Introduction
Triangular fibrocartilage complex (TFCC) tears are a
common cause of ulnar-sided wrist pain and usually affect the grip
strength and wrist range of motion (1-3).
TFCC injuries were noted to increase with age, with a 49%
prevalence among patients aged ≥70 and a 27% prevalence among those
aged ≤30(4). TFCC also plays an
important role in the stability of the distal radioulnar joint
(DRUJ) by its foveal attachment (1,2). The
DRUJ joint consists of six primary components, which are the dorsal
and volar radioulnar ligaments, central articular disc, meniscus
homologue, ulnar collateral ligament, extensor carpi ulnaris (ECU)
sub-sheath and the origin of ulnolunate and ulnotriquetrial
ligaments (2). The radioulnar
ligaments are separated into the deep fibres, known as the
ligamentum subcruentum, which are attached to the ulnar fovea
(5), while superficial fibres are
attached to the ulnar styloid.
The peripheral part of the TFCC is well
vascularised, while the central portion is avascular (6). Lesions of the TFCC are classified
according to the Palmer classification as either traumatic (type I)
or degenerative (type II) depending on the cause of injury.
Depending on the location of the tear within the TFCC, type 1 is
further classified into 1A isolated central tears, 1B tears located
on the ulnar side of the TFCC, also called ulnar avulsion of the
TFCC, 1C tears on the distal tear of the TFCC (the origin of the
ulnolunate and ulnotriquetrial ligaments) and 1D radial avulsion
(6,7). A traumatic tear of the ulnar side of
the TFCC (type IB) is one of the most common causes of ulnar-sided
discomfort and impairment in the wrist (7-9).
Ultrasound imaging is a non-invasive method that
uses high-frequency sound waves to generate real-time images of
internal structures, enabling detection of translational movement
in the DRUJ without radiation or contrast agents (10). It allows for visualizing joint
motion during active exercise, facilitating the early
identification of DRUJ instability and the development of improved
treatment approaches (3,11).
Grayscale ultrasound imaging faces challenges due to
TFCC varied echogenicity, making it difficult to distinguish injury
from normal tissue. The central disk of the TFCC lacks blood
supply, while the periphery receives blood from nearby vessels
(2). Doppler signals are typically
absent, but in certain cases, small vessels along the ulnocarpal
ligament may be observable. The increased vascularity at the deep
border of the ulnocarpal ligament and the outer margin of the TFCC,
along with other indications such as joint widening and visible
gaps, aid in diagnosing TFCC injury (3). Power Doppler, a specialized
ultrasound technique that detects blood flow, along with dynamic
imaging during functional tasks, enhances the diagnostic accuracy
of TFCC injury (11).
For diagnosing tears in the TFCC, arthroscopy has
been considered the gold standard. However, arthroscopy and
magnetic resonance (MR) arthrography, despite their efficacy,
present certain drawbacks, such as invasiveness, prolonged
procedural durations, high cost and being operator dependent
(8,12-14).
By contrast, high-resolution conventional MRI offers a valuable
non-invasive alternative for diagnosing TFCC tears. This imaging
modality provides an accurate imaging protocol that detects the
location and extent of injury without invasive procedures. Studies
have demonstrated the efficacy of high-resolution conventional MRI
in visualizing most surgically relevant TFCC pathology, making it a
reliable diagnostic tool (2,12).
Ultrasound and high-resolution MRI offer
non-invasive, accurate imaging for detecting DRUJ instability and
diagnosing TFCC tears. These advancements improve diagnostics and
may lead to more effective treatment options for DRUJ and TFCC
injury (3,6).
Ulnar-sided wrist pain caused by TFCC injury is
treated initially using non-operative methods, including
immobilization, physiotherapy, cortisone injection (15,16).
Surgery is considered once non-operative treatment has failed.
Surgical interventions include arthroscopic debridement and
arthroscopic-assisted (outside-in, inside-out, all-inside) or open
repair. Ulnar shortening osteotomy is used to decrease the load on
the ulnocarpal joint, in the case of ulna abutment association from
ulna positive variance (1,17).
Treatment is chosen depending on the location of the
tear (15,18). Tears in the peripheral superficial
parts of the TFCC are sutured to the dorsal ulnocarpal capsule and
the ECU sub-sheath (18). TFCC
tears in the deep part, which is the main stabilizer of the DRUJ,
or any injury to its foveal insertion can cause instability
(19). Foveal avulsions are
considered as atypical variation on type 1B TFCC tear (20) and are usually treated by
reattaching the avulsed TFCC region either by trans-osseous sutures
or suture anchors, which can be performed by either open or
arthroscopically assisted repair (18,20).
To the best of our knowledge, however, functional outcomes are
comparable and there is no clear evidence regarding which technique
gives better results (15).
The present retrospective study aimed to compare
functional and clinical outcomes between open TFCC repair using
micro suture anchors and using trans-osseous sutures.
Materials and methods
Study overview and patient
selection
The present retrospective comparative study aimed to
evaluate the clinical and functional outcomes of open TFCC repair
using micro suture anchors and trans-osseous sutures. The study
included 51 patients who underwent open surgical repair between
July 2017 and March 2021 performed by hand and upper limb surgeons
at the Royal Rehabilitation Centre, King Hussein Medical Centre
(Amman, Jordan). A total of 38 patients (27 males and 11 females)
underwent open repair using micro suture anchors, while 13 (7 males
and 6 females) underwent trans-osseous repair.
Assessment and data collection
The present study included patients with a specific
tear pattern involving the Palmer portion of the TFCC, known as
TFCC tear Palmer type 1B. These tears are typically caused by
trauma or injury. The patient population consisted of individuals
between the ages of 18 and 55 years to ensure a consistent and
comparable group for analysis, taking into account potential
age-related factors such as bone density, vascularization,
comorbidities, muscle mass and strength, that could affect the
outcomes of TFCC repair. The minimum follow-up time for patients
was 6 months, with a mean follow-up period of 27 months. This
duration allowed comprehensive evaluation of long-term outcomes and
the assessment of the stability and effectiveness of the surgical
technique. Patients with arthritic changes in DRUJ or ulnocarpal
abutment, as well as those with wrist pathology in the
contralateral side, were excluded to maintain a homogeneous patient
population without confounding factors that could influence the
outcome.
Grip strength assessment was performed using
dynamometer. Immediate preoperative assessments were conducted,
followed by evaluations at 2 weeks, and subsequently at 6, 12 and
annually thereafter, compared with the contralateral side. Wrist
range of motion and presence or absence of pain and local
tenderness were recorded. Modified Mayo Wrist Score (MMWS) was
performed pre- and post-operatively, as was the Disability of the
Arm, Shoulder and Hand (DASH) score (1,21-23).
Pre-operative wrist MRI was used for diagnostic purposes.
Surgical procedure
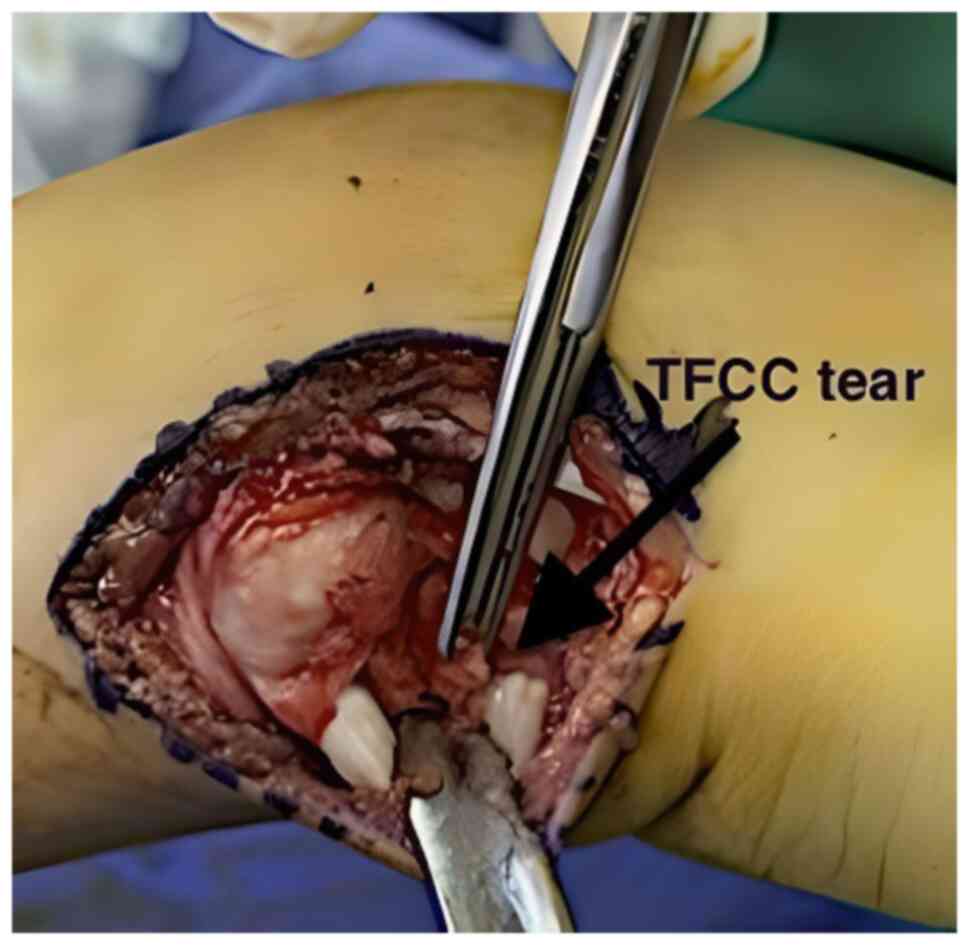
Both surgical techniques utilized a longitudinal
skin incision at the dorsal aspect of the wrist between the fifth
(extensor digiti minimi) and sixth extensor compartments (extensor
carpi ulnaris; Fig. 1). The fifth
extensor compartment was opened, and the extensor digiti minimi
tendon was retracted to ensure adequate exposure of the surgical
field. Moving proximally, the sub sheath of the extensor carpi
ulnaris was opened and retracted in an ulnar direction. This step
facilitated clear visualization of the underlying structures and
allowed further exploration and manipulation of the target area.
Then, an L-shaped capsulotomy was performed, extending
longitudinally along the margin of the sigmoid notch and angled
towards the ulna, proximal to the dorsal radioulnar ligament of the
TFCC. A second capsulotomy was performed transversely along the
distal edge of the dorsal radioulnar ligament to expose the distal
surface of the TFCC (Fig. 2). The
implementation of these capsulotomies in a standardized manner
ensured consistent and controlled access to targeted structures,
allowing for a thorough evaluation and appropriate management of
the TFCC during the repair process.
Trans-osseous group
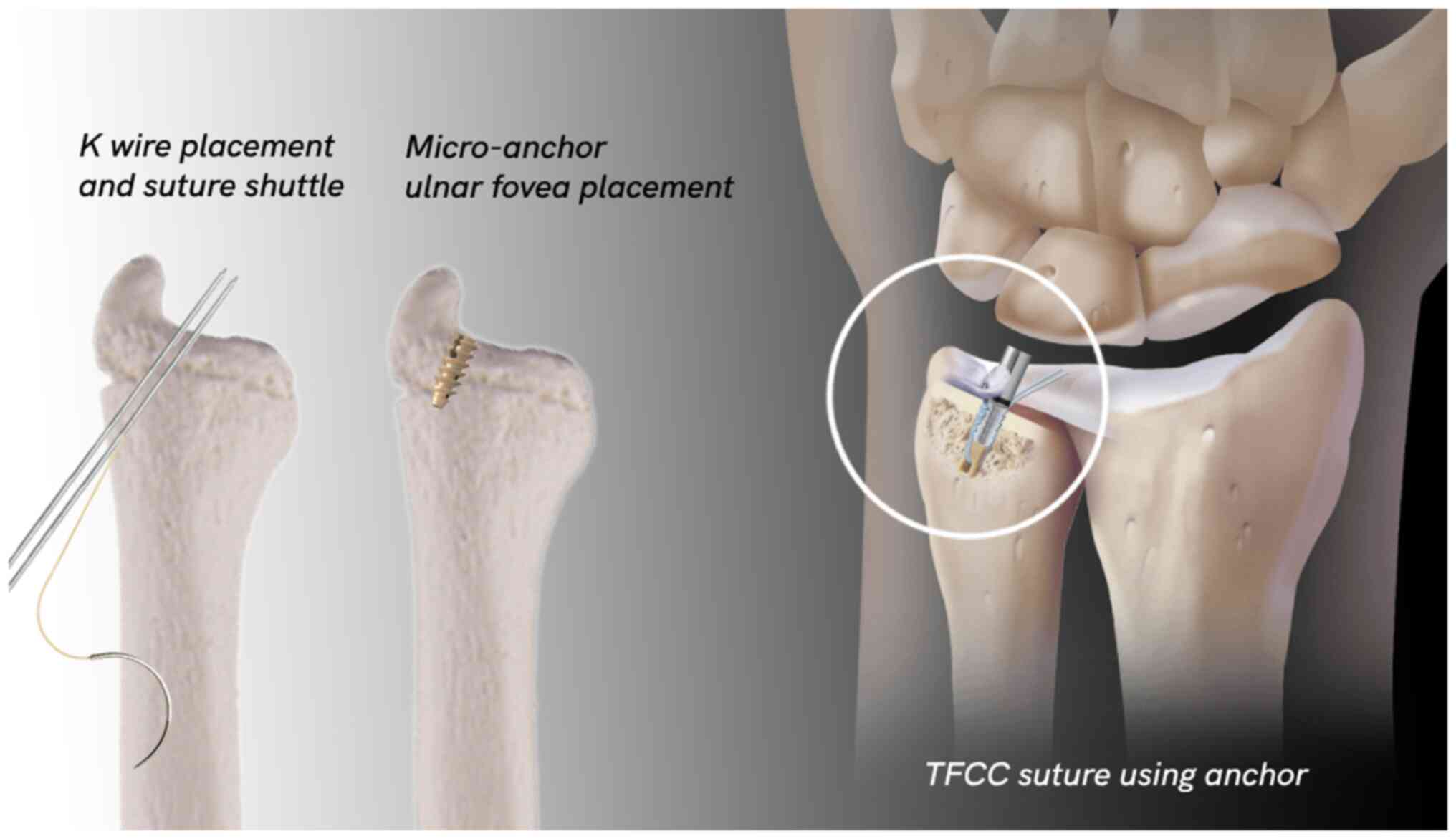
In the trans-osseous suture technique, 0.062-inch
K-wire was used to create two holes in the distal ulna. These holes
were carefully positioned, passing from the dorsal aspect of the
ulnar neck to the ulnar fovea. Subsequently, two horizontal
mattress 2-0 sutures were passed distally to proximally through the
periphery of the TFCC and the K-wire holes (Fig. 3). This configuration ensured secure
attachment and stabilization of the TFCC. Sutures were tied over
the ulnar neck with the DRUJ joint reduced before suturing the
TFCC, and the forearm positioned in neutral rotation. To reinforce
the repair, the dorsal DRUJ capsule, and retinaculum were closed
together, while ensuring that the extensor digiti minimi tendon was
superficial to the retinaculum. The closure was not excessively
imbricated to avoid potential loss of pronation.
Suture anchor group
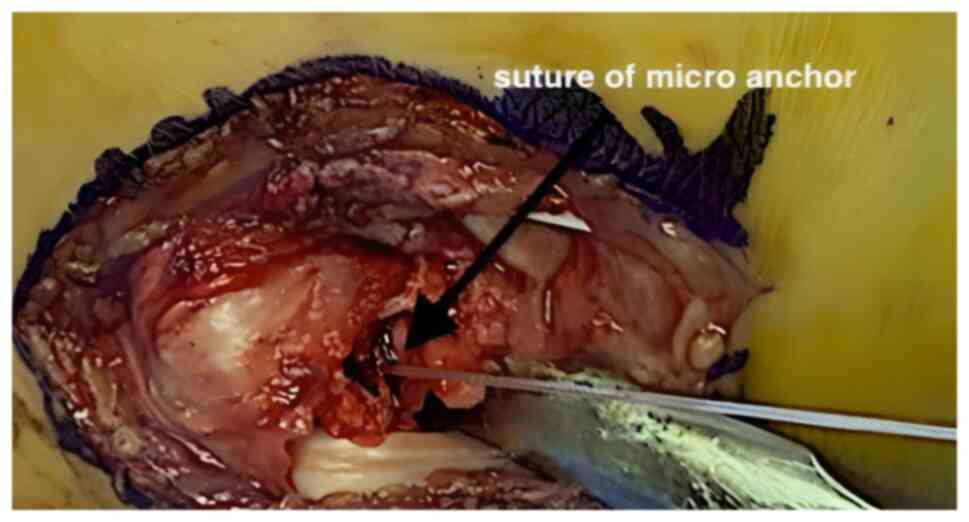
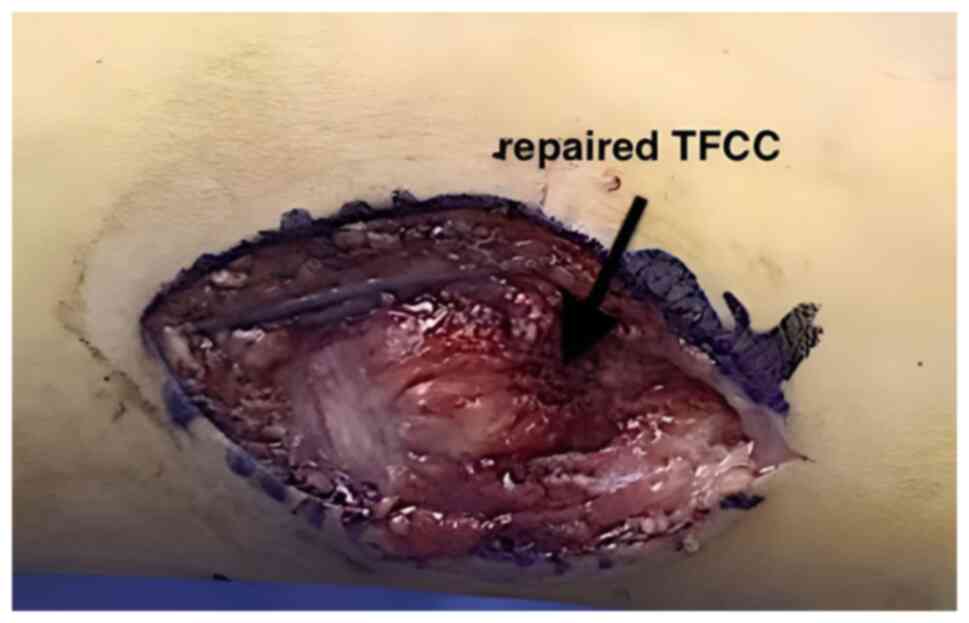
In the suture anchor technique, the micro suture
anchor was carefully positioned and inserted at the ulnar fovea
(Fig. 4), a key anatomical
landmark within the wrist joint (2). This small but robust anchor serves as
a stable point of attachment for the repair process (Fig. 3). Subsequently, two horizontal
mattress sutures, using high-quality suturing material, were passed
through the periphery of the TFCC, ensuring secure and reliable
fixation. These sutures reattached the TFCC firmly to the ulnar
fovea (Fig. 5), re-establishing
its proper anatomical position and restoring its key role in wrist
stability and function.
Following the surgical procedure, a long arm splint
was applied to the forearm, with the forearm rotated 45˚ towards
the most stable joint position, which was often in supination. This
splint was maintained for 2 weeks. At this point, the splint was
converted to a sugar tongue splint, worn for an additional 4 weeks.
Finally, a removable splint was utilized for the subsequent 4 weeks
to regain motion and facilitate the healing process.
Statistical analysis
Data were analysed using SPSS (version 27;
https://www.ibm.com/products/spss-statistics). A
paired t-test was applied to assess paired data, comparing the pre-
and post-operative outcomes within each surgical technique group.
P<0.05 was considered to indicate a statistically significant
difference. Data were presented as mean ± SD.
Results
Functional assessment and comparison
of surgical techniques
All patients who underwent open TFCC repair either
by trans-osseous or micro anchor suture underwent a periodic
thorough assessment and evaluation of degree of pain, wrist range
of motion and grip strength using a dynamometer, with assessment of
both DASH and MMWS, to compare the pre- and post-operative
functional status for both surgical techniques.
Range of motion enhancement
Significant improvements in range of motion were
observed in both the trans-osseous suture and the suture anchor
technique for patients undergoing open TFCC repair. In the
trans-osseous suture group, patients experienced significant gains
in range of movement, with mean flexion increasing from 37 to 46˚,
extension from 39 to 51˚, radial deviation from 8 to 13˚ and ulnar
deviation from 18 to 26˚ (Table
I). Similarly, in the suture anchor group, patients exhibited
significant enhancements in the range of movement. Mean flexion
increased from 39 to 51˚, extension from 41 to 56˚, radial
deviation from 10 to 14˚ and ulnar deviation from 21 to 32˚
(Table II). These findings
suggest that both the trans-osseous suture and the suture anchor
technique were highly effective in improving wrist range of motion.
The substantial improvements observed in flexion, extension, radial
deviation and ulnar deviation demonstrate the positive impact of
these surgical techniques on enhancing range of movement in
patients undergoing open TFCC repair (Tables I and II).
 | Table IMean wrist ROM improvement using the
trans-osseous suture technique (compared with the contralateral
side). |
Table I
Mean wrist ROM improvement using the
trans-osseous suture technique (compared with the contralateral
side).
| Movement | Pre-operative ROM,
˚ | Post-operative ROM,
˚ | Improvement, ˚ | P-value |
|---|
| Flexion | 36.9±5.6 | 46.2±4.5 | 9 | <0.001 |
| Extension | 38.9±4.5 | 51.2±6.0 | 12 | <0.001 |
| Radial deviation | 7.9±2.1 | 13.2±2.5 | 5 | 0.016 |
| Ulnar
deviation | 18.1±4.5 | 26.3±4.0 | 8 | <0.001 |
 | Table IIMean wrist ROM improvement using
micro anchor suture technique (compared with the contralateral
side). |
Table II
Mean wrist ROM improvement using
micro anchor suture technique (compared with the contralateral
side).
| Movement | Pre-operative ROM,
˚ | Post-operative ROM,
˚ | Improvement, ˚ | P-value |
|---|
| Flexion | 39.1±5.9 | 51.0±4.5 | 12 | <0.001 |
| Extension | 41.0±7.5 | 56.0±3.9 | 15 | <0.001 |
| Radial
deviation | 10.0±2.0 | 14.1±2.0 | 4 | 0.016 |
| Ulnar
deviation | 20.9±5.5 | 31.9±1.6 | 11 | <0.001 |
Pain improvement
Significant improvements in pain were observed in
both surgical techniques, as indicated by the MMWS and DASH score.
In the trans-osseous suture group, the pain score showed a marked
improvement after 6 months, increasing from 65% pre-operatively to
85% post-operatively, demonstrating a significant enhancement in
pain relief. Similarly, in the suture anchor group, the pain score
improved significantly from 70% pre-operatively to 90%
post-operatively, indicating a significant increase in pain relief
(Table III).
 | Table IIIPain improvement according to MMWS
and DASH score. |
Table III
Pain improvement according to MMWS
and DASH score.
| Pain
assessment | Trans-osseous
suture | Micro anchor |
|---|
| Pre-operative pain
MMWS score, % | 65 | 70 |
| Post-operative pain
MMWS score, % | 85 | 90 |
| MMWS pain
improvement, % (P-value <0.001) | 20 | 20 |
| DASH pain
improvement, % (P-value <0.001) | 45 | 55 |
| Pain-free range of
movement, % | 90 | 97 |
DASH score was used to assess the improvement in
pain. The results revealed a substantial improvement in pain from
the preoperative to postoperative period. Specifically, the pain
decreased significantly from 60 to 15% in the trans-osseous suture
group and from 70 to 15% in the suture anchor group. In the micro
suture anchor technique, all patients achieved a pain-free state
after a mean follow-up of 7 months, indicating a substantial
improvement in pain intensity. However, one patient showed pain
improvement from 0 points preoperatively to 15 points
postoperatively according to the MMWS (Table III).
Similarly, in the trans-osseous technique, nearly
all patients were pain-free after a mean follow-up of 9 months.
Only one patient experienced improvement in pain intensity over a
longer post-operative period, showing pain improvement from 5
points preoperatively to 20 points postoperatively according to the
MMWS. Overall, the MMWS and DASH scores provide strong evidence of
significant improvements in pain following surgery in both the
trans-osseous suture and the suture anchor group (Table IV).
 | Table IVMMWS and DASH score improvement. |
Table IV
MMWS and DASH score improvement.
| Score | Trans-osseous
(%) | Micro anchor
(%) | P-value |
|---|
| MMWS | 85 | 90 | <0.05 |
| DASH | 15 | 15 | >0.05 |
Grip strength enhancement
Grip strength, measured using a dynamometer and
compared with the contralateral healthy side, showed significant
improvements in patients undergoing open TFCC repair using
trans-osseous sutures. The mean grip strength increased from 60%
preoperatively to 90% postoperatively according to the MMWS,
indicating 50% improvement in grip strength following the
trans-osseous suture technique (Table
V).
 | Table VGrip strength assessment. |
Table V
Grip strength assessment.
| Surgical
technique | Pre-operative grip
strength, % | Post-operative grip
strength, % | Grip strength
improvement, % | P-value |
|---|
| Trans-osseous
suture | 60 | 90 | 50 | <0.001 |
| Micro anchor | 65 | 90 | 38 | 0.01 |
In patients undergoing open TFCC repair using suture
anchors, there was an improvement in grip strength postoperatively.
The mean grip strength increased from 65% preoperatively to 90%
postoperatively according to the MMWS, demonstrating a significant
38% improvement in grip strength following the suture anchor
technique. These findings highlight the effectiveness of both
surgical techniques in enhancing grip strength in patients
undergoing open TFCC repair (Table
V).
Discussion
The present study aimed to compare the clinical and
functional outcomes of open TFCC repair using trans-osseous suture
and micro anchor suture technique.
Foveal disruption of TFCC is a common condition
associated with DRUJ instability. TFCC tears significantly impact
wrist function and lead to persistent pain and instability.
Conservative treatment is the primary approach for managing all
types of TFCC injury. This treatment modality aims to alleviate
symptoms and provides provide symptomatic relief in ~33% of
patients (1). While non-surgical
treatments are successful for TFCC tears without DRUJ instability,
surgical intervention is necessary in cases where conservative
measures fail to provide relief (16,24).
If the TFCC is avulsed from the foveal insertion, a reattachment
procedure to re-fix the foveal insertion of radio-ulnar ligaments
to the bone is the treatment of choice to restore DRUJ stability
and function (1).
Surgical repair techniques have predominantly
focused on addressing type 1B tears in TFCC (1). Both open (which have been
successfully utilized for decades) (1), and arthroscopic repair (recognized
for their reliability and effectiveness) (15), have shown comparable results in
terms of DRUJ instability for TFCC tears (15,25,26).
Moreover, these techniques have demonstrated efficacy in relieving
ulnar-sided wrist pain commonly associated with TFCC tears
(26). Anderson et al
(21) compared open and
arthroscopic repair techniques in 76 patients with TFCC tears. The
findings indicated no significant differences in clinical outcomes,
including grip strength, range of motion, visual analogue scale,
DASH and Patient Reported Wrist Evaluation scores and only a minor
decrease in wrist flexion-extension in the open repair group.
However, both groups experienced recurrent DRUJ instability
necessitating re-intervention, indicating the need for improved
primary treatment strategies (21). Furthermore, no notable disparities
were observed in postoperative range of motion, grip strength or
functional outcome scores between the two techniques, highlighting
the lack of evidence to recommend one approach over the other in
clinical practice (15).
Conversely, arthroscopic treatment for peripheral tears
consistently yields positive outcomes, with various studies
reporting success rates ranging from 60 to 90% (1,21).
Previous studies have conducted retrospective
evaluations of outcome measures to assess the effectiveness of
treatment: These measures typically include parameters such as
pain, DRUJ instability, range of motion, grip strength, MMWS and
DASH score (1,21-23).
The assessment of grip strength is widely used to
evaluate the functional status and clinical outcomes of the upper
extremity after trauma or surgery (1,21,25,27).
It serves as a valuable measure to determine the recovery progress
and set realistic expectations for patients during preoperative
consultation (22). In the present
study, there was significant improvement in grip strength
post-operatively for both trans-osseous and the micro anchors
suture techniques. The improvement in grip strength was 90% for
both techniques, consistent with another study supporting the
positive impact of these surgical techniques on grip strength
(10,27). Furthermore, the trans-osseous
suture group showed mean improvement in grip strength of 30
percentage points, while the suture anchor group showed mean
improvement of 25 percentage points. Although the difference
between the groups was not statistically significant, it suggests a
slightly greater improvement in grip strength in the trans-osseous
suture group. These results highlight the effectiveness of both
techniques in enhancing grip strength, with the trans-osseous
suture technique potentially yielding a slightly greater
improvement.
The limitation of wrist range of motion can greatly
impact daily activities and functional ability. Therefore,
improvements in wrist range of motion following treatment indicates
a successful intervention and enhanced wrist function (22). Here, the use of the micro anchors
suture technique resulted in a 90% improvement, while the
trans-osseous suture technique showed an 80% improvement. Notably,
97% of patients who underwent open TFCC repair using the micro
anchors suture technique achieved pain-free range of motion,
compared with 90% in the trans-osseous suture group, consistent
with previous research demonstrating pain improvement following
surgery (25,27).
Additionally, in the trans-osseous suture group,
there was a mean increase of ~41.5˚ in flexion, ~45.0˚ in
extension, ~10.5˚ in radial deviation and ~22.0˚ in ulnar
deviation. Similarly, the suture anchor group showed significant
improvements in range of motion, with a mean increase of ~45.0˚ in
flexion, ~48.5˚ in extension, ~12.0˚ in radial deviation and ~26.5˚
in ulnar deviation. These results highlight the positive impact of
both techniques on wrist range of motion, with the suture anchor
technique potentially leading to slightly greater improvements.
Both MMWS and DASH scores have been widely utilized
to assess the effectiveness of surgical treatments for similar
conditions such as foveal tears and DRUJ instabilities (21,23).
For the MMWS, there was a 90% improvement in patients who underwent
open TFCC repair using the micro anchors suture technique, while
those who underwent the trans-osseous suture technique exhibited an
85% improvement, consistent with previous studies that reported
similar improvements in the MMWS following open repair (21,27).
Regarding the DASH score, both techniques demonstrated a 15%
improvement. Both the trans-osseous and micro anchors suture
techniques were viable options for open TFCC repair, yielding
favourable clinical and functional outcomes. However, there were
slightly better results with the suture anchor technique regarding
pain relief, wrist range of motion and MMWS.
Both techniques showed significant improvement in
grip strength. The trans-osseous suture technique exhibited
slightly better outcomes, as evidenced by a greater percentage
point improvement. This suggests that the trans-osseous suture
technique may offer a slight advantage in terms of grip strength
recovery.
In terms of wrist range of motion, both techniques
yielded satisfactory results. However, the micro anchor technique
showed better outcomes in terms of pain relief, wrist range of
motion, and improvement in MMWS. Although the differences between
the two techniques were not significant, indicating comparable
clinical outcomes, the micro anchor technique demonstrated slightly
better results.
MMWS and DASH score provide a comprehensive
assessment of wrist function, pain and patient satisfaction. The
improvements in these scores suggest successful intervention and
enhanced wrist function following open TFCC repair using either
technique.
The contralateral side of all patients demonstrated
normal measurements and values for all the criteria assessed,
including grip strength within the normal range. This fact is
attributed to the rigorous patient selection process, which
excluded individuals with pathological conditions in the
contralateral wrists. By ensuring the normalcy of the contralateral
side, it served as a reliable baseline for comparing and evaluating
the functional outcomes of the post-operative results. The presence
of normal mean grip strength on the contralateral side further
underscores the significance of the observed improvements in grip
strength following open TFCC repair using both the trans-osseous
suture technique and the micro suture anchors suture technique.
The present study supported the effectiveness of
open TFCC repair using both the micro anchor and trans-osseous
suture techniques in managing pain, improving grip strength and
enhancing wrist range of motion. The micro anchor technique
demonstrated a higher success rate, with all patients experiencing
pain relief. However, it is important to acknowledge the
limitations of the study, such as the small sample size, and
further research with larger cohorts and robust methodologies is
necessary to validate these results and determine the optimal
surgical approach for pain management in TFCC repair.
To summarize, the present study highlighted the
positive impact of both the micro anchor and trans-osseous suture
techniques in open TFCC repair. While the micro anchor technique
showed a higher success rate in pain relief, further research is
needed to validate these findings in larger cohorts. Both
techniques effectively improved grip strength and wrist range of
motion, with the trans-osseous suture technique potentially
offering a slight advantage in grip strength recovery. These
results support surgical interventions for TFCC injuries and
underscore the importance of future research to optimize surgical
decision-making and functional outcomes in TFCC repair.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YK and SM performed surgery, designed the study and
revised the manuscript. AM designed the study and revised the
manuscript. EA and MQ performed surgery, analyzed data and wrote
the manuscript. DA performed the literature search, designed the
study, analyzed and interpreted data and wrote the manuscript. AO
performed the literature review, analyzed and interpreted data and
revised the manuscript. YK and SM confirm the authenticity of all
the raw data. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
The present study was approved by Royal Medical
Services, Jordan Ethical Committee, Amman, Jordan (approval no.
27). Written and oral consent to participate was obtained from all
participants.
Patient consent for publication
Written and oral consent for publication of data and
images was obtained from all participants.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Jawed A, Ansari MT and Gupta V: TFCC
injuries: How we treat? J Clin Orthop Trauma. 11:570–579.
2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Haugstvedt JR, Langer MF and Berger RA:
Distal radioulnar joint: Functional anatomy, including
pathomechanics. J Hand Surg Eur Vol. 42:338–345. 2017.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Wu WT, Chang KV, Mezian K, Naňka O, Yang
YC, Hsu YC, Hsu PC and Özçakar L: Ulnar Wrist Pain Revisited:
Ultrasound diagnosis and guided injection for triangular
fibrocartilage complex injuries. J Clin Med. 8(1540)2019.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Chan JJ, Teunis T and Ring D: Prevalence
of triangular fibrocartilage complex abnormalities regardless of
symptoms rise with age: Systematic review and pooled analysis. Clin
Orthop Relat Res. 472:3987–3994. 2014.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Spies CK, Müller LP, Oppermann J, Hahn P
and Unglaub F: Instability of the distal radioulnar joint-an
overview of clinical and radiological procedures regarding their
efficacies. Handchir Mikrochir Plast Chir. 46:137–150.
2014.PubMed/NCBI View Article : Google Scholar : (In German).
|
|
6
|
Ng AWH, Griffith JF, Fung CSY, Lee RKL,
Tong CSL, Wong CWY, Tse WL and Ho PC: MR imaging of the traumatic
triangular fibrocartilaginous complex tear. Quant Imaging Med Surg.
7:443–460. 2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Atzei A, Luchetti R and Garagnani L:
Classification of ulnar triangular fibrocartilage complex tears. A
treatment algorithm for Palmer type IB tears. J Hand Surg Eur Vol.
42:405–414. 2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Zhan H, Bai R, Qian Z, Yang Y, Zhang H and
Yin Y: Traumatic injury of the triangular fibrocartilage complex
(TFCC)-a refinement to the Palmer classification by using
high-resolution 3-T MRI. Skeletal Radiol. 49:1567–1579.
2020.PubMed/NCBI View Article : Google Scholar
|
|
9
|
McNamara CT, Colakoglu S and Iorio ML: A
systematic review and analysis of palmer type I triangular
fibrocartilage complex injuries: Outcomes of treatment. J Hand
Microsurg. 12:116–122. 2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Jung HS, Kim SH, Jung CW, Woo SJ, Kim JP
and Lee JS: Arthroscopic transosseous repair of foveal tears of the
triangular fibrocartilage complex: A systematic review of clinical
outcomes. Arthroscopy. 37:1641–1650. 2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Hung CY, Chang KV and Özçakar L: Dynamic
and doppler ultrasound imaging for the diagnosis of triangular
fibrocartilage complex injury and ulnocarpal wrist instability. Am
J Phys Med Rehabil. 95:e111–e112. 2016.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Casadei K and Kiel J: Triangular
Fibrocartilage Complex. In: StatPearls (Internet). StatPearls
Publishing, Treasure Island, FL, 2022.
|
|
13
|
Boer BC, Vestering M, van Raak SM, van
Kooten EO, Huis In ‘t Veld R and Vochteloo AJH: MR arthrography is
slightly more accurate than conventional MRI in detecting TFCC
lesions of the wrist. Eur J Orthop Surg Traumatol. 28:1549–1553.
2018.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Cody ME, Nakamura DT, Small KM and
Yoshioka H: MR Imaging of the triangular fibrocartilage complex.
Magn Reson Imaging Clin N Am. 23:393–403. 2015.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Andersson JK, Åhlén M and Andernord D:
Open versus arthroscopic repair of the triangular fibrocartilage
complex: A systematic review. J Exp Orthop. 5(6)2018.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Lee JK, Hwang JY, Lee SY and Kwon BC: What
is the natural history of the triangular fibrocartilage complex
tear without distal radioulnar joint instability? Clin Orthop Relat
Res. 477:442–449. 2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Saito T, Sterbenz JM and Chung KC:
Chronologic and geographic trends of triangular fibrocartilage
complex repair. Hand Clin. 33:593–605. 2017.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Liu EH, Suen K, Tham SK and Ek ET:
Surgical repair of triangular fibrocartilage complex tears: A
systematic review. J Wrist Surg. 10:70–83. 2021.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Matsumoto T, Tang P, Fujio K, Strauch RJ
and Rosenwasser MP: The optimal suture placement and bone tunnels
for TFCC repair: A cadaveric study. J Wrist Surg. 7:375–381.
2018.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Kim B, Yoon HK, Nho JH, Park KH, Park SY,
Yoon JH and Song HS: Arthroscopically assisted reconstruction of
triangular fibrocartilage complex foveal avulsion in the ulnar
variance-positive patient. Arthroscopy. 29:1762–1728.
2013.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Anderson ML, Larson AN, Moran SL, Cooney
WP, Amrami KK and Berger RA: Clinical comparison of arthroscopic
versus open repair of triangular fibrocartilage complex tears. J
Hand Surg Am. 33:675–682. 2008.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Lee SH and Gong HS: Grip strength
measurement for outcome assessment in common hand surgeries. Clin
Orthop Surg. 14:1–12. 2022.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Atzei A, Luchetti R and Braidotti F:
Arthroscopic foveal repair of the triangular fibrocartilage
complex. J Wrist Surg. 4:22–30. 2015.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Im J, Kang SJ and Lee SJ: A comparative
study between conservative and surgical treatments of triangular
fibrocartilage complex injury of the wrist with distal radius
fractures. Clin Orthop Surg. 13:105–109. 2021.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Feitz R, van der Oest MJW, van der Heijden
EPA, Slijper HP, Selles RW and Hovius SER: Hand-Wrist Study Group.
Patient-reported outcomes and function after reinsertion of the
triangular fibrocartilage complex by open surgery. Bone Joint J.
103-B:711–717. 2021.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Luchetti R, Atzei A, Cozzolino R, Fairplay
T and Badur N: Comparison between open and arthroscopic-assisted
foveal triangular fibrocartilage complex repair for post-traumatic
distal radio-ulnar joint instability. J Hand Surg Eur Vol.
39:845–855. 2014.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Moritomo H: Open repair of the triangular
fibrocartilage complex from palmar aspect. J Wrist Surg. 4:2–8.
2015.PubMed/NCBI View Article : Google Scholar
|