|
1
|
Wiener G, Moore HB, Moore EE, Gonzalez E,
Diamond S, Zhu S, D'Alessandro A and Banerjee A: Shock releases
bile acid inducing platelet inhibition and fibrinolysis. J Surg
Res. 195:390–395. 2015.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Bertók L: Role of endotoxins and bile
acids in the pathogenesis of septic circulatory shock. Acta Chir
Hung. 36:33–36. 1997.PubMed/NCBI
|
|
3
|
Engler S, Elsing C, Flechtenmacher C,
Theilmann L, Stremmel W and Stiehl A: Progressive sclerosing
cholangitis after septic shock: A new variant of vanishing bile
duct disorders. Gut. 52:688–693. 2003.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Luyer MD, Buurman WA, Hadfoune M, Jacobs
JA, Dejong CH and Greve JW: High-fat enteral nutrition reduces
endotoxin, tumor necrosis factor-alpha and gut permeability in bile
duct-ligated rats subjected to hemorrhagic shock. J Hepatol.
41:377–383. 2004.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Xu C, Huang XE, Wang SX, Lv PH, Sun L and
Wang FA: Comparison of infection between internal-external and
external percutaneous transhepatic biliary drainage in treating
patients with malignant obstructive jaundice. Asian Pac J Cancer
Prev. 16:2543–2546. 2015.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Saettini F, Agazzi R, Giraldi E, Foglia C,
Cavalleri L, Morali L, Fasolini G, Spotti A and Provenzi M:
Percutaneous transhepatic biliary drainage in an infant with
obstructive jaundice caused by neuroblastoma. Pediatr Hematol
Oncol. 32:223–228. 2015.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Arkadopoulos N, Kyriazi MA, Papanikolaou
IS, Vasiliou P, Theodoraki K, Lappas C, Oikonomopoulos N and
Smyrniotis V: Preoperative biliary drainage of severely jaundiced
patients increases morbidity of pancreaticoduodenectomy: Results of
a case-control study. World J Surg. 38:2967–2972. 2014.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Shinya S, Sasaki T, Yamashita Y, Kato D,
Yamashita K, Nakashima R, Yamauchi Y and Noritomi T: Procalcitonin
as a useful biomarker for determining the need to perform emergency
biliary drainage in cases of acute cholangitis. J Hepatobiliary
Pancreat Sci. 21:777–785. 2014.PubMed/NCBI View
Article : Google Scholar
|
|
9
|
McNabb-Baltar J, Trinh QD and Barkun AN:
Biliary drainage method and temporal trends in patients admitted
with cholangitis: A national audit. Can J Gastroenterol.
27:513–518. 2013.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Itoi T, Tsuyuguchi T, Takada T, Strasberg
SM, Pitt HA, Kim MH, Belli G, Mayumi T, Yoshida M, Miura F, et al:
TG13 indications and techniques for biliary drainage in acute
cholangitis (with videos). J Hepatobiliary Pancreat Sci. 20:71–80.
2013.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Abdelkader AM, Zidan AM and Younis MT:
Temporary CBD stenting with a nelaton tube is a more practical and
safer option than T-tube drainage after conventional CBD
exploration for choledocholithiasis. HPB Surg.
2018(8035164)2018.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Wang L, Zhao B, Chen Y, Ma L, Chen EZ and
Mao EQ: Biliary tract external drainage protects against intestinal
barrier injury in hemorrhagic shock rats. World J Gastroenterol.
21:12800–12813. 2015.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Wang L, Zhao B, Chen Y, Ma L, Chen EZ and
Mao EQ: Inflammation and edema in the lung and kidney of
hemorrhagic shock rats are alleviated by biliary tract external
drainage via the heme oxygenase-1 pathway. Inflammation.
38:2242–2251. 2015.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Wang L, Zhao B, Chen Y, Ma L, Chen EZ and
Mao EQ: Biliary tract external drainage increases the expression
levels of heme oxygenase-1 in rat livers. Eur J Med Res.
20(61)2015.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Wang L, Zhao B, Chen Y, Ma L, Chen EZ and
Mao EQ: Biliary tract external drainage alleviates kidney injury in
shock. J Surg Res. 199:564–571. 2015.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Suzuki H, Iyomasa S, Nimura Y and Yoshida
S: Internal biliary drainage, unlike external drainage, does not
suppress the regeneration of cholestatic rat liver after partial
hepatectomy. Hepatology. 20:1318–1322. 1994.PubMed/NCBI
|
|
17
|
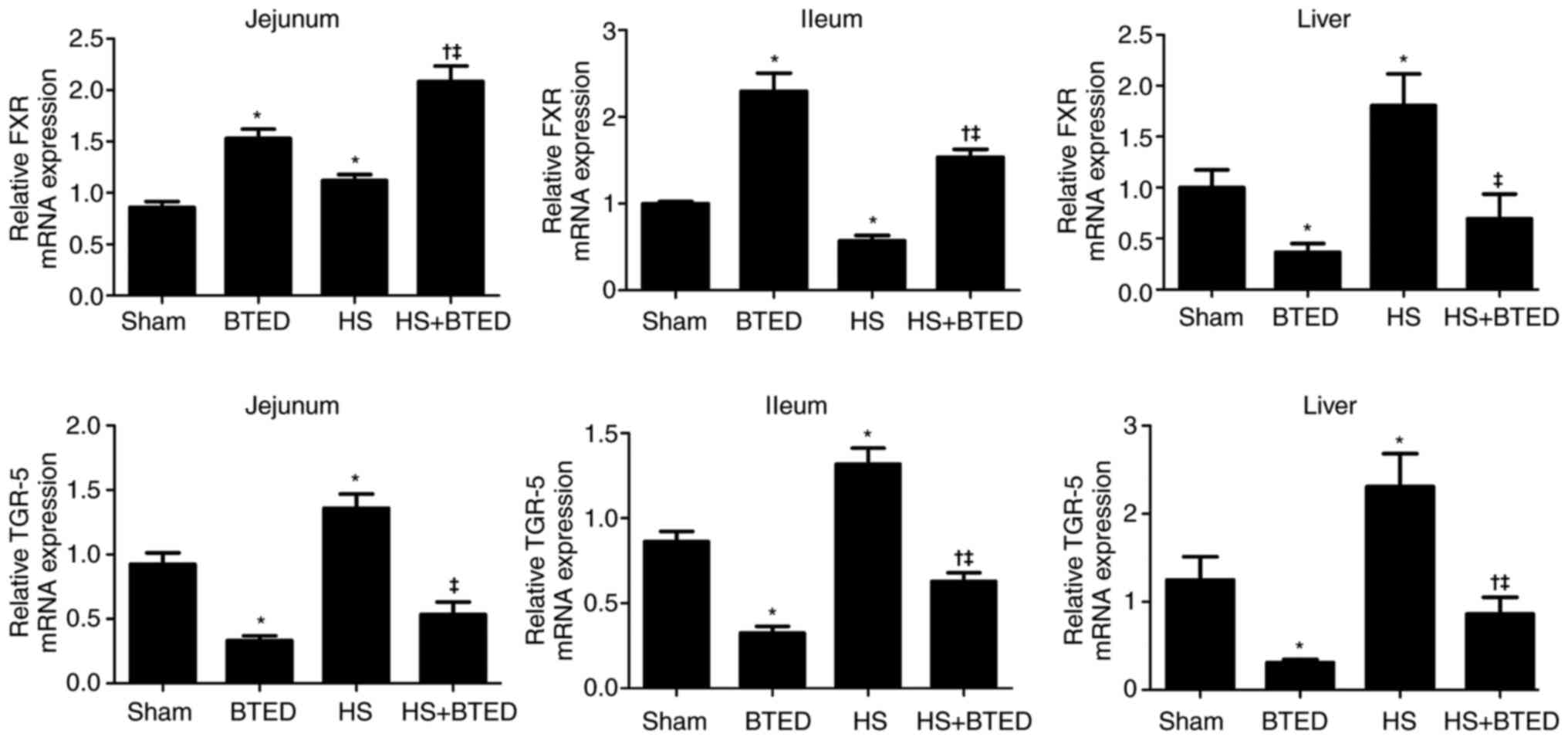
Iracheta-Vellve A, Calenda CD, Petrasek J,
Ambade A, Kodys K, Adorini L and Szabo G: FXR and TGR5 agonists
ameliorate liver injury, steatosis, and inflammation after binge or
prolonged alcohol feeding in mice. Hepatol Commun. 2:1379–1391.
2018.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Mertens KL, Kalsbeek A, Soeters MR and
Eggink HM: Bile acid signaling pathways from the enterohepatic
circulation to the central nervous system. Front Neurosci.
11(617)2017.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Wang YD, Chen WD, Moore DD and Huang W:
FXR: A metabolic regulator and cell protector. Cell Res.
18:1087–1095. 2008.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Lee FY, Lee H, Hubbert ML, Edwards PA and
Zhang Y: FXR, a multipurpose nuclear receptor. Trends Biochem Sci.
31:572–580. 2006.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Horikawa T, Oshima T, Li M, Kitayama Y,
Eda H, Nakamura K, Tamura A, Ogawa T, Yamasaki T, Okugawa T, et al:
Chenodeoxycholic acid releases proinflammatory cytokines from small
intestinal epithelial cells through the farnesoid X receptor.
Digestion. 100:286–294. 2019.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Tuominen I and Beaven SW: Intestinal
farnesoid X receptor puts a fresh coat of wax on fatty liver.
Hepatology. 62:646–648. 2015.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Hou Y, Fan W, Yang W, Samdani AQ, Jackson
AO and Qu S: Farnesoid X receptor: An important factor in blood
glucose regulation. Clin Chim Acta. 495:29–34. 2019.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Meng Q, Chen X, Wang C, Liu Q, Sun H, Sun
P, Peng J and Liu K: Alisol B 23-acetate promotes liver
regeneration in mice after partial hepatectomy via activating
farnesoid X receptor. Biochem Pharmacol. 92:289–298.
2014.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Zhang L, Wang YD, Chen WD, Wang X, Lou G,
Liu N, Lin M, Forman BM and Huang W: Promotion of liver
regeneration/repair by farnesoid X receptor in both liver and
intestine in mice. Hepatology. 56:2336–2343. 2012.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Chen WD, Wang YD, Zhang L, Shiah S, Wang
M, Yang F, Yu D, Forman BM and Huang W: Farnesoid X receptor
alleviates age-related proliferation defects in regenerating mouse
livers by activating forkhead box m1b transcription. Hepatology.
51:953–962. 2010.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Kawamata Y, Fujii R, Hosoya M, Harada M,
Yoshida H, Miwa M, Fukusumi S, Habata Y, Itoh T, Shintani Y, et al:
A G protein-coupled receptor responsive to bile acids. J Biol Chem.
278:9435–9440. 2003.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Finn PD, Rodriguez D, Kohler J, Jiang Z,
Wan S, Blanco E, King AJ, Chen T, Bell N, Dragoli D, et al:
Intestinal TGR5 agonism improves hepatic steatosis and insulin
sensitivity in Western diet-fed mice. Am J Physiol Gastrointest
Liver Physiol. 316:G412–G424. 2019.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Fiorucci S, Mencarelli A, Palladino G and
Cipriani S: Bile-acid-activated receptors: Targeting TGR5 and
farnesoid-X-receptor in lipid and glucose disorders. Trends
Pharmacol Sci. 30:570–580. 2009.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Jourdainne V, Péan N, Doignon I, Humbert
L, Rainteau D and Tordjmann T: The bile acid receptor TGR5 and
liver regeneration. Dig Dis. 33:319–326. 2015.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Péan N, Doignon I, Garcin I, Besnard A,
Julien B, Liu B, Branchereau S, Spraul A, Guettier C, Humbert L, et
al: The receptor TGR5 protects the liver from bile acid overload
during liver regeneration in mice. Hepatology. 58:1451–1460.
2013.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Berquist TH, May GR, Johnson CM, Adson MA
and Thistle JL: Percutaneous biliary decompression: Internal and
external drainage in 50 patients. AJR Am J Roentgenol. 136:901–906.
1981.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408.
2001.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Gordon D and Spiegel R: Fluid
resuscitation: History, physiology, and modern fluid resuscitation
strategies. Emerg Med Clin North Am. 38:783–793. 2020.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Nakatani T and Kobayashi K: Post-traumatic
jaundice-its mechanism from a view point of hepatic mitochondrial
function. Nihon Geka Gakkai Zasshi. 92:441–447. 1991.PubMed/NCBI(In Japanese).
|
|
36
|
Shimada H, Nakagawara G, Kobayashi M,
Tsuchiya S, Kudo T and Morita S: Pathogenesis and clinical features
of acute cholangitis accompanied by shock. Jpn J Surg. 14:269–277.
1984.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Okaya T, Nakagawa K, Kimura F, Shimizu H,
Yoshidome H, Ohtsuka M, Kato A, Yoshitomi H, Ito H and Miyazaki M:
The alterations in hepatic microcirculation and Kupffer cell
activity after biliary drainage in jaundiced mice. J Hepatobiliary
Pancreat Sci. 19:397–404. 2012.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Otao R, Beppu T, Isiko T, Mima K, Okabe H,
Hayashi H, Masuda T, Chikamoto A, Takamori H and Baba H: External
biliary drainage and liver regeneration after major hepatectomy. Br
J Surg. 99:1569–1574. 2012.PubMed/NCBI View
Article : Google Scholar
|
|
39
|
Iyomasa S, Terasaki M, Kuriki H, Nimura Y,
Shionoya S, Kojima K and Yoshida S: Decrease in regeneration
capacity of rat liver after external biliary drainage. Eur Surg
Res. 24:265–272. 1992.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Yoshida Y, Ajiki T, Ueno K, Shinozaki K,
Murakami S, Okazaki T, Matsumoto T, Matsumoto I, Fukumoto T, Usami
M and Ku Y: Preoperative bile replacement improves immune function
for jaundiced patients treated with external biliary drainage. J
Gastrointest Surg. 18:2095–2104. 2014.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Ferrell JM, Pathak P, Boehme S, Gilliland
T and Chiang JY: Deficiency of both farnesoid X receptor and takeda
G protein-coupled receptor 5 exacerbated liver fibrosis in mice.
Hepatology. 70:955–970. 2019.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Ding L, Yang Y, Qu Y, Yang T, Wang K, Liu
W and Xia W: Bile acid promotes liver regeneration via farnesoid X
receptor signaling pathways in rats. Mol Med Rep. 11:4431–4437.
2015.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Garcia-Rodriguez JL, Barbier-Torres L,
Fernández-Álvarez S, Gutiérrez-de Juan V, Monte MJ, Halilbasic E,
Herranz D, Álvarez L, Aspichueta P, Marín JJ, et al: SIRT1 controls
liver regeneration by regulating bile acid metabolism through
farnesoid X receptor and mammalian target of rapamycin signaling.
Hepatology. 59:1972–1983. 2014.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Fan M, Wang X, Xu G, Yan Q and Huang W:
Bile acid signaling and liver regeneration. Biochim Biophys Acta.
1849:196–200. 2015.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Sun Q, Fang F, Lu GC, Mao HH, Xu JH, Zhou
SK, Tong XM, Guo Y, Wu JF and Jiang B: Effects of different
drainage methods on serum bile acid and hepatocyte apoptosis and
regeneration after partial hepatectomy in rats with obstructive
jaundice. J Biol Regul Homeost Agents. 33:571–579. 2019.PubMed/NCBI
|
|
46
|
Jung K, Kim M, So J, Lee SH, Ko S and Shin
D: Farnesoid X receptor activation impairs liver progenitor
cell-mediated liver regeneration via the PTEN-PI3K-AKT-mTOR axis in
zebrafish. Hepatology. 74:397–410. 2021.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Chiang JYL and Ferrell JM: Bile acid
receptors FXR and TGR5 signaling in fatty liver diseases and
therapy. Am J Physiol Gastrointest Liver Physiol. 318:G554–G573.
2020.PubMed/NCBI View Article : Google Scholar
|