Introduction
Uterine devascularization methods, including
bilateral ligation of hypogastric (internal iliac) arteries,
uterine devascularization procedures, and radiological arterial
embolization (1-4),
have long been practiced as effective management in obstetric
emergencies caused by excessive bleeding. As a quick and simple
surgical devascularization procedure, bilateral uterine artery
ligation (BUAL) can decrease the blood supply to the uterus and
effectively reduce intraoperative blood loss, and reduce the
incidence of postpartum hemorrhage (PPH) and the urgent
hysterectomy rate (5). However,
some obstetricians hold the view that the adverse effects of this
invasive procedure on patients' subsequent fertility and
obstetrical outcomes should be considered (6-8).
It has been suggested that infertility, intrauterine synechia,
placenta accreta, and certain adverse pregnancy outcomes are
associated with uterine devascularization, and therefore this
procedure should be performed taking these possibilities into
consideration.
Concerns regarding the impact following uterine
devascularization have led some investigators to conduct relevant
studies. Reports indicate that uterine devascularization does not
appear to adversely affect the menstrual and fertility outcomes of
the majority of women, but their sample sizes are small (9-11).
Conversely, there are also studies on uterine artery Doppler scans
revealing that the recanalization rate and isolated uterine blood
supply are low following BUAL (12,13),
and assessment for intrauterine fetal growth restriction in the
next pregnancy is recommended.
To date, to the best of our knowledge, no studies
have reported the fetal growth index in the subsequent pregnancy
and discussed whether intrauterine growth restriction (IUGR) is
related to BUAL. Therefore, the aim of the current case series was
to describe the fetal growth index and obstetrical outcomes during
the subsequent pregnancy of women who had undergone BUAL due to
obstetric emergencies in a single center over a 9-year period.
Patients and methods
The present study was approved by the Institutional
Board Review of Xiamen Women and Children's Hospital. A total of 12
cases were identified retrospectively from the clinical database of
Xiamen Women and Children's Hospital. This database is an
electronic record of all patients admitted to the Xiamen Women and
Children's Hospital since 2011. This database was queried to obtain
a list of all patients who had at least two hospital deliveries
from October 2011 to December 2020. Women who underwent BUAL during
cesarean section and had another delivery later were included.
Patients whose pregnancies did not continue beyond 20 weeks of
gestation were excluded, as delivery records were built in the
database only when the gestational age at delivery was ≥20
weeks.
The clinical characteristics of the 12 patients who
had undergone BUAL during cesarean delivery in a previous pregnancy
are described in Table I. BUAL was
performed in all patients for PPH. In all patients, the principal
contributor to hemorrhage was durative intrauterine bleeding and
uterine atony, which did not respond to oxytocic drugs. All the
patients required blood transfusions. No maternal deaths were
recorded, and no surgical complications arose during the BUAL.
 | Table IClinical characteristics of the
patients who underwent bilateral uterine artery ligation. |
Table I
Clinical characteristics of the
patients who underwent bilateral uterine artery ligation.
| Case | Age, years | Parity | Reason for
cesarean | Indication for
BUAL | Other surgical
management | Term of delivery,
weeks | Fetal birth weight,
g | Maternal and neonatal
outcome |
|---|
| 1 | 24 | 0 | Failed induction of
labor | Durative intrauterine
bleeding | Bakri Postpartum
Balloon | 41 | 3,870 | PPH |
| 2 | 21 | 0 | Central placenta | Durative intrauterine
bleeding | None | 32 | 1,300 | Neonatal death |
| 3 | 26 | 0 | Suspected of
macrosomia | Hematoma of
broad | None | 40 | 2,950 | PPH |
| 4 | 27 | 0 | Suspected of
macrosomia | Uterine atony | None | 40 | 4,100 | PPH |
| 5 | 29 | 0 | Amniotic fluid
pollution, OCT (+) | Uterine atony | B-lynch | 41 | 3,850 | PPH |
| 6 | 31 | 0 | Failed induction of
labor | Durative intrauterine
bleeding | None | 40 | 3,460 | Normal |
| 7 | 28 | 0 | Persistent OT | Durative intrauterine
bleeding | B-lynch | 39 | 3,510 | PPH |
| 8 | 21 | 0 | Persistent OP | Durative intrauterine
bleeding | B-lynch | 40 | 3,670 | PPH |
| 9 | 20 | 0 | Multiple
pregnancy | Uterine atony | None | 37 | 2,680, 2,800 | Normal |
| 10 | 27 | 0 | Failed induction of
labor | Durative intrauterine
bleeding | None | 41 | 4,220 | Normal |
| 11 | 32 | 1 | Suspected of
placental abruption | Durative intrauterine
bleeding | None | 28 | 1,130 | Normal |
| 12 | 29 | 0 | Multiple
pregnancy | Uterine atony | B-lynch | 37 | 2580, 2450 | Normal |
Results
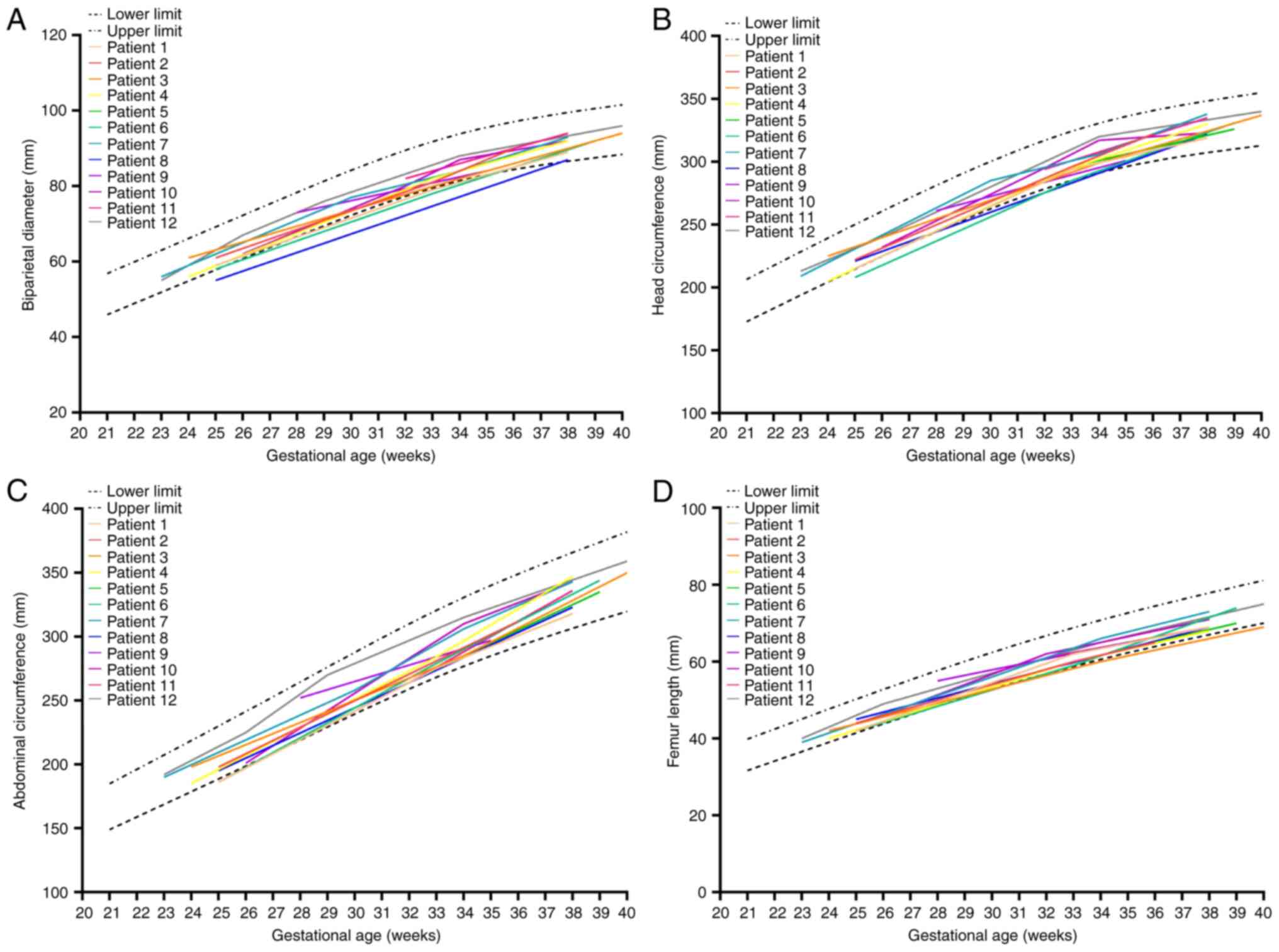
The delay before a subsequent pregnancy following
BUAL was 2-7 years. As biparietal diameter (BPD), head
circumference (HC), abdominal circumference (AC), and femur length
(FL) are fetal biometric parameters for intrauterine growth
restriction calculations, for the subsequent pregnancy, the data of
fetal biometry parameters were fitted to the gestational age in
weeks (gestational age) satisfactorily with a cubic polynomial
model (Fig. 1). Parameters for all
the patients were within the range of the 3rd-97th percentile
(14) according to gestational
age.
The outcomes of the 12 patients in the subsequent
pregnancy after BUAL are described in Table II. For 7 of the 12 cases, the mode
of delivery was cesarean section, and five had a vaginal delivery.
There were no cases of PPH or maternal or neonatal death in the
series. Follow-ups were performed by telephone annually, and all
children in the study exhibited normal development.
 | Table IIOutcomes of the subsequent pregnancies
after bilateral uterine artery ligation for obstetric
emergencies. |
Table II
Outcomes of the subsequent pregnancies
after bilateral uterine artery ligation for obstetric
emergencies.
| Case | Period since previous
delivery, months | Mode of delivery | Term of delivery,
weeks | BUAL | PPH | Fetal birth weight,
g | Maternal and neonatal
outcome |
|---|
| 1 | 41 | Cesarean section | 41 | Yes | No | 3,840 | Normal |
| 2 | 31 | Vaginal delivery | 36 | No | No | 2,485 | Normal |
| 3 | 35 | Cesarean section | 39 | No | No | 3,280 | Normal |
| 4 | 80 | Cesarean section | 38 | No | No | 3,490 | Normal |
| 5 | 52 | Cesarean section | 39 | No | No | 3,310 | Normal |
| 6 | 39 | Cesarean section | 39 | No | No | 3,420 | Normal |
| 7 | 84 | Cesarean section | 39 | No | No | 4,030 | Normal |
| 8 | 37 | Cesarean section | 40 | No | No | 3,540 | Normal |
| 9 | 34 | Vaginal delivery | 38 | No | No | 3,120 | Normal |
| 10 | 55 | Vaginal instrumental
delivery (forceps) | 40 | No | No | 3,965 | Normal |
| 11 | 87 | Vaginal delivery | 37 | No | No | 2,695 | Normal |
| 12 | 34 | Vaginal delivery | 38 | No | No | 3,325 | Normal |
Discussion
Ligation of the uterine artery is a simple procedure
that can be adopted in emergency situations, even by obstetricians
with limited training. For decades, ligation of the uterine artery
was theoretically and erroneously assumed to shut off the uterine
blood supply, which may thus result in hypoxemic injury of the
uterus, leading to endometrial or myometrial damage. Furthermore,
it may cause placental dysfunction and subsequent placental
disorders, leading to IUGR in subsequent pregnancies (15,16).
Apart from occasional reported complications,
overall data appear reassuring regarding the long-term fertility
and obstetric outcomes after ligation of the uterine artery
(9-11,17,18),
according to data on the return of menses, the subsequent new
pregnancies, and re-canalization of arteries and normal blood flow
in the uterine artery as shown by color Doppler examination
(19). To the best of our
knowledge, no previous studies have reported complications in
pregnancy, such as IUGR, and subsequent maternal and neonatal
outcomes. In the present study, no IUGR or maternal or neonatal
morbidity was observed. These results are consistent with the
absence of adverse effects of BUAL on the subsequent gestational
period. The underlying mechanism of unaffected pregnancy may be
that the blood flow shifts to the collateral circulation after the
blockage of the uterine artery and ensures adequate blood flow to
the uterus. Additionally, re-canalization of the arteries may
proceed during the period of uterine involution (Fig. 2) (13,20).
The results of the present study are based on
retrospective data from a single center, and clinical information,
including patient characteristics, maternal and neonatal outcomes,
and fetal biometry parameters (BPD, HC, AC, and FL) in each
pregnancy, was reported in detail. To the best of our knowledge,
the present study is the first to focus on IUGR in subsequent
pregnancy among women who had undergone BUAL in a previous
pregnancy. The primary limitations of the present study are the
small sample size, and that it was not possible to identify all
patients who underwent BUAL in our hospital and who had subsequent
pregnancies based on the database. Therefore, these results need to
be interpreted with caution and may should only serve as a
reference for future more comprehensive studies, and there is a
need for good-quality evidence-based prospective studies with
larger sample sizes to confirm these findings.
In conclusion, BUAL is a safe surgical technique,
and it does not appear to compromise a woman's subsequent obstetric
outcomes. Future pregnancies do not appear to pose an increased
risk of intrauterine growth retardation. Therefore, BUAL may be
more widely recommended in clinical practice.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
All data generated and/or analyzed during the
present study are included in this published article.
Authors' contribution
JA designed the study, analyzed data, wrote the
paper, and confirmed the authenticity of all the raw data. JA read
and approved the final manuscript.
Ethics approval and consent to
participate
This study was reviewed and approved by the
Institutional Board Review of Xiamen Women and Children's Hospital
(approval no. KY2023018). All the methodology was performed in
accordance with the relevant guidelines and regulations. The
Institutional Board Review of Xiamen Women and Children's Hospital
waived the requirement for informed consent from patients.
Patient consent for publication
Not applicable.
Competing interests
The authors declare they have no competing
interests.
References
|
1
|
O'Leary JA: Pregnancy following uterine
artery ligation. Obstet Gynecol. 55:112–113. 1980.PubMed/NCBI
|
|
2
|
Fahmy K: Uterine artery ligation to
control postpartum hemorrhage. Int J Gynaecol Obstet. 25:363–367.
1987.PubMed/NCBI View Article : Google Scholar
|
|
3
|
AbdRabbo SA: Stepwise uterine
devascularization: A novel technique for management of uncontrolled
postpartum hemorrhage with preservation of the uterus. Am J Obstet
Gynecol. 171:694–700. 1994.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Gonsalves M and Belli A: The role of
interventional radiology in obstetric hemorrhage. Cardiovasc
Intervent Radiol. 33:887–895. 2010.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Abbas AM, Shady NW and Sallam HF:
Bilateral uterine artery ligation plus intravenous tranexamic acid
during cesarean delivery for placenta previa: A randomized
double-blind controlled trial. J Gynecol Obstet Hum Reprod.
48:115–119. 2019.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Sentilhes L, Gromez A, Clavier E, Resch B,
Verspyck E and Marpeau L: Fertility and pregnancy following pelvic
arterial embolisation for postpartum haemorrhage. BJOG. 117:84–93.
2010.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Fiori O, Deux JF, Kambale JC, Uzan S,
Bougdhene F and Berkane N: Impact of pelvic arterial embolization
for intractable postpartum hemorrhage on fertility. Am J Obstet
Gynecol. 200:384.e1–e4. 2009.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Hardeman S, Decroisette E, Marin B,
Vincelot A, Aubard Y, Pouquet M and Maubon A: Fertility after
embolization of the uterine arteries to treat obstetrical
hemorrhage: A review of 53 cases. Fertil Steril. 94:2574–2579.
2010.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Wagaarachchi PT and Fernando L: Fertility
following ligation of internal iliac arteries for life-threatening
obstetric haemorrhage: Case report. Hum Reprod. 15:1311–1313.
2000.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Sentilhes L, Trichot C, Resch B, Sergent
F, Roman H, Marpeau L and Verspyck E: Fertility and pregnancy
outcomes following uterine devascularization for severe postpartum
haemorrhage. Hum Reprod. 23:1087–1092. 2008.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Unal O, Kars B, Buyukbayrak EE, Karsidag
AYK and Turan C: The effectiveness of bilateral hypogastric artery
ligation for obstetric hemorrhage in three different underlying
conditions and its impact on future fertility. J Matern Fetal
Neonatal Med. 24:1273–1276. 2011.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Domingo S, Perales-Puchalt A, Soler I,
Marcos B, Tamarit G and Pellicer A: Clinical outcome, fertility and
uterine artery Doppler scans in women with obstetric bilateral
internal iliac artery ligation or embolisation. J Obstet Gynaecol.
33:701–704. 2013.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Kaplanoglu M, Karateke A, Un B, Gunsoy L
and Baloglu A: Evaluation of uterine artery recanalization and
Doppler parameters after bilateral uterine artery ligation in women
with postpartum hemorrhage. Int J Clin Exp Med. 8:7823–7829.
2015.PubMed/NCBI
|
|
14
|
Zhang Y, Meng H, Jiang Y, Xu Z, Ouyang Y,
Li S, Chen Q, Wu Q, Li R, Ru T, et al: Chinese fetal biometry:
Reference equations and comparison with charts from other
populations. J Matern Fetal Neonatal Med. 32:1507–1515.
2019.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Gizzo S, Saccardi C, Patrelli TS, Di Gangi
S, Breda E, Fagherazzi S, Noventa M, D'Antona D and Nardelli GB:
Fertility rate and subsequent pregnancy outcomes after conservative
surgical techniques in postpartum hemorrhage: 15 Years of
literature. Fertil Steril. 99:2097–2107. 2013.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Blanc J, Courbiere B, Desbriere R,
Bretelle F, Boubli L, d'Ercole C and Carcopino X: Is
uterine-sparing surgical management of persistent postpartum
hemorrhage truly a fertility-sparing technique? Fertil Steril.
95:2503–2506. 2011.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Sziller I, Hupuczi P and Papp Z:
Hypogastric artery ligation for severe hemorrhage in obstetric
patients. J Perinat Med. 35:187–192. 2007.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Doumouchtsis SK, Nikolopoulos K,
Talaulikar V, Krishna A and Arulkumaran S: Menstrual and fertility
outcomes following the surgical management of postpartum
haemorrhage: A systematic review. BJOG. 121:382–388.
2014.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Demirci F, Ozdemir I, Safak A, Ozden S and
Somunkiran A: Comparison of colour Doppler indices of pelvic
arteries in women with bilateral hypogastric artery ligation and
controls. J Obstet Gynaecol. 25:273–274. 2005.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Dubay ML, Holshauser CA and Burchell RC:
Internal iliac artery ligation for postpartum hemorrhage:
Recanalization of vessels. Am J Obstet Gynecol. 136:689–691.
1980.PubMed/NCBI View Article : Google Scholar
|