|
1
|
Yılmaz H, Zateri C, Kusvuran Ozkan A,
Kayalar G and Berk H: Prevalence of adolescent idiopathic scoliosis
in Turkey: An epidemiological study. Spine J. 20:947–955.
2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Kwan KYH, Koh HY, Blanke KM and Cheung
KMC: Complications following surgery for adolescent idiopathic
scoliosis over a 13-year period. Bone Joint J. 102-B:519–523.
2020.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Cognetti D, Keeny HM, Samdani AF, Pahys
JM, Hanson DS, Blanke K and Hwang SW: Neuromuscular scoliosis
complication rates from 2004 to 2015: A report from the Scoliosis
Research Society Morbidity and Mortality database. Neurosurg Focus.
43(E10)2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Patel H, Khoury H, Girgenti D, Welner S
and Yu H: Burden of Surgical Site Infections Associated with Select
Spine Operations and Involvement of Staphylococcus aureus. Surg
Infect (Larchmt). 18:461–473. 2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Casper DS, Zmistowski B, Hollern DA,
Hilibrand AS, Vaccaro AR, Schroeder GD and Kepler CK: The effect of
postoperative spinal infections on patient mortality. Spine (Phila
Pa 1976). 43:223–227. 2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Heyer JH, Cao NA, Amdur RL and Rao RR:
Postoperative complications following orthopedic spine surgery: Is
there a difference between men and women? Int J Spine Surg.
13:125–131. 2019.PubMed/NCBI View
Article : Google Scholar
|
|
7
|
Meyer AC, Eklund H, Hedström M and Modig
K: The ASA score predicts infections, cardiovascular complications,
and hospital readmissions after hip fracture-A nationwide cohort
study. Osteoporos Int. 32:2185–2192. 2021.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Buja A, Zampieron A, Cavalet S, Chiffi D,
Sandonà P, Vinelli A, Baldovin T and Baldo V: An update review on
risk factors and scales for prediction of deep sternal wound
infections. Int Wound J. 9:372–386. 2012.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Rodriguez-Merchan EC and Delgado-Martinez
AD: Risk factors for periprosthetic joint infection after primary
total knee arthroplasty. J Clin Med. 11(6128)2022.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Chung AS, Campbell D, Waldrop R and
Crandall D: metabolic syndrome and 30-day outcomes in elective
lumbar spinal fusion. Spine (Phila Pa 1976). 43:661–666.
2018.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Ding JZ, Kong C, Sun XY and Lu SB:
Perioperative complications and risk factors in degenerative lumbar
scoliosis surgery for patients older than 70 years of age. Clin
Interv Aging. 14:2195–2203. 2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
TollB J, Samdani AF, Janjua MB, Gandhi S,
Pahys JM and Hwang SW: Perioperative complications and risk factors
in neuromuscular scoliosis surgery. J Neurosurg Pediatr.
22:207–213. 2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Zhang XN, Sun XY, Hai Y, Meng XL and Wang
YS: Incidence and risk factors for multiple medical complications
in adult degenerative scoliosis long-level fusion. J Clin Neurosci.
54:14–19. 2018.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Rudic TN, Althoff AD, Kamalapathy P and
Bachmann KR: Surgical site infection after primary spinal fusion
surgery for adolescent idiopathic scoliosis: An analysis of risk
factors from a nationwide insurance database. Spine (Phila Pa
1976). 48:E101–E106. 2023.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Menger RP, Kalakoti P, Pugely AJ, Nanda A
and Sin A: Adolescent idiopathic scoliosis: Risk factors for
complications and the effect of hospital volume on outcomes.
Neurosurg Focus. 43(E3)2017.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Jammer I, Wickboldt N, Sander M, Smith A,
Schultz MJ, Pelosi P, Leva B, Rhodes A, Hoeft A, Walder B, et al:
Standards for definitions and use of outcome measures for clinical
effectiveness research in perioperative medicine: European
Perioperative Clinical Outcome (EPCO) definitions: A statement from
the ESA-ESICM joint taskforce on perioperative outcome measures.
Eur J Anaesthesiol. 32:88–105. 2015.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Peduzzi P, Concato J, Kemper E, Holford TR
and Feinstein AR: A simulation study of the number of events per
variable in logistic regression analysis. J Clin Epidemiol.
49:1373–1379. 1996.PubMed/NCBI View Article : Google Scholar
|
|
18
|
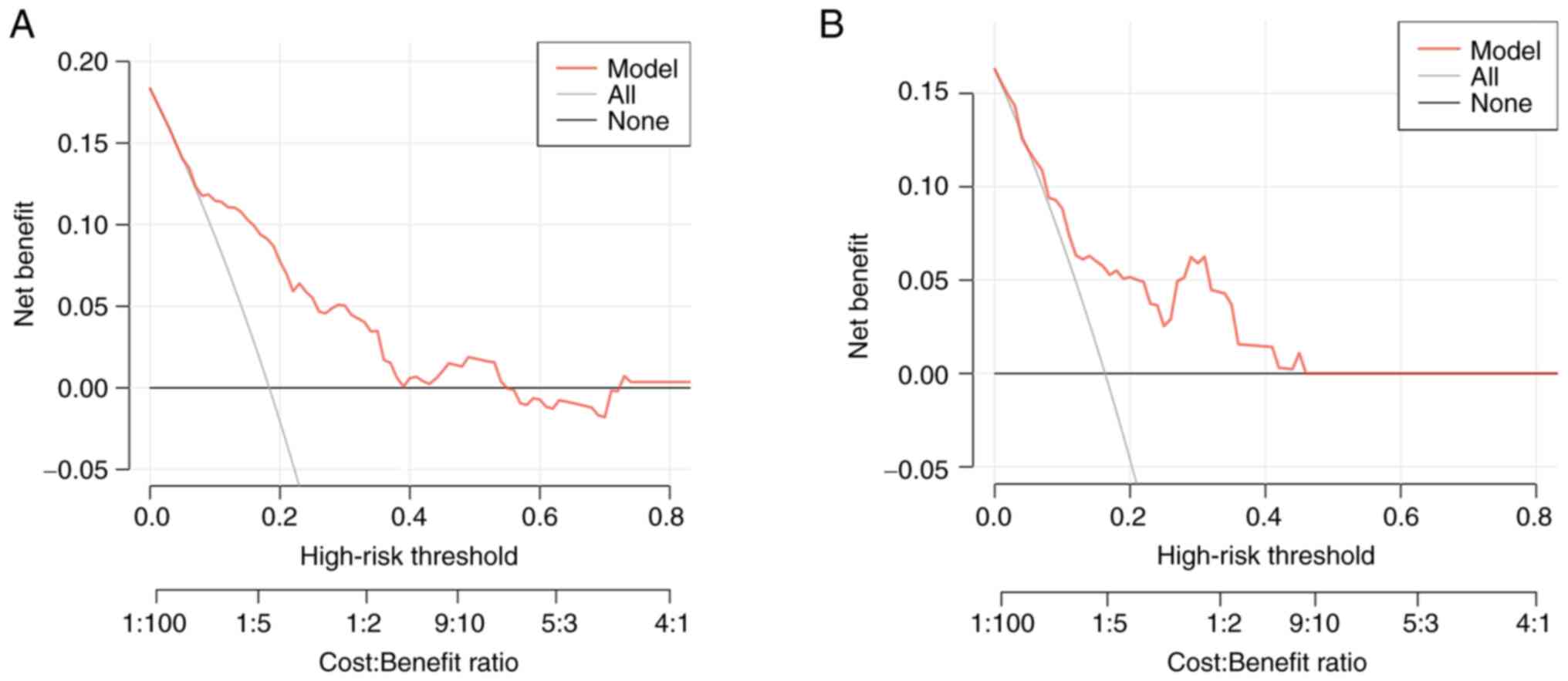
Van Calster B, Wynants L, Verbeek JFM,
Verbakel JY, Christodoulou E, Vickers AJ, Roobol MJ and Steyerberg
EW: Reporting and interpreting decision curve analysis: A guide for
investigators. Eur Urol. 74:796–804. 2018.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Desborough JP: The stress response to
trauma and surgery. Br J Anaesth. 85:109–117. 2000.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Apisarnthanarak A, Jones M, Waterman BM,
Carroll CM, Bernardi R and Fraser VJ: Risk factors for spinal
surgical-site infections in a community hospital: A case-control
study. Infect Control Hosp Epidemiol. 24:31–36. 2003.PubMed/NCBI View
Article : Google Scholar
|
|
21
|
Blanco JF, Díaz A, Melchor FR, da Casa C
and Pescador D: Risk factors for periprosthetic joint infection
after total knee arthroplasty. Arch Orthop Trauma Surg.
140:239–245. 2020.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Palestro CJ and Love C: Role of nuclear
medicine for diagnosing infection of recently implanted lower
extremity arthroplasties. Semin Nucl Med. 47:630–638.
2017.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Sigmund IK, Dudareva M, Watts D,
Morgenstern M, Athanasou NA and McNally MA: Limited diagnostic
value of serum inflammatory biomarkers in the diagnosis of
fracture-related infections. Bone Joint J. 102-B:904–911.
2020.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Colborn KL, Zhuang Y, Dyas AR, Henderson
WG, Madsen HJ, Bronsert MR, Matheny ME, Lambert-Kerzner A, Myers
QWO and Meguid RA: Development and validation of models for
detection of postoperative infections using structured electronic
health records data and machine learnin]. Surgery. 173:464–471.
2023.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Aghdassi SJS, Schröder C and Gastmeier P:
Gender-related risk factors for surgical site infections. Results
from 10 years of surveillance in Germany. Antimicrob Resist Infect
Control. 8(95)2019.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Soroceanu A, Burton DC, Oren JH, Smith JS,
Hostin R, Shaffrey CI, Akbarnia BA, Ames CP, Errico TJ, Bess S, et
al: Medical complications after adult spinal deformity surgery:
Incidence, risk factors, and clinical impact. Spine (Phila Pa
1976). 41:1718–1723. 2016.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Tse EY, Cheung WY, Ng KF and Luk KD:
Reducing perioperative blood loss and allogeneic blood transfusion
in patients undergoing major spine surgery. J Bone Joint Surg Am.
93:1268–1277. 2011.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Allegranzi B, Bischoff P, de Jonge S,
Kubilay NZ, Zayed B, Gomes SM, Abbas M, Atema JJ, Gans S, van Rijen
M, et al: New WHO recommendations on preoperative measures for
surgical site infection prevention: An evidence-based global
perspective. Lancet Infect Dis. 16:e276–e287. 2016.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Onesti MG, Carella S and Scuderi N:
Effectiveness of antimicrobial-coated sutures for the prevention of
surgical site infection: A review of the literature. Eur Rev Med
Pharmacol Sci. 22:5729–5739. 2018.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Guo Y, Song G, Sun M, Wang J and Wang Y:
Prevalence and therapies of antibiotic-resistance in staphylococcus
aureus. Front Cell Infect Microbiol. 10(107)2020.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Mizan T and Taghipour S: Medical resource
allocation planning by integrating machine learning and
optimization models. Artif Intell Med. 134(102430)2022.PubMed/NCBI View Article : Google Scholar
|
|
32
|
El Sharouni MA, Ahmed T, Varey AHR, Elias
SG, Witkamp AJ, Sigurdsson V, Suijkerbuijk KPM, van Diest PJ,
Scolyer RA, van Gils CH, et al: Development and validation of
nomograms to predict local, regional, and distant recurrence in
patients with thin (T1) melanomas. J Clin Oncol. 39:1243–1252.
2021.PubMed/NCBI View Article : Google Scholar
|