Introduction
The onset of depression and anxiety during the
antenatal stage of pregnancy is prominent (1,2).
According to the World Health Organization, it is a substantial
public and mental health concern for women of childbearing age
(3,4). Recent epidemiological studies suggest
that approximately 15% of all pregnant women worldwide suffer from
depression and anxiety-related disorders (5,6). These
levels have been reported to be even higher in low- and
middle-income countries (7,8).
Studies suggest a wide array of underlying
pathophysiological mechanisms that may predispose the onset of
these psychological disorders (9,10). For
instance, Leung and Kaplan (9)
suggested pregnancy-induced changes in the maternal hormones,
hypothalamus-pituitary axis (HP-axis), and levels of cortisol to be
the main biological mechanisms behind the development of depression
and anxiety. Meltzer-Brody (11)
supported these outcomes and reported that changes in the level of
hormones such as estrogen, estradiol, thyroxine, thyroid
stimulation hormone, or prolactin, particularly during the third
trimester, may lead to an HP-axis shift (12,13).
Furthermore, changes in epigenetic mechanisms, i.e., gene
methylation due to varying antenatal conditions have been shown to
act as a supplementary co-factor promoting depression and anxiety
(14,15). Similarly, a range of environmental
(16), and socioeconomic factors
(17), have been suggested to act as
additional precursors for the development of these psychological
disorders.
Depression and anxiety have been reported to impart
a wide range of negative implications on maternal, fetal health
outcomes (18). In terms of maternal
health, high levels of antenatal anxiety (fear of childbirth) have
been associated with higher incidences of surgical interventions
(19), premature delivery (20), and pregnancy-related complications
(18). In addition, a positive
correlation was reported between the onset of antenatal depression
with higher levels of postnatal depression and child-rearing stress
(21). Existing studies have also
reported a proportional relationship between these antenatal
psychological disorders with fetal complications, such as inhibited
fetal growth and hyperactivity (22,23).
Moreover, higher levels of anxiety and depression during pregnancy
have also been reported to adversely impact maternal-fetal
attachment and neonatal mental development (24).
Despite previous medical advancements and the
development of numerous novel interventions (25), epidemiological studies show no sign
of decline in the onset of depression and anxiety during the
antenatal stage of pregnancy (26).
The main reason behind this could be negligence. In their review,
Atif et al (27) mentioned
that primary health care programs tend to focus more on maternal
physical health as compared to mental health. The authors added
that this prevalence was highest in developing countries where the
treatment gap for managing antenatal depression and anxiety is as
high as 85% (28). Conventionally,
psychotherapeutic interventions are considered as front-line
management approaches to alleviate depression and anxiety during
the antenatal stage of pregnancy (29). However, scarcity of expert health
care personnel and financial resources hinder the application of
these interventions in middle- and low-income settings (30). Recent evidence promotes the use of
non-specialist personnel for administering these interventions
(30).
Taking this into consideration the use of
midwife-supported psychotherapy has garnered a lot of attention
(31,32). Midwifery is an integral component of
an obstetric care unit in low-, middle- and high-income countries
(33). The approach has been
reported to influence maternal and neonatal health-related outcomes
during pregnancy (33-35).
Previous findings suggest that the intricate midwife-mother-child
bonding (36), cultural competence
(37), community embeddedness
(38), and cost-effectiveness
(33), are potential underlying
reasons making this approach successful (31,39).
Nevertheless, to date and to the best of our knowledge, no
systematic review or meta-analysis has attempted to synthesize the
evidence evaluating the effects of midwife-supported psychotherapy
on depression and anxiety during the antenatal stage of pregnancy.
Such an attempt would be useful for primary healthcare providers to
determine best practice evidence for developing effective
interventions for antenatal psychological care.
Therefore, in this present systematic review and
meta-analysis, we aim to assess the role of midwife-supported
psychotherapy on antenatal depression, anxiety, and maternal
health-status outcome.
Materials and methods
This systematic review and meta-analysis was carried
in adherence to PRISMA guidelines (40). A PRISMA checklist is provided in
Table SI.
Data search strategy
We searched four academic databases (MEDLINE,
CENTRAL, EMBASE and Scopus) from January 1960 until December 2019
using MeSH keywords: ‘antenatal’, ‘pregnancy’, ‘perinatal’,
‘before-birth’, ‘pre-birth’, ‘psychotherapy’, ‘counselling’,
‘cognitive therapy’, ‘behavioral therapy’, ‘cognitive behavioral
therapy’, ‘CBT’, ‘psychoeducation’, ‘interpersonal therapy’,
‘crisis oriented therapy’, ‘midwifery’, ‘midwife’, ‘nurse midwife’,
‘anxiety’, ‘depression’, ‘fear of birth’, ‘fear of child birth’. In
addition, we screened the bibliography of the included studies for
any additional relevant study.
Inclusion criteria for the studies were: i) Studies
evaluating the efficacy of midwife-supported psychotherapy on
depression, anxiety and health-status outcome during the antenatal
stage of pregnancy. ii) Studies evaluating pregnant women in the
antenatal stage of pregnancy. iii) Studies evaluating the
depression, anxiety and/or maternal health-status outcome through a
valid and reliable assessment method (e.g., State trait anxiety
inventory, Edinburg perinatal depression scale, fear of birth
scale, pregnancy worry and stress questionnaire, Wijma delivery
expectancy scale, and EuroQol). iv) Studies were randomized
controlled trials, quasi-randomized controlled trials, controlled
clinical trials, prospective observational trials with control
groups, or retrospective trials. v) Studies published in
peer-reviewed scientific journals, conferences. vi) Studies
published in English language.
The selection procedure was independently replicated
via two reviewers to avoid biasing. Data extracted from the
included studies were: authors, sample description (sex, age),
method of assessment, intervention, comparator, stage of assessment
and outcome measures. In the articles where quantitative data
outcomes were incomplete or not mentioned the reviewers made
attempts to contact respective corresponding authors for additional
data.
Quality assessment
Risk of bias in the included studies was assessed by
Cochrane's risk of bias assessment tool for randomized controlled
trials and non-randomized controlled trials, i.e., ROBINS-I
(41,42). The included studies were
independently appraised via two reviewers. The appraisal was
performed based on the presence of low, high or unclear risk of
bias. The thresholds for interpretation of Cochrane's risk of bias
assessment tool according to the Agency for Healthcare Research and
Quality standards was: good quality (all criteria are attained),
fair quality (one high-risk criteria or two unclear criteria) or
poor quality (two or more criteria attained with high risks).
Inadequate randomization, concealment of allocation and reporting
of selective outcomes were considered as major threats for biasing
(43). In cases of ambiguity,
discussions were held between the reviewers until a consensus was
reached. Moreover, a level of evidence analysis based on the Center
for Evidence-Based Medicine outcome was reported based on the type
of included studies (44).
Data analysis
A within group meta-analysis of the included studies
was carried out using CMA (Comprehensive Meta-analysis version 2.0)
(45). The data were distributed and
separately analyzed for depression, anxiety, and maternal
health-status outcomes. A meta-analysis was conducted based on the
random effects model (46). The
effect sizes are reported as weighted Hedge's g. The threshold for
interpreting the weighted effect sizes were: ≤0.2, small effect;
≤0.5, medium effect; and ≥0.8, large effect (47). Heterogeneity was assessed using
computing I2 statistics. The threshold for interpreting
heterogeneity was: 0-25% with negligible heterogeneity; 25-75% with
moderate heterogeneity; and ≥75% with substantial heterogeneity
(48). Sensitivity analyses were
performed in cases where substantial sources of heterogeneity
persisted (49). In the present
meta-analysis, based on the presence or absence of inadequate
randomization methods in the studies, the results were included or
excluded. For each evaluated parameter details of weighted effect
size, 95% confidence intervals (CIs), level of significance and
heterogeneity were duly reported. In addition, publication bias was
analyzed by performing the trim and fill procedure (50). This non-parametric method estimates
the number of missing studies and computes the effect that these
studies may have on the outcome of meta-analyses. Asymmetric
studies were imputed from the left side of the plotted graph to
identify the unbiased effect. Thereafter, these trimmed effects
were refilled in the plotted graph and then the combined effect
recalculated. In the present review, the alpha level was set at
5%.
Results
A preliminary search on four academic databases
resulted in a total of 921 studies, 90 more studies were included
after the bibliography of these articles were screened (Fig. 1). Thereafter, following exclusion of
the duplicates and applying the inclusion criteria, a total of 17
studies were retained. In the included studies, 12 were randomized
controlled trials (32,51-61),
whereas five were controlled clinical trials (35,62-65).
Significant reduction (P<0.05) in depression and anxiety was
reported in 13 of the included studies which received
midwife-supported psychotherapy (19,32,51,52,54-58,60-62,64).
Two studies reported an insignificant reduction (P>0.05)
(53,59), and two studies reported no effect
(63,65), of midwife-supported psychotherapy on
depression, anxiety and maternal health-status outcome during the
antenatal stage of pregnancy. Qualitative and quantitative data
were then extracted from all the studies and summarized in Table I.
 | Table ICharacteristics of the included
studies. |
Table I
Characteristics of the included
studies.
| Author (Ref) | Age: mean ± SD
years | Sample size | Assessment | Intervention
(sessions) | Control group | Stage of
assessment | Outcome |
|---|
| Daley et al
(53) | Exp: 29.4±5 Ct:
29.7±5.2 | Exp: 329 Ct:
327 | Hospital anxiety
and depression scale | Midwife-supported
self-regulation intervention (8) | Conventional
obstetric care | Baseline: 10-14
weeks Follow-up: 38 weeks | Reduction in
hospital anxiety and depression scores for Exp as compared to
Ct |
| Hildingsson et
al (62) | Exp: - Ct: - | 70 | Fear of birth
scale | Midwife-supported
psychoeducation counselling (-) | - | Baseline: 8 weeks
Follow-up: 36 weeks | Significant
reduction in fear of birth score with midwife-supported
counselling |
| Rondung et
al (59) | 29.6±4.8 Exp: - Ct:
- | Exp: 131 Ct:
127 | Fear of birth
scale | Midwife-supported
psychoeducation counselling (2-4) | Guided internet
based cognitive therapy | Baseline: 20-25
weeks Follow-up: 30-36 weeks | Reduction in fear
of birth scores for Exp as compared to Ct |
| Ghasemi et
al (54) | Exp: 25.8±4.8 Ct:
26.8±3.4 | Exp: 30 Ct: 30 | Self-efficacy
questionnaire score for fear and anxiety | Midwife-supported
cognitive behavioral therapy (4) | Conventional
obstetric care | Baseline: -
Follow-up: 37-40 weeks | Significant
reduction in self-efficacy questionnaire for fear and anxiety for
Exp as compared to Ct |
| Kildea et al
(57) | Exp: 30.8±4.6 Ct:
31.3±5.2 | Exp: 55 Ct: 71 | Edinburgh perinatal
depression scale | Midwife-supported
psychoeducation counselling (-) | Conventional
obstetric care | Baseline: 14 weeks
Follow-up: - | Significant
reduction in Edinburg postnatal depression score in Exp as compared
to Ct |
| Turkstra et
al (65) | Exp: - Ct: - | Exp: 89 Ct: 31 | Wijma delivery
expectancy scale, EQ-5D | Midwife-supported
psychoeducation counselling (-) | Conventional
obstetric care | Baseline: 16-21
weeks Follow-up: - | No effect on Wijma
delivery expectancy scale, EQ-5D scores in Exp as compared to
Ct |
| Kaboli et al
(56) | 18-35 Exp: - Ct:
- | Exp: 31 Ct: 31 | Pregnancy worries
and stress questionnaire | Midwife-supported
cognitive behavioral therapy and counselling (6) | Conventional
obstetric care | Baseline: 20-32
weeks Follow-up: - | Significant
reduction in pregnancy worries and stress questionnaire score in
Exp as compared to Ct |
| Beattie et
al (51) | Exp: - Ct: - | Exp: 11 Ct: 11 | Perceived stress
scale, Edinburg perinatal depression scale | Midwife-supported
mindful cognitive therapy (-) | Conventional
obstetric care | Baseline: 24-38
weeks Follow-up: - | Significant
reduction in perceived stress scale score and Edinburg postnatal
depression scale in Exp as compared to Ct |
| Brugha et al
(32) | Exp: - Ct: - | Exp: 126 Ct:
103 | State trait anxiety
inventory, Edinburg perinatal depression scale | Midwife-supported
psychoeducation counselling (-) | Conventional
obstetric care | Baseline: 12 weeks
Follow-up: - | Significant
reduction in state trait anxiety inventory score and Edinburg
perinatal depression score in Exp as compare to Ct |
| Jesse et al
(55) | Exp: 24.9±5.6 Ct:
25.1±5.3 | Exp: 72 Ct: 74 | Edinburg perinatal
depression scale, Beck depression inventory | Midwife-supported
cognitive-behavioral therapy (6) | Conventional
obstetric care | Baseline: -
Follow-up: - | Significant
reduction in Edinburg perinatal depression score, Beck depression
inventory in Exp as compare to Ct |
| Rouhe et al
(60) | Exp: - Ct: - | Exp: 131 Ct:
240 | Edinburg perinatal
depression scale, Wijma delivery expectancy scale | Midwife-supported
psychoeducation counselling (-) | Conventional
obstetric care | Baseline: -
Follow-up: - | Significant
reduction in Wijma delivery expectancy score, Edinburg perinatal
depression scale in Exp as compared to Ct |
| Larsson et
al (63) | Exp: - Ct: - | Exp: 70 Ct:
866 | Self-reported
childbirth fear questionnaire | Midwife-supported
psychoeducation counselling (-) | Conventional
obstetric care | Baseline: -
Follow-up: - | No effect on
self-reported childbirth fear questionnaire in Exp |
| Toohill et
al (61) | Exp: 29±5.9 Ct:
29.2±4.9 | Exp: 101 Ct:
97 | Edinburg perinatal
depression scale, Wijma delivery expectancy scale | Midwife-supported
psychoeducation counselling (-) | Conventional
obstetric care | Baseline: 24 weeks
Follow-up: 36 weeks | Significant
reduction in Wijma delivery expectancy score in Exp as compared to
Ct Reduction in Edinburg perinatal depression scale in Exp as
compared to Ct |
| Burns et al
(52) | Exp: 30.1±6.2 Ct:
28±5 | Exp: 18 Ct: 18 | Edinburg perinatal
depression scale, EQ-5D | Midwife-supported
psychoeducation counselling (-) | Cognitive
therapy | Baseline: 15 weeks
Follow-up: 33 weeks | Significant
enhancement in EQ-5D scores for Exp as compared to Ct Significant
reduction in Edinburg perinatal depression score in Ct as compared
to Exp |
| Ngai et al
(64) | Exp: 32.1±3.7 Ct:
30.5±3.7 | Exp: 92 Ct: 92 | Edinburg perinatal
depression scale | Midwife-supported
psychoeducation counselling (-) | Conventional
obstetric care | Baseline: -
Follow-up: - | Significant
reduction in Edinburg perinatal depression score in Exp as compared
to Ct |
| Waldenström et
al (19) | Exp: - Ct: - | Exp: 240 Ct:
2,422 | Pregnancy worries
and stress questionnaire, Edinburg perinatal depression scale | Midwife-supported
psychoeducation counselling (-) | Conventional
obstetric care | Baseline: -
Follow-up: - | Significant
reduction in pregnancy worries and stress, Edinburg perinatal
depression score in Exp as compared to Ct |
| Middlemiss et
al (58) | Exp: 28.8±5.9 Ct:
26±3.5 | Exp: 40 Ct: 17 | Zung depression
scale, State trait anxiety inventory score | Midwife-supported
psychoeducation counselling (-) | Conventional
obstetric care | Baseline: 35 weeks
Follow-up: - | Significant
reduction in State trait anxiety score in Exp as compared to Ct
Reducing in Zung depression score in Exp as compared to Ct |
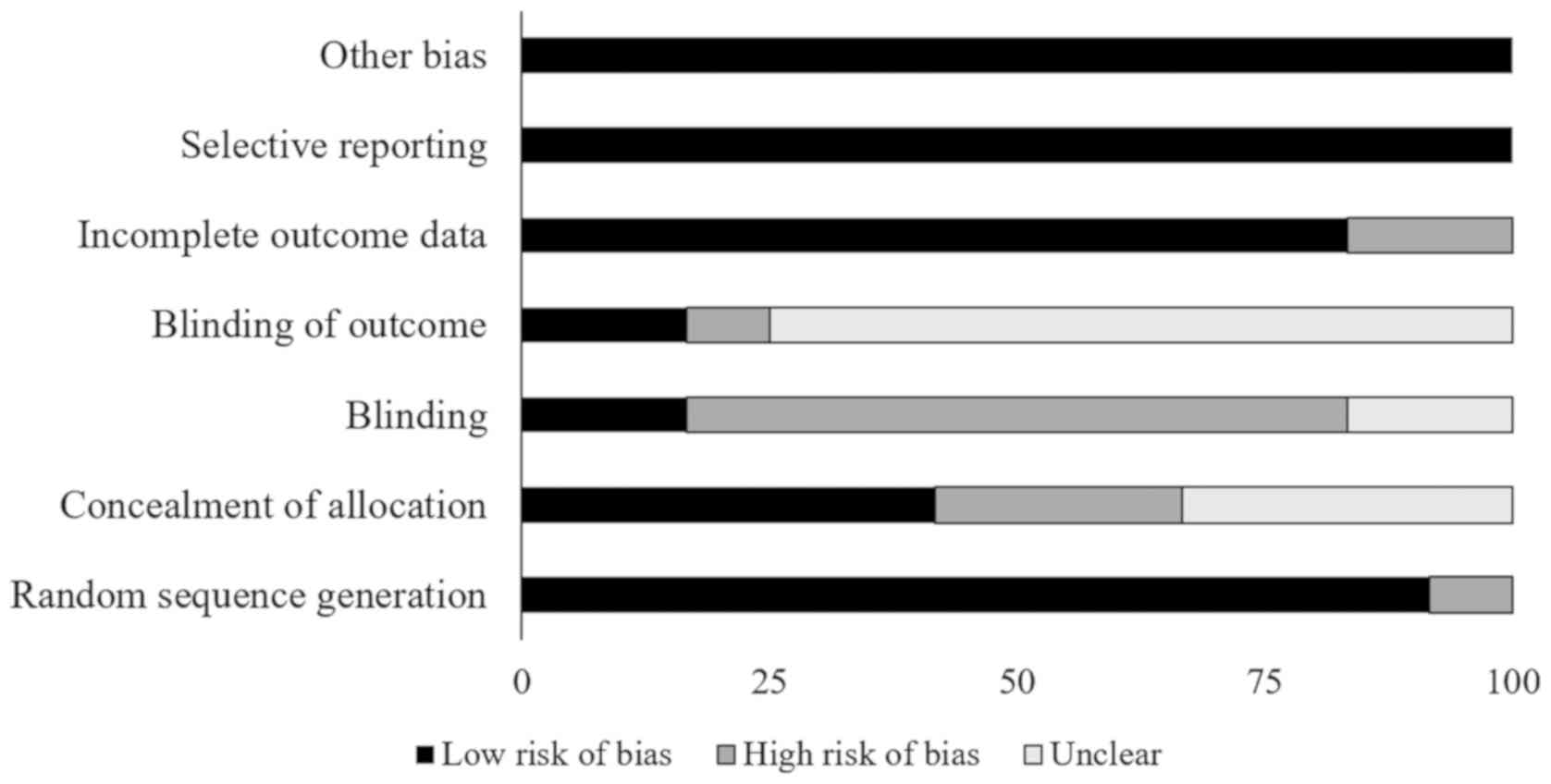
Risk of bias Randomized controlled
trials
The risk of bias for the randomized controlled
trials according to Cochrane's risk of bias assessment tool for
randomized controlled trials is presented in Table II. The overall risk in the included
studies was poor. The highest risk of bias was observed to be due
to lack of blinding of the participants, researchers, outcomes, and
due to lack of concealed allocation (Fig. 2). A level of evidence of 1b was
observed for all the included studies based on their experimental
design.
 | Table IIQuality of the analyzed studies
according to the Cochrane risk of bias assessment tool for
randomized controlled trials. |
Table II
Quality of the analyzed studies
according to the Cochrane risk of bias assessment tool for
randomized controlled trials.
| Study | Random sequence
generation | Concealment of
allocation | Blinding | Blinding of
outcome | Incomplete outcome
data | Selective
reporting | Other bias | Level of
evidence |
|---|
| Daley et al
(53) | + | + | - | + | + | + | + | 1b |
| Rondung et
al (59) | + | - | - | ? | + | + | + | 1b |
| Ghasemi et
al (54) | + | - | - | ? | + | + | + | 1b |
| Kildea et al
(57) | - | + | - | + | + | + | + | 1b |
| Kaboli et al
(56) | + | - | - | ? | + | + | + | 1b |
| Beattie et
al (51) | + | + | + | ? | + | + | + | 1b |
| Brugha et al
(32) | + | + | - | ? | + | + | + | 1b |
| Jesse et al
(55) | + | ? | - | ? | + | + | + | 1b |
| Rouhe et al
(60) | + | ? | ? | ? | - | + | + | 1b |
| Toohill et
al (61) | + | ? | - | - | - | + | + | 1b |
| Burns et al
(52) | + | + | ? | ? | + | + | + | 1b |
| Middlemiss et
al (58) | + | ? | + | ? | + | + | + | 1b |
Controlled clinical trials
The prevalence of risk of bias for the controlled
clinical trials according to Cochrane's risk of bias assessment
tool for non-randomized controlled trials ROBINS-I is presented in
Table III. The overall risk in the
included studies was again poor. The highest risk of bias was
observed to be due to the lack of clarity in the confounding
factors, and outcome measurement (Fig.
3). Furthermore, the studies refrained from explaining the
measures they undertook to manage missing data and/or analyses for
intention to treat analysis. A level of evidence of 2b was observed
for all the included studies based on their experimental
design.
 | Table IIIQuality of the analyzed studies
according to the Cochrane risk of bias assessment tool for
non-randomized controlled trials ROBINS-I. |
Table III
Quality of the analyzed studies
according to the Cochrane risk of bias assessment tool for
non-randomized controlled trials ROBINS-I.
| Study | Confounding
bias | Selection bias | Deviation from
intended intervention | Missing data | Measurement in
outcome | Selection of
reported result | Classification of
intervention | Level of
evidence |
|---|
| Hildingsson, et
al (62) | ? | + | + | - | + | + | + | 2b |
| Turkstra et
al (65) | + | + | - | - | - | ? | + | 2b |
| Larsson et
al (63) | ? | - | ? | - | - | + | + | 2b |
| Ngai et al
(64) | + | + | ? | - | + | + | + | 2b |
| Waldenström et
al (19) | + | ? | ? | - | - | ? | + | 2b |
Publication bias
The trim and fill procedure identified two missing
studies on the left side of the mean effect (Fig. 4). In addition, according to the
random effects model, the point estimates and 95% confidence
intervals for the evaluated parameters were -0.8 (-1.1 to -0.5).
The trim and fill procedure report the imputed point estimate as
-0.9 (-1.1 to 0.5).
Participant information
A total of 6,193 pregnant women were evaluated in
the studies included in this review. From these, a total of 1,636
women were a part of the experimental group where midwife-supported
psychotherapy was administered, whereas 4,557 women were a part of
the control group receiving conventional obstetric care. Eight of
the included studies did not mention the age of the included sample
(19,32,51,55,56,62,63,65).
However, from the studies that did report the age of their
participants, the mean age of the included participants was
28.9±2.2 years for the experimental and 28.2±2.3 years for the
control group.
Assessment
Three studies assessed the influence of
midwife-supported psychotherapy on depression alone (55,57,64),
whereas six studies assessed its influence on anxiety (19,56,59,63,65,66).
Eight studies jointly evaluated the effects of midwife-supported
psychotherapy on both depression and anxiety (32,51,52,54,58,60,61,66). The
average baseline, follow-up assessments for the included studies
was performed at 19.8±2.3 and 35.7±2.3 weeks, respectively.
However, from the included studies six did not report the initial
baseline stage of assessment (19,54,55,60,63,64),
whereas eleven did not report the stage at which the follow-up
assessment was performed (19,32,51,55-58,60,63-65).
Intervention
In the included studies, midwife-supported
psychoeducation counselling was administered by 12 studies
(19,32,52,57-61,63-66).
Four studies used midwife-supported cognitive behavioral therapy
(51,54-56),
and one study used midwife-supported self-regulation therapy
(53), for managing depression and
anxiety during the antenatal stage of pregnancy.
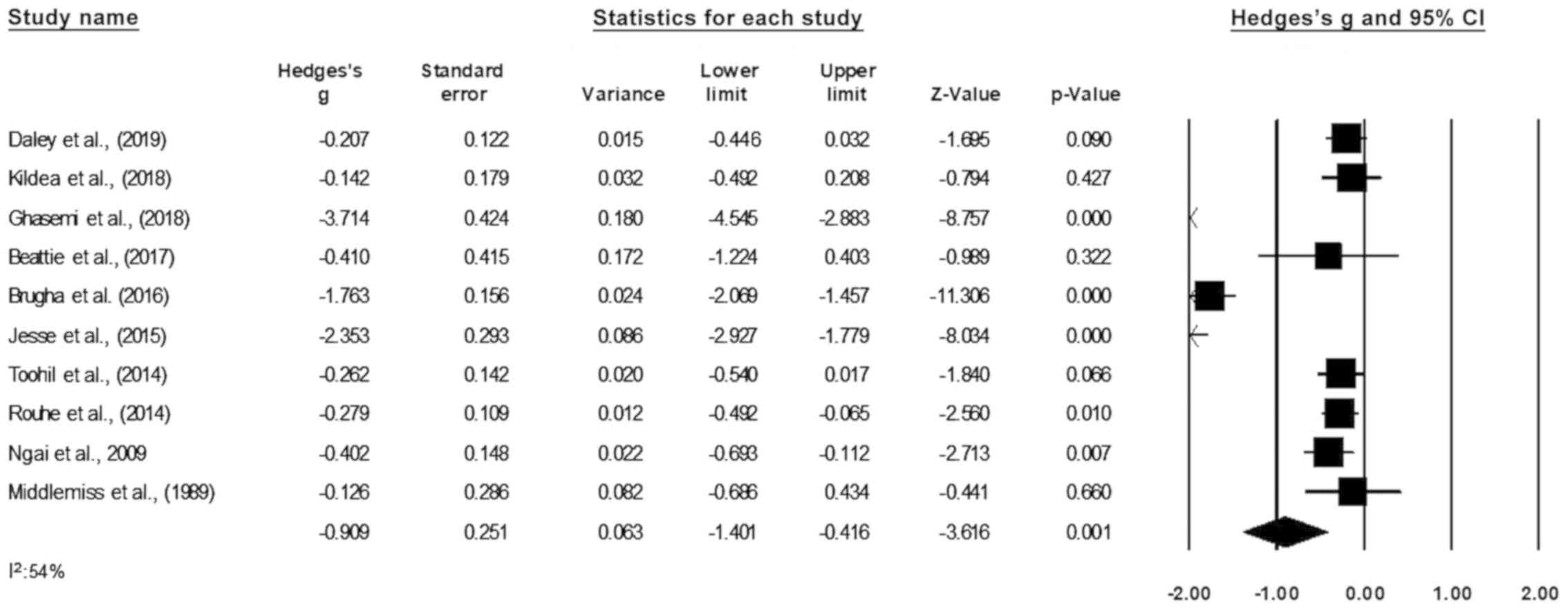
Meta-analysis reports Depression
Depression was assessed in 10 studies (32,51,53-55,57,58,60,61,64).
In those studies, data from 761 participants were assessed in the
experimental group receiving midwife-supported psychotherapy as
compared to 833 in the control group. The assessment of depression
was performed in six studies using the Edinburg perinatal
depression scale (32,51,54,60,61,64), and
one study each using Zung self-rating depression scale (58), hospital anxiety-depression scale
(53), Beck depression inventory
(55), and self-efficacy
questionnaire (54). An across
group, random-effect analysis (Fig.
5) revealed a large negative and significant effect of
midwife-supported psychotherapy on depression as compared to
conventional obstetric care (g: -0.909, 95% CI: -1.401 to -0.416,
P=0.001) with moderate heterogeneity (I2: 54%).
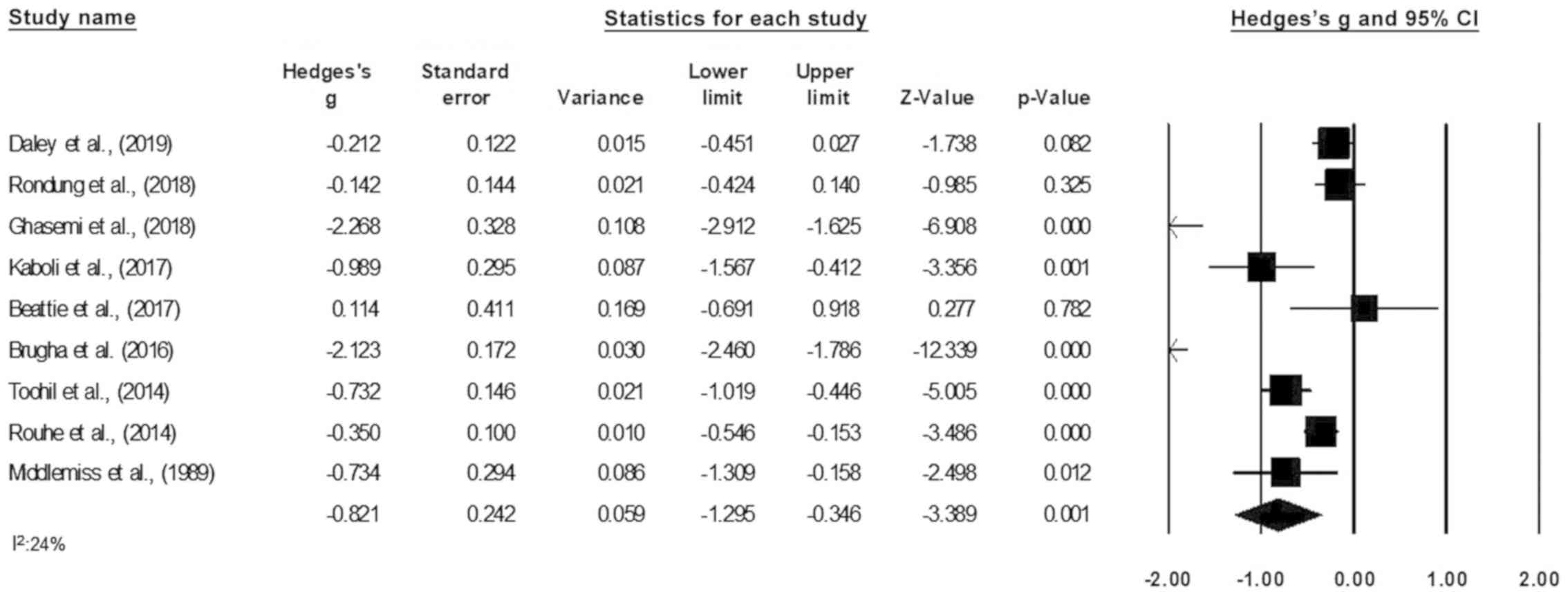
Anxiety
Anxiety was assessed in nine studies (32,51,53,54,56,58-61).
In those studies, data from 778 participants were assessed in the
experimental group receiving midwife-supported psychotherapy as
compared to 694 in the control group. The assessment of anxiety was
performed by two studies each using the Wijma delivery expectancy
scale (60,61), state trait anxiety inventory scale
(32,58), one study each using hospital
anxiety-depression scale (53),
perceived stress scale (51),
self-efficacy questionnaire (54),
pregnancy worry and stress scale (56), and fear of birth scale (59). An across group, random-effect
analysis (Fig. 6) revealed a medium
negative and significant effects of midwife-supported psychotherapy
on anxiety as compared to conventional obstetric care (g: -0.821,
95% CI: -1.296 to -0.346, P=0.001) with negligible heterogeneity
(I2: 24%).
Maternal health-status outcome
Maternal health-status outcome was assessed in two
studies (52,65). Both the studies used EQ-5D scoring to
assess health-status outcome. Data from 102 participants were
assessed in the experimental group receiving midwife-supported
psychotherapy as compared to 106 in the control group. An across
group, random-effect analysis (Fig.
7) revealed a small positive and non-significant effects of
midwife-supported psychotherapy on health-status outcome as
compared to conventional obstetric care (g: 0.172, 95% CI: -0.098
to 0.443, P=0.213) with no heterogeneity (I2: 0%).
Discussion
To the best of our knowledge, this review has for
the first time evaluated the effects of midwife-supported
psychotherapy on depression, anxiety and maternal health-status
outcome during the antenatal stage of pregnancy. We report a
beneficial effect of midwife-supported psychotherapy as compared to
conventional obstetric care for alleviating depression and anxiety.
Moreover, we report beneficial effects of midwife-supported
psychotherapy for enhancing maternal health-status during the
antenatal stage of pregnancy.
In the past decade, psychotherapeutic interventions
have been extensively used as the first line of treatment to manage
depression and anxiety during pregnancy (67,68).
Predominantly, the ability of this approach has been favored
because of its capability to avoid pharmacological complications
(69). Wikner et al (70), for instance, reported the use of
antidepressants such as Benzodiazepines during the antenatal stage
of pregnancy to be highly associated with increased risks of poorer
maternal health, fetal defects and congenital malformations
(71). Furthermore, the use of
psychotherapeutic interventions has been preferred because of their
ability to enhance maternal motivation (72), allowing self-regulation of thoughts
(73), and restructuring of negative
emotions (74). In a systematic
review, Sockol (75) reported that
of all the psychotherapeutic interventions the efficacy of
cognitive psychotherapy was far more superior in reducing and
preventing the onset of depression during the later stages of
pregnancy. The author mentioned that the complex cognitive
procedures during cognitive psychotherapy could promote the
development of a flexible and adaptive problem-solving approach for
the patient which then, in turn, could be used to effectively
reduce depression and anxiety (75,76).
Nevertheless, the use of these effective interventions has been
marred by the shortfalls in terms of specialist personnel and
finances especially in low- and middle-income countries (77,78).
To counteract these detrimental effects, the use of
non-specialist staff such as midwives for delivering
psychotherapeutic interventions during the antenatal stage of
pregnancy has been recommended in literature (79-81).
Brugha et al (32), for
instance, reported a substantial reduction in anxiety and
depression with trained midwife-supported psychotherapy. The
authors of that study reported that higher compliance,
accessibility and confided emotional support offered by the
midwives to be the main reasons behind these effects. Further work
by Beattie et al (51)
reported reduced depression and anxiety with midwife-supported
behavioral therapy. Authors suggested that midwife-supported
behavioral therapy could promote an enhanced state of acceptability
during childbirth, which, in turn, could enhance the experience of
labor (51,82). In addition, a compassionate
midwife-mother bonding could be an important reason which would
have allowed enhancements in self-acceptability, awareness and
social independence. In the current meta-analyses, we too observed
large effect reduction in the levels of depression (Hedge's g:
-0.909) and anxiety (g: -0.821) with midwife-supported
psychotherapy.
In addition to reducing psychosomatic
manifestations, midwife-supported therapy has also been reported to
have beneficial effects on overall maternal health (33,80). We
presume that the ability of midwife-supported care to effectively
impart antenatal care education could be a main reason behind its
ability to enhance maternal health. Turkstra et al (65) reported that midwife-supported
psychoeducation was, not only efficient in minimally enhancing the
maternal health-outcomes (EQ-5D scores), but was also competent in
reducing costs towards obstetric care. Accordingly, a recent
Cochrane review also reported benefits of midwife-supported care on
maternal health. The authors mentioned that mothers receiving
midwife-supported care during the antenatal stage of pregnancy were
less likely to experience severe labor-related pains and discomfort
(83). Our findings concerning
maternal-health outcomes are in line with the existing literature.
In this present meta-analysis, we encountered small beneficial
effect of midwife-supported psychotherapy for enhancing maternal
health-status outcome (g: -0.998).
Finally, in the present literature review a few
limitations persist. Firstly, this systematic review was not
registered in a prospective registry such as PROSPERO. The reason
for this lack of registration was that the communication delays
from PROSPERO affected the preset project deadlines. Therefore, we
decided to commence with the publication of this review even
without the registration. We understand that this may raise
questions concerning validity of this review. Secondly, a scarcity
of statistical data in the included studies could have biased our
interpretations concerning the influence of midwife-supported
psychotherapy on maternal health-status outcome. The evaluation of
health-status outcome was performed in only two studies including a
total of 102, 106 women in the experimental and control groups,
respectively. In this instance, the outcome due to a small sample
size could possibly influence the results due to a type II error
(84). We recommend future studies
to address this paucity of data by evaluating health-status
outcomes and sharing descriptive statistics in open access data
repositories. Thirdly, as we incorporated broad inclusion criteria
in our review study, we were able to include a wide range of
studies assessing different midwife-supported psychotherapeutic
interventions with different assessment tools. Due to this,
moderate heterogeneity, i.e., 54% was observed in one of the
meta-analysis reports analyzing the effects of midwife-supported
psychotherapy on depression. Therefore, we would strongly recommend
our readers to carefully interpret these results.
In conclusion, this systematic review and
meta-analysis provides a 1b level of evidence for the randomized
controlled trials and a 2b level of evidence for non-randomized
controlled trials to support the use of midwife-supported
psychotherapy to reduce depression, anxiety and enhance maternal
health outcomes during the antenatal stage of pregnancy. The
findings from the current meta-analyses can have widespread
implications for developing best practice antenatal care approaches
worldwide. However, further investigations are required to verify
our findings.
Supplementary Material
PRISMA checklist.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
QH and XX designed the paper. MG, FR, and DD were
involved in literature search and data interpretation. QH, MG and
FR were responsible for the data analysis. QH prepared the
manuscript. XX edited the manuscript. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Lee AM, Lam SK, Sze Mun Lau SM, Chong CS,
Chui HW and Fong DY: Prevalence, course, and risk factors for
antenatal anxiety and depression. Obstet Gynecol. 110:1102–1112.
2007.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Pawlby S, Hay DF, Sharp D, Waters CS and
O'Keane V: Antenatal depression predicts depression in adolescent
offspring: Prospective longitudinal community-based study. J Affect
Disord. 113:236–243. 2009.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Fisher J, Cabral de Mello M, Patel V,
Rahman A, Tran T, Holton S and Holmes W: Prevalence and
determinants of common perinatal mental disorders in women in low-
and lower-middle-income countries: A systematic review. Bull World
Health Organ. 90:139G–149G. 2012.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Husain N, Bevc I, Husain M, Chaudhry IB,
Atif N and Rahman A: Prevalence and social correlates of postnatal
depression in a low income country. Arch Women Ment Health.
9:197–202. 2006.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Engle PL: Maternal mental health: Program
and policy implications. Am J Clin Nutr. 89:963S–966S.
2009.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Saxena S, Funk M and Chisholm D: World
Health Assembly adopts Comprehensive Mental Health Action Plan
2013-2020. Lancet. 381:1970–1971. 2013.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Karmaliani R, Asad N, Bann CM, Moss N,
Mcclure EM, Pasha O, Wright LL and Goldenberg RL: Prevalence of
anxiety, depression and associated factors among pregnant women of
Hyderabad, Pakistan. Int J Soc Psychiatry. 55:414–424.
2009.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Rahman A, Bunn J, Lovel H and Creed F:
Association between antenatal depression and low birthweight in a
developing country. Acta Psychiatr Scand. 115:481–486.
2007.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Leung BMY and Kaplan BJ: Perinatal
depression: Prevalence, risks, and the nutrition link--a review of
the literature. J Am Diet Assoc. 109:1566–1575. 2009.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Waters CS, Hay DF, Simmonds JR and van
Goozen SHM: Antenatal depression and children's developmental
outcomes: Potential mechanisms and treatment options. Eur Child
Adolesc Psychiatry. 23:957–971. 2014.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Meltzer-Brody S: New insights into
perinatal depression: Pathogenesis and treatment during pregnancy
and postpartum. Dialogues Clin Neurosci. 13:89–100. 2011.PubMed/NCBI
|
|
12
|
Gelman PL, Flores-Ramos M, López-Martínez
M, Fuentes CC and Grajeda JPR: Hypothalamic-pituitary-adrenal axis
function during perinatal depression. Neurosci Bull. 31:338–350.
2015.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Kammerer M, Taylor A and Glover V: The HPA
axis and perinatal depression: A hypothesis. Arch Women Ment
Health. 9:187–196. 2006.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Perera F and Herbstman J: Prenatal
environmental exposures, epigenetics, and disease. Reprod Toxicol.
31:363–373. 2011.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Tarantino LM, Sullivan PF and
Meltzer-Brody S: Using animal models to disentangle the role of
genetic, epigenetic, and environmental influences on behavioral
outcomes associated with maternal anxiety and depression. Front
Psychiatry. 2(44)2011.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Nestler EJ, Barrot M, DiLeone RJ, Eisch
AJ, Gold SJ and Monteggia LM: Neurobiology of depression. Neuron.
34:13–25. 2002.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Bleker LS, de Rooij SR and Roseboom TJ:
Malnutrition and depression in pregnancy and associations with
child behaviour and cognitive function: A review of recent evidence
on unique and joint effects. Can J Physiol Pharmacol. 97:158–173.
2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Chung TK, Lau TK, Yip AS, Chiu HF and Lee
DT: Antepartum depressive symptomatology is associated with adverse
obstetric and neonatal outcomes. Psychosom Med. 63:830–834.
2001.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Waldenström U, Hildingsson I and Ryding
EL: Antenatal fear of childbirth and its association with
subsequent caesarean section and experience of childbirth. BJOG.
113:638–646. 2006.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Glover V and O'Connor TG: Effects of
antenatal stress and anxiety: Implications for development and
psychiatry. Br J Psychiatry. 180:389–391. 2002.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Misri S, Kendrick K, Oberlander TF, Norris
S, Tomfohr L, Zhang H and Grunau RE: Antenatal depression and
anxiety affect postpartum parenting stress: A longitudinal,
prospective study. Can J Psychiatry. 55:222–228. 2010.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Field T, Diego M and Hernandez-Reif M:
Prenatal depression effects on the fetus and newborn: A review.
Infant Behav Dev. 29:445–455. 2006.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Nguyen TM and Castro LC: Hypertensive
Disorders and Depression in Pregnancy: Pregnancy Complications and
Fetal Versus Neonatal Outcomes. J Womens Health (Larchmt).
28:1451–1453. 2019.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Brouwers EPM, van Baar AL and Pop VJM:
Maternal anxiety during pregnancy and subsequent infant
development. Infant Behav Dev. 24:95–106. 2001.
|
|
25
|
Dennis CL, Ross LE and Grigoriadis S:
Psychosocial and psychological interventions for treating antenatal
depression. Cochrane Database Syst Rev.
2007(CD006309)2007.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Milgrom J, Schembri C, Ericksen J, Ross J
and Gemmill AW: Towards parenthood: An antenatal intervention to
reduce depression, anxiety and parenting difficulties. J Affect
Disord. 130:385–394. 2011.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Atif N, Lovell K and Rahman A: Maternal
mental health: The missing ‘m’ in the global maternal and child
health agenda. Semin Perinatol. 39:345–352. 2015.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Demyttenaere K, Bruffaerts R, Posada-Villa
J, Gasquet I, Kovess V, Lepine JP, Angermeyer MC, Bernert S, de
Girolamo G, Morosini P, et al: WHO World Mental Health Survey
Consortium: Prevalence, severity, and unmet need for treatment of
mental disorders in the World Health Organization World Mental
Health Surveys. JAMA. 291:2581–2590. 2004.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Middleton H, Shaw I, Hull S and Feder G:
NICE guidelines for the management of depression. BMJ. 330:267–268.
2005.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Rahman A, Malik A, Sikander S, Roberts C
and Creed F: Cognitive behaviour therapy-based intervention by
community health workers for mothers with depression and their
infants in rural Pakistan: A cluster-randomised controlled trial.
Lancet. 372:902–909. 2008.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Anderson T: Feeling Safe Enough to Let Go:
The Relationship Between a Woman and her Midwife During the Second
Stage of Labour. In: The Midwife-Mother Relationship. Kirkham K
(ed). 2nd edition. Macmillan, Basingstoke, pp116-143, 2010.
|
|
32
|
Brugha TS, Smith J, Austin J, Bankart J,
Patterson M, Lovett C, Morgan Z, Morrell CJ and Slade P: Can
community midwives prevent antenatal depression? An external pilot
study to test the feasibility of a cluster randomized controlled
universal prevention trial. Psychol Med. 46:345–356.
2016.PubMed/NCBI View Article : Google Scholar
|
|
33
|
ten Hoope-Bender P, de Bernis L, Campbell
J, Downe S, Fauveau V, Fogstad H, Homer CS, Kennedy HP, Matthews Z,
McFadden A, et al: Improvement of maternal and newborn health
through midwifery. Lancet. 384:1226–1235. 2014.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Sandall J, Devane D, Soltani H, Hatem M
and Gates S: Improving quality and safety in maternity care: The
contribution of midwife-led care. J Midwifery Womens Health.
55:255–261. 2010.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Waldenström U and Turnbull D: A systematic
review comparing continuity of midwifery care with standard
maternity services. Br J Obstet Gynaecol. 105:1160–1170.
1998.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Attarha M, Keshavarz Z, Bakhtiari M and
Jamilian M: The Outcome of Midwife-Mother Relationship in Delivery
Room: A Qualitative Content Analysis. Health. 8:720–726. 2016.
|
|
37
|
Rorie JA, Paine LL and Barger MK: Primary
care for women. Cultural competence in primary care services. J
Nurse Midwifery. 41:92–100. 1996.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Hunter B: The importance of reciprocity in
relationships between community-based midwives and mothers.
Midwifery. 22:308–322. 2006.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Deery R and Hunter B: Emotion Work and
Relationships. In: The Midwife-Mother Relationship. Kirkham M (ed).
Palgrave Mcmillan, London, 2010.
|
|
40
|
Moher D, Liberati A, Tetzlaff J and Altman
DG: PRISMA Group. Preferred reporting items for systematic reviews
and meta-analyses: The PRISMA statement. PLoS Med.
6(e1000097)2009.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Jørgensen L, Paludan-Müller AS, Laursen
DRT, Savović J, Boutron I, Sterne JA, Higgins JP and Hróbjartsson
A: Evaluation of the Cochrane tool for assessing risk of bias in
randomized clinical trials: Overview of published comments and
analysis of user practice in Cochrane and non-Cochrane reviews.
Syst Rev. 5(80)2016.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Sterne JA, Hernán MA, Reeves BC, Savović
J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT,
Boutron I, et al: ROBINS-I: A tool for assessing risk of bias in
non-randomised studies of interventions. BMJ.
355(i4919)2016.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Viswanathan M, Ansari MT, Berkman ND, et
al: Assessing the Risk of Bias of Individual Studies in Systematic
Reviews of Health Care Interventions. In: Methods Guide for
Effectiveness and Comparative Effectiveness Reviews. Agency for
Healthcare Research and Quality (US), Rockville, MD, 2008.
|
|
44
|
Burns PB, Rohrich RJ and Chung KC: The
levels of evidence and their role in evidence-based medicine. Plast
Reconstr Surg. 128:305–310. 2011.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Bax L, Yu LM, Ikeda N and Moons KG: A
systematic comparison of software dedicated to meta-analysis of
causal studies. BMC Med Res Methodol. 7(40)2007.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Higgins JPT, Thompson SG and Spiegelhalter
DJ: A re-evaluation of random-effects meta-analysis. J R Stat Soc
Ser A Stat Soc. 172:137–159. 2009.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Rosenthal R: Parametric measures of effect
size. In: The handbook of research synthesis. Russell Sage
Foundation, New York, NY, pp231-244, 1994.
|
|
48
|
Higgins JPT and Thompson SG: Quantifying
heterogeneity in a meta-analysis. Stat Med. 21:1539–1558.
2002.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Petitti DB: Approaches to heterogeneity in
meta-analysis. Stat Med. 20:3625–3633. 2001.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Duval S and Tweedie R: Trim and fill: A
simple funnel-plot-based method of testing and adjusting for
publication bias in meta-analysis. Biometrics. 56:455–463.
2000.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Beattie J, Hall H, Biro MA, East C and Lau
R: Effects of mindfulness on maternal stress, depressive symptoms
and awareness of present moment experience: A pilot randomised
trial. Midwifery. 50:174–183. 2017.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Burns A, O'Mahen H, Baxter H, Bennert K,
Wiles N, Ramchandani P, Turner K, Sharp D, Thorn J, Noble S, et al:
A pilot randomised controlled trial of cognitive behavioural
therapy for antenatal depression. BMC Psychiatry.
13(33)2013.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Daley A, Jolly K, Jebb SA, Roalfe A,
Mackilllop L, Lewis A, Clifford S, Usman M, Ohadike C, Kenyon S, et
al: Effectiveness of a behavioural intervention involving regular
weighing and feedback by community midwives within routine
antenatal care to prevent excessive gestational weight gain: POPS2
randomised controlled trial. BMJ Open. 9(e030174)2019.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Ghasemi F, Bolbol-Haghighi N, Mottaghi Z,
Hosseini SR and Khosravi A: The Effect of Group Counseling with
Cognitive-Behavioral Approach on Self-Efficacy of Pregnant Women's
Choice of Vaginal Delivery. Iran J Psychiatry Behav Sci In Press
(In Press).
|
|
55
|
Jesse DE, Gaynes BN, Feldhousen EB, Newton
ER, Bunch S and Hollon SD: Performance of a Culturally Tailored
Cognitive-Behavioral Intervention Integrated in a Public Health
Setting to Reduce Risk of Antepartum Depression: A Randomized
Controlled Trial. J Midwifery Womens Health. 60:578–592.
2015.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Kaboli KS, Mahmoodi Z, Tourzani ZM,
Tehranizadeh M, Kabir K and Dolatian M: The Effect of Group
Counseling Based on Cognitive-Behavioral Approach on
Pregnancy-Specific Stress and Anxiety. Shiraz E Med J (In
Press).
|
|
57
|
Kildea S, Simcock G, Liu A, Elgbeili G,
Laplante DP, Kahler A, Austin MP, Tracy S, Kruske S, Tracy M, et
al: Continuity of midwifery carer moderates the effects of prenatal
maternal stress on postnatal maternal wellbeing: The Queensland
flood study. Arch Womens Ment Health. 21:203–214. 2018.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Middlemiss C, Dawson AJ, Gough N, Jones ME
and Coles EC: A randomised study of a domiciliary antenatal care
scheme: Maternal psychological effects. Midwifery. 5:69–74.
1989.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Rondung E, Ternström E, Hildingsson I,
Haines HM, Sundin Ö, Ekdahl J, Karlström A, Larsson B, Segeblad B,
Baylis R, et al: Comparing Internet-Based Cognitive Behavioral
Therapy With Standard Care for Women With Fear of Birth: Randomized
Controlled Trial. JMIR Ment Health. 5(e10420)2018.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Rouhe H, Salmela-Aro K, Toivanen R, Tokola
M, Halmesmäki E, Ryding EL and Saisto T: Group psychoeducation with
relaxation for severe fear of childbirth improves maternal
adjustment and childbirth experience - a randomised controlled
trial. J Psychosom Obstet Gynaecol. 36:1–9. 2015.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Toohill J, Fenwick J, Gamble J, Creedy DK,
Buist A, Turkstra E and Ryding EL: A randomized controlled trial of
a psycho-education intervention by midwives in reducing childbirth
fear in pregnant women. Birth. 41:384–394. 2014.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Hildingsson I, Karlström A, Rubertsson C
and Haines H: Women with fear of childbirth might benefit from
having a known midwife during labour. Women Birth. 32:58–63.
2019.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Larsson B, Karlström A, Rubertsson C and
Hildingsson I: The effects of counseling on fear of childbirth.
Acta Obstet Gynecol Scand. 94:629–636. 2015.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Ngai FW, Chan SWC and Ip WY: The effects
of a childbirth psychoeducation program on learned resourcefulness,
maternal role competence and perinatal depression: A
quasi-experiment. Int J Nurs Stud. 46:1298–1306. 2009.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Turkstra E, Mihala G, Scuffham PA, Creedy
DK, Gamble J, Toohill J and Fenwick J: An economic evaluation
alongside a randomised controlled trial on psycho-education
counselling intervention offered by midwives to address women's
fear of childbirth in Australia. Sex Reprod Healthc. 11:1–6.
2017.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Hildingsson I, Rubertsson C, Karlström A
and Haines H: A known midwife can make a difference for women with
fear of childbirth- birth outcome and women's experiences of
intrapartum care. Sex Reprod Healthc. 21:33–38. 2019.PubMed/NCBI View Article : Google Scholar
|
|
67
|
Glover V: Maternal depression, anxiety and
stress during pregnancy and child outcome; what needs to be done.
Best Pract Res Clin Obstet Gynaecol. 28:25–35. 2014.PubMed/NCBI View Article : Google Scholar
|
|
68
|
Stoll K, Swift EM, Fairbrother N, Nethery
E and Janssen P: A systematic review of nonpharmacological prenatal
interventions for pregnancy-specific anxiety and fear of
childbirth. Birth. 45:7–18. 2018.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Dubovicky M, Belovicova K, Csatlosova K
and Bogi E: Risks of using SSRI / SNRI antidepressants during
pregnancy and lactation. Interdiscip Toxicol. 10:30–34.
2017.PubMed/NCBI View Article : Google Scholar
|
|
70
|
Wikner BN, Stiller CO, Bergman U, Asker C
and Källén B: Use of benzodiazepines and benzodiazepine receptor
agonists during pregnancy: Neonatal outcome and congenital
malformations. Pharmacoepidemiol Drug Saf. 16:1203–1210.
2007.PubMed/NCBI View Article : Google Scholar
|
|
71
|
Arch JJ, Dimidjian S and Chessick C: Are
exposure-based cognitive behavioral therapies safe during
pregnancy? Arch Women Ment Health. 15:445–457. 2012.PubMed/NCBI View Article : Google Scholar
|
|
72
|
Cho HJ, Kwon JH and Lee JJ: Antenatal
cognitive-behavioral therapy for prevention of postpartum
depression: A pilot study. Yonsei Med J. 49:553–562.
2008.PubMed/NCBI View Article : Google Scholar
|
|
73
|
Beck R and Fernandez E:
Cognitive-Behavioral Self-Regulation of the Frequency, Duration,
and Intensity of Anger. J Psychopathol Behav Assess. 20:217–229.
1998.
|
|
74
|
Mueser KT, Gottlieb JD, Xie H, Lu W, Yanos
PT, Rosenberg SD, Silverstein SM, Duva SM, Minsky S, Wolfe RS, et
al: Evaluation of cognitive restructuring for post-traumatic stress
disorder in people with severe mental illness. Br J Psychiatry.
206:501–508. 2015.PubMed/NCBI View Article : Google Scholar
|
|
75
|
Sockol LE: A systematic review of the
efficacy of cognitive behavioral therapy for treating and
preventing perinatal depression. J Affect Disord. 177:7–21.
2015.PubMed/NCBI View Article : Google Scholar
|
|
76
|
Silverstein M, Feinberg E, Cabral H,
Sauder S, Egbert L, Schainker E, Kamholz K, Hegel M and Beardslee
W: Problem-solving education to prevent depression among low-income
mothers of preterm infants: A randomized controlled pilot trial.
Arch Women Ment Health. 14:317–324. 2011.PubMed/NCBI View Article : Google Scholar
|
|
77
|
Beck A, Nadkarni A, Calam R, Naeem F and
Husain N: Increasing access to Cognitive Behaviour Therapy in Low
and Middle Income Countries: A strategic framework. Asian J
Psychiatr. 22:190–195. 2016.PubMed/NCBI View Article : Google Scholar
|
|
78
|
Blane D, Williams C, Morrison J, Wilson A
and Mercer S: Cognitive behavioural therapy: Why primary care
should have it all. Br J Gen Pract. 63:103–104. 2013.PubMed/NCBI View Article : Google Scholar
|
|
79
|
Chowdhary N, Sikander S, Atif N, Singh N,
Ahmad I, Fuhr DC, Rahman A and Patel V: The content and delivery of
psychological interventions for perinatal depression by
non-specialist health workers in low and middle income countries: A
systematic review. Best Pract Res Clin Obstet Gynaecol. 28:113–133.
2014.PubMed/NCBI View Article : Google Scholar
|
|
80
|
Homer CSE, Friberg IK, Dias MAB, ten
Hoope-Bender P, Sandall J, Speciale AM and Bartlett LA: The
projected effect of scaling up midwifery. Lancet. 384:1146–1157.
2014.PubMed/NCBI View Article : Google Scholar
|
|
81
|
Mendenhall E, De Silva MJ, Hanlon C,
Petersen I, Shidhaye R, Jordans M, Luitel N, Ssebunnya J, Fekadu A,
Patel V, et al: Acceptability and feasibility of using
non-specialist health workers to deliver mental health care:
Stakeholder perceptions from the PRIME district sites in Ethiopia,
India, Nepal, South Africa, and Uganda. Soc Sci Med. 118:33–42.
2014.PubMed/NCBI View Article : Google Scholar
|
|
82
|
Whitburn LY: Labour pa in: From the
physical brain to the conscious mind. J Psychosom Obstet Gynaecol.
34:139–143. 2013.PubMed/NCBI View Article : Google Scholar
|
|
83
|
Sandall J, Soltani H, Gates S, Shennan A
and Devane D: Midwife-led continuity models versus other models of
care for childbearing women. Cochrane Database Syst Rev.
4(CD004667)2016.PubMed/NCBI View Article : Google Scholar
|
|
84
|
Harmon LJ and Losos JB: The effect of
intraspecific sample size on type I and type II error rates in
comparative studies. Evolution. 59:2705–2710. 2005.PubMed/NCBI
|