Introduction
Nonalcoholic fatty liver disease (NAFLD) is a
condition in which the liver of individuals with little or no
history of alcohol consumption has excessive fatty deposits
(1). In 2023, NAFLD affects
approximately 30% of the adult population worldwide, making it a
common chronic liver disease (2).
Nonalcoholic steatohepatitis (NASH) is a type of NAFLD
characterized by fatty liver degeneration, inflammatory cell
infiltration, and balloon-like cell degeneration; persistent
inflammation can lead to liver fibrosis (3-4). The
risk of cirrhosis and hepatocellular carcinoma rises as fibrosis
progresses, and the liver fibrosis stage of NASH is an important
prognostic factor (3-5).
A liver biopsy is frequently used to confirm NASH
diagnosis and determine the stage of liver fibrosis (6,7). A
liver biopsy is required to distinguish NASH, but the number of
patients with suspected NASH is growing, and performing the
procedure on all patients is difficult (5). Furthermore, liver biopsy is an
effected tool for diagnosing NASH. Additionally, the tissue sampled
by liver biopsy does not reflect the condition of the entire liver,
and variability in histologic characteristics between samples is a
challenge (8). Furthermore, there
is interobserver variability when evaluating sampled tissue
(9). Hence, there is an increased
demand for noninvasive alternatives to invasive liver biopsy
(10).
Biomarker testing using blood samples is known to be
less invasive. Major biomarkers include the liver enzymes aspartate
aminotransferase (AST) and alanine aminotransferase (ALT). These
are known as common liver injury markers; specifically, ALT has
been used to estimate the degree of fibrosis progression in NASH
(11). However, ALT is not a
NASH-specific biomarker because it also fluctuates in various
diseases other than NASH (12).
Furthermore, scoring systems, such as the AST to platelet ratio
index, Fib-4 index, and NAFLD fibrosis score, which assess fibrosis
by combining multiple measures, are useful in determining the
severity of fibrosis in NASH but have not been used for its
definitive diagnosis (13-15).
Furthermore, the cytokeratin 18 fragment (CK18), which has recently
gained attention as a NASH biomarker, has been shown to help
distinguish between simple fatty liver (NAFL) and NASH in patients
with NAFLD (16-17). However, CK18 has not been used for
definitive diagnosis, and issues among reagent kits of variability
and low sensitivity have been reported (17,18).
Therefore, developing a new noninvasive test for definitive NASH
diagnosis and early liver fibrosis detection in NASH is
desirable.
MicroRNAs (miRNAs) are short single-stranded RNAs
with 21-23 nucleotides. MiRNAs bind to the 3'-UTR region of target
mRNAs, inhibit mRNA translation into proteins, and regulate gene
expression (19). Recently, miRNAs
have been released from cells and are involved in intercellular
communication (20). Furthermore,
miRNAs are known to change expression in various diseases, and
their potential as biomarkers is promising (20,21).
This study focused on miRNAs to find biomarkers that can detect
NASH-induced liver fibrosis caused early on.
Materials and methods
Mice
We purchased a total of 75 male 5-week-old
C57BL/6NJcl mice (body weight, 20.6±0.7 g) from CLEA Japan. All
mice were housed in a conventional animal room with 12/12-h
light/dark cycle. Treatment began after a 1-week acclimatization
period. Mice were observed 2-3 times per day for monitoring, and
health or behavior abnormalities were not observed during the
rearing period. The NASH model group was fed a choline-deficient
high-fat (CDAHFD) supplemented with 0.1% (w/v) methionine (Research
Diets Inc., A06071302). The control group was given a commercial
standard diet called CE-2 (CLEA Japan). It was not suitable for the
purpose of this study, where we wanted to confirm even the
appearance of fibrosis, because fibrosis does not appear with a
simple high-fat diet, even after long-term feeding. In addition,
the methionine/choline-deficient diet is not suitable for long-term
rearing because of the significant weight loss of the mice and
increased risk of mortality. Therefore, this diet was used in this
study to create a NASH model mouse, which has less weight loss and
is suitable for long-term observation.
Both groups were fed and watered ad libitum,
with replacements once a week. All mice were kept under the
conditions described above for 1-12 weeks after feeding, with five
mice assigned to each week. The sample size was determined to
provide adequate statistical treatment. Sampling was done up to 12
weeks after feeding to check the progression of fibrosis. Blood
samples from five mice were collected using cardiac blood sampling
under anesthesia with the inhalation anesthetic solution isoflurane
(Pfizer) at the end of the 0-, 1-, 2-, 4-, 6-, 8-, 10-, and 12-week
after feeding. Sampling for the control and NASH groups was
conducted on the same day. Anesthesia was administered via
inhalation from a small animal anesthesia machine (Muromachi Kikai)
that was vaporized to a concentration of 4-5% and maintained at
2-3%. The cervical dislocation was used for euthanasia, and death
was determined by the cessation of respiration and heartbeat.
Under anesthesia, 0.5-1.0 ml of blood was received
from the heart, and all mice were promptly cervically dislocated to
minimize distress. For this study, the criteria for applying the
humane endpoint were symptoms of anguish (e.g., self-injury,
abnormal posture, breathing problems, squealing), long-term
abnormal appearance (e.g., diarrhea, bleeding, vulvar smears), and
rapid weight loss (>20% in a few days). No mice during this
study required a humane endpoint prior to study termination. The
start of anesthesia to the end of blood collection took <10 min
per animal. Death was confirmed by respiratory and cardiac arrest.
Blood samples were serum-separated immediately after collection.
Blood samples were then placed in a Microtainer (Becton Dickinson),
and the coagulated blood was centrifuged at 6,000 G for 3 min to
separate the serum. Livers were removed from euthanized mice. The
experiments with mice were performed twice during the study period
and we have confirmed that the data in this study are reproducible.
The Hirosaki University Ethics Committee for Animal Experiments
approved this experiment, which followed the Hirosaki University
Guidelines for Animal Experiments (Approval No. AE01-2023-004).
Tissue fixation and tissue block
preparation
Liver tissues that had been excited after perfusion
fixation were fixed with 4% (w/v) paraformaldehyde for 48 h and
paraffin-embedded blocks were prepared using a Sakura-sealed
automatic fixation and embedding device (Sakura Finetek Japan) and
Tissue-Tek TEC5 (Sakura Finetek Japan).
Hematoxylin and eosin (HE)
staining
Paraffin-embedded tissue blocks were thinly sliced
to a 4-µm thickness and attached to glass slides. We deparaffinized
tissue sections with xylene and ethanol then rinsed them with water
for 5 min. Nuclear staining was conducted in Meyer's hematoxylin
solution (Fujifilm Wako) for 1 min, followed by color removal in
warm water for 10 min. The samples were then stained with 0.5%
(w/v) eosin Y in 80% (v/v) ethanol solution (Fujifilm wako) for 10
sec, rinsed with water to remove the excess staining solution, and
fractionated with 75% (v/v) ethanol. The samples were treated with
ethanol and xylene before being sealed with Marinol (Muto Chemical)
and cover glass (Matsunami Glass).
Sirius red staining
Glass slides with paraffin-embedded sections
attached were rinsed with running water for 5 min following
deparaffinization and hydrophilic treatment. Sirius red staining
solution was created by combining 100 ml of saturated picric acid
solution with 3 ml of 1% (w/v) Sirius red solution (Fujifilm Wako).
The glass slides were rinsed under running water for 5 min after
being stained with Sirius red staining solution for 10 min to
remove the color. The slides were then dehydrated using ethanol,
permeated with xylene, and sealed with Marinol (Muto Chemical) and
cover glass (Matsunami Glass).
Immunohistochemical staining
Glass slides with paraffin sections attached were
rinsed with water for 5 min following deparaffinization and
hydrophilic treatment. Glass slides were treated with 3% (v/v)
H2O2 for 5 min before being rinsed in water
for 5 min to deactivate endogenous peroxidase. Incubation was made
in citrate buffer (pH of 6.0) at 115˚C for 5 min to activate
antigen. Glass slides were then washed with Tris-buffered saline
(TBS) buffer (25 mM of Tris-HCl and 150 mM of NaCl, pH of 7.2) for
5 min before incubating with a drop of blocking solution [5% (v/v)
sheep serum in TBS buffer] on glass slides for 30 min at room
temperature. Anti-α-smooth muscle actin (α-SMA) rabbit monoclonal
antibody (Cell Signaling Technologies, cat. 19245S) was diluted
500-fold in blocking solution, applied to glass slides, and
incubated at room temperature for 60 min. The liquid on the glass
slides was removed, washed 3 times with TBS buffer for 5 min, and
then incubated dropwise with EnVision + System-HRP-labeled polymer
anti-rabbit (Dako, cat. K4003) for 60 min at room temperature. The
liquid on the glass slides was removed, washed three times with TBS
buffer for 5 min, and colored with 3,3'-diaminobenzidine
tetrahydrochloride solution (Sigma-Aldrich). Glass slides were
washed with water, nuclear stained with Meyer's hematoxylin
solution (Muto Chemical) for 1 min, and the color was removed by
washing with warm water for 10 min. They were dehydrated with
ethanol, permeated with xylene, and sealed with Marinol (Muto
Chemical) and covered glass.
Pathological evaluation
A scoring system has been used to assess the
histology of NAFLD/NASH in humans (22). Matsumoto et al (23) reported a histological evaluation of
NAFLD/NASH in mice fed the same CDAHFD diet as us, similar to the
human scoring system. In this study, we also used the histological
examination of the liver described by Matsumoto et al
(23).
Biochemical tests
Serum AST and ALT were determined by pocH-100iV Diff
(Sysmex) at the Hirosaki University Laboratory Animal Facility.
RNA extraction
Total RNA was extracted from livers and 200 µl of
serum using ISOGEN II (Nippon Gene) as per the manufacturer's
instructions. The total RNA concentration in livers was measured
using a NanoDrop spectrophotometer (NanoDrop Technologies). All
total RNA from livers had 260/280 nm absorbance ratios ranging from
1.8-2.0. Ethachinmate (Nippon Gene) was used to precipitate total
RNA from serum. A Quant-iT RiboGreen RNA Reagent and Kit (Thermo
Fisher Scientific, Inc.) was used to determine the total RNA
concentration from serum.
miRNA microarray analysis
The miRNA Complete Labeling and Hyb kit was used to
label miRNAs in 2.5 ng of serum total RNA and 100 ng of liver total
RNA. The microRNA Spike In Kit (cat. no. 5190-1934; Agilent
Technologies, Inc.) was used to conduct quality checks on the
microarray experiments. The RNA samples were labeled with Cyanine 3
(Cy3) fluorescent dye per the manufacturer's instructions. The
Cy3-labeled miRNA was incubated for hybridization with miRNA
microarray slides (SurePrint G3 Mouse 8x60-K miRNA microarray
slides (cat. no. G4872A; Agilent Technologies, Inc.) at 55˚C and 20
rpm for 20 h. Cy3 fluorescence signals on glass slides were
detected using a SureScan microarray scanner (cat. no. G4900DA;
Agilent Technologies, Inc.), and fluorescence quantification was
done with Agilent Feature Extraction 12.0 (Agilent Technologies,
Inc.). As a method of evaluating Spike-In, Agilent Feature
Extraction 12.0 was used to ensure that the calculated values of
LabelingSpike-InSignal and HybSpike-InSignal were both >2.5. A
90% shift normalization was conducted using the obtained data, and
GeneSpring GX14.5 software was used for expression analysis. These
data were registered with the Gene Expression Omnibus (https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE252035).
Prediction of miRNA target genes
OmicsNet (https://www.omicsnet.ca/) was used to predict the
target genes and functions of miRNAs whose gene expression in the
liver is affected by NASH.
Statistical analysis
The Shapiro-Wilk test confirmed that each population
exhibited a normal distribution. An F test was also performed to
confirm the variance of the two groups, and all data were confirmed
to be equal variance. Values were expressed as mean ±2 standard
deviation. Each sample size was determined to be sufficient at n=5
because the standard deviation was sufficiently small. Significant
differences in liver weight, AST, and ALT levels between the
control and NASH groups were determined using Student's t-test.
P-values of <0.05 indicate significant differences and are
marked with an asterisk in each graph.
Results
Changes in biochemical components and
liver tissue structure in NASH mice
We showed the changes in body weight of mice fed the
Control or CDAHDF diet (Fig. SI).
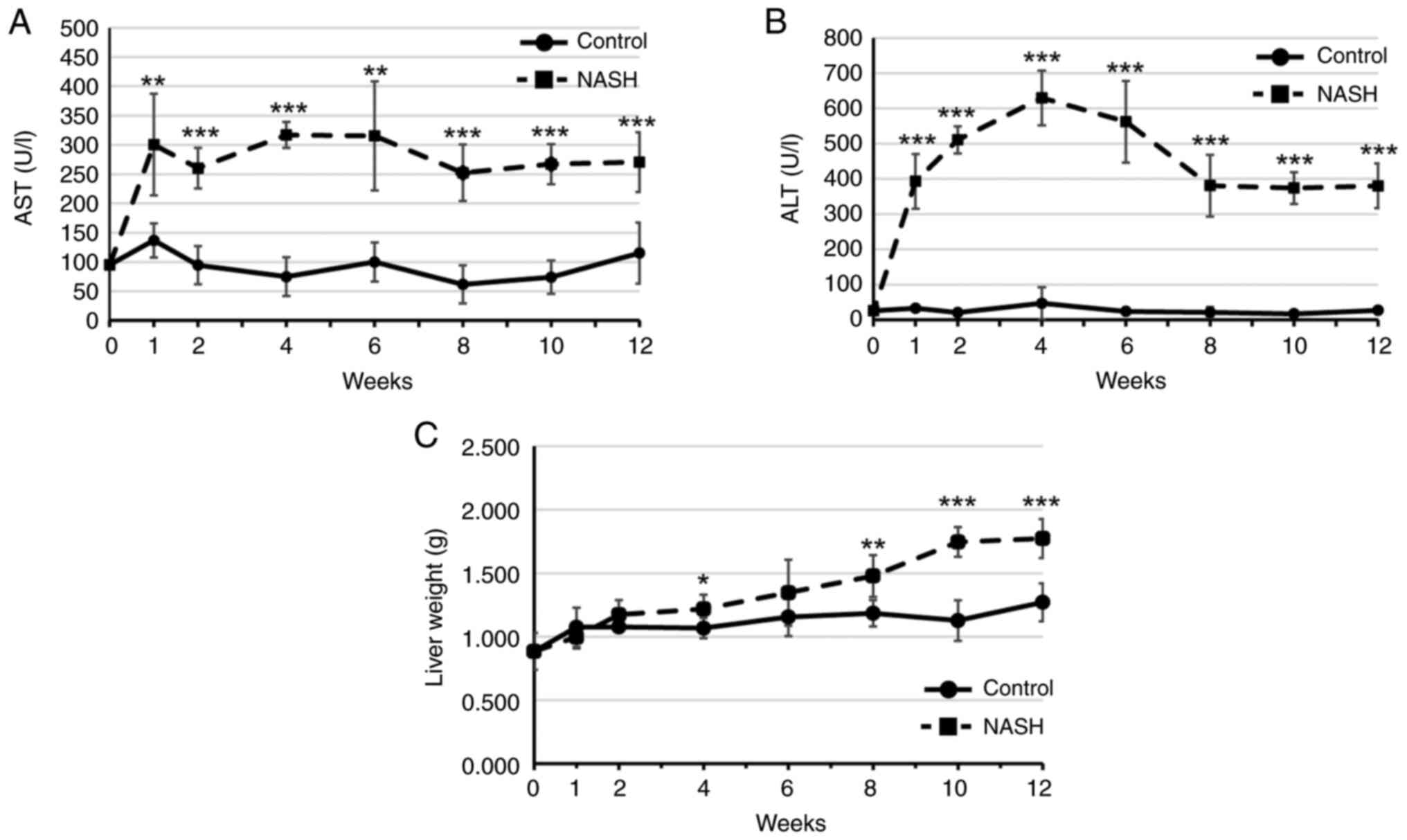
Serum AST and ALT levels, which are markers of liver injury, of the
control and NASH groups were measured from 0 to 12 weeks after
starting a high-fat diet (Fig. 1A,
B). Both AST and ALT levels in the
NASH group were significantly higher than those in the control
group after 1 week of feeding a high-fat diet. Liver weights were
then measured from 0 to 12 weeks after the beginning of the
high-fat diet (Fig. 1C). The NASH
group had a higher liver weight over time, with significant
increases at 4 weeks and 8-12 weeks of feeding compared to the
control group.
Histological changes in the livers of
NASH-induced mice
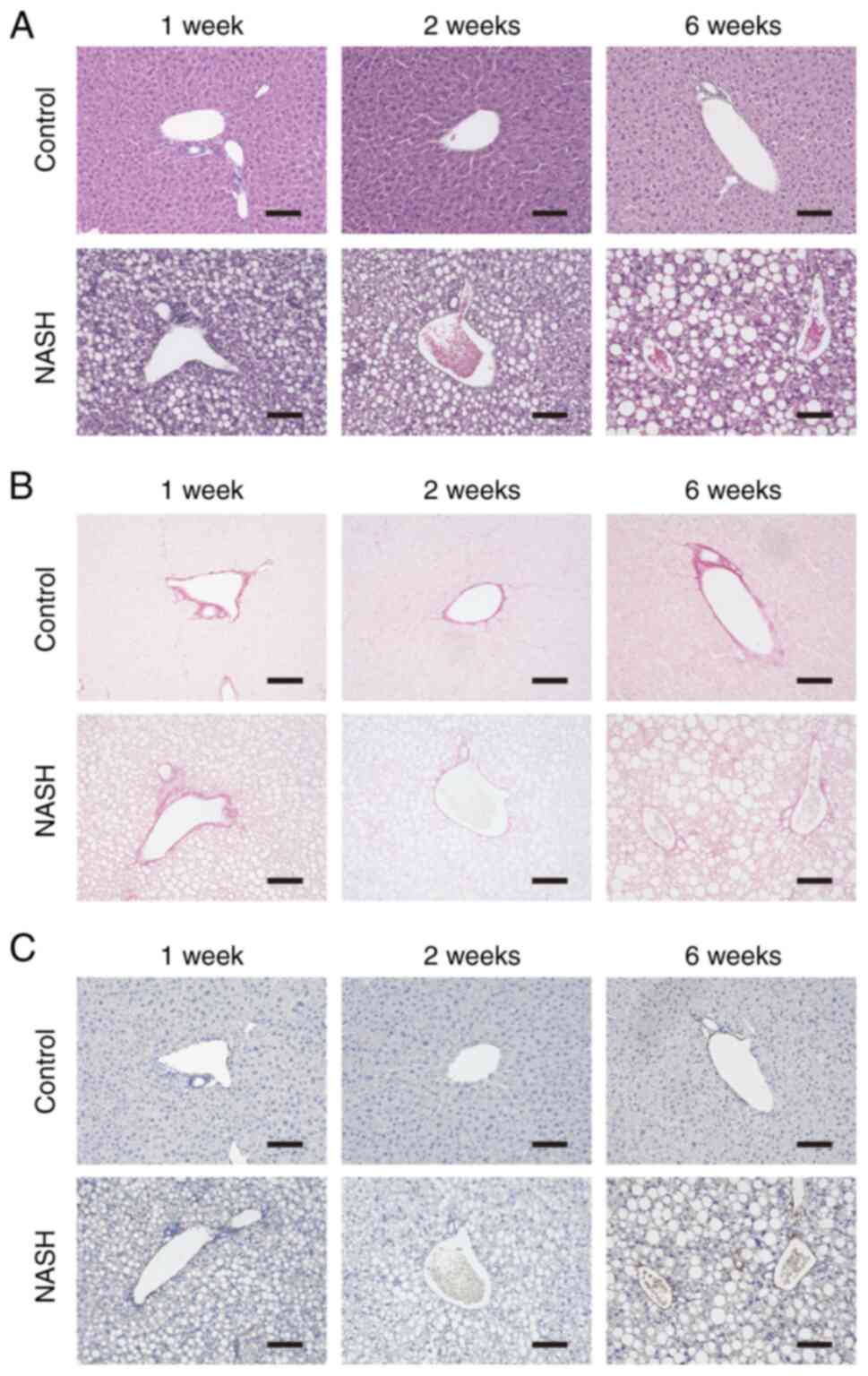
HE, Sirius red, and α-SMA immunohistochemical
staining were used to confirm histopathological changes in the
liver of NASH-induced mice (Fig.
2). The stained images in the control group consistently showed
normal liver histology up to 12 weeks of feeding, regardless of
staining method. HE staining revealed fatty degeneration,
balloon-like degeneration, and inflammatory cell infiltration
throughout the liver at 2 weeks of feeding in the NASH group, with
similar findings at 6 weeks. Sirius red staining revealed clear
fibrosis at 6 weeks. Further, α-SMA immunohistochemical staining
revealed numerous positive cells at 6 weeks of feeding. The
observation was continued for 12 weeks, but there were no
significant changes compared to the tissue at 6 weeks.
The above staining results were used to calculate
scores for hepatic steatosis, inflammation, ballooning-like
degeneration, and hepatic fibrosis (Table I). At 1 week of feeding, the score
was evaluated as follows: Steatosis grade 2, Inflammation grade 1,
Ballooning grade 0, and Fibrosis grade 0. At 2 weeks of feeding,
the animals were classified as having Steatosis grade 3,
Inflammation grade 2, Ballooning grade 2, and Fibrosis grade 0. Six
weeks of feeding were assessed as Steatosis grade 3, Inflammation
grade 3, Ballooning grade 3, and Fibrosis grade 2. These
pathological analyses suggest that mouse livers at 2-6 weeks of
CDAHDF feeding are in the early stages of fibrosis due to NASH.
 | Table IHistological examination of the
NAFLD/NASH liver in mice. |
Table I
Histological examination of the
NAFLD/NASH liver in mice.
| Histopathological
changes | 1 week | 2 weeks | 6 weeks |
|---|
| Steatosis | Grade2 | Grade3 | Grade3 |
| Inflammation | Grade1 | Grade2 | Grade3 |
| Ballooning | Grade0 | Grade2 | Grade3 |
| Fibrosis | Grade0 | Grade0 | Grade2 |
Changes in miRNA expression in the
liver of NASH mice model
To investigate the changes in miRNA expression
caused by NASH development, miRNA microarray analysis was performed
on livers from the NASH mice model. We investigated miRNA
expression in the liver of NASH model mice at 2 weeks of feeding, a
NASH state in which fibrosis is not readily visible, based on
stained images of liver tissue. Table
II lists the miRNAs with an expression difference of more than
1.5-fold compared to the control group. Nine miRNAs were
upregulated, while 47 miRNAs were downregulated.
 | Table IIDifferences in the expression levels
of miRNAs in the liver of NASH model mice fed for 2 weeks. |
Table II
Differences in the expression levels
of miRNAs in the liver of NASH model mice fed for 2 weeks.
| miRNA name | Accession no. | Fold-change | Up/down |
|---|
| miR-1224-5p | MIMAT0005460 | 1.75 | Up |
| miR-15b-5p | MIMAT0000124 | 1.50 | Up |
| miR-223-3p | MIMAT0000665 | 2.43 | Up |
| miR-342-3p | MIMAT0000590 | 4.44 | Up |
| miR-34a-5p | MIMAT0000542 | 6.03 | Up |
| miR-3960 | MIMAT0019336 | 3.86 | Up |
| miR-5126 | MIMAT0020637 | 2.90 | Up |
| miR-7118-5p | MIMAT0028133 | 9.94 | Up |
| miR-8110 | MIMAT0031416 | 4.91 | Up |
| let-7a-5p | MIMAT0000521 | -1.61 | Down |
| let-7b-5p | MIMAT0000522 | -1.54 | Down |
| let-7c-5p | MIMAT0000523 | -1.54 | Down |
| let-7f-5p | MIMAT0000525 | -2.52 | Down |
| let-7g-5p | MIMAT0000121 | -2.85 | Down |
| miR-101a-3p | MIMAT0000133 | -4.63 | Down |
| miR-101c | MIMAT0019349 | -5.55 | Down |
| miR-103-3p | MIMAT0000546 | -1.62 | Down |
| miR-107-3p | MIMAT0000647 | -1.82 | Down |
| miR-10a-5p | MIMAT0000648 | -1.84 | Down |
| miR-122-3p | MIMAT0017005 | -5.11 | Down |
| miR-122-5p | MIMAT0000246 | -2.87 | Down |
| miR-126a-3p | MIMAT0000138 | -2.19 | Down |
| miR-130a-3p | MIMAT0000141 | -1.59 | Down |
| miR-148a-3p | MIMAT0000516 | -2.37 | Down |
| miR-15a-5p | MIMAT0000526 | -2.50 | Down |
| miR-16-5p | MIMAT0000527 | -1.71 | Down |
| miR-192-5p | MIMAT0000517 | -3.87 | Down |
| miR-193a-3p | MIMAT0000223 | -2.60 | Down |
| miR-194-5p | MIMAT0000224 | -3.07 | Down |
| miR-19a-3p | MIMAT0000651 | -3.79 | Down |
| miR-19b-3p | MIMAT0000513 | -3.87 | Down |
| miR-20a-5p | MIMAT0000529 | -2.02 | Down |
| miR-20b-5p | MIMAT0003187 | -1.93 | Down |
| miR-21a-5p | MIMAT0000530 | -1.82 | Down |
| miR-22-3p | MIMAT0000531 | -2.34 | Down |
| miR-23b-3p | MIMAT0000125 | -1.92 | Down |
| miR-26a-5p | MIMAT0000533 | -2.09 | Down |
| miR-26b-5p | MIMAT0000534 | -3.25 | Down |
| miR-27b-3p | MIMAT0000126 | -1.93 | Down |
| miR-29a-3p | MIMAT0000535 | -1.74 | Down |
| miR-29b-3p | MIMAT0000127 | -2.28 | Down |
| miR-29c-3p | MIMAT0000536 | -2.59 | Down |
| miR-30a-3p | MIMAT0000129 | -2.37 | Down |
| miR-30a-5p | MIMAT0000128 | -2.40 | Down |
| miR-30b-5p | MIMAT0000130 | -2.83 | Down |
| miR-30c-5p | MIMAT0000514 | -2.51 | Down |
| miR-30d-5p | MIMAT0000515 | -1.68 | Down |
| miR-30e-5p | MIMAT0000248 | -2.93 | Down |
| miR-365-3p | MIMAT0000711 | -2.35 | Down |
| miR-3963 | MIMAT0019341 | -2.83 | Down |
| miR-3968 | MIMAT0019352 | -3.15 | Down |
| miR-451a | MIMAT0001632 | -3.66 | Down |
| miR-5100 | MIMAT0020607 | -3.12 | Down |
| miR-6366 | MIMAT0025110 | -1.66 | Down |
| miR-6368 | MIMAT0025112 | -1.52 | Down |
| miR-99a-5p | MIMAT0000131 | -1.62 | Down |
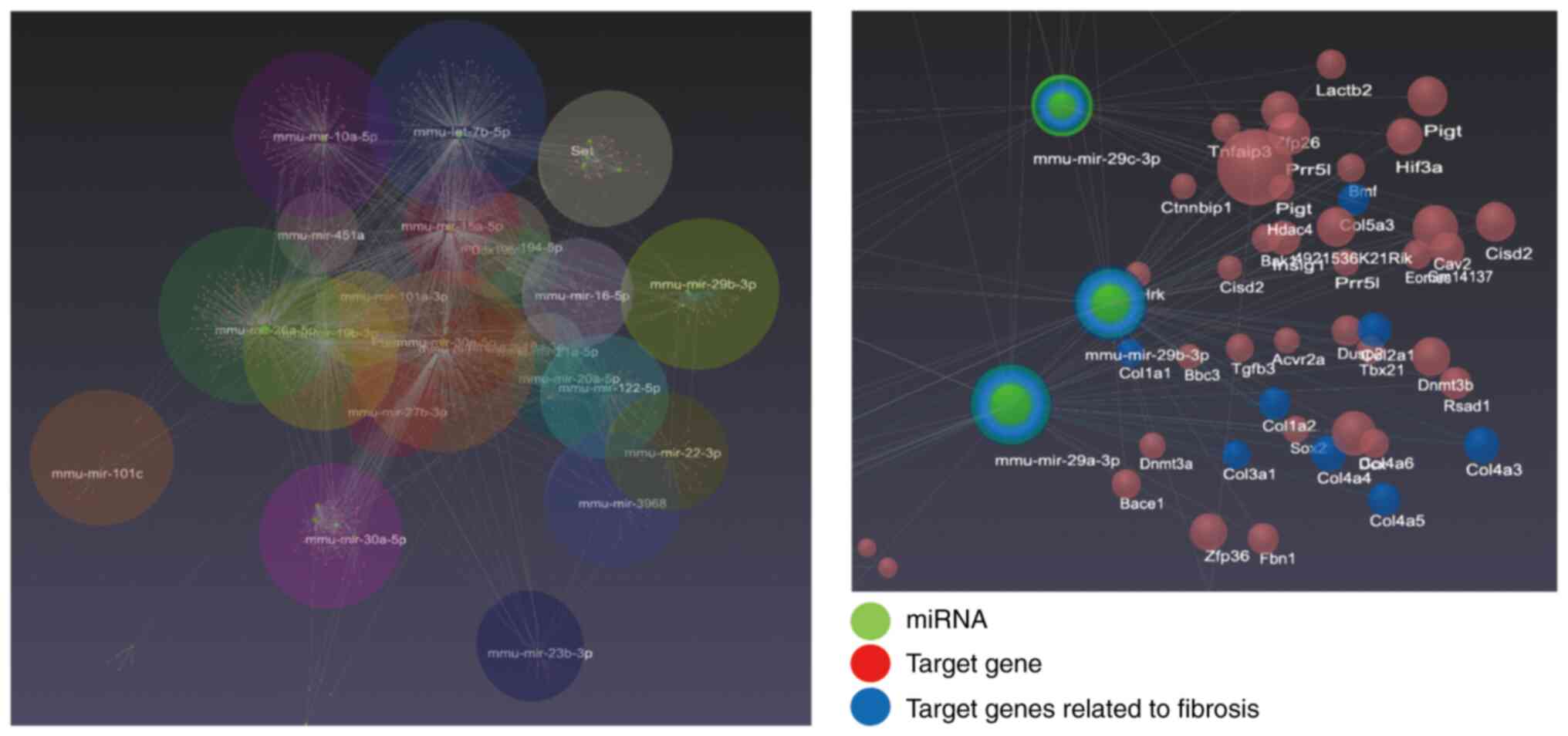
The 47 miRNAs predicted to be downregulated by miRNA
microarray analysis in the liver of the NASH group were analyzed
using OmicsNet. The target genes of these miRNAs and their
associated functions were linked by lines. In the enlarged figure,
green circles indicated miRNAs, red circles indicated target genes,
and blue circles indicated target genes involved in fibrosis. The
relationship between miRNAs and target genes associated with
fibrosis predicted a link between the miR-29-3p family and collagen
genes in the 47 miRNAs (Fig. 3). A
search of the OmicsNet Reactome database for fibrosis-related
functions revealed ‘collagen formation’ and ‘collagen biosynthesis
and modifying enzymes’ (Table
SI). Collagen genes play roles in both of these functions, and
the miR-29 family was identified as miRNAs that regulate collagen
genes.
Changes in miRNA expression in the
serum of NASH mice model
We performed miRNA microarray analysis in the serum
of the NASH mice model at 2 weeks of feeding. Table III shows the miRNAs that had a
more than 1.5-fold difference in expression between the NASH and
control groups. Twenty-one miRNAs were upregulated, while seven
were downregulated. Among the miR-29 family, miR29a-3p and
miR-29c-3p, which were linked to collagen genes by OmicsNet
results, were upregulated in NASH model mouse serum.
 | Table IIIDifferences in the expression levels
of miRNAs in the serum of NASH model mice fed for 2 weeks. |
Table III
Differences in the expression levels
of miRNAs in the serum of NASH model mice fed for 2 weeks.
| miRNA name | Accession no. | Fold-change | Up/down |
|---|
| let-7c-5p | MIMAT0000523 | 1.59 | Up |
| let-7i-5p | MIMAT0000122 | 1.59 | Up |
| miR-122-5p | MIMAT0000246 | 26.58 | Up |
| miR-130a-3p | MIMAT0000141 | 1.73 | Up |
| miR-148a-3p | MIMAT0000516 | 5.00 | Up |
| miR-16-5p | MIMAT0000527 | 1.75 | Up |
| miR-192-5p | MIMAT0000517 | 8.60 | Up |
| miR-21a-5p | MIMAT0000530 | 2.85 | Up |
| miR-22-3p | MIMAT0000531 | 2.11 | Up |
| miR-27a-3p | MIMAT0000537 | 1.56 | Up |
| miR-2861 | MIMAT0013803 | 1.79 | Up |
| miR-29a-3p | MIMAT0000535 | 1.55 | Up |
| miR-29c-3p | MIMAT0000536 | 2.22 | Up |
| miR-30a-5p | MIMAT0000128 | 1.79 | Up |
| miR-342-3p | MIMAT0000590 | 3.03 | Up |
| miR-3473f | MIMAT0031390 | 1.53 | Up |
| miR-34a-5p | MIMAT0000542 | 5.28 | Up |
| miR-3960 | MIMAT0019336 | 2.36 | Up |
| miR-6931-5p | MIMAT0027762 | 2.79 | Up |
| miR-7118-5p | MIMAT0028133 | 1.54 | Up |
| miR-8110 | MIMAT0031416 | 1.58 | Up |
| miR-133a-3p | MIMAT0000145 | -3.03 | Down |
| miR-133b-3p | MIMAT0000769 | -2.97 | Down |
| miR-140-3p | MIMAT0000152 | -1.97 | Down |
| miR-1897-5p | MIMAT0007864 | -1.69 | Down |
| miR-486a-5p | MIMAT0003130 | -2.54 | Down |
| miR-6366 | MIMAT0025110 | -1.86 | Down |
| miR-7047-5p | MIMAT0027998 | -2.84 | Down |
Discussion
The current study discovered that microarray
analysis in a NASH mice model at an early fibrosis the appeared
found a link between NASH-induced liver fibrosis and miR-29
(miR-29a-3p and miR-29c-3p). Expression of these miRNAs was reduced
in the livers of NASH mice fed a high-fat diet for 2 weeks but
increased in serum, suggesting that these miRNAs were released into
the blood from the NASH-induced livers.
MiR-29 contains miR-29a, miR-29b, and miR-29c, all
of which have different sequences. MiR-29a and miR-29c are encoded
on distinct chromosomes in humans and mice, respectively. MiR-29
regulates gene expression, specifically cellular gene expression
profiles and protein synthesis. The miR-29 family is important in a
variety of biological processes and has been studied concerning
diseases and cancers. Previous research has shown that the miR-29
family regulates gene expression in fibrosis (24), neurodegenerative diseases (25), and breast cancer (26). In particular, the miR-29 family has
recently received attention for its crucial role in the process of
multiorgan fibrosis (24). MiR-29
binds to the 3'-UTR of collagen genes, inhibiting collagen protein
expression. Wang et al (27) found that reduced miR-29 expression
by TGF-β/SMAD signaling in vascular smooth muscle cells promotes
collagen synthesis. Ezhilarasan et al (28) recently discovered that miR-29 plays
a crucial role in liver fibrosis by regulating collagen gene
expression in astrocytes in the liver. Matsumoto et al
(29) discovered that miR-29a
suppressed human liver astrocyte activation and reduced liver
fibrosis. Interestingly, Lin et al (30) found that miR-29 overexpression
suppresses collagen genes, reducing liver fibrosis and inhibiting
hepatocyte lipogenesis by lowing PPARγ levels. This suggests that
miR-29 not only suppresses liver fibrosis via collagen regulation
but also controls NAFLD development. Our miRNA microarray results
confirmed a reduction in miR-29 in NASH livers (Table II). Analysis in conjunction with
immunohistological analysis of the liver showed a decrease in
miR-29 expression in the liver after 2 weeks of consuming a
high-fat diet, a stage before α-SMA positivity.
This study found that serum miRNA microarray
analysis of mice fed a high-fat diet showed increased serum
miR-29a-3p and miR-29c-3p expression after 2 weeks of NASH
induction (Table III). Several
studies have identified miR-29 as one of the microRNAs that are
upregulated in serum in NASH/NAFLD and liver fibrosis (31-34).
Our findings support that point. Conversely, Jampoka et al
(35) found that miR-29a levels
were lower in patient serum with advanced fibrosis, indicating s
significant difference in serum miR-29a levels in the advanced
stage of liver fibrosis. Understanding of the behavior changes of
serum miR-29 during the progression of NASH/NAFLD-induced liver
fibrosis remained limited although miR-29 has been linked to
various types of fibrosis. Therefore, further study of serum miR-29
is warranted in the future.
Some of the miRNAs in Tables II and III identified in this study include
those previously reported by other researchers. The miRNA
expression changes observed in this study are likely to be closely
associated with liver fibrosis. However, many other miRNAs are also
altered in expression at the same time, suggesting that fibrosis is
regulated by a complex network of miRNAs and cytokines other than
miR-29, which are also associated with fibrosis. For example,
TGF-β/Smad has been detected in Table
SI as a signal related to fibrosis other than collagen, and
miR-122-5p is predicted to be a miRNA associated with this pathway.
miR-122-5p has been reported to be associated with the TGF-β
signaling pathway in liver fibrosis (36,37).
On the other hand, TNF-α is known to be another molecule involved
in liver fibrosis besides miRNAs, which induces liver fibrosis by
causing activation of hepatic astrocytes (38). Therefore, a comprehensive
interpretation including molecules other than miRNAs will be
required to fully understand the mechanism of fibrosis
development.
The clinical significance of this study is that it
may be possible to detect fibrosis in patients with suspected NASH
without a liver biopsy, and that measurement of miR-29 may aid in
the diagnosis of early fibrosis. While the treatment of NASH
generally involves improvement of the underlying disease, exercise,
and diet, this study suggests a role for miR-29 in inhibiting
fibrosis, which may allow miR-29 to be used as a treatment for
NASH. Replenishing the liver with miR-29 as a new treatment may
improve or inhibit the progression of liver fibrosis.
In this study we identified miR-29 as an early
marker of NASH liver fibrosis in mice. Although miRNAs are highly
conserved between humans and mice, the dynamics of miRNAs in blood
may differ in human NASH versus mice. A previous study found that
miR-29 levels are elevated in NAFLD/NASH serum in humans (34), but the blood dynamics of miR-29 in
patients with NASH have been reported only in a few cases and will
need to be investigated in more detail in the future.
In humans, however, NAFLD/NASH is frequently linked
to underlying conditions such as obesity, hypertension,
dyslipidemia, and diabetes (39,40).
This study used mice without underlying diseases such as diabetes.
In this study, miR-29 was increased in the blood when mice without
underlying disease were used in the early stages of fibrosis.
However, the blood miR-29 kinetics in mice with underlying disease
are not clear. Also, the relationship between the underlying
disease and miR-29 is not clear at this time. The type of fat in
the diet used for feeding may also affect the experimental results.
Therefore, it is necessary to analyze the changes in miR-29
expression in mouse models with underlying diseases, such as
diabetes, in the future.
Also, although we used CDAHDF to rapidly induce NASH
in this study, there are several known diets of laboratory animals
that induce NASH, each with different fat components and other
nutrients in the diet. It is possible that the type of fat that
accumulates in the liver may differ depending on the diet used.
Therefore, it is necessary to understand the differences in the
types of fat that accumulate in the liver with different
NASH-inducing diets used and to verify in the future which diets
are more similar to the fat components of the human NASH
condition.
Supplementary Material
Body weight change in mice. Body
weight changes in mice fed CE-2 (Control) and mice fed a high-fat
diet (CDAHFD) (NASH) were measured up to 12 weeks (each n=5). The
data are expressed as means ± 2 standard deviations.
Analysis results using Reactome
database.
Acknowledgements
Not applicable.
Funding
Funding: The present study was supported in part by The JSPS
KAKENHI (grant nos. 21H04844 and 20K21692).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request. The datasets generated and/or analyzed during the current
study are available in the Gene Expression Omnibus repository
(https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE252035).
Authors' contributions
KM and MC were major contributors in performing the
experiments and writing the manuscript. YO, CT, MH, YK, and MO
helped conduct the experiments. All authors read and approved the
final manuscript. KM and MC confirm the authenticity of all the raw
data.
Ethics approval and consent to
participate
All experiments were performed following The
Guideline for Animal Experimentation of Hirosaki University. The
Animal Research Committee of Hirosaki University (approval no.
AE01-2023-004) approved and monitored the procedures.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Hashimoto E, Taniai M and Tokushige K:
Characteristics and diagnosis of NAFLD/NASH. J Gastroenterol
Hepatol. 28:64–70. 2013.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Younossi ZM, Golabi P, Paik JM, Henry A,
Van Dongen C and Henry L: The global epidemiology of nonalcoholic
fatty liver disease (NAFLD) and nonalcoholic steatohepatitis
(NASH): A systematic review. Hepatology. 77:1335–1347.
2023.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Parthasarathy G, Revelo X and Malhi H:
Pathogenesis of nonalcoholic steatohepatitis: An overview. Hepatol
Commun. 4:478–492. 2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Fraile JM, Palliyil S, Barelle C, Porter
AJ and Kovaleva M: Non-alcoholic steatohepatitis (NASH)-A review of
a crowded clinical landscape, driven by a complex disease. Drug Des
Dev Ther. 15:3997–4009. 2021.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Sanyal AJ, Van Natta ML, Clark J,
Neuschwander-Tetri BA, Diehl A, Dasarathy S, Loomba R, Chalasani N,
Kowdley K, Hameed B, et al: Prospective study of outcomes in adults
with nonalcoholic fatty liver disease. N Engl J Med. 385:1559–1569.
2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Schuppan D, Surabattula R and Wang XY:
Determinants of fibrosis progression and regression in NASH. J
Hepatol. 68:238–250. 2018.PubMed/NCBI View Article : Google Scholar
|
|
7
|
European Association for the Study of the
Liver. Electronic address: simpleeasloffice@easloffice.eu;
Clinical Practice Guideline Panel, Chair:; EASL Governing Board
representative:; and Panel members. EASL clinical practice
guidelines on non-invasive tests for evaluation of liver disease
severity and prognosis-2021 update. J Hepatol. 75:659–689.
2021.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Ratziu V, Charlotte F, Heurtier A, Gombert
S, Giral P, Bruckert E, Grimaldi A, Capron F and Poynard T: LIDO
study group. Sampling variability of liver biopsy in nonalcoholic
fatty liver disease. Gastroenterology. 128:1898–1906.
2005.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Merriman RB, Ferrell LD, Patti MG, Weston
SR, Pabst MS, Aouizerat BE and Bass NM: Correlation of paired liver
biopsies in morbidly obese patients with suspected nonalcoholic
fatty liver disease. Hepatology. 44:874–880. 2006.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Ajmera V and Loomba R: Imaging biomarkers
of NAFLD, NASH, and fibrosis. Mol Metab. 50(101167)2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Seko Y, Sumida Y, Tanaka S, Mori K,
Taketani H, Ishiba H, Hara T, Okajima A, Yamaguchi K, Moriguchi M,
et al: Serum alanine aminotransferase predicts the histological
course of non-alcoholic steatohepatitis in Japanese patients.
Hepatol Res. 45:E53–E61. 2015.PubMed/NCBI View Article : Google Scholar
|
|
12
|
McGill MR: The past and present of serum
aminotransferases and the future of liver injury biomarkers. Excli
J. 15:817–828. 2016.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Kruger FC, Daniels CR, Kidd M, Swart G,
Brundyn K, van Rensburg C and Kotze M: APRI: A simple bedside
marker for advanced fibrosis that can avoid liver biopsy in
patients with NAFLD/NASH. S Afr Med J. 101:477–480. 2011.PubMed/NCBI
|
|
14
|
Shah AG, Lydecker A, Murray K, Tetri BN,
Contos MJ and Sanyal AJ: Nash Clinical Research Network. Comparison
of noninvasive markers of fibrosis in patients with nonalcoholic
fatty liver disease. Clin Gastroenterol Hepatol. 7:1104–1112.
2009.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Angulo P, Hui JM, Marchesini G, Bugianesi
E, George J, Farrell GC, Enders F, Saksena S, Burt AD, Bida JP, et
al: The NAFLD fibrosis score: A noninvasive system that identifies
liver fibrosis in patients with NAFLD. Hepatology. 45:846–854.
2007.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Wieckowska A, Zein NN, Yerian LM, Lopez
AR, McCullough AJ and Feldstein AE: In vivo assessment of liver
cell apoptosis as a novel biomarker of disease severity in
nonalcoholic fatty liver disease. Hepatology. 44:27–33.
2006.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Pimentel CF, Jiang ZG, Otsubo T,
Feldbrügge L, Challies TL, Nasser I, Robson S, Afdhal N and Lai M:
Poor inter-test reliability between CK18 kits as a biomarker of
NASH. Dig Dis Sci. 61:905–912. 2016.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Cusi K, Chang Z, Harrison S, Lomonaco R,
Bril F, Orsak B, Ortiz-Lopez C, Hecht J, Feldstein AE, Webb A, et
al: Limited value of plasma cytokeratin-18 as a biomarker for NASH
and fibrosis in patients with non-alcoholic fatty liver disease. J
Hepatol. 60:167–174. 2014.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Felekkis K, Touvana E, Stefanou Ch and
Deltas C: MicroRNAs: A newly described class of encoded molecules
that play a role in health and disease. Hippokratia. 14:236–240.
2010.PubMed/NCBI
|
|
20
|
Saliminejad K, Khorshid HR, Fard SS and
Ghaffari SH: An overview of microRNAs: Biology, functions,
therapeutics, and analysis methods. J Cell Physiol. 234:5451–5465.
2019.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Yu X, Odenthal M and Fries JW: Exosomes as
miRNA carriers: Formation-function-future. Int J Mol Sci.
17(2028)2016.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Kleiner DE, Brunt EM, Van Natta M, Behling
C, Contos MJ, Cummings OW, Ferrell LD, Liu YC, Torbenson MS,
Unalp-Arida A, et al: Design and validation of a histological
scoring system for nonalcoholic fatty liver disease. Hepatology.
41:1313–1321. 2005.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Matsumoto M, Hada N, Sakamaki Y, Uno A,
Shiga T, Tanaka C, Ito T, Katsume A and Sudoh M: An improved mouse
model that rapidly develops fibrosis in non-alcoholic
steatohepatitis. Int J Exp Pathol. 94:93–103. 2013.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Wang M, Huo Z, He X, Liu F, Liang J, Wu L
and Yang D: The role of MiR-29 in the mechanism of fibrosis. Mini
Rev Med Chem. 23:1846–1858. 2023.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Ebada MA, Mostafa A, Gadallah AHA, Alkanj
S, Alghamdi BS, Ashraf GM, Abuzenadah AM, Alserihi RF, Wadaa-Allah
A and Salama M: Potential regulation of miRNA-29 and miRNA-9 by
estrogens in neurodegenerative disorders: An insightful
perspective. Brain Sci. 13(243)2023.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Amirian M, Jafari-Nozad AM, Darroudi M,
Farkhondeh T and Samarghandian S: Overview of the miR-29 family
members' function in breast cancer. Int J Biol Macromol.
230(123280)2023.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Wang T, Li Y, Chen J, Xie L and Xiao T:
TGF-β1/Smad3 signaling promotes collagen synthesis in pulmonary
artery smooth muscle by down-regulating miR-29b. Int J Clin Exp
Pathol. 11:5592–5601. 2018.PubMed/NCBI
|
|
28
|
Ezhilarasan D: MicroRNA interplay between
hepatic stellate cell quiescence and activation. Eur J Pharmacol.
885(173507)2020.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Matsumoto Y, Itami S, Kuroda M, Yoshizato
K, Kawada N and Murakami Y: MiR-29a assists in preventing the
activation of human stellate cells and promotes recovery from liver
fibrosis in mice. Mol Ther. 24:1848–1859. 2016.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Lin HY, Wang FS, Yang YL and Huang YH:
MicroRNA-29a suppresses CD36 to ameliorate high fat diet-induced
steatohepatitis and liver fibrosis in mice. Cells.
8(1298)2019.PubMed/NCBI View Article : Google Scholar
|
|
31
|
López-Riera M, Conde I, Quintas G, Pedrola
L, Zaragoza Á, Perez-Rojas J, Salcedo M, Benlloch S, Castell JV and
Jover R: Non-invasive prediction of NAFLD severity: A
comprehensive, independent validation of previously postulated
serum microRNA biomarkers. Sci Rep. 8(10606)2018.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Kim TH, Lee Y, Lee YS, Gim JA, Ko E, Yim
SY, Jung YK, Kang S, Kim MY, Kim H, et al: Circulating miRNA is a
useful diagnostic biomarker for nonalcoholic steatohepatitis in
nonalcoholic fatty liver disease. Sci Rep. 11(14639)2021.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Liu J, Xiao Y, Wu X, Jiang L, Yang S, Ding
Z, Fang Z, Hua H, Kirby MS and Shou J: A circulating microRNA
signature as noninvasive diagnostic and prognostic biomarkers for
nonalcoholic steatohepatitis. BMC Genomics. 19(188)2018.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Khalifa O, Errafii K, Al-Akl NS and
Arredouani A: Noncoding RNAs in nonalcoholic fatty liver disease:
Potential diagnosis and prognosis biomarkers. Dis Markers.
2020(8822859)2020.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Jampoka K, Muangpaisarn P, Khongnomnan K,
Treeprasertsuk S, Tangkijvanich P and Payungporn S: Serum miR-29a
and miR-122 as potential biomarkers for non-alcoholic fatty liver
disease (NAFLD). Microrna. 7:215–222. 2018.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Zhou Z, Zhang R, Li X, Zhang W, Zhan Y,
Lang Z, Tao Q, Yu J, Yu S, Yu Z and Zheng J: Circular RNA cVIM
promotes hepatic stellate cell activation in liver fibrosis via
miR-122-5p/miR-9-5p-mediated TGF-β signaling cascade. Commun Biol.
7(113)2024.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Sun Y, Wang H, Li Y, Liu S, Chen J and
Ying H: MiR-24 and miR-122 negatively regulate the transforming
growth factor-β/Smad signaling pathway in skeletal muscle fibrosis.
Mol Ther Nucleic Acids. 11:528–537. 2018.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Xu R, Zhang Z and Wang FS: Liver fibrosis:
Mechanisms of immune-mediated liver injury. Cell Mol Immunol.
9:296–301. 2012.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Dietrich P and Hellerbrand C:
Non-alcoholic fatty liver disease, obesity and the metabolic
syndrome. Best Pract Res Clin Gastroenterol. 28:637–653.
2014.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Younossi ZM, Koenig AB, Abdelatif D, Fazel
Y, Henry L and Wymer M: Global epidemiology of nonalcoholic fatty
liver disease-meta-analytic assessment of prevalence, incidence,
and outcomes. Hepatology. 64:73–84. 2016.PubMed/NCBI View Article : Google Scholar
|