Introduction
In impoverished nations, tuberculosis (TB) has
historically been a devastating infectious disease (1). Spinal TB (STB) is the most frequently
occurring form of extrapulmonary TB, accounting for 50% of all
skeletal TB cases (2). The primary
treatment for STB is anti-TB chemotherapy; however, surgical
treatment is useful for the alleviation of kyphosis-associated
clinical symptoms, easing spinal cord compression and eliminating
abscesses (3,4).
In 1968, Wiltse proposed a new method for spinal
surgery that utilizes the gap between the multifidus and
longissimus muscles. This approach significantly reduces the
dissection time and traction of the multifidus muscle during
surgery. It also takes full advantage of the integrity of the
posterior bone and ligamentous structural complexes (5). The Wiltse transforaminal thoracic
interbody fusion (TTIF) surgical approach has demonstrated
excellent results in the treatment of intervertebral disc
herniation and STB (6). However,
reports on its application in the surgical treatment of
single-segment thoracic TB (SSTTB) in elderly patients with
osteoporosis are limited in the available literature, with the
exception of a few case reports published in mainstream academic
journals. In the present study, the preoperative and postoperative
information of 20 patients with SSTTB who underwent Wiltse TTIF at
a single institution were evaluated to assess the effects of this
surgical approach on older patients with osteoporosis.
Materials and methods
Criteria for patient inclusion and
exclusion
Wiltse TTIF is standard clinical surgical procedure
and the Ethics Committee of the First Affiliated Hospital of
Guangxi Medical University (Nanning, China) approved the present
study (ref. no. KY-E-152). All patients provided written informed
consent for inclusion in this retrospective study. Between January
2017 and January 2019, the same surgeon operated on 20 elderly
patients with SSTTB and osteoporosis at the First Affiliated
Hospital of Guangxi Medical University. There were 12 males and 8
females, ranging in age from 65 to 80 years (mean, 70.25±4.19
years). The following criteria were used to make a diagnosis: i)
Clinical symptoms and signs; ii) computed tomography (CT) and
magnetic resonance imaging (MRI) findings; iii) laboratory test
results, including hemoglobin, erythrocyte sedimentation rate (ESR)
and C-reactive protein (CRP) concentration, as well as TB antibody
(IgG and IgM) and tuberculin skin tests; iv) anti-TB chemotherapy
was effective, as indicated by obvious radiographic changes; and v)
histological microscopy and acid-fast bacillus test as the gold
standard. The exclusion criteria were as follows: i) age <65
years; ii) normal femoral neck bone mineral density (BMD) T-score
>-2.5(7); iii) no neurological
deficits; iv) multi-segment disease or lesions that require
anterior bone fusion; and v) inaccessible para-vertebral or deep
muscle abscesses and severe kyphotic deformities (>50˚). Only
patients with neurological deficits were selected to reflect the
characteristics and efficacy of Wiltse TTIF more clearly. The
Frankel classification was used to assess nerve damage as follows:
Grade A, complete loss of movement and sensation below the lesion
level; Grade B, partial loss of sensation below the lesion level;
Grade C, motor and sensory preservation below the lesion level, but
with loss of function; Grade D, movement and sensation below the
lesion plane are preserved, but with limited mobility; and Grade E,
normal function.
Preoperative procedure
The majority of the patients were diagnosed with and
treated for STB in the First Affiliated Hospital of Guangxi Medical
University, and received anti-TB chemotherapy with the isoniazid,
rifampicin, ethambutol and pyrazinamide (HREZ) regimen for 2-4
weeks prior to surgery. The remaining few patients came to the
hospital for treatment after they had started anti-TB treatment
with the HREZ regimen elsewhere. As their symptoms gradually
worsened they were referred to the First Affiliated Hospital of
Guangxi Medical University for surgical treatment. In a small
number of cases, the patients had complex and changeable symptoms,
and the diagnosis of TB was challenging. Therefore, anti-TB
treatment was administered and if it was found that the symptoms of
these patients improved significantly after anti-TB treatment, a
diagnosis of TB was made. Patients who were paralyzed had received
anti-TB treatment prior to admission to the hospital, and when they
were admitted to the hospital, they had surgery immediately. One
notable patient had been treated with the HREZ scheme for 3 weeks
in the infectious diseases department of the First Affiliated
Hospital of Guangxi Medical University, but his symptoms gradually
worsened and paralysis occurred, so he immediately received
surgery. The HREZ chemotherapy regimen constituted part of the
anti-TB regimen and comprised the following drugs: Isoniazid (5-10
mg/kg/day), rifampicin (5-10 mg/kg/day), ethambutol (15 mg/kg/day)
and pyrazinamide (25 mg/kg/day). The anti-TB drug HREZ when used
preoperatively has two functions, one of which is the effective
control of TB while the other is to improve the tolerance of
patients to surgery and promote postoperative recovery. Patient's
temperature was measured four times a day. Blood tests were
performed every 3 days. Surgery was performed when anemia and
hypoalbuminemia were completely under control and the ESR, CRP and
body temperature of the patient had returned to normal or were
markedly decreased. Calcitriol (0.25 µg/day) and calcium carbonate
D3 (1 g/day) were administered orally prior to surgery in patients
who had osteoporosis. Furthermore, zoledronic (4 mg) acid was
infused intravenously once per year for 3-5 years after the surgery
until the femoral neck BMD returned to normal levels.
Surgical procedure
After receiving general anesthesia, patients were
placed in the prone position and an X-ray of the C-arm was used to
locate the surgical segment. The preoperative MRI indicated the
distance separating the muscle space from spinous processes. The
subcutaneous tissues and fascia were then carefully separated by
making a posterior midline longitudinal incision until the medial
multifidus and lateral longissimus muscles were separated, and the
intermuscular space was entered. The paravertebral muscles were
then separated using a hemilaminectomy retractor to reveal the
transverse processes, laminae and interlaminar spaces.
Subsequently, in order to avoid complications such as loosening,
fracture and delayed healing after screw implantation in elderly
patients with osteoporosis, pedicle screws were implanted under the
guidance of C-arm CT. If only one side of the vertebral body was
involved, a screw was implanted on the uninvolved side, and then
two screws were applied to the vertebral bodies above and below the
affected vertebral body. If it was not possible to implant screws
into the affected vertebral body, then two screws were respectively
applied to the two vertebral bodies above the affected vertebral
body and two screws were respectively applied to the two vertebral
bodies below the affected vertebral body. During local debridement
and decompression, a temporary pre-curved rod was placed on the
side where the spinal cord and nerves were less compressed, to
prevent spinal instability. Subsequently, unilateral facetectomy
and laminectomy were performed along the medial pedicle on the side
with symptoms or severe paravertebral abscess. A rib adjacent to
the costovertebral joint was removed, if necessary. In cases where
improved exposure was required, the thoracic nerve root was
sacrificed. The extent of paravertebral abscesses and degree of
spinal stenosis typically determined the decompression range. The
paravertebral space was flushed using a suitable flushing tube
until pus was no longer observed. Subsequently, the necrotic
vertebrae and discs were removed with a curette until only healthy
bones remained. Then, the titanium cage was placed in position, the
rods were tightened, and kyphosis was slowly and carefully
corrected via the compression and extension of the internal
fixation instruments. Following local debridement and
decompression, the involved segments were fused posteriorly with
allografts or autografted bone. Relatively large pieces of bone
were used for grafting when the defects were loose or extensive.
Grafts obtained from debridement could also be used to fill this
gap. A combination of 1.0 g streptomycin and 0.2 g isoniazid was
then administered locally. Drainage was preferentially performed
using negative pressure drainage. The resected specimens were sent
for postoperative bacterial culture and pathological diagnosis.
Postoperative care
When <30 ml drainage was observed, which usually
occurred on postoperative day 3, the negative-pressure drainage
tube was removed. Continuous administration of oral HREZ anti-TB
chemotherapy was performed until 6 months postoperatively.
Pyrazinamide was then discontinued and an HRE regimen was
administered over the next 9-12 months. Postoperative treatment for
osteoporosis was continued for ≥3 months postoperatively. To
promote bone graft fusion and prevent the internal fixation from
loosening, bed rest for ≥3 months and the use of braces during
limited activities were advised for patients with severe
osteoporosis who had undergone extensive bone grafting. At 1 week
and 3, 6 and 12 months after surgery, all patients underwent
clinical and radiological examinations. Annual follow-up visits
were recommended following these examinations. Postoperative
follow-up CT was also recommended to assess the degree of graft
fusion, complete bone union, pseudoarthrosis and other
conditions.
Statistical analysis
The values are expressed as the mean ± standard
deviation. The statistical significance of differences in kyphosis
angle, ESR and CRP at preoperative, postoperative, 3-month
postoperative and final follow-up time points were assessed using
univariate repeated measure ANOVA with Bonferroni hoc test.
Friedman and Nemenyi tests were used to assess the statistical
significance of differences in Frankel grades at the aforementioned
time points. The analysis was performed using SPSS software
(version 24.0; IBM Corp.). P<0.05 was considered to indicate a
statistically significant difference.
Results
Basic conditions
In total, 20 cases were examined, 12 of which were
male and 8 female, with an average age of 70.25±4.19 years. The
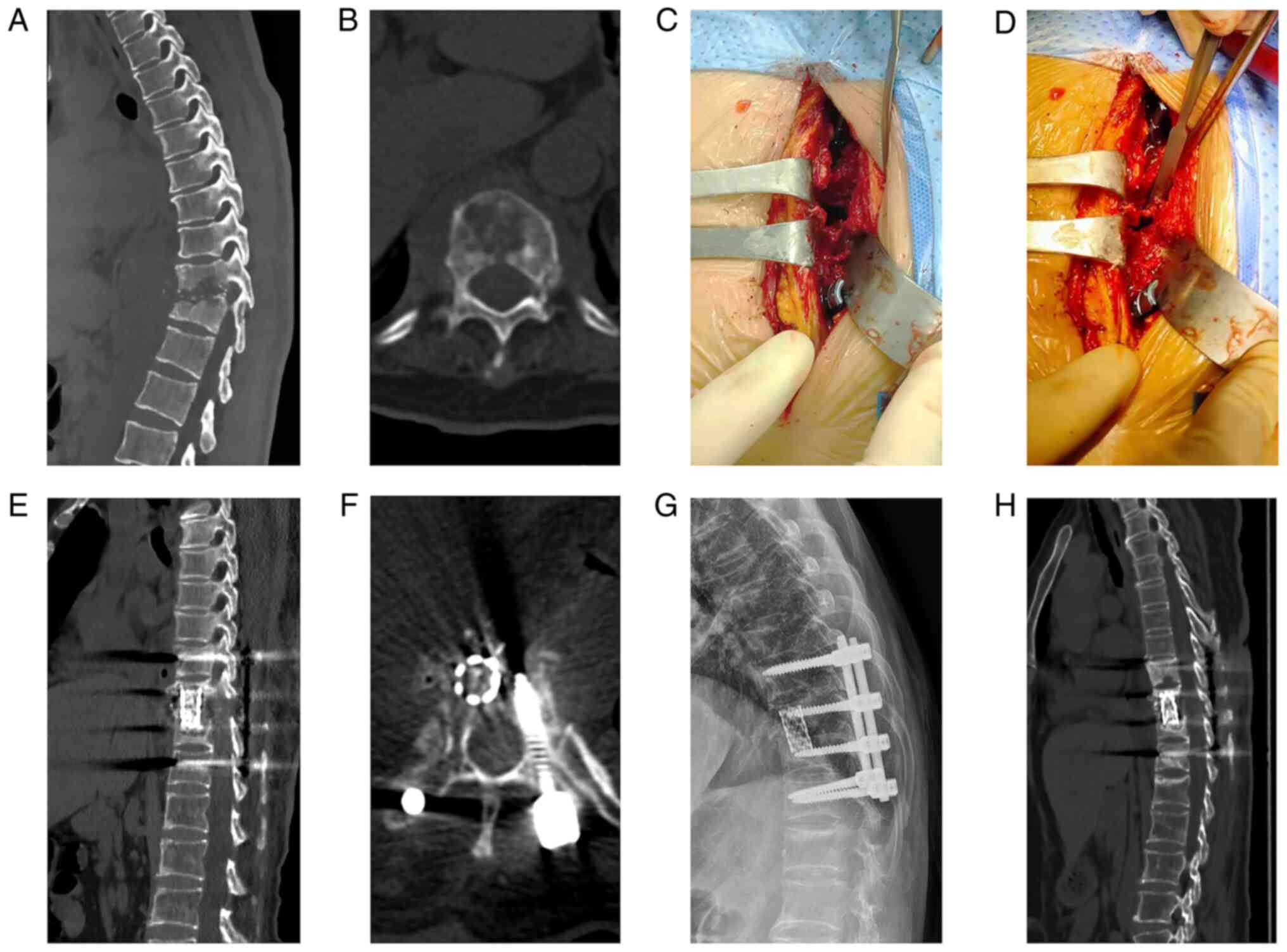
involved thoracic segments are shown in Fig. 1. The mean duration of surgery was
155.00±52.92 min, and the mean intraoperative blood loss was
153.75±41.64 ml. The mean length of hospital stay was 6.80±1.51
days, and the follow-up period was 37.15±7.37 months. The average
BMD T-score was -4.27±1.51 (Table
I). During the follow-up period, postoperative complications
included cerebrospinal fluid leakage (1 case), imbalanced water and
electrolytes (5 cases), infection of a superficial wound (1 case)
and mild intestinal obstruction (2 cases). The internal fixation
and bone grafting were not associated with any complications.
Following the first week of anti-inflammatory or symptomatic
supportive treatment, the symptoms of the patients markedly
improved.
 | Table IClinical details of the 20 patients
with single-segment thoracic tuberculosis. |
Table I
Clinical details of the 20 patients
with single-segment thoracic tuberculosis.
| Parameter | Mean ± SD |
|---|
| Duration of surgery,
min | 155.00±52.92 |
| Intraoperative blood
loss, ml | 153.75±41.64 |
| Hospital stay,
days | 6.80±1.51 |
| Follow-up period,
months | 37.15±7.37 |
| BMD T-score | -4.27±1.51 |
| Bony fusion,
months | 7.70±1.46 |
Nervous system status
The neurological symptoms of all patients gradually
improved during the follow-up period. The results of the
preoperative Frankel classification assessment were as follows:
Grade A, 1 case; Grade B, 3 cases; Grade C, 7 cases; and Grade D, 9
cases. Only two patients had Grade D at the most recent follow-up,
and the remaining 18 patients had full functional recovery and were
classified as Grade E (Fig. 2). At
the most recent follow-up, the statistical analysis revealed a
significant difference (P=0.012; Table II) between the preoperative and
postoperative Frankel classifications.
 | Table IIStatistical analysis of the clinical
results. |
Table II
Statistical analysis of the clinical
results.
| Schedule | Preoperative | Postoperative | 3 months after
surgery | Final follow-up |
X2/Fa | P-value |
|---|
| Frankel, n | | | | | 10.886 | 0.012 |
|
A | 1 | 0 | 0 | 0 | | |
|
B | 3 | 1 | 0 | 0 | | |
|
C | 7 | 3 | 1 | 0 | | |
|
D | 9 | 6 | 5 | 2 | | |
|
E | 0 | 10 | 14 | 18 | | |
| Kyphosis angle,
˚ | 35.41±6.71 |
8.80±0.79b |
9.23±0.53b |
9.99±0.92b-d | 344.532 | <0.001 |
| ESR, mm/h | 68.70±16.76 |
19.85±3.50b |
8.45±1.73b,c |
6.45±1.03b,c,d | 426.787 | <0.001 |
| CRP, mg/l | 25.15±9.60 |
9.09±3.01b | 4.8±1.95b,c | 5.1±1.62b,c | 94.901 | <0.001 |
Kyphosis, bone fusion, ESR and
CRP
The mean preoperative kyphotic angle was
35.41±6.71˚, which significantly reduced to 8.80±0.79˚
postoperatively (P<0.05). At the last follow-up, the mean
kyphotic angle was 9.99±0.92˚ with a correction loss of 1.18±0.37˚,
and the difference from the previous angles was statistically
significant (P<0.05). A statistically significant difference was
also detected between the preoperative and postoperative ESR and
CRP levels (both P<0.05; Table
II). Postoperative lateral X-ray/CT was used to measure the
degree of fusion in all patients after bone grafting and impact
drafting. Within 7.70±1.46 months after surgery, all patients had
adequate bone fusion (Table I).
Representative images for a single patient are presented in
Fig. 3.
Discussion
Approximately one-half of all cases of bone and
joint TB are STB, a common musculoskeletal disease (2). Despite ongoing efforts by the World
Health Organization and local health authorities, TB continues to
affect vulnerable individuals, including the elderly (8).
The most commonly used treatment options for STB
include anti-TB medication, bed rest and supportive medication.
However, in the absence of drug treatment, the risks of surgery,
mortality, infection transmission and recurrence are often greatly
increased (9). The risks
associated with surgical treatment are also markedly increased due
to elderly patients frequently having various accompanying chronic
diseases or disorders. Therefore, anti-TB chemotherapy and
conservative treatments are preferred over surgical treatment for
elderly patients to avoid the risks and complications associated
with surgery. However, this may result in the onset of neurological
symptoms and the worsening of any existing spinal deformities
(10). Similarly, prolonged bed
rest as part of conservative treatment not only has an impact on
quality of life but also has associated adverse effects. The
inability of anti-TB drugs to penetrate tuberculous bone lesions
results in inadequate or ineffective treatment. As a result, the
removal of necrotic tissues and paravertebral abscesses,
alleviation of neurological symptoms, and improvement or
stabilization of spinal deformities all require surgical treatment
in elderly patients.
However, there are conflicting opinions regarding
the surgical options for elderly patients with SSTTB. Although
anterior surgery is effective in correcting kyphosis and relieving
nerve compression (11), it does
not directly remove tuberculous lesions or facilitate bone
grafting. Additionally, the mediastinal organs, sternum, clavicle
and ribs interfere with surgical procedures, making anterior
surgery more challenging and prone to intra- and postoperative
complications. The combined anterior-posterior approach has a
positive clinical effect, but requires at least two separate
surgeries, takes several hours to complete, frequently results in
extensive blood loss, has a prolonged recovery period after surgery
and is unsuitable for elderly patients (12).
Posterior surgery has made significant progress in
the treatment of STB over the past few decades. The posterior
pedicle screw system has been widely used to improve spinal
stability and correct spinal deformities. It has been demonstrated
to be effective in treating disorders of the thoracic spine,
resulting in neurological dysfunction and segmental instability
(8).
Harms and Rolinger (13) first advocated for posterior TTIF,
which is regarded as an improvement on posterior thoracic interbody
fusion (PTIF) and was successful in resolving the issue of
excessive nerve retraction and its associated complications.
However, the multifidus muscle is extensively stripped during the
traditional TTIF procedure, which damages its blood supply and
innervation. As a result, the multifidus muscle degenerates,
atrophies and undergoes fibrosis and the deposition of adipose
tissue after surgery. Additionally, the procedure requires a long
time to complete. When surgeries are prolonged, the extensive
retraction of the paraspinal muscles, which are the innermost
multifidus muscle groups, raises intramuscular pressure. This
results in local hypoxia and sometimes irreversible ischemic
degeneration and necrosis, which frequently has a significant
impact on the physiological function of the multifidus muscle and
increases the risk of persistent lower back pain after surgery
(14). In 1968, Wiltse (5) proposed a novel strategy by utilizing
the space between the longissimus and multifidus muscles. The
integrity of the posterior bone and ligamentous structures is
maximized by this strategy, which can significantly reduce damage
to the multifidus muscle caused by dissection or traction.
In practice, the intermuscular TTIF approach is
rarely used to treat osteoporosis in elderly patients with STB.
However, the Wiltse TTIF method benefits from the following: It is
anatomically straightforward, easing the learning curve for novice
surgeons. Natural spaces between the multifidus and longissimus
muscles are used for access, instead of crude dissection and
extensive retraction of the paraspinal muscle complexes. This
prevents denervation and devascularization of the multifidus
muscle, which can lead to ischemic degeneration and necrosis. As a
result, it maintains the physiological functions of the multifidus
muscle while maintaining the stability of the spine. Therefore,
postoperative chronic lower back pain is less common but
postoperative recovery takes longer. According to the present
research, patients who underwent Wiltse TTIF spent an average of
6.80±1.51 days in the hospital. For thoracic TB treated using a
posterior-only approach, our previous study found that the mean
hospital stay was 12.4±4.1 days (15). This suggests that the Wiltse TTIF
approach effectively reduced hospital stay. Second, the Wiltse
intramuscular TTIF strategy shortens the duration of surgery and
anesthesia, which typically results in less blood loss during the
procedure and lower overall risks associated with the procedure.
Among the 20 patients in the present study, there were few cases
where the upper thoracic vertebrae were involved, and mainly the
middle and lower thoracic vertebrae were affected. It was necessary
to remove some rib bones to reach the intervertebral disc; however,
the bone was loose and not particularly hard. In addition, the use
of an ultrasonic osteotome simplified the surgical process. This
may be advantageous because the majority of elderly patients have
accompanying medical conditions and comorbidities, which could be
deemed fatal or cause the patient to be unsuitable for prolonged
surgical treatment. According to the findings of the present study,
the Wiltse TTIF approach took an average of 155.00±52.92 min to
perform on patients and resulted in a blood loss of 153.75±41.64 ml
on average. The surgery time for patients who underwent a
posterior-only approach was 152.1±24.4 min, and the amount of blood
lost was 650.7±150.2 ml (15).
Although the Wiltse TTIF approach is effective at reducing
intraoperative blood loss, it does not discernibly reduce the
duration of surgery. Third, it can achieve the same internal
fixation as obtained using PLIF, assisting in the stabilization of
the spinal column and preventing the worsening of kyphosis and the
neurological manifestations that accompany it. Finally, the
surgical area enables the removal of any paraspinal abscesses that
may be present, which is advantageous for the successful surgical
treatment of STB and its healing. The Wiltse TTIF method, by
contrast, has two major drawbacks. First, there is the possibility
of further injury to the spinal cord and nerve roots, similar to
that observed with PTIF spinal decompression. Second, complete
anterolateral debridement is challenging, but anti-TB drugs have
made it possible for TB lesions to spontaneously merge and heal;
therefore, thorough debridement is not essential (8).
The treatment plan for elderly patients with
osteoporosis and STB may be based on the findings of the present
study, with conservative treatment, such as bed rest, anti-TB
chemotherapy and anti-osteoporosis treatment being considered in
addition to regular MRI and blood sample reviews and evaluations
every 4-8 weeks. Second, after the adjacent vertebral segments
without tuberculous lesions have been cemented, cortical bone
trajectory (bicortical bone screw) or root screws can be used in
elderly patients with severe osteoporosis and aggravated
neurological symptoms. The fixed segment can be appropriately
extended if the fixation is loose or insecure. In elderly patients
with severe osteoporosis, the Wiltse approach can also aid in
maintaining adequate postoperative spinal stability by preserving
the spinous processes and associated attachments, including the
spinous process, interspinous ligament, lamina and other bony
structures. Lastly, TB genetic analysis, drug susceptibility
testing and drug resistance testing can be performed on
intraoperative specimens to guide the selection of postoperative
anti-TB medications.
In conclusion, the one-step Wiltse TTIF approach is
feasible and efficient for the treatment of elderly patients with
osteoporosis and SSTTB. The postoperative clinical and imaging
results in the present study are very promising; however, the
follow-up time was short. Further confirmation of the findings of
the study requires a larger number of patients and extended
follow-up period for this type of surgical procedure. New research
projects may also be performed to study the effect of this surgical
method on patients with other complications.
Acknowledgements
Not applicable.
Funding
Funding: This study was supported by the National Natural
Science Foundation of China (grant no. 82160420) and the Clinical
Climbing Program of the First Affiliated Hospital of Guangxi
Medical University (grant no. YYZS2020022).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
HZ designed and supervised the study. YL and SL
performed the data collection and analysis. AM and HQ assisted with
pathology and image preparation. HQ and GC prepared and revised the
manuscript. GC conducted data analysis and interpretation. All
authors read and approved the final manuscript. HZ and HQ confirm
the authenticity of all the raw data.
Ethics approval and consent to
participate
The study was approved by the Medical Ethics
Committee of the First Affiliated Hospital of Guangxi Medical
University (ref. no. KY-E-152).
Patient consent for publication
Informed written consent was obtained from all 20
patients for the publication of this case report and the
accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Zhao Y, Li M and Yuan S: Analysis of
transmission and control of tuberculosis in Mainland China,
2005-2016, based on the age-structure mathematical model. Int J
Environ Res Public Health. 14(1192)2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Cormican L, Hammal R, Messenger J and
Milburn HJ: Current difficulties in the diagnosis and management of
spinal tuberculosis. Postgrad Med J. 82:46–51. 2006.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Zeng H, Shen X, Luo C, Xu Z, Zhang Y, Liu
Z, Wang X and Cao Y: 360-degree cervical spinal arthrodesis for
treatment of pediatric cervical spinal tuberculosis with kyphosis.
BMC Musculoskelet Disord. 17(175)2016.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Wang LJ, Zhang HQ, Tang MX, Gao QL, Zhou
ZH and Yin XH: Comparison of three surgical approaches for thoracic
spinal tuberculosis in adult: Minimum 5-year follow up. Spine
(Phila Pa 1976). 42:808–817. 2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Wiltse LL: The paraspinal
sacrospinalis-splitting approach to the lumbar spine. Clin Orthop
Relat Res. (91):48–57. 1973.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Jin YM, Chen Q, Chen CY, Lyu J, Shi B,
Yang C and Xia C: Clinical research and technique note of TTIF by
wiltse approach for the treatment of degenerative lumbar. Orthop
Surg. 13:1628–1638. 2021.PubMed/NCBI View
Article : Google Scholar
|
|
7
|
Kan B, Zhao Q, Wang L, Xue S, Cai H and
Yang S: Association between lipid biomarkers and osteoporosis: A
cross-sectional study. BMC Musculoskelet Disord.
22(759)2021.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Zhang HQ, Lin MZ, Shen KY, Ge L, Li JS,
Tang MX, Wu JH and Liu JY: Surgical management for multilevel
noncontiguous thoracic spinal tuberculosis by single-stage
posterior transforaminal thoracic debridement, limited
decompression, interbody fusion, and posterior instrumentation
(modified TTIF). Arch Orthop Trauma Surg. 132:751–757.
2012.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Hayashi S, Takeuchi M, Hatsuda K, Ogata K,
Kurata M, Nakayama T, Ohishi Y and Nakamura H: The impact of
nutrition and glucose intolerance on the development of
tuberculosis in Japan. Int J Tuberc Lung Dis. 18:84–88.
2014.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Moon MS: Tuberculosis of the spine.
Controversies and a new challenge. Spine (Phila Pa 1976).
22:1791–1797. 1997.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Lu G, Wang B, Li J, Liu W and Cheng I:
Anterior debridement and reconstruction via thoracoscopy-assisted
mini-open approach for the treatment of thoracic spinal
tuberculosis: Minimum 5-year follow-up. Eur Spine J. 21:463–469.
2012.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Zhang HQ, Guo CF, Xiao XG, Long WR, Deng
ZS and Chen J: One-stage surgical management for multilevel
tuberculous spondylitis of the upper thoracic region by anterior
decompression, strut autografting, posterior instrumentation, and
fusion. J Spinal Disord Tech. 20:263–267. 2007.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Harms J and Rolinger H: A one-stager
procedure in operative treatment of spondylolistheses: Dorsal
traction-reposition and anterior fusion (author's transl). Z Orthop
Ihre Grenzgeb. 120:343–347. 1982.PubMed/NCBI View Article : Google Scholar : (In German).
|
|
14
|
Kawaguchi Y, Yabuki S, Styf J, Olmarker K,
Rydevik B, Matsui H and Tsuji H: Back muscle injury after posterior
lumbar spine surgery. Topographic evaluation of intramuscular
pressure and blood flow in the porcine back muscle during surgery.
Spine (Phila Pa 1976). 21:2683–2688. 1996.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Zeng H, Zhang P, Shen X, Luo C, Xu Z,
Zhang Y, Liu Z and Wang X: One-stage posterior-only approach in
surgical treatment of single-segment thoracic spinal tuberculosis
with neurological deficits in adults: A retrospective study of 34
cases. BMC Musculoskelet Disord. 16(186)2015.PubMed/NCBI View Article : Google Scholar
|