1. Introduction
Papillary thyroid cancer (PTC) is the most prevalent
type of thyroid malignancy in the endocrine system, accounting for
85-90% of all thyroid carcinoma cases (1-3).
According to the 2020 Global Cancer Observatory survey, ~586,000
new PTC cases are reported worldwide (4). Thyroid carcinoma primarily
encompasses papillary, follicular, myeloid and undifferentiated
histopathological subtypes. PTC is highly treatable and curable,
provided that it is diagnosed and managed appropriately at an early
stage. Even in cases involving lymph node metastasis, the prognosis
for patients with PTC remains favorable, with minimal impact on
survival rates compared with other thyroid carcinoma types.
Consequently, the need for radical thyroid surgery in patients with
PTC remains controversial, as the primary clinical challenge faced
by these patients has been proposed to be overdiagnosis and
overtreatment (5). Therefore, a
novel readily detectable and definitive biomarker of PTC is in
urgent demand, which may genuinely minimize the risk of
overdiagnosis in such patients and alleviate the financial burden
associated with their medical expenses.
The development and progression of PTC has been
attributed to both genetic and environmental risk factors. Numerous
studies have identified gene mutations in tumor-suppressing
oncogenes, including V-Raf murine sarcoma viral oncogene homolog B1
(BRAF), RAS, Ret protooncogene (RET/PTC) and paired
box gene 8/peroxisome proliferator-activated receptor γ
(PAX8/PPARγ), which contribute to PTC carcinogenesis
(6,7). Due to important advancements in PTC
research, the American Thyroid Association (ATA) updated its
management guidelines for adult patients with thyroid nodules and
differentiated thyroid cancer in 2015. For thyroid nodules where
cytology cannot provide definitive diagnosis, detection of BRAF,
RAS, RET/PTC and PAX8/PPARγ fusion protein variants has
been proposed to enhance the accuracy and reliability of the
pathological diagnosis (8,9). This may in turn facilitate the
exploration of personalized therapeutic options.
The BRAF gene encodes a protein
kinase-dependent kinase and harbors a notable single-nucleotide
polymorphism (SNP) at codon 600, where valine is substituted by
glutamate (V600E). This SNP is one of the most common genotypic
hallmarks among the >300 mutations reported to be associated
with PTC to date, and is found in ≤80% of patients with PTC
(10-12).
This BRAF V600E mutation has been previously shown to modulate
factors in the MAPK signaling pathway, leading to the stimulation
of the ERK signaling pathway, as well as and cancer cell
proliferation and transformation (13-15).
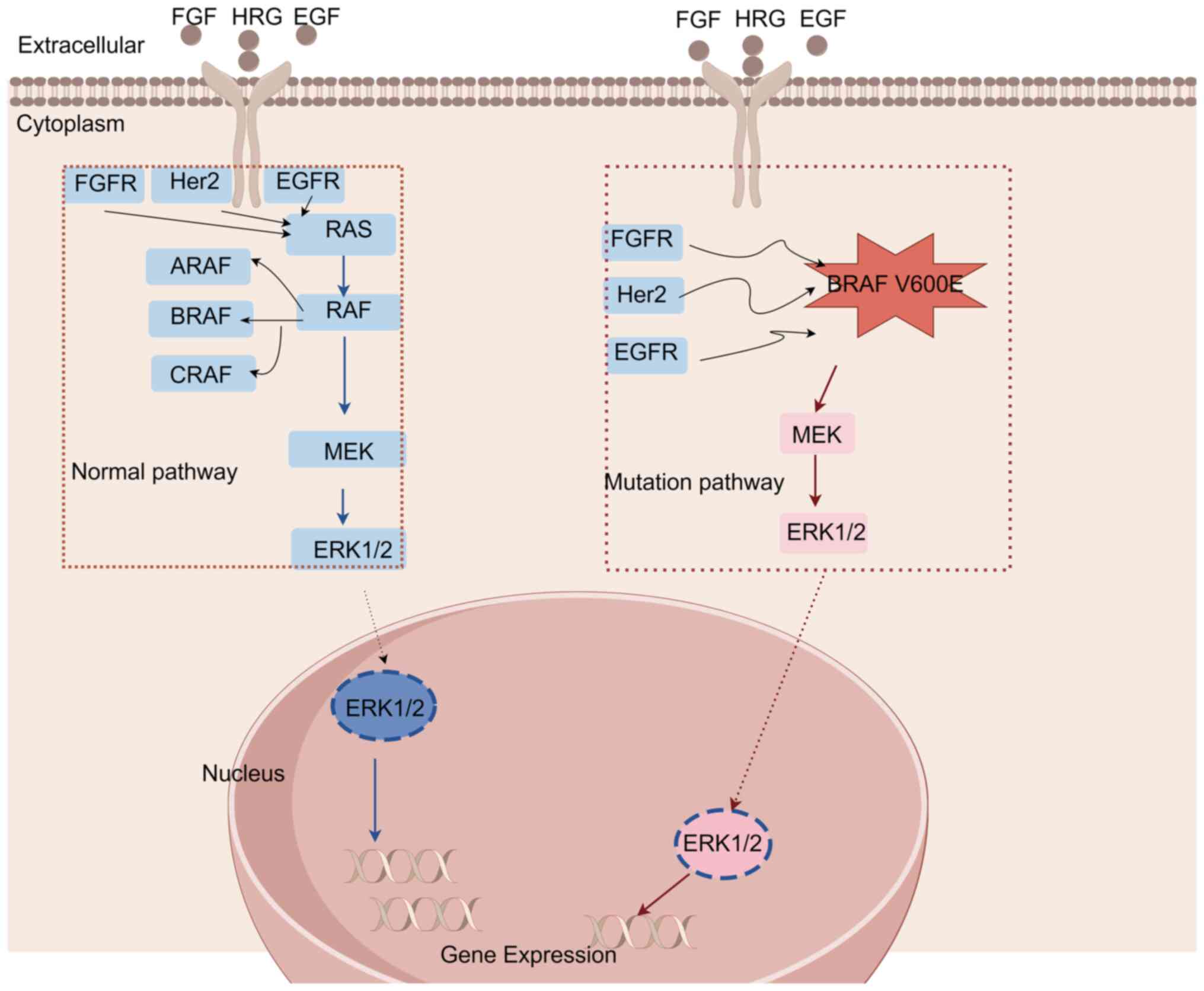
A schematic representation of the various signaling pathways
involved in PTC is depicted in Fig.
1, highlighting the importance of the BRAF gene in the
pathogenesis of PTC. In addition, accurate detection of this BRAF
V600E mutation in patients with thyroid nodules can significantly
improve the diagnostic accuracy whilst reducing the likelihood of
overtreatment and unnecessary surgery (16). Therefore, early detection of this
BRAF mutation is likely to be pivotal to the treatment process, as
it enables positively diagnosed patients to receive personalized
targeted therapy based on the type of carcinoma, which should lead
to favorable clinical and survival outcomes (17).
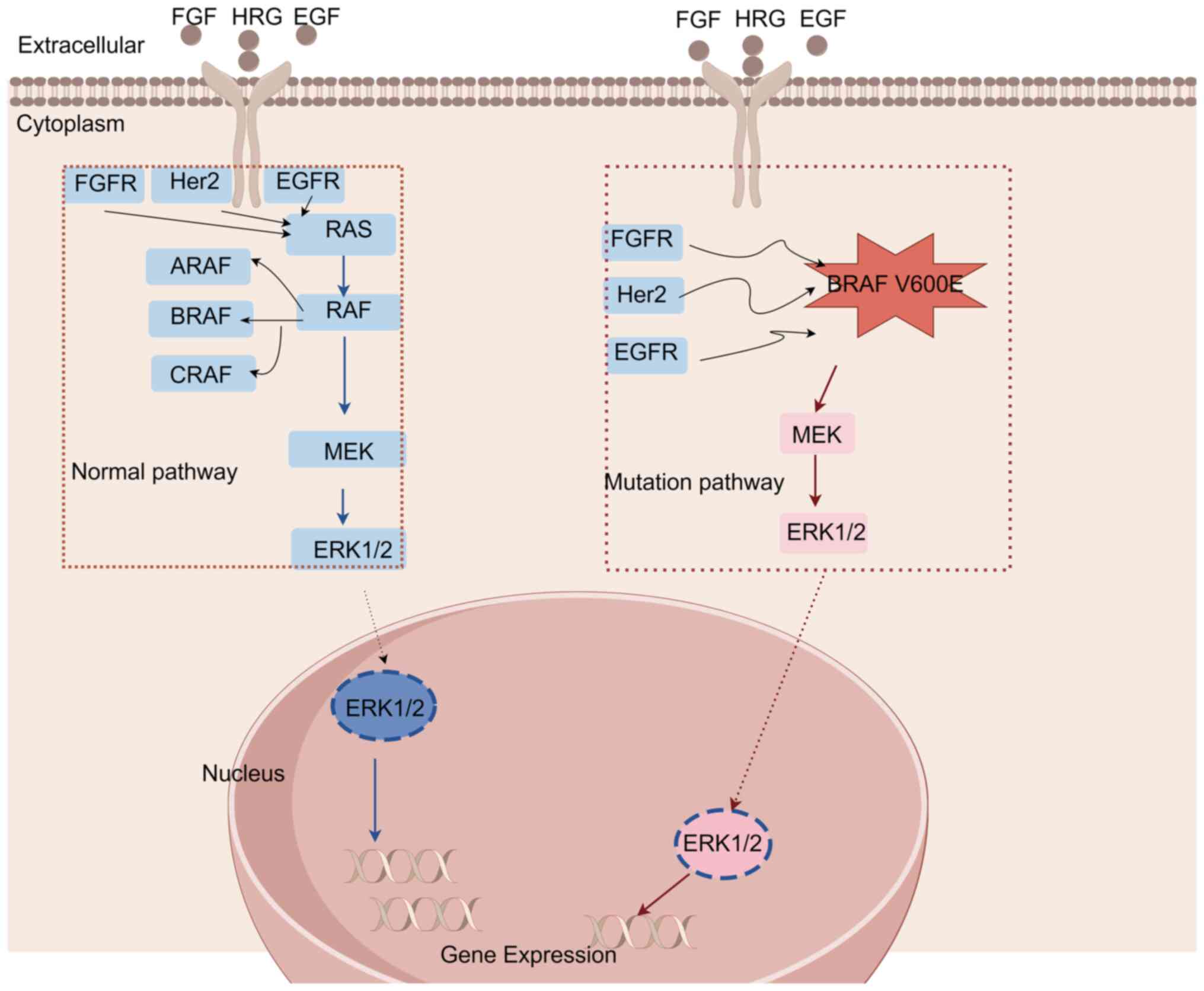 | Figure 1BRAF gene signaling pathway. Normal
pathway: RAF kinase, a protein encoded by BRAF, can activate
downstream MEK through phosphorylation. The MAPK/ERK signaling
pathway can regulate cell proliferation, differentiation, migration
and apoptosis. BRAF gene mutated pathway: BRAF remains active if a
pathogenic mutation occurs, which can lead to the continuous
activation of RAF protein, which in turn continuously transmits
signals to its downstream pathway when no chemical signal is
received, thus resulting in uncontrolled cell proliferation. V600E
is a common carcinogenic gene mutation site. BRAF, V-Raf murine
sarcoma viral oncogene homolog B1; FGF, fibroblast growth factor;
HRG, histidine-rich glycoprotein; EGF, epidermal growth factor;
Her2, human epidermal growth factor receptor 2. |
In the era of next-generation sequencing (NGS)
techniques, detection and analysis of the BRAF V600E mutation have
been performed under clinical settings using a variety of different
methods such as Sanger sequencing (18), pyrosequencing (19), reverse transcription-quantitative
PCR (RT-qPCR) (20), amplification
refractory mutation system (ARMS), NGS technology, high-resolution
melting (HRM), droplet digital PCR (ddPCR) (21), MassArray (22) and immunohistochemistry (IHC)-based
mutation detection (23). Among
these methods, Sanger sequencing is considered to be the ‘gold
standard’ in the majority of diagnostic studies. However,
significant heterogeneity exists in the specificity and sensitivity
of these techniques for identifying the BRAF V600E mutation in
patient samples. Therefore, the application of specific detection
methods for certain types of carcinoma and/or tissue sample origins
should facilitate the rapid and precise detection of cancer
genotypes, in turn improving the prognosis and treatment outcomes.
Following a comprehensive search of the published literature, the
present review aimed to discuss the precision of the BRAF V600E
mutation detection strategies available in various different
cohorts of patients with PTC in order to provide a guideline for
improving the diagnostic strategy of PTC.
2. Literature search
Search strategy
The China National Knowledge Infrastructure (CNKI)
(https://www.cnki.net/), PubMed (https://pubmed.ncbi.nlm.nih.gov/) and Web of
Science (https://www.webofscience.com/wos/) databases were
systematically searched using the key words or Medical Subject
Headings terms ‘BRAF V600E’, ‘mutation’, ‘Papillary thyroid
carcinoma’ and ‘Thyroid cancer test method’ to identify the
relevant full-length research articles, where ≥3 possible gene
mutations were evaluated for identifying BRAF gene mutations in PTC
cases.
Search process
Keyword combinations ‘BRAF V600E gene’, ‘mutation’,
‘papillary thyroid carcinoma’ and ‘test method’ were used in CNKI
(https://www.cnki.net/), PubMed (https://pubmed.ncbi.nlm.nih.gov/) and Web of
Science databases (https://www.webofscience.com/wos/) to identify
potential articles. Through a comprehensive search of various
databases, a total of 47 articles that specifically addressed the
detection methods for BRAF gene mutations were screened. All
articles reported controlled study designs. However, the 30
articles compared the performance of ≤4 detection methods for BRAF
V600E mutation. Therefore, all the available and routinely
practiced methods in clinical settings were discussed in the
present review, in order to assist clinicians in finding the best
method based on cancer subtype and/or sample criteria.
3. Techniques
Sanger sequencing
Sanger sequencing, also known as chain termination
PCR, takes advantage of the nucleotide polymerization process
starting at a fixed point and terminating at a random base at
certain distances (24). In this
type of PCR, unlike standard PCR, the polymerase incorporates
modified deoxyribonucleotides at random bases before ceasing the
PCR, thus generating amplicons of various lengths (25). For this procedure, a DNA polymerase
is typically used to extend the primers bound to the template of
the undetermined sequence, until a chain termination nucleotide is
incorporated. However, formation of base-paired single-stranded DNA
loops is a serious issue in resolving the bands at certain points
using this technique. To overcome this, a denaturing
polyacrylamide-urea gel is used, where the DNA bands can then be
visualized using either autoradiography or ultraviolet light.
Sanger sequencing is considered to be the ‘gold
standard’ for sequencing (26) and
can be used to directly detect gene mutations. However, it consists
of a highly complex operation process, is time consuming, and has
mandatory requirements for high DNA template quality and quantity.
Due to the methodological limitations of this method, its detection
sensitivity is limited, as well as the length of the DNA sequences
read using this method. Therefore, Sanger sequencing is currently
only used as a confirmatory method to another sequencing method in
clinical settings for tumor genotype identification.
Pyrosequencing
Pyrosequencing is a method that is based on an
enzyme cascade reaction mediated by four enzymes, namely DNA
polymerase, ATP sulfatase, luciferase and double phosphatase, which
was developed by Nyrén (27) in
1987. Pyrosequencing uses small fragments of PCR (amplicons) to
initiate the synthesis of a new strand, followed by the detection
of the incorporated bases by fluorescence. It is one of the most
accurate methods for detecting SNPs (28) whilst also being suitable for
sequencing and analyzing known short sequences (29,30).
Colozza-Gama et al (19) previously compared Sanger sequencing
and pyrosequencing for detecting a somatic driver mutation, and
observed that pyrosequencing was vastly superior for the detection
of single nucleotide variants, particularly in highly degraded
tumor samples derived from formalin-fixed paraffin-embedded (FFPE)
specimens. Using DNA samples isolated from FFPE specimens, all
papillary thyroid microcarcinoma and lymph node metastases samples
were screened for BRAF V600E mutation by pyrosequencing. In total,
103/115 (89.6%) samples tested positive for BRAF V600E by
pyrosequencing, while 101/115 (87.8%) samples tested positive by
Sanger sequencing. These comparisons were independently performed,
which suggested that Sanger sequencing was not as sensitive as
pyrosequencing. It was therefore concluded that pyrosequencing was
a viable method for detecting the BRAF V600E point mutation in DNA
isolated from FFPE sections.
Since pyrosequencing is highly reproducible and its
accuracy is similar to that of Sanger sequencing but with faster
detection speed (31), it is the
recommended method for the analysis and detection of various
genetic polymorphism markers such as SNPs, mutations,
insertions/deletions, methylations and gene copy numbers. However,
pyrosequencing has a notably low level of variability compared with
other methods.
RT-qPCR
RT-qPCR determines the quantity of each PCR product
by using fluorescent signals emitted by fluorescent-tagged
nucleotides incorporated during the DNA amplification reaction in a
real-time manner, which can be used to quantitatively measure the
content of specific DNA sequences in the sample by using as a
reference to internal control or housekeeping gene (32,33).
There is a linear association between the quantification threshold
(Cq) value of the template and the number of cycles of
amplification, where an increase in the template copy number is
reflected in the reduction of Cq value. RT-qPCR technology
effectively resolves the limitation of traditional quantitative
end-point detection methods by detecting and recording the
fluorescence signal intensity once in each cycle. Finally, the
quantitative results are obtained according to a standard curve by
calculating the Cq value of each sample or by using a comparative
2-∆∆Cq method (34).
Tian et al (35) previously found that the total
coincidence rate of the RT-qPCR and Sanger sequencing methods was
98.4% in 312 patients with PTC treated in the Cancer Hospital of
Peking Union Medical College. The positive concordance rate for the
RT-qPCR method was 100%, while the negative concordance rate was
95.6%. Although the sensitivity of RT-qPCR was observed to be
higher compared with that of the Sanger sequencing method, the
difference was not found to be statistically significant.
In a previous study by Yu et al (36), a comparison of the detection
efficiencies of RT-qPCR and IHC-based methods for identifying PTC
genotype revealed that the positive rates of the two methods were
identical (both 83.82%) in 136 PTC cases. Within this cohort, one
case was found to be negative by RT-qPCR but positive by IHC
testing, whilst another case exhibited the opposite result.
Consequently, the positive coincidence rate of the two methods was
calculated to be 99.1%, whilst the negative coincidence rate was
95.5%. These findings suggest that the RT-qPCR method is the most
suitable method for detecting the BRAF V600E mutation. RT-qPCR is
currently a widely applied technique for BRAF V600E mutation
identification. Although this method enables the real-time
quantification of DNA sequences with high sensitivity, its
limitations are similar to those of standard PCR, since it cannot
be used to detect novel mutations. In addition, successful RT-qPCR
demands high levels of technical expertise and requires specific
training and relevant molecular biology knowledge, since the
experimental conditions are markedly stringent. Due to such
limitations, hospitals prefer to use IHC for detecting the BRAF
V600E mutation.
High-throughput sequencing
High-throughput sequencing is also known as NGS
technology. It can be used to simultaneously sequence millions of
DNA molecules with the highest sensitivity and specificity. NGS
mainly includes the following methods: Whole-genome sequencing
(37), whole-exome sequencing
(38,39) and deep sequencing (40). At present, available NGS platforms
include 454 (Roche Diagnostics), Solexa (Illumina, Inc.), ABI Solid
(Applied Biosystems; Thermo Fisher Scientific, Inc.), Ion Torrent
(Thermo Fisher Scientific, Inc.) and BGISEQ (Beijing Genomics
Institute). The specific operation steps vary depending on the
different sequencing platforms used (41).
Smallridge et al (42) previously found a key clinical
association between BRAF gene mutations, immune gene expression and
lymphocyte infiltration in patients with PTC with different Tumor
Node Metastasis stages by NGS analysis, suggesting a role for BRAF
in immune modulation.
The high-throughput and high-resolution capacities
of NGS yield comprehensive genetic information, greatly reducing
the cost and time of sequencing. However, previous studies have
also shown that both V600E and V600K mutations can cross-react with
each other (43-45)
and may even cross-react with V600R. Therefore, NGS is typically
used to search for candidate gene mutations for certain disease
genotypes (46).
ARMS
ARMS is an enhanced PCR method also known as
allele-specific amplification. Based on the principle that the 3'
terminal base of a primer must complement its template DNA for
effective amplification, allele-specific PCR amplification primers
are designed to detect mutations in ARMS. In a typical experimental
scheme of ARMS, four primers are used to amplify the sequence on
one side of the mutation site, whereas the other three primers are
used to amplify the sequence on the other side.
ARMS has been previously compared with other methods
for BRAF V600E mutation detection in PTC samples. Among 371
patients with confirmed PTC, the detection rate of this mutation
using the ARMS method was 74.1% vs. 76.5% yielded by the ddPCR
method. However, no significant difference could be found between
the two groups. In addition, both methods exhibited a have similar
accuracy and high sensitivity (47).
ARMS has the advantages of a relatively simple
operational procedure, high degree of sensitivity, short detection
cycles and small sample requirements. By contrast, its shortcomings
include low-throughput, high cost and unsuitability for SNP
detection at sites that are too near or too far from GC-rich
sequences. In addition, it cannot detect unknown mutations.
Therefore, ARMS is suitable only for the detection of a small
number of biopsy specimens with known target mutations.
IHC
IHC uses the specific antigen-antibody binding
principle, whereby a primary antibody is detected by labeling with
a chromogenic agent (such as fluorescein, enzyme, metal ions or
isotopes) to detect target antigens (peptides or proteins) in
tissues. IHC can be used to examine the cellular localization and
expression levels of proteins in tissues from various diseases. VE1
is a sensitive mouse monoclonal antibody that can target mutated
and constitutively active BRAF V600E protein. Capper et al
(48) previously developed a
method for synthesizing the V600E mutant amino acid sequence based
on the 11 amino acids of BRAF 596-606. This was then injected into
immunized mice to form a hybridoma cell line and obtain the
aforementioned VE1 monoclonal antibody. The mechanism of action of
the VE1 antibody is mediated by binding onto specific amino acid
residues of the BRAF V600E mutant protein, thereby recognizing and
labeling the positions where the BRAF V600E mutation is present.
The VE1 antibody can recognize this mutation because its active
site matches the specific amino acid residues on the BRAF V600E
mutant protein, thus forming a stable antigen-antibody complex
(48). VE1 can be used to reveal
the existence of tumor heterogeneity, such that in a small number
of biopsy specimens, as well as the presence of BRAF
mutation-positive tumor cells. IHC with VE1 monoclonal antibody has
been previously found to be efficient for detecting BRAF V600E
mutations in brain metastases of thyroid cancer (49,50).
Rashid et al (51) previously reported an IHC analysis
method for PTC tissues using VE1 antibody, where a rate of
concordance of 98.6% was found between IHC and sequencing-based
mutation detection in 72 patients with PTC. In addition, the
detection rate of BRAF mutation was higher in IHC analysis compared
with Sanger sequencing. The same conclusion was reached in the
studies conducted by Bullock et al (52) and Zhao et al (53). Choden et al (54) also reported a high specificity for
IHC with VE1 antibody in a cohort study of 514 patients with PTC
compared with Sanger sequencing. Specifically, VE1 in IHC yielded
99.3% sensitivity and 100% specificity, while Sanger sequencing
yielded 84.2% sensitivity and 84.2% specificity. Furthermore, IHC
with VE1 monoclonal antibody exhibited high sensitivity and
specificity for the detection of BRAF V600E mutation in melanoma
(55) and colorectal carcinoma
(56). Several studies have also
observed that VE1 antibody can be used not only for surgical
specimens but also for needle aspiration cytology specimens with
high sensitivity and specificity (57,58).
Although the traditional IHC method has low
sensitivity and specificity, with the identification of the VE1
antibody, the detection specificity of a particular BRAF gene
mutation has been significantly improved, without any
cross-reactions with similar mutations. Since IHC is a relatively
cost-effective screening method, it has been widely used for the
diagnosis of PTC, malignant melanoma and thyroid nodule puncture
specimens, although it is not recommended for colorectal cancer.
Colorectal cancer diagnosis typically relies on colonoscopy and
biopsy, which allow direct observation and sampling of tumor
tissue. By contrast, IHC is primarily used to detect specific
proteins in tissue samples, and its role in the diagnosis of
colorectal cancer is limited. Secondly, the treatment of colorectal
cancer usually requires knowledge of the tumor's molecular
characteristics, which are typically obtained through methods such
as genetic sequencing rather than IHC. Numerous studies have
suggested the appearance of weak or focal immunostaining in certain
cases, which may lead to diagnostic ambiguities. In these cases,
additional genetic analysis may be required to determine the BRAF
status of the patient (49).
ddPCR
ddPCR is a third-generation PCR technology and an
absolute quantification method for nucleic acid molecules. The
underlying principle entails treatment of the sample with a
microdrop prior to PCR amplification, so that the reaction system
containing the nucleic acid molecules is divided into numerous
microdroplets, and each microdroplet is amplified to detect the
presence or absence of the target nucleic acid.
In a study of PTC-associated BRAF V600E mutation
conducted by Yanping et al (47), the total coincidence rate between
the ddPCR and ARMS methods was found to be 92.5%, whilst the
positive accuracy of ddPCR and ARMS was 97.9% and 94.1%,
respectively. In conclusion, the positive mutations detected by
these two methods were suggested to have similar accuracies. In a
previous study by Qingqing et al (32), the positive rate of BRAF V600E
mutation detected by ddPCR was found to be 94.3%, although only 35
specimens were analyzed.
Fu et al (50) previously used a ddPCR-based
molecular assay that enabled the sensitive and specific detection
of BRAF V600E variation by incorporating the use of locked nucleic
acid technology. It was also found to facilitate the discrimination
of single nucleotide mismatches compared with traditional real-time
PCR probes. Additionally, BRAF mutations were successfully
identified in 26.7% residual fine-needle aspiration (FNA) biopsies.
Follow-up of 48 patients who underwent surgical resection
identified a concordance in BRAF status between the FNA
tissue and the matched surgical specimens using the ddPCR
assay.
ddPCR has high sensitivity and requires only a small
number of templates to complete the detection, which overcomes the
various limitations of second-generation PCR technology, such as
low accuracy, difficulty in accurately determining the gene copy
number, and inability to qualitatively and quantitatively detect
trace mutations (59). It is
therefore widely used for the early screening of tumors, detection
of secondary drug resistance and real-time monitoring of tumor
load. However, it cannot detect unknown mutations, and the number
of detected mutations in one run is limited.
HRM
HRM is a quantitative analytical method for the melt
curves of DNA amplicons following PCR amplification (60). HRM relies on the principle that PCR
amplification of a gene containing certain mutations leads to the
denaturation of the duplex DNA strands during heating. This
breaking of the DNA strands subsequently releases the incorporated
fluorescent dye, which can be quantified with respect to time
(61). Previous studies have
suggested this technique to be a reliable and reproducible DNA
mutation detection method suitable for FNA biopsies.
Junming et al (62) previously found that the specificity
and sensitivity of the HRM method for detecting the BRAF gene V600E
mutation were 90 and 100%, respectively, compared with those of
Sanger sequencing in 16 patients of PTC. Sanger sequencing was used
to assess 16 PTC specimens, from which 1 specimen could not be
assessed due to the poor quality of the extracted DNA, and 6/15
cases were actually detected (40.00%). The HRM method detected 7/16
positive cases (43.75%). The specimens that could not be detected
by sequencing method could be detected by the HRM method. This
previous study has showed that HRM could be used for the detection
of the BRAF V600E mutation in fine needle puncture specimens of
PTC. Loes et al (63)
previously applied this method to detect the BRAF V600E mutation in
melanoma and colorectal cancer samples.
In conclusion, the HRM method is simple, sensitive,
and superior to Sanger sequencing and IHC. Its sensitivity is
equivalent to that of ARMS, but is more cost effective. In
addition, it can detect both known and unknown mutations with
considerable reproducibility. However. a major disadvantage of this
method is that it cannot be used for RNA detection, and its ability
to identify base mutations is low. It can only be used to detect
small fragments of amplification products and cannot distinguish
mutations with similar melting curves.
MassARRAY
MassARRAY is a method that integrates the high
sensitivity of PCR with high-throughput chip technology and the
high accuracy of mass spectrometry technology. It is the only
technology platform that enables the direct detection of SNP by
mass spectrometry. Using this technique, SNP genotyping, gene
expression detection, gene methylation analysis, DNA sequencing,
pathogen typing and prenatal diagnosis can all be performed in one
platform (64).
Qingqing et al (32) previously applied the MassARRAY
method to detect the BRAF V600E mutation in PTC. The positive rate
of BRAF V600E mutation detected by this method was 74.3%, which was
higher than that of Sanger sequencing (60.0%).
The MassARRAY technique is typically used for
genotyping and mutation detection, methylation analysis, gene
expression analysis and pathogen detection. Its advantage is the
ability to simultaneously detect known mutations in multiple genes
with high specificity and sensitivity. However, the operational
protocols are highly complex and it cannot be applied to detect
unknown mutations.
Restriction fragment length
polymorphism (RFLP)
RFLP is a first-generation DNA molecular marker
technology that is widely used for the construction of genetic maps
for evolution studies and classification of species. It is based on
the mutation, insertion or deletion of bases in restriction sites
in the genomes of individuals, resulting in changes in the size of
restriction fragments (65). This
change can be detected by specific probe hybridization, where the
frequency of mutation can be compared by measuring the differences
in DNA length (polymorphism) in different samples. The comparison
of multiple probes can be applied to establish the evolutionary and
taxonomic associations among organisms. The probes used in RFLP are
derived from the same or different types of genomic DNA clones
located at different sites of chromosomes, so that they can be used
as a molecular marker for constructing molecular maps.
Due to its high specificity and sensitivity, Lin
et al (66) previously
applied this method to successfully detect the BRAF V600E mutation
in a molecular study of PTC. Sezer et al (67) also used this method in incidental
papillary thyroid microcarcinoma.
RFLP is frequently used for detecting gene
polymorphism and genotyping. Its sample stability is good, but the
analysis cost is high, and the operational procedure is complex and
at times tedious. Therefore, RFLP can only be used to detect known
SNPs or insertion/deletion mutations.
Single-strand conformation
polymorphism (SSCP)
SSCP was established by Orita et al (68) in 1989 to analyze differences
between DNA sequences. This method is widely used for the screening
of different genomic variants in a large sample and in a broad
range of organisms. At low temperatures, single-stranded DNA folds
into a three-dimensional conformation mediated by intermolecular
interactions, which affects its mobility in non-denatured gels. DNA
molecules with the same length but different nucleotide sequences
are separated in the gel by mobility shift assay. Bands with
different mobility can then be detected by silver staining or
fluorescently labeled primers and then analyzed by automatic DNA
sequencing. PCR-SSCP can be used to detect sequence differences,
but its sensitivity decreases with increasing DNA fragment lengths.
SSCP has been previously used in cancer prognosis (69,70),
asthma (71), blood group test
(72), Gilbert syndrome (73), diabetes (74), respiratory distress syndrome
(75), male varicocele infertility
(76), gastric mucosa (77), traditional Chinese medicine
(78), bacterial DNA detection
(79) and identification of
Trichomonas vaginalis (80).
Hashim and Al-Shuhaib (81) previously compared the advantages
and disadvantages of RFLP with SSCP, and found that both methods
had certain limitations and advantages, such that neither was
superior. The PCR-SSCP method is widely used for the detection of
novel mutations in both basic and applied biological and
environmental sciences (82).
Since there are multiple BRAF examination methods, SSCP is seldomly
considered first choice under clinical settings at present.
Overall, SSCP exhibits high sensitivity, low cost and operational
convenience (83), but its
reproducibility is poor.
4. Discussion
PTC is typically diagnosed by thyroid color Doppler
ultrasound during physical examination. The application of its
high-frequency probe can clearly show the internal microstructure,
blood vessels and blood flow in the thyroid, and can even detect
micro lesions measuring >2 mm in size, resulting in a high
preoperative diagnostic rate of thyroid cancer (84,85).
However, despite the high sensitivity and specificity of this
technique for detecting thyroid nodules, the missed diagnosis and
misdiagnosis rates of suspected thyroid cancer or multiple thyroid
cancer foci are relatively high, rendering it insufficient to
diagnose PTC alone. Therefore, FNA should be performed in patients
with suspected PTC for a definitive diagnosis. In particular, the
ATA recommends FNA for thyroid nodules of >1 cm in diameter.
Furthermore, FNA should be performed for thyroid nodules measuring
<1 cm in diameter that are also suspected of being thyroid
cancer, especially for patients with a family history of thyroid
cancer or childhood history of neck radiation. Although the
sensitivity and specificity of FNA examination are reported to
reach 83 and 92%, respectively, due to insufficient sampling and
the inability to distinguish between benign and malignant
follicular thyroid lesions, 20-30% of thyroid nodules typically
cannot be diagnosed clinically (86). In these cases, malignancies can
only be identified after surgery (9). Therefore, accurate diagnosis of
ambiguous FNA remains a challenge to clinicians treating patients
with thyroid disease. Gene mutation detection compensate the
deficiency of FNA detection to a certain extent. For patients who
are FNA-negative but highly suspected of suffering from thyroid
cancer, postoperative pathological detection combined with gene
mutation detection can be used to determine the risk level of PTC
recurrence, adopt appropriate surgical methods, reduce unnecessary
diagnostic surgery and formulate a reasonable follow-up plan
(87).
Genes that have been previously associated with the
occurrence and development of thyroid cancer include BRAF,
RAS, RET/PTC and PAX8/PPARγ. Previous studies
have found that single gene mutations have low sensitivity for the
diagnosis of PTC, whilst the combined detection of mutations in two
or multiple genes can improve its sensitivity by several folds
(59,88). BRAF is a member of the RAF family
of serine/threonine-specific protein kinases and has three
conserved regions (CR), namely CR1, CR2 and CR3(89). RAS genes, including
H-Ras, N-Ras and K-Ras, encode four proteins
(one H-Ras, one N-Ras and two K-Ras) with a relative molecular
weight of ~21 kDa, which have been documented to regulate cell
proliferation, differentiation and death (84). Ras can simultaneously activate a
variety of signaling pathways, inducing several tumor-related
phenotypic changes. Gene mutations in RAS have been found to
occur in 20-50% of thyroid follicular carcinoma (90), 10% of PTC (mainly the follicular
subtype), poorly differentiated thyroid carcinoma (18-52%)
(91) and follicular adenoma
(24-53%) (92). The RET
oncogene is located on chromosome 10 (10q11.2) and encodes
transmembrane tyrosine kinase receptors glial cell-derived
neurotrophic factor, neurturin, artemin and persephin (93), which serve as growth factor
receptors coupled with different glycosylphosphatidylinositol
α-receptor-activated RET (94).
There are mainly three different subtypes of RET, namely RET51,
RET43 and RET9(95), and their
C-terminal domain contains 51, 43 and 9 amino acids, respectively.
Under normal circumstances, RET expression in thyroid follicular
cells is negligible. The RET/PTC oncogene is the rearranged
form of the RET protooncogene in PTC. The PAX8 gene
is located on chromosome 2 and belongs to the Pax transcription
factor family (96). By contrast,
the PPARγ gene is located at p25 on chromosome 3 and encodes
a group of nuclear receptor proteins, which participate in the
expression of genes associated with cell differentiation,
development and metabolism as transcription factors (97). A previous study found that the
PAX8/PPARγ fusion protein was expressed in a group of thyroid
follicular adenoma subsets (98).
The neurotrophic receptor tyrosine kinase 1 (NTRK1) oncogene, also
known as TRK, is located in the q arm of chromosome 1 (1q21-22).
Its coding protein is a member of the NTRK family (99). The incidence of NTRK1 oncogene
variation in PTC has been documented to be ~10% (100). p53 is encoded by the TP53
gene on the short arm of chromosome 17 (17p13.1). This gene is
highly conserved in vertebrates, especially in the five regions of
exons 2, 5, 6, 7 and 8. p53 point mutations, which weaken its
original transcriptional activity, have been observed in 55% of
undifferentiated thyroid cancer (101). A list of commonly found mutated
genes in various pathological types of thyroid cancer are
summarized in Table I. In addition
to the aforementioned genes, differentially expressed genes between
PTC and normal thyroid tissue have also been identified, including
thyroid peroxidase, metallophosphoesterase domain-containing 2 and
cadherin 16, which may become potential alternative biomarkers for
the diagnosis and treatment of PTC. However, further validation is
required for clinical applications (102).
 | Table ICommon gene mutations in thyroid
cancer. |
Table I
Common gene mutations in thyroid
cancer.
| Mutation | Pathological
types |
|---|
| BRAF | PTC (classic, tall
cell and follicular variants) and anaplastic thyroid cancer |
| RAS | Follicular
carcinoma, papillary thyroid cancer (follicular variant) and
follicular adenoma |
| RET/PTC | PTC |
| PAX8-PPARγ | Follicular
carcinoma |
| TRK | PTC |
| P53 | Anaplastic thyroid
cancer |
The BRAF V600E mutation is most common one in PTC
but rarely occurs in other subtypes of thyroid carcinoma and benign
thyroid tumor lesions (103).
Previous studies have confirmed that the BRAF V600E mutation can
affect multiple processes, such as thyroid growth, infiltration and
dedifferentiation (14,104-106),
and can be used as a molecular biological marker for the diagnosis
and prognosis of PTC. Therefore, the BRAF V600E test is generally
preferred for diagnosing suspected patients with PTC, due to its
high specificity and positive predictive value (107). The BRAF V600E mutation serves an
important role not only in the diagnosis of the disease but also in
targeted therapy. The main treatment mode of PTC is surgery plus
iodine-131 plus postoperative hormone inhibition treatment, which
is generally effective. However, for aggressive thyroid cancer,
specifically for subtypes with low differentiation, weak iodine
uptake ability or even no iodine uptake, iodine-131 treatment
cannot achieve a good curative effect. At present, targeted drugs
for medullary thyroid carcinoma (108,109) and anaplastic thyroid carcinoma
(110), such as sorafenib and
lenvatinib, have been used in the clinic with satisfactory results,
although they also cause adverse reactions. In addition, a human
phage single-chain fragment variable antibody library have been
successfully constructed to screen for their effects on medullary
thyroid carcinoma (111) and
anaplastic thyroid carcinoma (112). However, despite having been
tested in nude mice and yielded potential therapeutic effects, it
has not been applied in the clinic thus far. These aforementioned
previous studies suggest that targeted therapy or immunotherapy may
benefit patients with aggressive thyroid cancer. Furthermore, BRAF
mutations have been proposed to predict the therapeutic effect of
targeted drugs for colorectal cancer and malignant melanoma, which
frequently predicts poor patient prognosis. For a number of mutant
PTC cases, it has been documented that the application of BRAF
inhibitors can block the activation of MAPK signaling, facilitating
PTC therapy. In a gene expression study on BRAF mutant PTC,
transcriptome sequencing and gene mutation data revealed that the
expression of programmed death ligand (PD-L)1, PD-L2, CD80, CD86
and cytotoxic T-lymphocyte associated protein 4 (CTLA4) was
upregulated (113). A previous
small-sample clinical study including 22 patients found that
pembrolizumab had an antitumor effect on PD-L1-positive advanced
thyroid cancer (114). It has
also been found that the BRAF V600E mutation in PTC is positively
correlated with PD-L1 expression (115), suggesting that immunotherapy may
have a superior therapeutic effect on patients with BRAF gene
mutations in PTC. However, studies on the association between PTC,
and PD-L2, CD80, CD86 and CTLA4 remain in their infancy.
There have been numerous studies that attempted to
predict the pathogenesis of thyroid cancer based on molecular,
morphological and immunological characteristics, with specific
focus on the detection of cancer-related protein-coding genes to
explore the possibility of targeted or immunotherapy. Trybek et
al (116) previously found
that patients with PTC with BRAF V600E and telomerase reverse
transcriptase mutations exhibited poor prognosis and clinical
course, suggesting that such mutations could be used to predict
poor treatment response and recurrence. BRAF mutations combined
with PIK3CA, TP53 and AKT1 mutations have also been associated with
the invasive characteristics of PTC (117). Therefore, before initiating
targeted therapy, accurate detection of high-risk genes is highly
recommended to efficiently guide the treatment course. In addition,
analysis of the above mutations can also be used to develop a
personalized therapeutic strategy for patients with PTC. Due to the
existence of different detection methods, sample types, and
sensitivity and specificity rates, the positive rates of the
various BRAF V600E mutation detection methods in PTC tissues are
also heterogenous. Therefore, using more sensitive detection
methods for different specimen types may facilitate diagnosis and
predict prognosis. The differences between the aforementioned
methods are shown in Table
II.
 | Table IIComparison of different detection
methods. |
Table II
Comparison of different detection
methods.
| Method | Advantages | Disadvantages | Application | BRAF mutation |
|---|
| Sanger | Effective, direct
detection of gene mutation | Low sensitivity,
complex operation, time-consuming, unsuitable for a large number of
samples | ‘Gold standard’ for
sequencing | Rarely
utilized |
| Pyrosequencing | High specificity
and sensitivity, fast detection | Low
variability | SNPs, mutation,
insertion/deletion, methylation, gene copy number detection | Rarely
utilized |
| RT-PCR | High specificity
and sensitivity, less human factors | Cross-reaction,
high operation training requirements, unknown mutations cannot be
detected | First-choice
detection method for gene mutations | Commonly used |
| NGS | High throughput and
sensitivity, less time | Cross-reaction | Search for
candidate genes for diseases | Commonly used |
| ARMS | High specificity
and sensitivity, less time, simple operation | Low throughput,
unknown mutations cannot be detected, unsuitable for SNP detection
with excessive or insufficient proximity to the GC site | Detection of a
small number of biopsy specimens | Commonly used |
| IHC | Low cost, high
specificity, and sensitivity | Complicated
operation | Preliminary
screening method for gene mutation detection | Commonly used |
| ddPCR | High sensitivity,
small sample size, low cost, less human factors | Detection of a
limited number of mutations | Early screening and
detection of tumor drug resistance | Uncommonly
used |
| High resolution
melting | High throughput,
specificity and sensitivity, good repeatability, low cost,
detection of known and unknown mutations | Unsuitable for RNA
detection, weak detection ability of basic mutations, small
amplified products can be detected, variation of similar melting
curves cannot be distinguished | Gene mutation
detection for fine needle aspiration biopsy specimens | Uncommonly
used |
| MassARRAY | High specificity
and sensitivity, simultaneous detection of multiple genes | Complicated
operation, unknown mutations cannot be detected | Genotyping and
mutation detection, methylation analysis, gene expression analysis,
pathogen detection | Uncommonly
used |
| RFLP | Good stability, no
phenotypic effect | Complicated
operation, time-consuming, high cost, low polymorphic information,
unknown mutations cannot be detected | Genotyping, genetic
map construction, gene location, biological evolution | Uncommonly
used |
| Single-strand
conformation polymorphism | High sensitivity,
less time, simple operation, detection of known and unknown
mutations | Poor
repeatability | Genetic analysis,
gene mutation detection | Uncommonly
used |
There are various methods for detecting BRAF gene
mutations, among which gene sequencing is the most direct method.
It mainly includes first-, second- and third-generation sequencing.
First-generation sequencing methods, also known as direct
sequencing methods, mainly include Sanger sequencing and
pyrosequencing. Second-generation sequencing mainly refers to NGS,
whereas third-generation sequencing technology refers to
single-molecule sequencing technology, where each DNA molecule is
sequenced separately without PCR amplification. Therefore,
third-generation sequencing technology is also called de
novo sequencing technology or single-molecule real-time DNA
sequencing, and is mainly used in genome sequencing, methylation
research and mutation identification (SNP detection). In addition,
RT-qPCR, ARMS, HRM, ddPCR and MassARRAY can be used to detect BRAF
gene mutations. IHC uses the principle of the specific binding of
an antigen by an antibody to examine protein localization and
expression levels. Traditional IHC methods require tissue samples
with a high abundance of tumor cells, while the detection rate in
FNA is low. However, the VE1 monoclonal antibody can reveal the
existence of tumor heterogeneity and determine the proportion of
mutant cells in tumors in IHC sections, which greatly increases the
detection rate of IHC, thus facilitating its application for the
detection of gene mutation in FNA. Furthermore, the detection
methods described in the present review are not limited to BRAF
mutations but can also be applied to other genes. Therefore, they
can serve a supplementary role in preoperative diagnosis.
Nevertheles, due to its low cost and lack of need for specialist
instruments and equipment, IHC appears to currently be the main
diagnostic method of choice.
This present article aimed to provide an overview of
the various methods available for detecting the BRAF V600E
mutation, which can help to guide clinical decisions in the
treatment of patients with cancer. Knowing the type of specimen
(e.g., tissue biopsy, blood or urine) can help clinicians to select
the most appropriate testing method. However, the present article
is based on clinical needs and does not focus on innovation or
highlight new technologies, which may be considered a limitation of
the study, as it does not address the latest advancements in the
field. Future research will incorporate the novel technologies and
innovations that have recently emerged.
At present, the clinical diagnosis of patients
suspected of thyroid cancer primarily relies on the method of
percutaneous tissue biopsy, which may lead to false-negative
results. When combined with genetic testing, if the tumor cells in
the submitted samples are sparse and mixed with a large number of
wild-type somatic cells, detection then becomes challenging, and
conventional sequencing methods may fail to accurately detect the
mutations. This obstacle can significantly delay patients from
receiving active and effective treatment. Therefore, for the
detection of BRAF V600E mutations in patients with PTC, selecting
an optimal detection method for different sample types can
effectively improve the detection rate of mutations. Accurate
detection of gene mutations is also important for guiding the
immunotherapy of PTC, particularly in cases of aggressive thyroid
carcinoma.
In summary, RT-qPCR and IHC remain the most commonly
used detection methods for tissue samples from patients with PTC,
especially with the application of VE1 antibody, which
significantly enhances the sensitivity and specificity of IHC. IHC
is typically used as a preliminary screening method, whilst ARMS
and HRM have high specificity, and are suitable for FNA biopsies of
thyroid nodules. NGS is an ideal choice for a large number of
samples and high-throughput analyses. However, it is worth noting
that clinical diagnosis based on single-gene detection frequently
suffers from reduced diagnostic efficacy, making multigene combined
diagnosis more accurate.
Acknowledgements
Not applicable.
Funding
Funding: The present study was supported by the Scientific
Research Fund of Chengdu Medical College (grant no. CYZ18-24),
Scientific Research Project of Medicine Department of Sichuan
Province (grant no. S18001), Health Commission of Sichuan Province
(grant no. 20PJ227) and Scientific Research Project of Medicine
Department of Chengdu City (grant no. 2021051).
Availability of data and materials
Not applicable.
Authors' contributions
All authors contributed to the study conception and
design. XX and YS contributed to the conception of the study. XJ
contributed to data analysis and manuscript preparation. WT, LL, YH
and YX participated in data analysis with constructive discussions.
The data collection, analysis and first draft of the manuscript was
written by QL and all authors commented on previous versions of the
manuscript, confirmed the accuracy of the data and agreed to submit
the manuscript. All authors read and approved the final version of
the manuscript. Data authentication is not applicable.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2020. CA Cancer J Clin. 70:7–30. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Li M, Maso LD and Vaccarella S: Global
trends in thyroid cancer incidence and the impact of overdiagnosis.
Lancet Diabetes Endocrinol. 8:468–470. 2020.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Bray F, Ferlay J, Soerjomataram I, Siegel
RL, Torre LA and Jemal A: Global cancer statistics 2018: GLOBOCAN
estimates of incidence and mortality worldwide for 36 cancers in
185 countries. CA Cancer J Clin. 68:394–424. 2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Sung H, Ferlay J, Siegel RL, Laversanne M,
Soerjomataram I, Jemal A and Bray F: Global cancer statistics 2020:
GLOBOCAN estimates of incidence and mortality worldwide for 36
cancers in 185 countries. CA Cancer J Clin. 71:209–249.
2021.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Jegerlehner S, Bulliard JL, Aujesky D,
Rodondi N, Germann S, Konzelmann I and Chiolero A: NICER Working
Group. Overdiagnosis and overtreatment of thyroid cancer: A
population-based temporal trend study. PLoS One.
12(e0179387)2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Prescott JD and Zeiger MA: The RET
oncogene in papillary thyroid carcinoma. Cancer. 121:2137–2146.
2015.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Raman P and Koenig RJ: Pax-8-PPAR-γ fusion
protein in thyroid carcinoma. Nat Rev Endocrinol. 10:616–623.
2014.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Haugen BR: 2015 american thyroid
association management guidelines for adult patients with thyroid
nodules and differentiated thyroid cancer: What is new and what has
changed? Cancer. 123:372–381. 2017.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Cabanillas ME, Mcfadden DG and Durante C:
Thyroid cancer. Lancet. 388(2783)2016.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Cohen Y, Xing M, Mambo E, Guo Z, Wu G,
Trink B, Beller U, Westra WH, Ladenson PW and Sidransky D: BRAF
mutation in papillary thyroid carcinoma. J Natl Cancer Inst.
95:625–627. 2003.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Delellis RA, Lloyd RV and Heitz PU:
Pathology and genetics of tumours of endocrine organs. IARC Press.
2004.
|
|
12
|
Nikiforov YE: Molecular diagnostics of
thyroid tumors. Arch Pathol Lab Med. 135:569–577. 2011.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Xing M: BRAF mutation in papillary thyroid
cancer: Pathogenic role, molecular bases, and clinical
implications. Endo Rev. 28:742–762. 2007.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Ali KM, Awny S, Ibrahim DA, Metwally IH,
Hamdy O, Refky B, Abdallah A and Abdelwahab K: Role of P53,
E-cadherin and BRAF as predictors of regional nodal recurrence for
papillary thyroid cancer. Ann Diagno Pathol. 40:59–65.
2019.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Ahmed AU, Sarvestani ST, Gantier MP,
Williams BR and Hannigan GE: Integrin-linked kinase modulates
lipopolysaccharide- and helicobacter pylori-induced nuclear factor
κB-activated tumor necrosis factor-α production via regulation of
p65 serine 536 phosphorylation. J Biol Chem. 289:27776–27793.
2014.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Yin L, Tang Y, Yu S, Wang C, Xiao M, Wang
Y, Liu SJ, Gao L, Huang K and Jin L: The role of BRAF V600E in
reducing AUS/FLUS diagnosis in thyroid fine needle aspiration.
Endocr Pathol. 30:312–317. 2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Tanda ET, Vanni I, Boutros A, Andreotti V,
Bruno W, Ghiorzo P and Spagnolo F: Current state of target
treatment in BRAF mutated melanoma. Front Mol Biosci.
7(154)2020.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Cheng LY, Haydu LE, Song P, Nie J,
Tetzlaff MT, Kwong LN, Gershenwald JE, Davies MA and Zhang DY: High
sensitivity sanger sequencing detection of BRAF mutations in
metastatic melanoma FFPE tissue specimens. Sci Rep.
11(9043)2021.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Colozza-Gama GA, Callegari F, Bešič N,
Paniza ACJ and Cerutti JM: Machine learning algorithm improved
automated droplet classification of ddPCR for detection of BRAF
V600E in paraffin-embedded samples. Sci Rep.
11(12648)2021.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Lung J, Hung MS, Lin YC, Jiang YY, Fang
YH, Lu MS, Hsieh CC, Wang CS, Kuan FC, Lu CH, et al: A highly
sensitive and specific real-time quantitative PCR for BRAF V600E/K
mutation screening. Sci Rep. 10(16943)2020.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Malicherova B, Burjanivova T, Grendar M,
Minarikova E, Bobrovska M, Vanova B, Jasek K, Jezkova E, Kapinova
A, Antosova M, et al: Droplet digital PCR for detection of BRAF
V600E mutation in formalin-fixed, paraffin-embedded melanoma
tissues: A comparison with Cobas((R)) 4800, Sanger sequencing, and
allele-specific PCR. Am J Transl Res. 10:3773–3781. 2018.PubMed/NCBI
|
|
22
|
Sutton BC, Birse RT, Maggert K, Ray T,
Hobbs J, Ezenekwe A, Kazmierczak J, Mosko M, Kish J, Bullock A, et
al: Assessment of common somatic mutations of EGFR, KRAS, BRAF,
NRAS in pulmonary non-small cell carcinoma using iPLEX(R) HS, a new
highly sensitive assay for the MassARRAY(R) System. PLoS One.
12(e0183715)2017.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Zhu X, Luo Y, Bai Q, Lu Y, Lu Y, Wu L and
Zhou X: Specific immunohistochemical detection of the BRAF V600E
mutation in primary and metastatic papillary thyroid carcinoma. Exp
Mol Pathol. 100:236–241. 2016.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Estrada-Rivadeneyra D: Sanger sequencing.
FEBS J. 284(4174)2017.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Xu J and Zhang S: Mitogen-activated
protein kinase cascades in signaling plant growth and development.
Trends Plant Sci. 20:56–64. 2015.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Sanger F, Sanger F, Nicklen S and Coulson
AR: DNA sequencing with chain-terminating inhibitors.
Biotechnology. 24:104–108. 1992.PubMed/NCBI
|
|
27
|
Nyrén P: The history of pyrosequencing.
Methods Mol Biol. 373:1–14. 2007.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Harrington CT, Lin EI, Olson MT and
Eshleman JR: Fundamentals of pyrosequencing. Arch Pathol Lab Med.
137:1296–1303. 2013.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Spittle C, Ward MR, Nathanson KL, Gimotty
PA, Rappaport E, Brose MS, Medina A, Letrero R, Herlyn M and
Edwards RH: Application of a BRAF pyrosequencing assay for mutation
detection and copy number analysis in malignant melanoma. J Mol
Diagn. 9:464–471. 2007.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Mcevoy AC, Wood BA, Ardakani NM, Pereira
M, Pearce R, Cowell L, Robinson C, Grieu-Iacopetta F, Spicer AJ,
Amanuel B, et al: Droplet digital PCR for mutation detection in
formalin-fixed, paraffin-embedded melanoma tissues: A comparison
with sanger sequencing and pyrosequencing. J Mol Diagn. 20:240–252.
2018.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Ronaghi M, Karamohamed S, Pettersson B,
Uhlen M and Nyren P: Real-time DNA sequencing using detection of
pyrophosphate release. Anal Biochem. 242:84–89. 1996.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Qingqing Y, Dongyu L, Junfeng S, Shuang S,
Rong Y and Qing C: Comparative study of BRAF V600E gene mutation
detection methods in paraffin specimens of thyroid papillary
carcinoma. Int J Lab Med. 41:1674–1681. 2020.
|
|
33
|
Matsuda K: PCR-based detection methods for
single-nucleotide polymorphism or mutation: Real-time PCR and its
substantial contribution toward technological refinement. Adv Clin
Chem. 80:45–72. 2017.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408.
2001.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Tian Q, Wen-ting H, Lei G, Hai-zhen L, Yun
L, Ling S, et al: Comparison of real-time PCR method with Sanger
sequencing for detection of BRAF muta tion in papillary thyroid
carcinoma. J Clin Exp Pathol. 31:756–758. 2015.
|
|
36
|
Yu Y, Xiaohua D, Ying L, Xirun Z and
Guangjuan Z: Comparative analysis of detection methods for V600E
mutation of B-Raf gene in papillary thyroid cancer. J Clin Exp
Pathol. 33:815–816. 2017.
|
|
37
|
Aguilar-Mahecha A, Lafleur J, Brousse S,
Savichtcheva O, Holden KA, Faulkner N, McLennan G, Jensen TJ and
Basik M: Early, on-treatment levels and dynamic changes of genomic
instability in circulating tumor DNA predict response to treatment
and outcome in metastatic breast cancer patients. Cancers (Basels).
13(1331)2021.PubMed/NCBI View Article : Google Scholar
|
|
38
|
van Dijk EL, Auger H, Jaszczyszyn Y and
Thermes C: Ten years of next-generation sequencing technology.
Trends Genet. 30:418–426. 2014.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Leprieur EG, Helias-Rodzewicz Z, Kamga PT,
Costantini A, Julie C, Corjon A, Dumenil C, Dumoulin J, Giraud V,
Labrune S, et al: Sequential ctDNA whole-exome sequencing in
advanced lung adenocarcinoma with initial durable tumor response on
immune checkpoint inhibitor and late progression. J Immunother
Cancer. 8(e000527)2020.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Beaubier N, Tell R, Lau D, Parsons JR,
Bush S, Perera J, Sorrells S, Baker T, Chang A, Michuda J, et al:
Clinical validation of the tempus xT next-generation targeted
oncology sequencing assay. Oncotarget. 10:2384–2396.
2019.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Glenn TC: Field guide to next-generation
DNA sequencers. Mol Ecol Resour. 11:759–769. 2011.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Smallridge RC, Ana-Maria C, Asmann YW,
Casler JD, Serie DJ, Reddi HV, Cradic KW, Rivera M, Grebe SK,
Necela BM, et al: RNA sequencing identifies multiple fusion
transcripts, differentially expressed genes, and reduced expression
of immune function genes in BRAF (V600E) mutant vs BRAF wild-type
papillary thyroid carcinoma. J Clin Endocrinol Metab. 99:E338–E347.
2014.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Ihle M, Fassunke J, König K, Grünewald I,
Schlaak M, Kreuzberg N, Tietze L, Schildhaus HU, Büttner R and
Merkelbach-Bruse S: Comparison of high resolution melting analysis,
pyrosequencing, next generation sequencing and immunohistochemistry
to conventional Sanger sequencing for the detection of p.V600E and
non-p.V600E BRAF mutations. BMC Cancer. 14(13)2014.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Tetzlaff M, Pattanaprichakul P, Wargo J,
Fox P, Patel K, Estrella J, Broaddus RR, Williams MD, Davies MA,
Routbort MJ, et al: Utility of BRAF V600E immunohistochemistry
expression pattern as a surrogate of BRAF mutation status in 154
patients with advanced melanoma. Hum Pathol. 46:1101–1110.
2015.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Forthun R, Hovland R, Schuster C,
Puntervoll H, Brodal H, Namløs H, Aasheim LB, Meza-Zepeda LA,
Gjertsen BT, Knappskog S and Straume O: ctDNA detected by ddPCR
reveals changes in tumour load in metastatic malignant melanoma
treated with bevacizumab. Sci Rep. 9(17471)2019.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Pellecchia S, Sepe R, Federico A, Cuomo M,
Credendino S, Pisapia P, Bellevicine C, Nicolau-Neto P, Ramundo MS,
Crescenzi E, et al: The Metallophosphoesterase-domain-containing
protein 2 (MPPED2) gene acts as tumor suppressor in breast
cancer. Cancers (Basel). 11(797)2019.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Yanping X, Yanping J, Jiayi F and Shirong
Z: Detection of BRAF gene mutation in papillary thyroid carcinoma
by probe amplification block mutation and digital PCR. J Clin Exp
Pathol. 37:227–229. 2021.
|
|
48
|
Capper D, Berghoff AS, Magerle M, Ilhan A,
Wohrer A, Hackl M, Pichler J, Pusch S, Meyer J, Habel A, et al:
Immunohistochemical testing of BRAF V600E status in 1,120 tumor
tissue samples of patients with brain metastases. Acta Neuropathol.
123:223–233. 2011.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Koperek O, Kornauth C, Capper D, Berghoff
AS, Asari R, Niederle B, von Deimling A, Birner P and Preusser M:
Immunohistochemical detection of the BRAF V600E-mutated protein in
papillary thyroid carcinoma. Am J Surg Pathol. 36:844–850.
2012.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Fu G, Chazen RS, MacMillan C and Witterick
IJ: Development of a molecular assay for detection and
quantification of the BRAF variation in residual tissue from
thyroid nodule fine-needle aspiration biopsy specimens. JAMA Netw
Open. 4(e2127243)2021.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Rashid FA, Tabassum S, Khan MS, Ansari HR,
Asif M, Sheikh AK and Aga SS: VE1 immunohistochemistry is an
adjunct tool for detection of BRAF(V600E) mutation: Validation in
thyroid cancer patients. J Clin Lab Anal. 35(e23628)2021.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Bullock M, O'Neill C, Chou A, Clarkson A,
Dodds T, Toon C, Sywak M, Sidhu SB, Delbridge LW, Robinson BG, et
al: Utilization of a MAB for BRAF (V600E) detection in papillary
thyroid carcinoma. Endocrin Related Cancer. 19:779–784.
2012.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Zhao J, Liu P, Yu Y, Zhi J, Zheng X, Yu J
and Gao M: Comparison of diagnostic methods for the detection of a
BRAF mutation in papillary thyroid cancer. Oncol Lett.
17:4661–4666. 2019.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Choden S, Keelawat S, Jung CK and Bychkov
A: VE1 immunohistochemistry improves the limit of genotyping for
detecting BRAFV600E mutation in papillary thyroid cancer. Cancers
(Basel). 12(596)2020.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Colomba E, Helias-Rodzewicz Z, Von
Deimling A, Marin C, Terrones N, Pechaud D, Surel S, Côté JF,
Peschaud F, Capper D, et al: Detection of BRAF p.V600E mutations in
melanomas: Comparison of four methods argues for sequential use of
immunohistochemistry and pyrosequencing. J Mol Diagn. 15:94–100.
2013.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Rössle M, Sigg M, Rüschoff JH, Wild PJ,
Moch H, Weber A and Rechsteiner M: Ultra-deep sequencing confirms
immunohistochemistry as a highly sensitive and specific method for
detecting BRAF V600E mutations in colorectal carcinoma. Virchows
Arch. 463:623–631. 2013.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Routhier CA, Mochel MC, Lynch K,
Dias-Santagata D, Louis DN and Hoang MP: Comparison of 2 monoclonal
antibodies for immunohistochemical detection of BRAF V600E mutation
in malignant melanoma, pulmonary carcinoma, gastrointestinal
carcinoma, thyroid carcinoma, and gliomas. Hum Pathol.
44:2563–2570. 2013.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Mfisher KE, Neill SG, Ehsani L, Caltharp
SA, Siddiqui MT and Cohen C: Immunohistochemical Investigation of
BRAF p.V600E mutations in thyroid carcinoma using 2 separate BRAF
antibodies. Appl Immunohistochem Mol Morphol. 22:562–567.
2014.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Czarniecka A, Oczko-Wojciechowska M and
Barczyński M: BRAF V600E mutation in prognostication of papillary
thyroid cancer (PTC) recurrence. Gland Surg. 5:495–505.
2016.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Liu LQ, Zhang HY, Xiao-Lia WU, Zhang W,
Chen XD and Wang J: Detection of KRAS and BRAF mutations in
non-small cell lung cancer by high resolution melting analysis.
Chin J Clin Laborat Sci. 2012.
|
|
61
|
Wang Z, Jing C, Cao H, Rong MA and
Jianzhong WU: Establishment and primary clinical application of
detecting EGFR mutations by high resolution melting analysis. Chin
J Surg Oncol. 2014.
|
|
62
|
Junming T, Q L, Xueca W and Guohong Q:
Establishment and primary clinical application of detecting BRAF
V600E mutations by HRM analysis. Chin J Surg Onco. 9:243–245.
2017.
|
|
63
|
Loes IM, Immervoll H, Angelsen JH, Horn A,
Geisler J, Busch C, Lønning PE and Knappskog S: Performance
comparison of three BRAF V600E detection methods in malignant
melanoma and colorectal cancer specimens. Tumour Biol.
36:1003–1013. 2015.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Tian HX, Zhang XC, Wang Z, Chen JG, Chen
SL, Guo WB and Wu YL: Establishment and application of a multiplex
genetic mutation-detection method of lung cancer based on MassARRAY
platform. Cancer Biol Med. 13:68–76. 2016.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Beckmann JS and Soller M: Restriction
fragment length polymorphism in genetic improvement: Methodologies,
mapping and costs. Theor Appl Genet. 67:35–43. 1983.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Lin AJ, Samson P, DeWees T, Henke L,
Baranski T, Schwarz J, Pfeifer J, Grigsby P and Markovina S: A
molecular approach combined with American thyroid association
classification better stratifies recurrence risk of classic
histology papillary thyroid cancer. Cancer Med. 8:437–446.
2019.PubMed/NCBI View Article : Google Scholar
|
|
67
|
Sezer H, Uren N and Yazici D: Association
between BRAF(V600E) mutation and the clinicopathological features
in incidental papillary thyroid microcarcinoma: A single-center
study in Turkish patients. North Clin Istanb. 7:321–328.
2020.PubMed/NCBI View Article : Google Scholar
|
|
68
|
Orita M, Suzuki Y, Sekiya T and Hayashi K:
Rapid and sensitive detection of point mutations and DNA
polymorphisms using the polymerase chain reaction. Genomics.
5:874–879. 1989.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Akhtar MS, Akhter N, Najm MZ, Deo SVS,
Shukla NK, Almalki SSR, Alharbi RA, Sindi AAA, Alruwetei A, Ahmad A
and Husain SA: Association of mutation and low expression of the
CTCF gene with Breast cancer progression. Saudi Pharm J.
28:607–614. 2020.PubMed/NCBI View Article : Google Scholar
|
|
70
|
Anwar M, Malhotra P, Kochhar R, Bhatia A,
Mahmood A, Singh R and Mahmood S: TCF 4 tumor suppressor: A
molecular target in the prognosis of sporadic colorectal cancer in
humans. Cell Mol Biol Lett. 25(24)2020.PubMed/NCBI View Article : Google Scholar
|
|
71
|
Al-Aaraji AJ, Al-Qaysi SA and SalihBaay A:
Haplotype in ABCC4 gene by PCR-SSCP technique in Iraqi Asthmatic
patients. Journal of Physics Conference Series.
1294(062037)2019.
|
|
72
|
Gogri H, Ray S, Agrawal S, Aruna S, Ghosh
K and Gorakshakar A: Heterogeneity of O blood group in India:
Peeping through the window of molecular biology. Asian J Transfus
Sci. 12:62–68. 2018.PubMed/NCBI View Article : Google Scholar
|
|
73
|
Aliarab A, Yaghmaei B, Ghaderian S,
Khoshnia M and Joshaghani HR: Effect of gilbert's syndrome
associated polymorphic alleles (rs8175347 and rs4148323) of
UDP-glucuronyl transferase on serum bilirubin level. Meta Gene.
26(100788)2020.
|
|
74
|
Al-Thuwaini T: Association between
polymorphism in BMP15 and GDF9 genes and impairing female fecundity
in diabetes type 2. Middle East Fertility Society J.
25(25)2020.
|
|
75
|
Wang X, Zhang Y, Mei H, An C, Liu C, Zhang
Y, Zhang Y and Xin C: Study on the relationship between respiratory
distress syndrome and SP-A1 (rs1059057) gene polymorphism in
mongolian very premature infants. Front Pediatr.
8(81)2020.PubMed/NCBI View Article : Google Scholar
|
|
76
|
Heidari MM, Khatami M, Danafar A, Dianat
T, Farahmand G and Talebi AR: Mitochondrial genetic variation in
Iranian infertile men with varicocele. Int J Fertil Steril.
10:303–309. 2016.PubMed/NCBI View Article : Google Scholar
|
|
77
|
Takano H, Shibata T, Nakamura M, Sakurai
N, Hayashi T, Ota M, Nomura-Horita T, Hayashi R, Shimasaki T,
Otsuka T, et al: Effect of DNMT3A polymorphisms on CpG island
hypermethylation in gastric mucosa. BMC Med Gene.
21(205)2020.PubMed/NCBI View Article : Google Scholar
|
|
78
|
Li M, Gao L, Qu L, Sun J, Yuan G, Xia W,
Niu J, Fu G and Zhang L: Characteristics of PCR-SSCP and RAPD-HPCE
methods for identifying authentication of Penis et testis cervi in
traditional Chinese medicine based on cytochrome b gene.
Mitochondrial DNA A DNA Mapp Seq Anal. 27:2757–2762.
2015.PubMed/NCBI View Article : Google Scholar
|
|
79
|
Hong B, Winkel A, Stumpp N, Abdallat M,
Saryyeva A, Runge J, Stiesch M and Krauss JK: Detection of
bacterial DNA on neurostimulation systems in patients without overt
infection. Clin Neurol Neurosurg. 184(105399)2019.PubMed/NCBI View Article : Google Scholar
|
|
80
|
Matini M, Rezaie S, Mohebali M, Maghsood
AH, Rabiee S, Fallah M and Rezaeian M: Genetic identification of
trichomonas vaginalis by using the actin gene and molecular based
methods. Iran J Parasitol. 9:329–335. 2014.PubMed/NCBI
|
|
81
|
Hashim HO and Al-Shuhaib MB: Exploring the
potential and limitations of PCR-RFLP and PCR-SSCP for SNP
detection: A review. J Appl Biotechnol Rep. 6:137–144. 2019.
|
|
82
|
Kakavas KV: Sensitivity and applications
of the PCR single-strand conformation polymorphism method. Mol Biol
Rep. 48:3629–3635. 2021.PubMed/NCBI View Article : Google Scholar
|
|
83
|
Barbacid M: ras genes. Ann Rev Biochem.
56:779–827. 1986.PubMed/NCBI View Article : Google Scholar
|
|
84
|
Shunbo L, Jingjing H and Dan G: Analysis
of clinical risk factors for cervical central lymph node metastasis
in papillary thyroid carcinoma. J Jinan Univ (Natural Science &
Medicine Edition). 2018;v.39;No.194(06):67-71.
|
|
85
|
Weichao C, Fan Y and Ankui Y: Status quo
of preoperative color Doppler ultrasound evaluation of central
lymph node metastasis of papillary thyroid cancer in China. Chin J
Clin Oncol. 046:1040–1045. 2019.
|
|
86
|
Davies L and Randolph G: Evidence-based
evaluation of the thyroid nodule. Otolaryngol Clin North Am.
47:461–474. 2014.PubMed/NCBI View Article : Google Scholar
|
|
87
|
Beisa A, Kvietkauskas M, Beisa V, Stoškus
M, Ostanevičiūtė E, Jasiūnas E, Griškevičius L, Šeinin D, Šileikytė
A and Strupas K: Significance of BRAF V600E mutation and
cytomorphological features for the optimization of papillary
thyroid cancer diagnostics in cytologically indeterminate thyroid
nodules. Exp Clin Endocrinol Diabetes. 127:247–254. 2019.PubMed/NCBI View Article : Google Scholar
|
|
88
|
Boursault L, Haddad V, Vergier B,
Cappellen D, Verdon S, Bellocq JP, Jouary T and Merlio JP: Tumor
homogeneity between primary and metastatic sites for braf status in
metastatic melanoma determined by immunohistochemical and molecular
testing. PLoS One. 8(e70826)2013.PubMed/NCBI View Article : Google Scholar
|
|
89
|
Sithanandam G, Druck T, Cannizzaro LA,
Leuzzi G, Huebner K and Rapp UR: B-raf and a B-raf pseudogene are
located on 7q in man. Oncogene. 7:795–799. 1992.PubMed/NCBI
|
|
90
|
Vasko V, Ferrand M, Di Cristofaro J,
Carayon P, Henry JF and de Micco C: Specific pattern of RAS
oncogene mutations in follicular thyroid tumors. J Clin Endocrinol
Metab. 6:2745–2752. 2003.PubMed/NCBI View Article : Google Scholar
|
|
91
|
Zhu Z, Manoj G, Nikiforova MN, Fischer AH
and Nikiforov YE: Molecular profile and clinical-pathologic
features of the follicular variant of papillary thyroid carcinoma.
An unusually high prevalence of ras mutations. Am J Clin Pathol.
1:71–77. 2003.PubMed/NCBI View Article : Google Scholar
|
|
92
|
Cantara S, Capezzone M, Marchisotta S,
Capuano S, Busonero GP, Toti P, Di Santo A, Caruso G, Carli AF,
Brilli L, et al: Impact of proto-oncogene mutation detection in
cytological specimens from thyroid nodules improves the diagnostic
accuracy of cytology. J Clin Endocrinol Metab. 95:1365–1369.
2010.PubMed/NCBI View Article : Google Scholar
|
|
93
|
Ce Ccherini I, Bocciardi R, Luo Y, Pasini
B, Hofstra R, Takahashi M and Romeo G: Exon structure and flanking
intronic sequences of the human RET proto-oncogene. Biochem Biophys
Res Commun. 196:1288–1295. 1993.PubMed/NCBI View Article : Google Scholar
|
|
94
|
Airaksinen MS, Titievsky A and Saarma M:
GDNF family neurotrophic factor signaling: Four masters, one
servant? Mol Cell Neurosci. 13:313–325. 1999.PubMed/NCBI View Article : Google Scholar
|
|
95
|
Myers SM, Eng C, Ponder BA and Mulligan
LM: Characterization of RET proto-oncogene 3' splicing variants and
polyadenylation sites: A novel C-terminus for RET. Oncogene.
11:2039–2045. 1995.PubMed/NCBI
|
|
96
|
Stapleton P, Weith A, Urbanek P, Kozmik Z
and Busslinger M: Chromosomal localization of seven PAX genes and
cloning of a novel family member, PAX-9. Nat Genet. 3:292–298.
1993.PubMed/NCBI View Article : Google Scholar
|
|
97
|
Michalik L, Auwerx J, Berger JP,
Chatterjee VK, Glass CK, Gonzalez FJ, Grimaldi PA, Kadowaki T,
Lazar MA, O'Rahilly S, et al: International Union of Pharmacology.
LXI. Peroxisome proliferator-activated receptors. Pharmacol Rev.
58:726–741. 2006.PubMed/NCBI View Article : Google Scholar
|
|
98
|
Marques AR, Espadinha C, Catarino AL,
Moniz S, Pereira T, Sobrinho LG and Leite V: Expression of
PAX8-PPAR gamma 1 rearrangements in both follicular thyroid
carcinomas and adenomas. J Clin Endocrinol Metabol. 8:3947–3952.
2002.PubMed/NCBI View Article : Google Scholar
|
|
99
|
Greco A, Miranda C and Pierotti MA:
Rearrangements of NTRK1 gene in papillary thyroid carcinoma. Mol
Cell Endocrinol. 321:44–49. 2010.PubMed/NCBI View Article : Google Scholar
|
|
100
|
Greco A, Miranda C, Pagliardini S, Fusetti
L, Bongarzone I and Pierotti MA: Chromosome 1 rearrangements
involving the genes TPR and NTRK1 produce structurally different
thyroid-specific TRK oncogenes. Genes Chromosomes Cancer.
19:112–123. 1997.PubMed/NCBI
|
|
101
|
Smallridge RC, Marlow LA and Copland JA:
Anaplastic thyroid cancer: Molecular pathogenesis and emerging
therapies. Endocr Relat Cancer. 16:17–44. 2009.PubMed/NCBI View Article : Google Scholar
|
|
102
|
Li W, Zhou J, Xu L, Su X, Liu Q and Pang
H: Identification of genes associated with papillary thyroid
carcinoma (PTC) for diagnosis by integrated analysis. Horm Metab
Res. 48:226–231. 2016.PubMed/NCBI View Article : Google Scholar
|
|
103
|
Sulaieva O, Chernenko O, Chereshneva Y,
Tsomartova D and Larin O: Thyroid stimulating hormone levels and
BRAFV600E mutation contribute to pathophysiology of papillary
thyroid carcinoma: Relation to outcomes? Pathophysiology.
26:129–135. 2019.PubMed/NCBI View Article : Google Scholar
|
|
104
|
Yanting L, Haiyong Z, Feixing Z, Xulian L
and Mengjun H: Consistency of BRAF (V600E) protein expression and
gene mutation in papillary thyroid cancer and its clinical
significance. J Clin Exp Pathol. 34:42–45. 2018.
|
|
105
|
Martinez JRW, Vargas-Salas S, Gamboa SU,
Munoz E, Dominguez JM, Leon A, Droppelmann N, Solar A, Zafereo M,
Holsinger FC and González HE: The combination of RET, BRAF and
demographic data identifies subsets of patients with aggressive
papillary thyroid cancer. Horm Cancer. 10:97–106. 2019.PubMed/NCBI View Article : Google Scholar
|
|
106
|
Xing M, Alzahrani AS, Carson KA, Viola D,
Elisei R, Bendlova B, Yip L, Mian C, Vianello F, Tuttle RM, et al:
Association between BRAF V600E mutation and mortality in patients
with papillary thyroid cancer. J Am Med Assoc.
310(535)2013.PubMed/NCBI View Article : Google Scholar
|
|
107
|
Melo M, da Rocha AG, Batista R, Vinagre J,
Martins MJ, Costa G, Ribeiro C, Carrilho F, Leite V, Lobo C, et al:
TERT, BRAF and NRAS in primary thyroid cancer and metastatic
disease. J Clin Endocrinol Metab. 6:1898–1907. 2017.PubMed/NCBI View Article : Google Scholar
|
|
108
|
Hong C, Zequan C and Yongli Y: Research
progress of targeted therapy in medullary thyroid carcinoma. J
Shanghai Jiaotong University (Medical Science). 31:1470–1474.
2011.
|
|
109
|
Kesby NL, Papachristos AJ, Gild M, Aniss
A, Sywak MS, Clifton-Bligh R, Sidhu SB and Glover AR: Outcomes of
advanced medullary thyroid carcinoma in the era of targeted
therapy. Ann Surg Oncol. 29:64–71. 2022.PubMed/NCBI View Article : Google Scholar
|
|
110
|
Tianle Y, Lisha X, Yutao F, Shuting W,
Renqi T and Xin J: Research status on sorafenib combined medication
in anapastic thyroid cancer. Chin J Clin Pharmacol. 37(4)2021.
|
|
111
|
Xiaoli H, Zhengjie W and Hua P:
Construction of human medullary thyroid carcinoma phage antibody
library and preliminary identification. J Chongqing Med University.
38:1040–1043. 2013.
|
|
112
|
Jimei X, Sen Z, Qiong L, Wenbo L and Hua
P: Construction and screenning of a natural phage antibody library
of human anaplastic thyroid carcinoma. Immunol J. 31:692–696.
2015.PubMed/NCBI View Article : Google Scholar
|
|
113
|
Chunping D, Zhilin L, Chunjun L, Changhong
W and Yun M: Gene expression and tumor microenvironment alterations
in BARF mutant papillary thyroid carcinoma. Shandong Med J.
60:25–28. 2020.
|
|
114
|
Mehnert JM, Varga A, Brose MS, Aggarwal
RR, Lin CC, Prawira A, de Braud F, Tamura K, Doi T, Piha-Paul SA,
et al: Safety and antitumor activity of the anti-PD-1 antibody
pembrolizumab in patients with advanced, PD-L1-positive papillary
or follicular thyroid cancer. BMC Cancer. 19(196)2019.PubMed/NCBI View Article : Google Scholar
|
|
115
|
Bai Y, Guo T, Huang X, Wu Q, Niu D, Ji X,
Feng Q, Li Z and Kakudo K: In papillary thyroid carcinoma,
expression by immunohistochemistry of BRAF V600E, PD-L1, and PD-1
is closely related. Virchows Arch. 472:779–787. 2018.PubMed/NCBI View Article : Google Scholar
|
|
116
|
Trybek T, Walczyk A, Gąsior-Perczak D,
Pałyga I, Mikina E, Kowalik A, Hińcza K, Kopczyński J, Chrapek M,
Góźdź S and Kowalska A: Impact of BRAF V600E and TERT promoter
mutations on response to therapy in papillary thyroid cancer.
Endocrinology. 160:2328–2338. 2019.PubMed/NCBI View Article : Google Scholar
|
|
117
|
Landa I and Knauf JA: Mouse models as a
tool for understanding progression in BrafV600E-driven thyroid
cancers. Endocrinol Metab (Seoul). 34:11–22. 2019.PubMed/NCBI View Article : Google Scholar
|