristics. Moreover, EJ extracts may exhibit potential as
therapeutic agents for the treatment of DE.
Acknowledgements
Not applicable.
Funding
The current study was supported by the Forest
Science & Technology Projects (grant no. S121313L50100) of the
Korean Forest Service and the CNUH Biomedical Research Institute
(grant nos. CRI 18093-1 and BCRI 20072)
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
KCY designed the experiment and revised the
manuscript. LL, RJ, YL, and YSJ performed the experiments. LL, LY,
WC, JHN and HJY analyzed and interpreted the data. LL and WC
drafted the manuscript. All authors read and approved the final
manuscript and agree to be accountable for all aspects of the
research in ensuring that the accuracy or integrity of any part of
the work are appropriately investigated and resolved.
Ethics approval and consent to
participate
This research protocol was approved by the Chonnam
National University Medical School Research Institutional Animal
Care and Use Committee. Maintenance of animals and all in
vivo experiments were performed in accordance with the
Association for Research in Vision and Ophthalmology statement for
the Use of Animals in Ophthalmic and Vision Research.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
No authors listed. The definition and
classification of dry eye disease. Report of the definition and
classification subcommittee of the international dry eye workshop
(2007). Ocul Surf. 5:75–92. 2007.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Paulsen AJ, Cruickshanks KJ, Fischer ME,
Huang GH, Klein BE, Klein R and Dalton DS: Dry eye in the beaver
dam offspring study: Prevalence, risk factors, and health-related
quality of life. Am J Ophthalmol. 157:799–806. 2014.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Gayton JL: Etiology, prevalence, and
treatment of dry eye disease. Clin Ophthalmol. 3:405–412.
2009.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Wan KH, Chen LJ and Young AL: Efficacy and
safety of topical 0.05% cyclosporine eye drops in the treatment of
dry eye syndrome: A systematic review and meta-analysis. Ocul Surf.
13:213–225. 2015.PubMed/NCBI View Article : Google Scholar
|
|
5
|
You IC, Li Y, Jin R, Ahn M, Choi W and
Yoon KC: Comparison of 0.1%, 0.18%, and 0.3% hyaluronic acid eye
drops in the treatment of experimental dry eye. J Ocul Pharmacol
Ther. 34:557–564. 2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Wakamatsu TH, Dogru M and Tsubota K:
Tearful relations: Oxidative stress, inflammation and eye diseases.
Arq Bras Oftalmol. 71:72–79. 2008.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Uchino Y, Kawakita T, Miyazawa M, Ishii T,
Onouchi H, Yasuda K, Ogawa Y, Shimmura S, Ishii N and Tsubota K:
Oxidative stress induced inflammation initiates functional decline
of tear production. PLoS One. 7(e45805)2012.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Shoham A, Hadziahmetovic M, Dunaief JL,
Mydlarski MB and Schipper HM: Oxidative stress in diseases of the
human cornea. Free Radic Biol Med. 45:1047–1055. 2008.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Yin Y, Zong R, Bao X, Zheng X, Cui H, Liu
Z and Zhou Y: Oxidative stress suppresses cellular autophagy in
corneal epithelium. Invest Ophthalmol Vis Sci. 59:3286–3293.
2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Choi W, Lee JB, Cui L, Li Y, Li Z, Choi
JS, Lee HS and Yoon KC: Therapeutic efficacy of topically applied
antioxidant medicinal plant extracts in a mouse model of
experimental dry eye. Oxid Med Cell Longev.
2016(4727415)2016.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Lee HS, Choi JH, Cui L, Li Y, Yang JM, Yun
JJ, Jung JE, Choi W and Yoon KC: Anti-inflammatory and
antioxidative effects of Camellia japonica on human corneal
epithelial cells and experimental dry eye: in vivo and in vitro
study. Invest Ophthalmol Vis Sci. 58:1196–1207. 2017.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Cui L, Lee HS, Li Y, Choi JH, Yun JJ, Jung
JE, Choi W and Yoon KC: Experimental and clinical applications of
Chamaecyparis obtusa extracts in dry eye disease. Oxid Med Cell
Longev. 2017(4523673)2017.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Choi W, Kim JC, Kim WS, Oh HJ, Yang JM,
Lee JB and Yoon KC: Clinical effect of antioxidant glasses
containing extracts of medicinal plants in patients with dry eye
disease: A multi-center, prospective, randomized, double-blind,
placebo-controlled trial. PLoS One. 10(e0139761)2015.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Park SY, Yang HC, Moon JY, Lee NH, Kim SJ,
Kang JH, Lee YK, Park DB, Yoo ES and Kang HK: Induction of the
apoptosis of HL-60 promyelocytic leukemia cells by Eurya
emarginata. Cancer Lett. 205:31–38. 2004.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Chung MG and Epperson BK: Clonal and
spatial genetic structure in Eurya emarginata (Theaceae). Heredity
(Edinb). 84 (Pt 2):170–177. 2000.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Park SY, Yang HC, Moon JY, Lee NH, Kim SJ,
Kang JH, Lee YK, Park DB, Yoo ES and Kang HK: The cytotoxicity of
eutigosides from Eurya emarginata against HL-60 promyelocytic
leukemia cells. Arch Pharm Res. 28:1047–1052. 2005.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Seo EJ, Kuete V, Kadioglu O, Krusche B,
Schröder S, Greten HJ, Arend J, Lee IS and Efferth T:
Antiangiogenic activity and pharmacogenomics of medicinal plants
from traditional korean medicine. Evid Based Complement Alternat
Med. 2013(131306)2013.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Yang Kuo LM, Zhang LJ, Huang HT, Lin ZH,
Liaw CC, Cheng HL, Lee KH, Morris Natschke SL, Kuo YH and Ho HO:
Antioxidant lignans and chromone glycosides from Eurya
japonica. J Nat Prod. 76:580–587. 2013.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Kim YH, Lee YS and Choi EM: Chrysoeriol
isolated from Eurya cilliata leaves protects MC3T3-E1 cells against
hydrogen peroxide-induced inhibition of osteoblastic
differentiation. J Appl Toxicol. 30:666–673. 2010.PubMed/NCBI View
Article : Google Scholar
|
|
20
|
Lee HJ, Oh TH, Yoon WJ, Kang GJ, Yang EJ,
Park SS, Lee NH, Kang HK and Yoo ES: Eutigoside C inhibits the
production of inflammatory mediators (NO, PGE (2), IL-6) by
down-regulating NF-kappaB and MAP kinase activity in LPS-stimulated
RAW 264.7 cells. J Pharm Pharmacol. 60:917–924. 2008.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Park SY, Lee HJ, Yoon WJ, Kang GJ, Moon
JY, Lee NH, Kim SJ, Kang HK and Yoo ES: Inhibitory effects of
eutigosides isolated from Eurya emarginata on the inflammatory
mediators in RAW264.7 cells. Arch Pharm Res. 28:1244–1250.
2005.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Kim C, Lee IH, Hyun HB, Kim JC, Gyawali R,
Lee SG, Lee J, Kim SH, Shim BS, Cho SK, et al: Supercritical fluid
extraction of citrus iyo hort. ex tanaka pericarp inhibits growth
and induces apoptosis through abrogation of STAT3 regulated gene
products in human prostate cancer xenograft mouse model. Integr
Cancer Ther. 16:227–243. 2017.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Sookwong P, Suttiarporn P, Boontakham P,
Seekhow P, Wangtueai S and Mahatheeranont S: Simultaneous
quantification of vitamin E, γ-oryzanols and xanthophylls from rice
bran essences extracted by supercritical CO2. Food Chem.
211:140–147. 2016.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Kim H, Roh HS, Kim JE, Park SD, Park WH
and Moon JY: Compound K attenuates stromal cell-derived growth
factor 1 (SDF-1)-induced migration of C6 glioma cells. Nutr Res
Pract. 10:259–264. 2016.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Kopalli SR, Cha KM, Jeong MS, Lee SH, Sung
JH, Seo SK and Kim SK: Pectinase-treated Panax ginseng ameliorates
hydrogen peroxide-induced oxidative stress in GC-2 sperm cells and
modulates testicular gene expression in aged rats. J Ginseng Res.
40:185–195. 2016.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Dalal S, Zha Q, Singh M and Singh K:
Osteopontin-stimulated apoptosis in cardiac myocytes involves
oxidative stress and mitochondrial death pathway: Role of a
pro-apoptotic protein BIK. Mol Cell Biochem. 418:1–11.
2016.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Yoon KC, De Paiva CS, Qi H, Chen Z, Farley
WJ, Li DQ, Stern ME and Pflugfelder SC: Desiccating environmental
stress exacerbates autoimmune lacrimal keratoconjunctivitis in
non-obese diabetic mice. J Autoimmun. 30:212–221. 2008.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Yoon KC, Ahn KY, Choi W, Li Z, Choi JS,
Lee SH and Park SH: Tear production and ocular surface changes in
experimental dry eye after elimination of desiccating stress.
Invest Ophthalmol Vis Sci. 52:7267–7273. 2011.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Pauly A, Brignole-Baudouin F, Labbė A,
Liang H, Warnet JM and Baudouin C: New tools for the evaluation of
toxic ocular surface changes in the rat. Invest Ophthalmol Vis Sci.
48:5473–5483. 2007.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Oh HJ, Li Z, Park SH and Yoon KC: Effect
of hypotonic 0.18% sodium hyaluronate eyedrops on inflammation of
the ocular surface in experimental dry eye. J Ocul Pharmacol Ther.
30:533–542. 2014.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Sung MS, Li Z, Cui L, Choi JS, Choi W,
Park MJ, Park SH and Yoon KC: Effect of topical
5-Aminoimidazole-4-carboxamide-1-β-d-ribofuranoside in a mouse
model of experimental dry eye. Invest Ophthalmol Vis Sci.
56:3149–3158. 2015.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Dogru M, Kojima T, Simsek C and Tsubota K:
Potential role of oxidative stress in ocular surface inflammation
and dry eye disease. Invest Ophthalmol Vis Sci. 59:DES163–DES168.
2018.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Devasagayam TP, Tilak JC, Boloor KK, Sane
KS, Ghaskadbi SS and Lele RD: Free radicals and antioxidants in
human health: Current status and future prospects. J Assoc
Physicians India. 52:794–804. 2004.PubMed/NCBI
|
|
34
|
Alió JL, Artola A, Serra A, Ayala MJ and
Mulet ME: Effect of topical antioxidant therapy on experimental
infectious keratitis. Cornea. 14:175–179. 1995.PubMed/NCBI
|
|
35
|
Gritz DC, Montes C, Atalla LR, Wu GS,
Sevanian A and Rao NA: Histochemical localization of superoxide
production in experimental autoimmune uveitis. Curr Eye Res.
10:927–931. 1991.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Erol Tinaztepe Ö, Ay M and Eser E: Nuclear
and mitochondrial DNA of age-related cataract patients are
susceptible to oxidative damage. Curr Eye Res. 42:583–588.
2017.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Pinazo Durán MD, Gallego Pinazo R, García
Medina JJ, Zanon Moreno V, Nucci C, Dolz Marco R, Martínez Castillo
S, Galbis Estrada C, Marco Ramírez C, López-Gálvez MI, et al:
Oxidative stress and its downstream signaling in aging eyes. Clin
Interv Aging. 9:637–652. 2014.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Craig JP, Nichols KK, Akpek EK, Caffery B,
Dua HS, Joo CK, Liu Z, Nelson JD, Nichols JJ, Tsubota K, et al:
TFOS DEWS II definition and classification report. Ocul Surf.
15:276–283. 2017.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Nakamura S, Shibuya M, Nakashima H,
Hisamura R, Masuda N, Imagawa T, Uehara M and Tsubota K:
Involvement of oxidative stress on corneal epithelial alterations
in a blink-suppressed dry eye. Invest Ophthalmol Vis Sci.
48:1552–1558. 2007.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Uchino Y, Kawakita T, Ishii T, Ishii N and
Tsubota K: A new mouse model of dry eye disease: Oxidative stress
affects functional decline in the lacrimal gland. Cornea. 31 (Suppl
1):S63–S67. 2012.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Wakamatsu TH, Dogru M, Matsumoto Y, Kojima
T, Kaido M, Ibrahim OM, Sato EA, Igarashi A, Ichihashi Y, Satake Y,
et al: Evaluation of lipid oxidative stress status in Sjögren
syndrome patients. Invest Ophthalmol Vis Sci. 54:201–210.
2013.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Li Y, Liu H, Zeng W and Wei J: Edaravone
protects against hyperosmolarity-induced oxidative stress and
apoptosis in primary human corneal epithelial cells. PLoS One.
12(e0174437)2017.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Deng R, Hua X, Li J, Chi W, Zhang Z, Lu F,
Zhang L, Pflugfelder SC and Li DQ: Oxidative stress markers induced
by hyperosmolarity in primary human corneal epithelial cells. PLoS
One. 10(e0126561)2015.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Lee HS, Jang JY, Lee SH, Im SK and Yoon
KC: Clinical effectiveness of topical cyclosporine a 0.05% after
laser epithelial keratomileusis. Cornea. 32:e150–e155.
2013.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Holland EJ, Darvish M, Nichols KK, Jones L
and Karpecki PM: Efficacy of topical ophthalmic drugs in the
treatment of dry eye disease: A systematic literature review. Ocul
Surf. 17:412–423. 2019.PubMed/NCBI View Article : Google Scholar
|