|
1
|
Lee AM, Lam SK, Sze Mun Lau SM, Chong CS,
Chui HW and Fong DY: Prevalence, course, and risk factors for
antenatal anxiety and depression. Obstet Gynecol. 110:1102–1112.
2007.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Pawlby S, Hay DF, Sharp D, Waters CS and
O'Keane V: Antenatal depression predicts depression in adolescent
offspring: Prospective longitudinal community-based study. J Affect
Disord. 113:236–243. 2009.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Fisher J, Cabral de Mello M, Patel V,
Rahman A, Tran T, Holton S and Holmes W: Prevalence and
determinants of common perinatal mental disorders in women in low-
and lower-middle-income countries: A systematic review. Bull World
Health Organ. 90:139G–149G. 2012.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Husain N, Bevc I, Husain M, Chaudhry IB,
Atif N and Rahman A: Prevalence and social correlates of postnatal
depression in a low income country. Arch Women Ment Health.
9:197–202. 2006.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Engle PL: Maternal mental health: Program
and policy implications. Am J Clin Nutr. 89:963S–966S.
2009.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Saxena S, Funk M and Chisholm D: World
Health Assembly adopts Comprehensive Mental Health Action Plan
2013-2020. Lancet. 381:1970–1971. 2013.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Karmaliani R, Asad N, Bann CM, Moss N,
Mcclure EM, Pasha O, Wright LL and Goldenberg RL: Prevalence of
anxiety, depression and associated factors among pregnant women of
Hyderabad, Pakistan. Int J Soc Psychiatry. 55:414–424.
2009.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Rahman A, Bunn J, Lovel H and Creed F:
Association between antenatal depression and low birthweight in a
developing country. Acta Psychiatr Scand. 115:481–486.
2007.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Leung BMY and Kaplan BJ: Perinatal
depression: Prevalence, risks, and the nutrition link--a review of
the literature. J Am Diet Assoc. 109:1566–1575. 2009.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Waters CS, Hay DF, Simmonds JR and van
Goozen SHM: Antenatal depression and children's developmental
outcomes: Potential mechanisms and treatment options. Eur Child
Adolesc Psychiatry. 23:957–971. 2014.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Meltzer-Brody S: New insights into
perinatal depression: Pathogenesis and treatment during pregnancy
and postpartum. Dialogues Clin Neurosci. 13:89–100. 2011.PubMed/NCBI
|
|
12
|
Gelman PL, Flores-Ramos M, López-Martínez
M, Fuentes CC and Grajeda JPR: Hypothalamic-pituitary-adrenal axis
function during perinatal depression. Neurosci Bull. 31:338–350.
2015.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Kammerer M, Taylor A and Glover V: The HPA
axis and perinatal depression: A hypothesis. Arch Women Ment
Health. 9:187–196. 2006.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Perera F and Herbstman J: Prenatal
environmental exposures, epigenetics, and disease. Reprod Toxicol.
31:363–373. 2011.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Tarantino LM, Sullivan PF and
Meltzer-Brody S: Using animal models to disentangle the role of
genetic, epigenetic, and environmental influences on behavioral
outcomes associated with maternal anxiety and depression. Front
Psychiatry. 2(44)2011.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Nestler EJ, Barrot M, DiLeone RJ, Eisch
AJ, Gold SJ and Monteggia LM: Neurobiology of depression. Neuron.
34:13–25. 2002.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Bleker LS, de Rooij SR and Roseboom TJ:
Malnutrition and depression in pregnancy and associations with
child behaviour and cognitive function: A review of recent evidence
on unique and joint effects. Can J Physiol Pharmacol. 97:158–173.
2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Chung TK, Lau TK, Yip AS, Chiu HF and Lee
DT: Antepartum depressive symptomatology is associated with adverse
obstetric and neonatal outcomes. Psychosom Med. 63:830–834.
2001.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Waldenström U, Hildingsson I and Ryding
EL: Antenatal fear of childbirth and its association with
subsequent caesarean section and experience of childbirth. BJOG.
113:638–646. 2006.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Glover V and O'Connor TG: Effects of
antenatal stress and anxiety: Implications for development and
psychiatry. Br J Psychiatry. 180:389–391. 2002.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Misri S, Kendrick K, Oberlander TF, Norris
S, Tomfohr L, Zhang H and Grunau RE: Antenatal depression and
anxiety affect postpartum parenting stress: A longitudinal,
prospective study. Can J Psychiatry. 55:222–228. 2010.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Field T, Diego M and Hernandez-Reif M:
Prenatal depression effects on the fetus and newborn: A review.
Infant Behav Dev. 29:445–455. 2006.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Nguyen TM and Castro LC: Hypertensive
Disorders and Depression in Pregnancy: Pregnancy Complications and
Fetal Versus Neonatal Outcomes. J Womens Health (Larchmt).
28:1451–1453. 2019.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Brouwers EPM, van Baar AL and Pop VJM:
Maternal anxiety during pregnancy and subsequent infant
development. Infant Behav Dev. 24:95–106. 2001.
|
|
25
|
Dennis CL, Ross LE and Grigoriadis S:
Psychosocial and psychological interventions for treating antenatal
depression. Cochrane Database Syst Rev.
2007(CD006309)2007.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Milgrom J, Schembri C, Ericksen J, Ross J
and Gemmill AW: Towards parenthood: An antenatal intervention to
reduce depression, anxiety and parenting difficulties. J Affect
Disord. 130:385–394. 2011.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Atif N, Lovell K and Rahman A: Maternal
mental health: The missing ‘m’ in the global maternal and child
health agenda. Semin Perinatol. 39:345–352. 2015.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Demyttenaere K, Bruffaerts R, Posada-Villa
J, Gasquet I, Kovess V, Lepine JP, Angermeyer MC, Bernert S, de
Girolamo G, Morosini P, et al: WHO World Mental Health Survey
Consortium: Prevalence, severity, and unmet need for treatment of
mental disorders in the World Health Organization World Mental
Health Surveys. JAMA. 291:2581–2590. 2004.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Middleton H, Shaw I, Hull S and Feder G:
NICE guidelines for the management of depression. BMJ. 330:267–268.
2005.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Rahman A, Malik A, Sikander S, Roberts C
and Creed F: Cognitive behaviour therapy-based intervention by
community health workers for mothers with depression and their
infants in rural Pakistan: A cluster-randomised controlled trial.
Lancet. 372:902–909. 2008.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Anderson T: Feeling Safe Enough to Let Go:
The Relationship Between a Woman and her Midwife During the Second
Stage of Labour. In: The Midwife-Mother Relationship. Kirkham K
(ed). 2nd edition. Macmillan, Basingstoke, pp116-143, 2010.
|
|
32
|
Brugha TS, Smith J, Austin J, Bankart J,
Patterson M, Lovett C, Morgan Z, Morrell CJ and Slade P: Can
community midwives prevent antenatal depression? An external pilot
study to test the feasibility of a cluster randomized controlled
universal prevention trial. Psychol Med. 46:345–356.
2016.PubMed/NCBI View Article : Google Scholar
|
|
33
|
ten Hoope-Bender P, de Bernis L, Campbell
J, Downe S, Fauveau V, Fogstad H, Homer CS, Kennedy HP, Matthews Z,
McFadden A, et al: Improvement of maternal and newborn health
through midwifery. Lancet. 384:1226–1235. 2014.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Sandall J, Devane D, Soltani H, Hatem M
and Gates S: Improving quality and safety in maternity care: The
contribution of midwife-led care. J Midwifery Womens Health.
55:255–261. 2010.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Waldenström U and Turnbull D: A systematic
review comparing continuity of midwifery care with standard
maternity services. Br J Obstet Gynaecol. 105:1160–1170.
1998.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Attarha M, Keshavarz Z, Bakhtiari M and
Jamilian M: The Outcome of Midwife-Mother Relationship in Delivery
Room: A Qualitative Content Analysis. Health. 8:720–726. 2016.
|
|
37
|
Rorie JA, Paine LL and Barger MK: Primary
care for women. Cultural competence in primary care services. J
Nurse Midwifery. 41:92–100. 1996.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Hunter B: The importance of reciprocity in
relationships between community-based midwives and mothers.
Midwifery. 22:308–322. 2006.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Deery R and Hunter B: Emotion Work and
Relationships. In: The Midwife-Mother Relationship. Kirkham M (ed).
Palgrave Mcmillan, London, 2010.
|
|
40
|
Moher D, Liberati A, Tetzlaff J and Altman
DG: PRISMA Group. Preferred reporting items for systematic reviews
and meta-analyses: The PRISMA statement. PLoS Med.
6(e1000097)2009.PubMed/NCBI View Article : Google Scholar
|
|
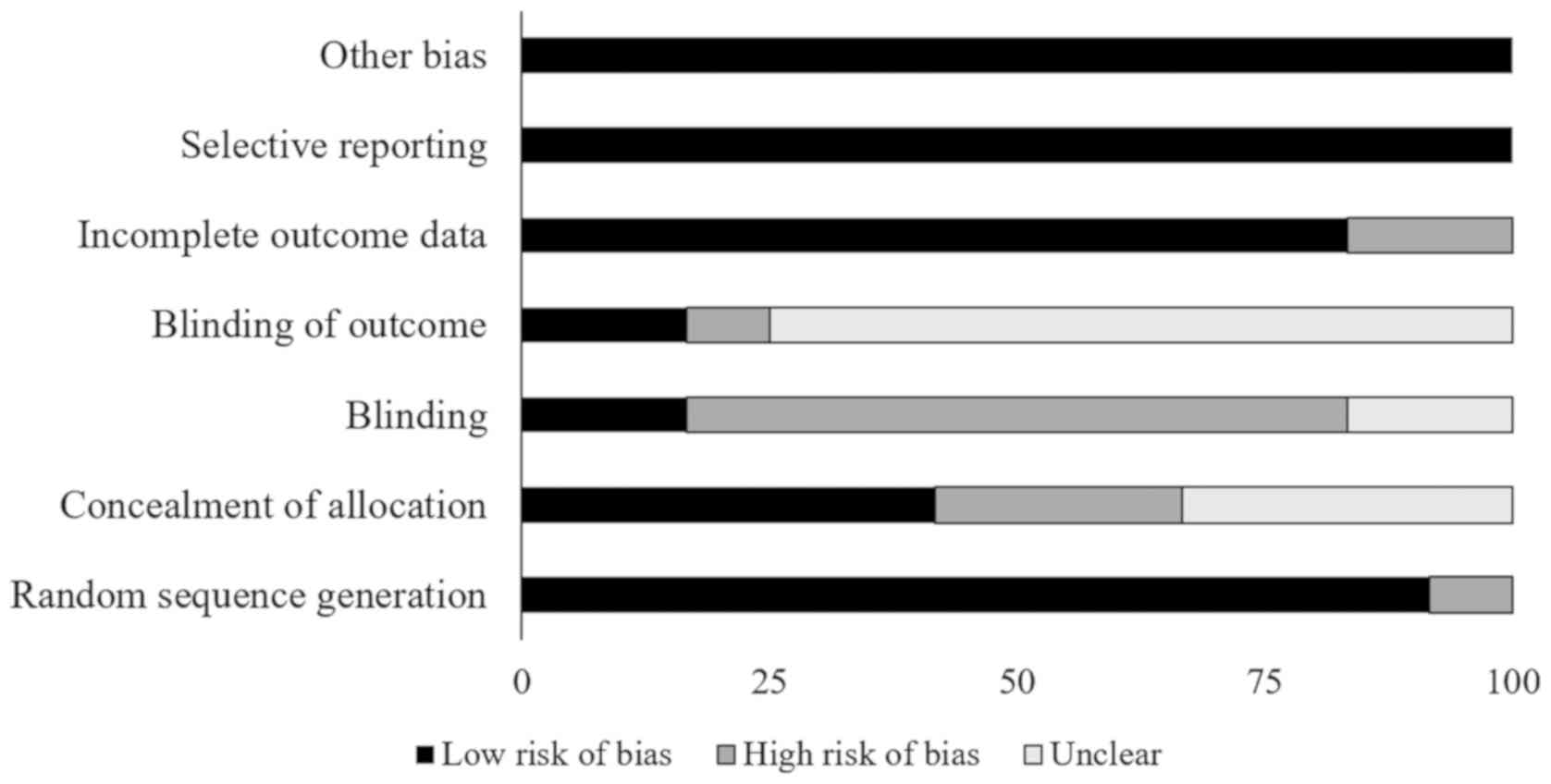
41
|
Jørgensen L, Paludan-Müller AS, Laursen
DRT, Savović J, Boutron I, Sterne JA, Higgins JP and Hróbjartsson
A: Evaluation of the Cochrane tool for assessing risk of bias in
randomized clinical trials: Overview of published comments and
analysis of user practice in Cochrane and non-Cochrane reviews.
Syst Rev. 5(80)2016.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Sterne JA, Hernán MA, Reeves BC, Savović
J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT,
Boutron I, et al: ROBINS-I: A tool for assessing risk of bias in
non-randomised studies of interventions. BMJ.
355(i4919)2016.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Viswanathan M, Ansari MT, Berkman ND, et
al: Assessing the Risk of Bias of Individual Studies in Systematic
Reviews of Health Care Interventions. In: Methods Guide for
Effectiveness and Comparative Effectiveness Reviews. Agency for
Healthcare Research and Quality (US), Rockville, MD, 2008.
|
|
44
|
Burns PB, Rohrich RJ and Chung KC: The
levels of evidence and their role in evidence-based medicine. Plast
Reconstr Surg. 128:305–310. 2011.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Bax L, Yu LM, Ikeda N and Moons KG: A
systematic comparison of software dedicated to meta-analysis of
causal studies. BMC Med Res Methodol. 7(40)2007.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Higgins JPT, Thompson SG and Spiegelhalter
DJ: A re-evaluation of random-effects meta-analysis. J R Stat Soc
Ser A Stat Soc. 172:137–159. 2009.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Rosenthal R: Parametric measures of effect
size. In: The handbook of research synthesis. Russell Sage
Foundation, New York, NY, pp231-244, 1994.
|
|
48
|
Higgins JPT and Thompson SG: Quantifying
heterogeneity in a meta-analysis. Stat Med. 21:1539–1558.
2002.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Petitti DB: Approaches to heterogeneity in
meta-analysis. Stat Med. 20:3625–3633. 2001.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Duval S and Tweedie R: Trim and fill: A
simple funnel-plot-based method of testing and adjusting for
publication bias in meta-analysis. Biometrics. 56:455–463.
2000.PubMed/NCBI View Article : Google Scholar
|
|
51
|
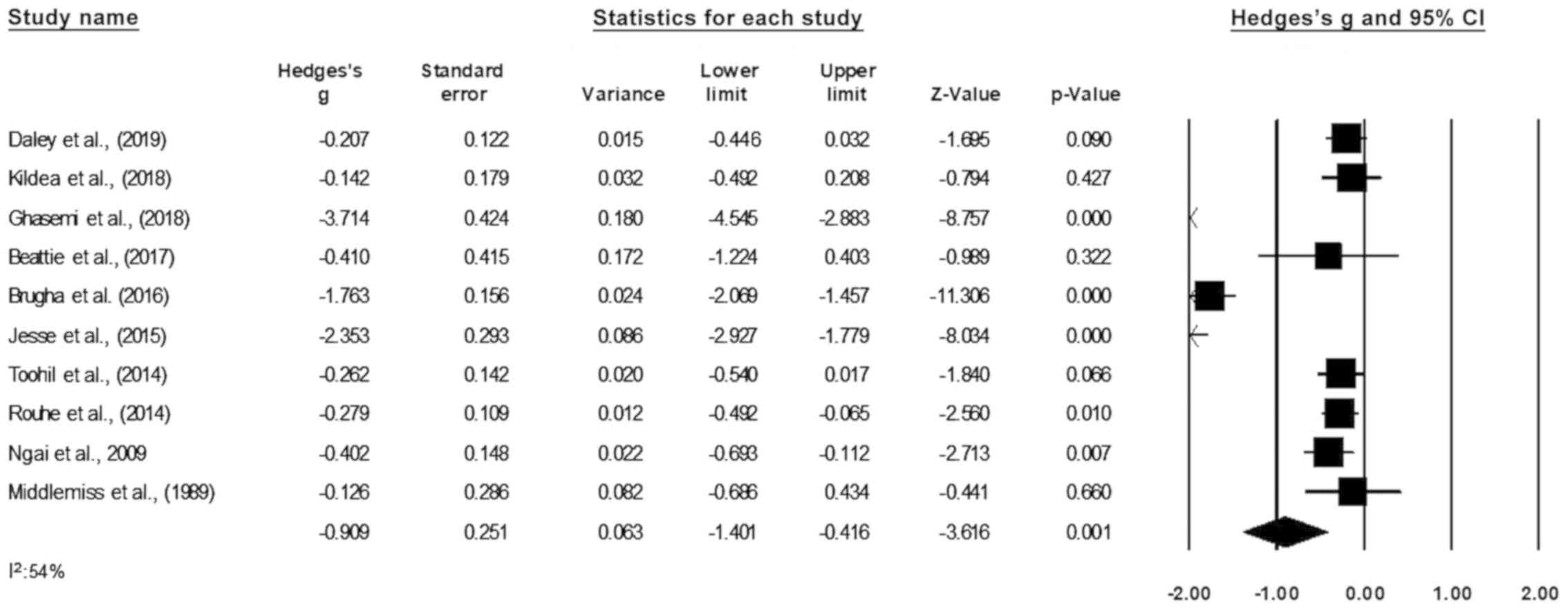
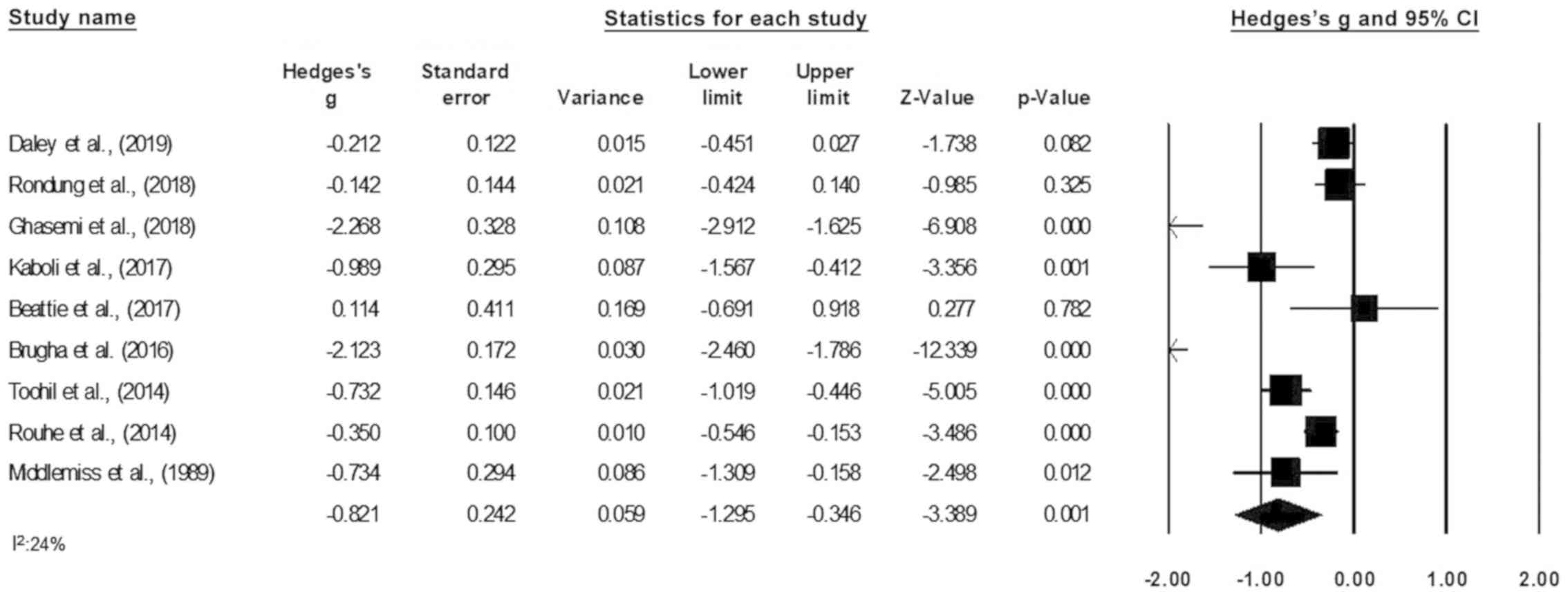
Beattie J, Hall H, Biro MA, East C and Lau
R: Effects of mindfulness on maternal stress, depressive symptoms
and awareness of present moment experience: A pilot randomised
trial. Midwifery. 50:174–183. 2017.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Burns A, O'Mahen H, Baxter H, Bennert K,
Wiles N, Ramchandani P, Turner K, Sharp D, Thorn J, Noble S, et al:
A pilot randomised controlled trial of cognitive behavioural
therapy for antenatal depression. BMC Psychiatry.
13(33)2013.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Daley A, Jolly K, Jebb SA, Roalfe A,
Mackilllop L, Lewis A, Clifford S, Usman M, Ohadike C, Kenyon S, et
al: Effectiveness of a behavioural intervention involving regular
weighing and feedback by community midwives within routine
antenatal care to prevent excessive gestational weight gain: POPS2
randomised controlled trial. BMJ Open. 9(e030174)2019.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Ghasemi F, Bolbol-Haghighi N, Mottaghi Z,
Hosseini SR and Khosravi A: The Effect of Group Counseling with
Cognitive-Behavioral Approach on Self-Efficacy of Pregnant Women's
Choice of Vaginal Delivery. Iran J Psychiatry Behav Sci In Press
(In Press).
|
|
55
|
Jesse DE, Gaynes BN, Feldhousen EB, Newton
ER, Bunch S and Hollon SD: Performance of a Culturally Tailored
Cognitive-Behavioral Intervention Integrated in a Public Health
Setting to Reduce Risk of Antepartum Depression: A Randomized
Controlled Trial. J Midwifery Womens Health. 60:578–592.
2015.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Kaboli KS, Mahmoodi Z, Tourzani ZM,
Tehranizadeh M, Kabir K and Dolatian M: The Effect of Group
Counseling Based on Cognitive-Behavioral Approach on
Pregnancy-Specific Stress and Anxiety. Shiraz E Med J (In
Press).
|
|
57
|
Kildea S, Simcock G, Liu A, Elgbeili G,
Laplante DP, Kahler A, Austin MP, Tracy S, Kruske S, Tracy M, et
al: Continuity of midwifery carer moderates the effects of prenatal
maternal stress on postnatal maternal wellbeing: The Queensland
flood study. Arch Womens Ment Health. 21:203–214. 2018.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Middlemiss C, Dawson AJ, Gough N, Jones ME
and Coles EC: A randomised study of a domiciliary antenatal care
scheme: Maternal psychological effects. Midwifery. 5:69–74.
1989.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Rondung E, Ternström E, Hildingsson I,
Haines HM, Sundin Ö, Ekdahl J, Karlström A, Larsson B, Segeblad B,
Baylis R, et al: Comparing Internet-Based Cognitive Behavioral
Therapy With Standard Care for Women With Fear of Birth: Randomized
Controlled Trial. JMIR Ment Health. 5(e10420)2018.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Rouhe H, Salmela-Aro K, Toivanen R, Tokola
M, Halmesmäki E, Ryding EL and Saisto T: Group psychoeducation with
relaxation for severe fear of childbirth improves maternal
adjustment and childbirth experience - a randomised controlled
trial. J Psychosom Obstet Gynaecol. 36:1–9. 2015.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Toohill J, Fenwick J, Gamble J, Creedy DK,
Buist A, Turkstra E and Ryding EL: A randomized controlled trial of
a psycho-education intervention by midwives in reducing childbirth
fear in pregnant women. Birth. 41:384–394. 2014.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Hildingsson I, Karlström A, Rubertsson C
and Haines H: Women with fear of childbirth might benefit from
having a known midwife during labour. Women Birth. 32:58–63.
2019.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Larsson B, Karlström A, Rubertsson C and
Hildingsson I: The effects of counseling on fear of childbirth.
Acta Obstet Gynecol Scand. 94:629–636. 2015.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Ngai FW, Chan SWC and Ip WY: The effects
of a childbirth psychoeducation program on learned resourcefulness,
maternal role competence and perinatal depression: A
quasi-experiment. Int J Nurs Stud. 46:1298–1306. 2009.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Turkstra E, Mihala G, Scuffham PA, Creedy
DK, Gamble J, Toohill J and Fenwick J: An economic evaluation
alongside a randomised controlled trial on psycho-education
counselling intervention offered by midwives to address women's
fear of childbirth in Australia. Sex Reprod Healthc. 11:1–6.
2017.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Hildingsson I, Rubertsson C, Karlström A
and Haines H: A known midwife can make a difference for women with
fear of childbirth- birth outcome and women's experiences of
intrapartum care. Sex Reprod Healthc. 21:33–38. 2019.PubMed/NCBI View Article : Google Scholar
|
|
67
|
Glover V: Maternal depression, anxiety and
stress during pregnancy and child outcome; what needs to be done.
Best Pract Res Clin Obstet Gynaecol. 28:25–35. 2014.PubMed/NCBI View Article : Google Scholar
|
|
68
|
Stoll K, Swift EM, Fairbrother N, Nethery
E and Janssen P: A systematic review of nonpharmacological prenatal
interventions for pregnancy-specific anxiety and fear of
childbirth. Birth. 45:7–18. 2018.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Dubovicky M, Belovicova K, Csatlosova K
and Bogi E: Risks of using SSRI / SNRI antidepressants during
pregnancy and lactation. Interdiscip Toxicol. 10:30–34.
2017.PubMed/NCBI View Article : Google Scholar
|
|
70
|
Wikner BN, Stiller CO, Bergman U, Asker C
and Källén B: Use of benzodiazepines and benzodiazepine receptor
agonists during pregnancy: Neonatal outcome and congenital
malformations. Pharmacoepidemiol Drug Saf. 16:1203–1210.
2007.PubMed/NCBI View Article : Google Scholar
|
|
71
|
Arch JJ, Dimidjian S and Chessick C: Are
exposure-based cognitive behavioral therapies safe during
pregnancy? Arch Women Ment Health. 15:445–457. 2012.PubMed/NCBI View Article : Google Scholar
|
|
72
|
Cho HJ, Kwon JH and Lee JJ: Antenatal
cognitive-behavioral therapy for prevention of postpartum
depression: A pilot study. Yonsei Med J. 49:553–562.
2008.PubMed/NCBI View Article : Google Scholar
|
|
73
|
Beck R and Fernandez E:
Cognitive-Behavioral Self-Regulation of the Frequency, Duration,
and Intensity of Anger. J Psychopathol Behav Assess. 20:217–229.
1998.
|
|
74
|
Mueser KT, Gottlieb JD, Xie H, Lu W, Yanos
PT, Rosenberg SD, Silverstein SM, Duva SM, Minsky S, Wolfe RS, et
al: Evaluation of cognitive restructuring for post-traumatic stress
disorder in people with severe mental illness. Br J Psychiatry.
206:501–508. 2015.PubMed/NCBI View Article : Google Scholar
|
|
75
|
Sockol LE: A systematic review of the
efficacy of cognitive behavioral therapy for treating and
preventing perinatal depression. J Affect Disord. 177:7–21.
2015.PubMed/NCBI View Article : Google Scholar
|
|
76
|
Silverstein M, Feinberg E, Cabral H,
Sauder S, Egbert L, Schainker E, Kamholz K, Hegel M and Beardslee
W: Problem-solving education to prevent depression among low-income
mothers of preterm infants: A randomized controlled pilot trial.
Arch Women Ment Health. 14:317–324. 2011.PubMed/NCBI View Article : Google Scholar
|
|
77
|
Beck A, Nadkarni A, Calam R, Naeem F and
Husain N: Increasing access to Cognitive Behaviour Therapy in Low
and Middle Income Countries: A strategic framework. Asian J
Psychiatr. 22:190–195. 2016.PubMed/NCBI View Article : Google Scholar
|
|
78
|
Blane D, Williams C, Morrison J, Wilson A
and Mercer S: Cognitive behavioural therapy: Why primary care
should have it all. Br J Gen Pract. 63:103–104. 2013.PubMed/NCBI View Article : Google Scholar
|
|
79
|
Chowdhary N, Sikander S, Atif N, Singh N,
Ahmad I, Fuhr DC, Rahman A and Patel V: The content and delivery of
psychological interventions for perinatal depression by
non-specialist health workers in low and middle income countries: A
systematic review. Best Pract Res Clin Obstet Gynaecol. 28:113–133.
2014.PubMed/NCBI View Article : Google Scholar
|
|
80
|
Homer CSE, Friberg IK, Dias MAB, ten
Hoope-Bender P, Sandall J, Speciale AM and Bartlett LA: The
projected effect of scaling up midwifery. Lancet. 384:1146–1157.
2014.PubMed/NCBI View Article : Google Scholar
|
|
81
|
Mendenhall E, De Silva MJ, Hanlon C,
Petersen I, Shidhaye R, Jordans M, Luitel N, Ssebunnya J, Fekadu A,
Patel V, et al: Acceptability and feasibility of using
non-specialist health workers to deliver mental health care:
Stakeholder perceptions from the PRIME district sites in Ethiopia,
India, Nepal, South Africa, and Uganda. Soc Sci Med. 118:33–42.
2014.PubMed/NCBI View Article : Google Scholar
|
|
82
|
Whitburn LY: Labour pa in: From the
physical brain to the conscious mind. J Psychosom Obstet Gynaecol.
34:139–143. 2013.PubMed/NCBI View Article : Google Scholar
|
|
83
|
Sandall J, Soltani H, Gates S, Shennan A
and Devane D: Midwife-led continuity models versus other models of
care for childbearing women. Cochrane Database Syst Rev.
4(CD004667)2016.PubMed/NCBI View Article : Google Scholar
|
|
84
|
Harmon LJ and Losos JB: The effect of
intraspecific sample size on type I and type II error rates in
comparative studies. Evolution. 59:2705–2710. 2005.PubMed/NCBI
|